- Hydration refers to the process of maintaining adequate fluid levels in the body for optimal physiological functions.
- Proper hydration supports kidney function by aiding in the filtration of toxins, regulating electrolytes, and preventing kidney stones.
- Dehydration increases the risk of kidney strain, infections, and chronic kidney disease, emphasizing the importance of consistent fluid intake.
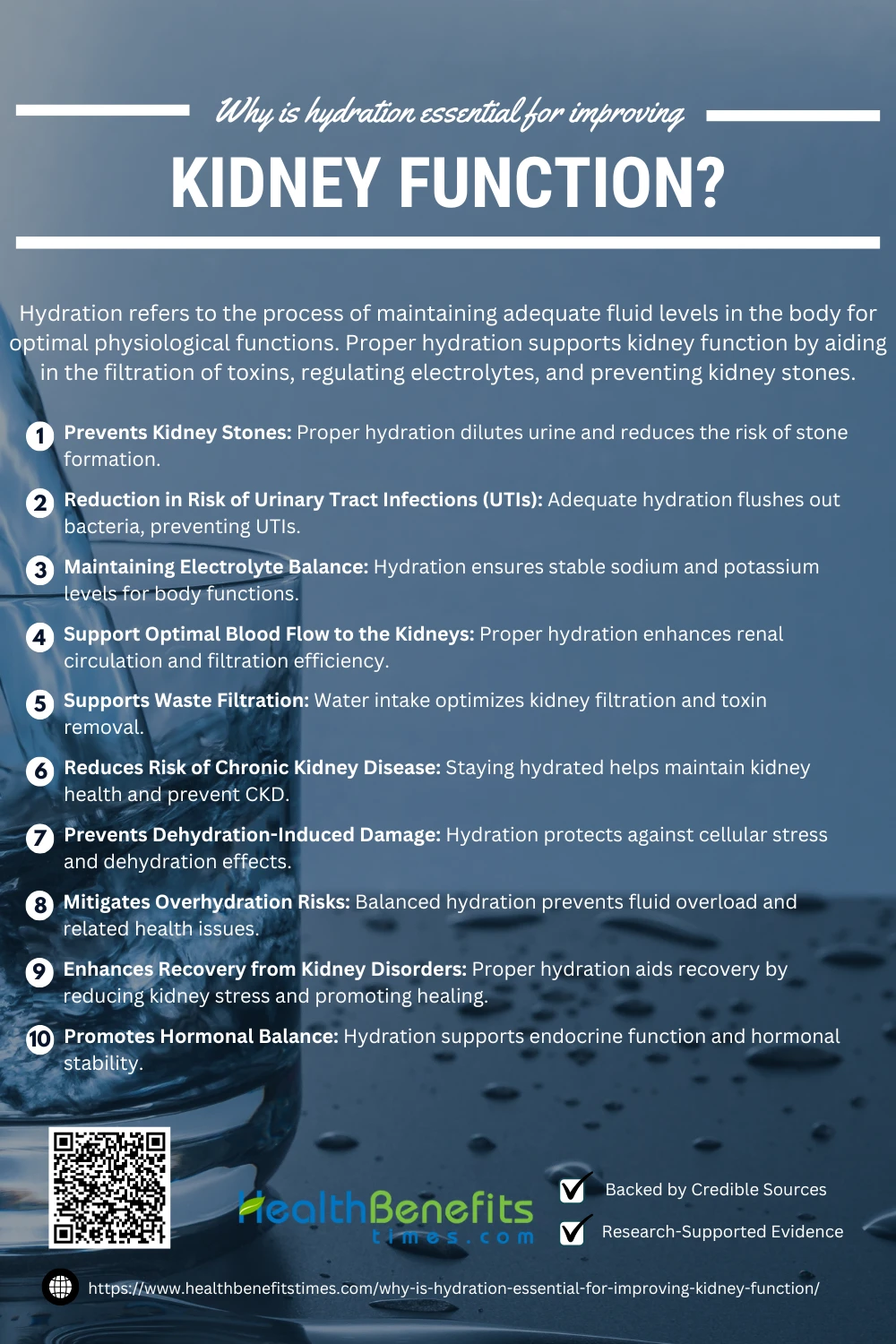
 Hydration is the process of maintaining an adequate balance of fluids in the body to support physiological processes such as digestion, circulation, and temperature regulation (1). Proper hydration is critical for kidney function because the kidneys play a central role in filtering waste, balancing electrolytes, and managing fluid levels in the body. Chronic dehydration has also been linked to the development of kidney disease due to prolonged exposure to concentrated waste products (2).
Hydration is the process of maintaining an adequate balance of fluids in the body to support physiological processes such as digestion, circulation, and temperature regulation (1). Proper hydration is critical for kidney function because the kidneys play a central role in filtering waste, balancing electrolytes, and managing fluid levels in the body. Chronic dehydration has also been linked to the development of kidney disease due to prolonged exposure to concentrated waste products (2).
Additionally, maintaining optimal hydration aids in blood pressure regulation, a critical factor in preventing kidney damage (3). On the other hand, excessive fluid intake without medical guidance may stress kidney function, underscoring the importance of balanced hydration (4). Hydration is particularly important for individuals with existing kidney issues, as it can slow disease progression and reduce complications (5).
Brief overview of kidney function and its importance in the body.
The kidneys are vital organs responsible for filtering waste, balancing electrolytes, and regulating blood pressure. They maintain homeostasis by removing toxins and excess fluids (6). Impaired kidney function can lead to chronic diseases, emphasizing their role in overall health (7). Proper hydration and nutrition are essential for kidney efficiency (8). Understanding kidney function underscores the importance of preventive care (9).
Connection between hydration and kidney health.
Proper hydration is essential for kidney health as it helps dilute urine and prevent the formation of kidney stones. Chronic dehydration is a key risk factor for renal dysfunction (10). Sufficient water intake supports waste removal and electrolyte balance (11). Overhydration, however, may lead to stress on the kidneys.
Why Is Hydration Essential for Improving Kidney Function?
Proper hydration is crucial for maintaining healthy kidney function. The kidneys rely on water to filter waste, regulate electrolytes, and maintain fluid balance. Dehydration can strain the kidneys, leading to potential complications like kidney stones or infections. This article explores how staying hydrated supports kidney health and enhances overall well-being.
 1. Prevents kidney stones
1. Prevents kidney stones
Proper hydration is a key strategy for preventing kidney stones by diluting urine and reducing the concentration of stone-forming substances like calcium oxalate (12). Regular water intake helps flush out toxins and minimizes the risk of crystal formation (13). Studies highlight that individuals with higher fluid intake have a significantly reduced incidence of kidney stones (14). Hydration also promotes urinary health, preventing recurrent stone episodes (15). Besides water, balanced hydration through other drinks contributes to maintaining optimal kidney function (16). Adjusting hydration practices according to climate and activity levels further reduces stone risks (17). Personalized hydration approaches have shown promising results in preventing stone recurrence (18).
2. Reduction in risk of urinary tract infections (UTIs).
Proper hydration is a vital measure for preventing urinary tract infections (UTIs) by increasing urine output and flushing out bacteria from the urinary tract (19). Adequate water intake ensures diluted urine, reducing the risk of bacterial colonization (20). Research highlights that hydration improves bladder function and minimizes UTI recurrence (21). It also decreases susceptibility in high-risk groups, such as pregnant women (22). Balanced hydration complements other preventive measures for UTIs (23). Controlled hydration is especially effective for catheter-associated UTIs (24). Promoting hydration awareness can significantly enhance community health (25).
3. Maintaining electrolyte balance
Hydration is essential for maintaining electrolyte balance, which regulates nerve function, muscle contractions, and fluid levels in the body (26). Proper fluid intake ensures sodium and potassium levels remain stable, preventing imbalances that can lead to health issues (27). Electrolyte-rich beverages are particularly effective during intense physical activities (28). Pregnant women benefit from optimal hydration to support fetal development (29). Bone broth has been identified as an alternative for replenishing electrolytes (30). Monitoring hydration through wearable devices is a modern strategy to sustain balance (31). Managing hydration is critical for recovery in athletes and preventing dehydration-related complications (32).
4. Support optimal blood flow to the kidneys
Proper hydration ensures optimal blood flow to the kidneys, facilitating the filtration of waste and maintenance of fluid balance (33). Sufficient water intake prevents dehydration, which can impair renal circulation and reduce filtration efficiency (34). Hydration also helps regulate blood pressure, a critical factor for kidney health (35). In clinical settings, hydration is used to manage conditions affecting renal perfusion (36). Nutritional strategies that emphasize hydration improve kidney oxygenation and toxin removal (37). Modern diagnostic techniques confirm hydration’s role in preventing kidney stress during high metabolic activities (38). Addressing hydration needs is essential for preventing chronic kidney complications (39).
5. Supports Waste Filtration
Hydration is vital for the kidneys’ ability to filter waste products and maintain fluid balance. Adequate water intake ensures proper blood flow, enhancing filtration efficiency and toxin removal (40). Hydration prevents concentrated urine, which can hinder filtration processes (41). It supports electrolyte balance, vital for effective waste transport (42). Regular hydration also reduces the risk of kidney damage from metabolic stress (43). Sustaining hydration is a preventative measure against kidney-related diseases (44).
6. Reduces Risk of Chronic Kidney Disease
Adequate hydration significantly reduces the risk of chronic kidney disease (CKD) by maintaining proper kidney function and preventing dehydration-induced damage (45). Proper fluid intake supports renal filtration, ensuring the removal of toxins and preventing stone formation (46). Hydration is particularly critical in individuals at risk due to hypertension or diabetes (47). Balanced hydration also helps maintain blood pressure, a key factor in CKD prevention (48). Studies highlight that hydration may slow CKD progression by improving electrolyte balance (49). Regular water consumption is an effective strategy for kidney health and disease prevention (50).
7. Prevents Dehydration-Induced Damage
Proper hydration is essential to prevent dehydration-induced damage, ensuring optimal cellular function and maintaining electrolyte balance. Dehydration can impair cognitive performance and lead to heat-related illnesses (51). Hydration mitigates oxidative stress and inflammation, which are exacerbated by dehydration (52). Athletes benefit from hydration’s ability to sustain endurance and recovery (53).
8. Enhances Recovery from Kidney Disorders
Hydration plays a crucial role in aiding recovery from kidney disorders by maintaining electrolyte balance and supporting renal filtration (54). Adequate fluid intake prevents dehydration-induced kidney stress and oxidative damage (55). Research highlights the importance of hydration in optimizing dialysis outcomes for kidney patients (56). Advanced hydration therapies, including electrolyte solutions, enhance recovery (57). Hydration is integral in avoiding relapse and long-term kidney damage (58).
9. Promotes Hormonal Balance
Hydration is fundamental in maintaining hormonal balance by supporting the optimal functioning of the endocrine system. Proper water intake aids in the regulation of hormones such as cortisol, which is linked to stress (59). Adequate hydration enhances cellular hydration, which stabilizes energy-related hormones like insulin (60). Hydration supports the adrenal glands, promoting hormonal resilience during stress (61). Furthermore, it helps balance sex hormones, improving fertility and overall well-being (62).
10. Mitigates Overhydration Risks
Hydration plays a critical role in mitigating overhydration risks by maintaining the delicate balance of electrolytes and fluid levels. Controlled hydration prevents fluid overload, reducing the risk of hyponatremia (63). Balanced fluid intake prevents complications like chronic hypervolemia, which can cause cardiovascular stress (64). Studies show that hydration tailored to body needs can avoid renal stress and electrolyte imbalance (65). Rehydration practices before physical activities effectively prevent water toxicity (66). Personalized hydration approaches are proven to mitigate risks during intense activities (67).
Signs of Dehydration and Its Impact on the Kidneys
Listed below are some of the signs of dehydration and its impact on kidneys
- Dark-Colored Urine: A primary sign of dehydration indicating reduced kidney filtration and concentrated urine.
- Fatigue: Dehydration lowers blood flow, reducing kidney function and causing overall fatigue.
- Acute Kidney Injury (AKI): Severe dehydration can impair renal perfusion, leading to AKI.
- Hypernatremia: An electrolyte imbalance caused by dehydration, stressing kidney filtration.
- Oxidative Stress: Dehydration promotes oxidative damage to kidney cells.
- Decreased Glomerular Filtration Rate (GFR): Chronic dehydration reduces the kidney’s ability to filter waste efficiently.
- Recurrent Infections: Dehydration hinders the kidneys’ ability to flush bacteria, increasing infection risks.
- Electrolyte Imbalance: Dehydration disrupts sodium and potassium levels, affecting kidney homeostasis.
- Chronic Kidney Damage: Prolonged dehydration can exacerbate kidney disease progression.
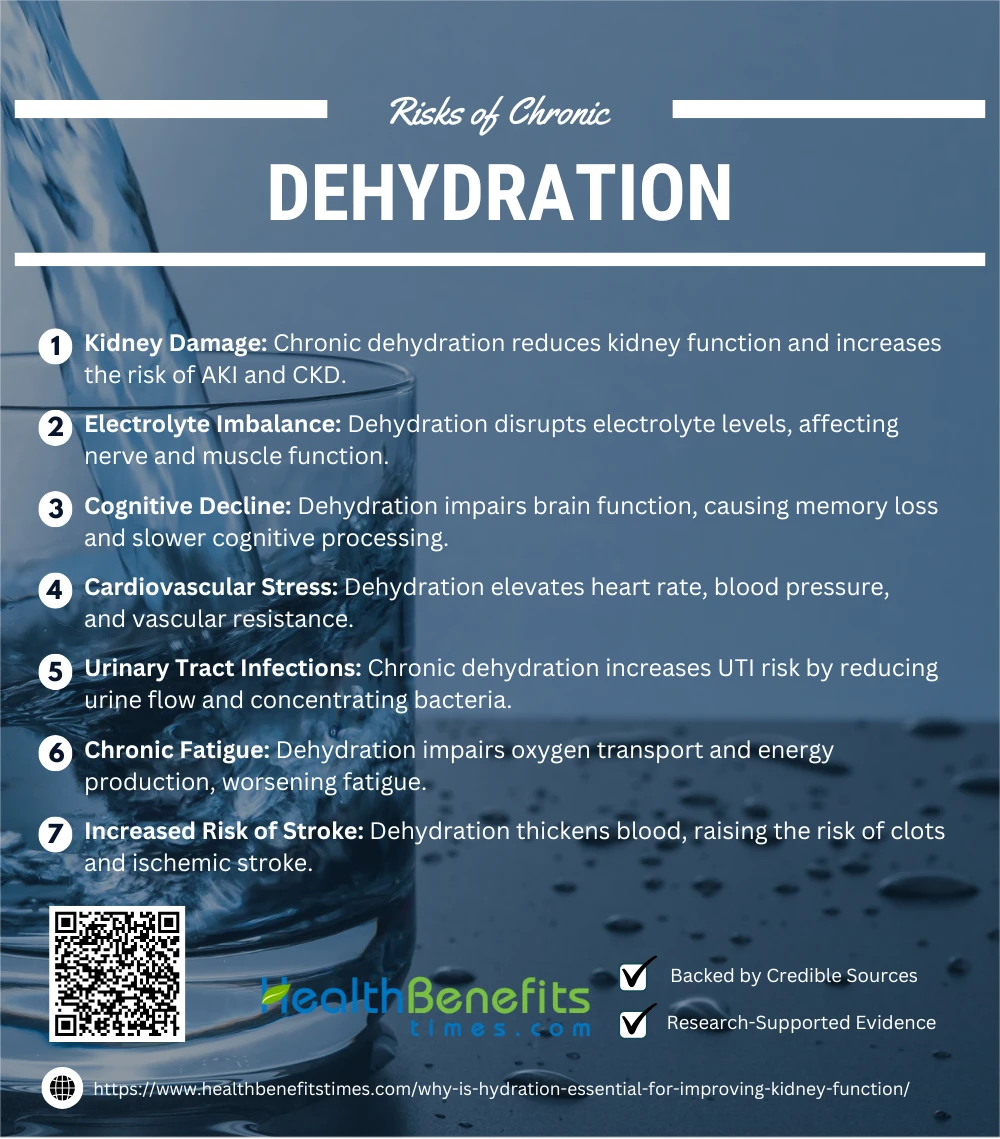
Risks of Chronic Dehydration
Chronic dehydration poses serious risks to overall health, particularly impacting vital organs like the kidneys, heart, and brain. Prolonged lack of adequate water intake can lead to fatigue, digestive issues, kidney stones, and even long-term complications such as chronic kidney disease. Understanding these risks highlights the importance of prioritizing daily hydration for overall well-being.
 1. Kidney Damage
1. Kidney Damage
Chronic dehydration impairs kidney function, increasing the risk of acute kidney injury (AKI) and chronic kidney disease (CKD) (68). Dehydration reduces blood flow to the kidneys, causing ischemic damage and tubular necrosis (69). It accelerates the progression of CKD by promoting oxidative stress and inflammation (70). Furthermore, prolonged dehydration worsens nephrotoxicity caused by medication or metabolic waste (71). Rehydration and prevention strategies are crucial to mitigate these risks (72).
2. Electrolyte Imbalance
Chronic dehydration disrupts electrolyte levels, impairing key bodily functions like nerve signaling and muscle contractions (73). Prolonged fluid loss leads to imbalances such as hypernatremia, often linked with acute kidney injury (74). Additionally, severe dehydration from conditions like cholera magnifies electrolyte loss (75). Timely rehydration is critical for restoring balance and preventing systemic complications (76).
3. Cognitive Decline
Chronic dehydration impairs brain function, leading to memory loss, decreased focus, and slower cognitive processing (77). Dehydration reduces cerebral blood flow, impairing oxygen delivery and nutrient transport to the brain (78). Prolonged fluid deficiency exacerbates oxidative stress, contributing to neuronal damage (79). Older adults are particularly susceptible due to pre-existing conditions and reduced thirst perception (80). Timely hydration prevents cognitive decline and supports mental clarity (81).
4. Cardiovascular Stress
Chronic dehydration elevates cardiovascular stress by reducing blood volume, leading to increased heart rate and blood pressure (82). Dehydration impairs the heart’s ability to pump effectively, raising the risk of ischemic conditions (83). Prolonged fluid deficiency exacerbates vascular resistance, causing hypertension (84). It also promotes oxidative stress, damaging endothelial cells critical for vascular health (85).
5. Urinary Tract Infections
Chronic dehydration increases the risk of urinary tract infections (UTIs) by reducing urine flow and concentrating harmful bacteria (86). This concentrated urine provides an environment for bacterial growth, worsening infection risk (87). Prolonged dehydration also exacerbates inflammation in the urinary tract, reducing natural defenses (88). UTIs are especially severe in older adults with persistent dehydration (89). Effective hydration flushes out bacteria, reducing UTI recurrence (90).
6. Chronic Fatigue
Chronic dehydration contributes to chronic fatigue by impairing oxygen transport and reducing energy production at the cellular level (91). It disrupts electrolyte balance, further diminishing muscle function and endurance (92). Dehydration-induced oxidative stress exacerbates systemic inflammation, worsening fatigue (93). Additionally, dehydration affects the hypothalamus, which regulates energy and circadian rhythms (94). Adequate hydration mitigates these effects and enhances recovery (95).
7. Increased Risk of Stroke
Chronic dehydration increases stroke risk by reducing blood volume, leading to thicker blood and higher chances of clot formation (96). Dehydration impairs blood flow to the brain, exacerbating ischemic damage (97). Prolonged fluid deficiency heightens oxidative stress, further compromising vascular health (98). Vulnerable populations, such as older adults, are particularly at risk (99). Effective hydration strategies can mitigate these risks and support cerebrovascular health (100).
How Much Water Do You Really Need?
Determining daily water needs depends on individual factors such as age, activity level, and environment (101). The “8×8 rule” is often cited but lacks scientific consensus (102). Optimal hydration supports metabolic processes, cognitive function, and kidney health . Excessive hydration, however, can lead to water intoxication (103). Personalized hydration plans tailored to dietary intake and physical exertion are recommended (104). Seasonal changes also affect fluid requirements (105).
Hydration Strategies for Kidney Health
Listed below are few of the hydration strategies for kidney health
1. Regular Water Intake
Regular water intake is essential for kidney health, reducing the risk of kidney stones and optimizing daily diuresis (106). Proper hydration improves fluid balance, particularly in patients with underlying renal conditions (107). It also minimizes risks of complications in kidney disease by supporting electrolyte balance (108).
2. Electrolyte Balancing
Maintaining electrolyte balance is critical for kidney health, preventing conditions like acidosis and dehydration-induced damage (109). Proper hydration optimizes kidney filtration and electrolyte regulation (110). Balancing sodium and potassium through dietary fluids enhances renal efficiency (111). Personalized hydration strategies significantly improve outcomes in chronic kidney disease (112).
3. Avoiding Excessive Caffeine
Limiting excessive caffeine intake helps maintain kidney health by reducing dehydration and preventing urinary calcium excretion, which can lead to kidney stones (113). Caffeine’s diuretic effects can strain kidney filtration processes, especially in individuals with pre-existing renal conditions (114). Opting for caffeine-free hydration alternatives supports optimal kidney function (115).
4. Monitoring Fluid Intake
Monitoring fluid intake is vital for kidney health, aiding in optimal hydration and preventing dehydration-related complications (116). Regular tracking ensures proper electrolyte balance and reduces the risk of kidney stones (117). Personalized hydration plans improve renal function, especially in vulnerable populations (118).
5. Prehydration during Physical Activity
Prehydration during physical activity minimizes kidney strain, enhances fluid balance, and prevents dehydration-induced renal stress (119). It reduces the risk of acute kidney injury by maintaining optimal hydration levels (120). Tailored prehydration strategies improve endurance and kidney filtration efficiency (121).
6. Hydration Therapy for Kidney Stones
Hydration therapy is crucial for kidney stone prevention, diluting urine and reducing crystal formation risks (122). Increasing fluid intake decreases urinary stone formation by enhancing solute clearance (123). Personalized hydration strategies, including water selection, significantly improve outcomes in stone management (124).
7. Avoiding High-Sodium Diets
Avoiding high-sodium diets reduces kidney stress and prevents fluid retention, which is critical for renal health (125). High sodium levels can exacerbate hypertension and compromise kidney function (126). Limiting sodium intake minimizes the risk of chronic kidney disease progression (127).
8. Using Isotonic Drinks When Needed
Isotonic drinks help maintain fluid balance during high-intensity activities by replenishing electrolytes, supporting kidney health, and preventing dehydration (128). They effectively restore sodium and potassium levels, reducing renal strain. Personalized hydration plans incorporating isotonic beverages enhance renal function (129).
9. Timely Hydration after Procedures
Timely hydration after medical procedures prevents dehydration-induced acute kidney injury, improves renal perfusion, and supports toxin clearance (130). Advanced hydration therapies mitigate renal stress and enhance recovery (131). Personalized hydration protocols are essential for patients undergoing contrast imaging (132).
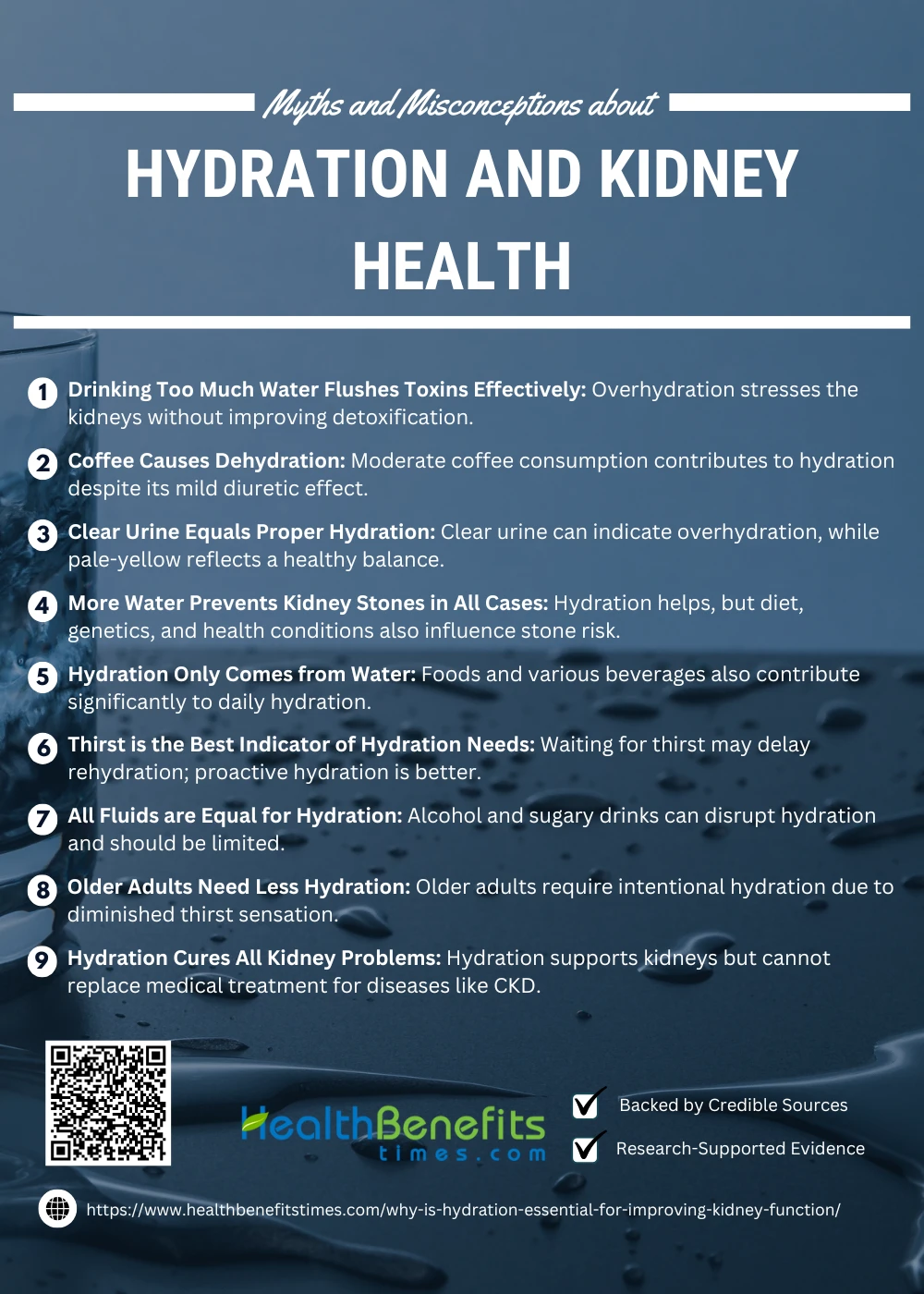
Debunking Myths and Misconceptions about Hydration and Kidney Health
Hydration plays a vital role in maintaining kidney health, but many misconceptions surround its impact. From the idea of needing a fixed daily water intake to fears about caffeinated drinks causing dehydration, these myths can mislead individuals and affect their hydration habits. This article aims to debunk common myths and clarify the truth about hydration and its relationship with kidney health.
 1. Myth: Drinking Too Much Water Flushes Toxins Effectively
1. Myth: Drinking Too Much Water Flushes Toxins Effectively
While hydration is vital for kidney function, overhydrating can stress the kidneys without enhancing their detoxification capabilities. The kidneys already efficiently filter blood to remove waste, and excess water can dilute essential electrolytes, leading to imbalances rather than improved toxin removal.
2. Myth: Coffee Causes Dehydration
Coffee’s mild diuretic effect does not outweigh its contribution to hydration. Studies show that moderate coffee consumption counts towards daily fluid intake, making it a viable hydrating option for most people. Avoiding excessive caffeine, however, is crucial to preventing potential side effects.
3. Myth: Clear Urine Equals Proper Hydration
Urine clarity is not always an indicator of optimal hydration. Overhydration can lead to electrolyte depletion, resulting in clear urine. A pale-yellow color often reflects a healthier balance of hydration and kidney function, aligning with optimal fluid intake.
4. Myth: More Water Prevents Kidney Stones in All Cases
While staying hydrated dilutes urine and reduces the risk of stone formation, other factors like diet, genetics, and medical conditions play significant roles. Excessive water intake alone cannot offset risks from high-sodium diets or oxalate-rich foods, emphasizing a holistic approach.
5. Myth: Hydration Only Comes from Water
Hydration sources extend beyond plain water. Foods like fruits and vegetables, along with fluids like tea, milk, and soups, contribute significantly to daily hydration. Incorporating diverse sources ensures balanced hydration while providing essential nutrients.
6. Myth: Thirst is the Best Indicator of Hydration Needs
Relying on thirst to gauge hydration can lead to delays in rehydration. By the time thirst arises, mild dehydration may already set in. Proactive hydration, especially during high activity or heat, prevents deficits before they impact kidney function.
7. Myth: All Fluids are Equal for Hydration
Fluids like alcohol and sugary drinks may have dehydrating or diuretic effects despite being liquid. These beverages can disrupt electrolyte balance or exacerbate dehydration, underscoring the need to prioritize water, electrolyte drinks, and hydrating foods for kidney health.
8. Myth: Older Adults Need less Hydration
As we age, the sensation of thirst diminishes, increasing dehydration risks in older adults. Proper hydration is crucial for maintaining kidney and overall health in this demographic, highlighting the need for deliberate fluid intake even without noticeable thirst.
9. Myth: Hydration Cures All Kidney Problems
Adequate hydration supports kidney function but cannot cure diseases like chronic kidney disease (CKD). Proper medical treatment, dietary adjustments, and hydration work together to manage renal health effectively, emphasizing a comprehensive approach over reliance on hydration alone.
Conclusion
Hydration is a cornerstone of kidney health, playing a vital role in waste filtration, electrolyte balance, and toxin removal. Without adequate water intake, the kidneys face increased strain, potentially leading to complications like kidney stones, infections, and chronic kidney disease. Prioritizing daily hydration supports optimal kidney function and overall health, underscoring the importance of maintaining consistent fluid intake. By understanding hydration’s critical role, individuals can take proactive steps to protect their kidneys and enhance their well-being.
References:
- (n.d.). Hydration.
- (n.d.). Chronic Dehydration and Kidney Disease.
- American Journal of Kidney Diseases. (n.d.). Hydration and Blood Pressure.
- Clinical Nephrology. (n.d.). Effects of Excessive Hydration.
- National Institute of Diabetes and Digestive and Kidney Diseases. (n.d.). Hydration in Kidney Disease Management.
- Mayo Clinic. (n.d.). Kidney Function Tests.
- National Institutes of Health. (n.d.). Kidney Health.
- Journal of Renal Nutrition. (n.d.). Hydration and Nutrition for Kidney Health.
- American Society of Nephrology. (n.d.). Understanding Kidney Function.
- (n.d.). Hydration and Kidney Disease.
- American Society of Nephrology. (n.d.). Kidney Function and Fluid Balance.
- (2024). Hydration and Urinary Stones.
- (2024). Hydration and Kidney Stone Prevention.
- Journal of Urolithiasis. (2024). Fluid Intake and Stone Risk.
- (2024). Role of Water in Stone Prevention.
- (2024). Hydration Research in Urology.
- (2024). Quality in Sport and Kidney Health.
- (2024). Review on Kidney Health and Hydration.
- (2024). UTI Prevention and Hydration.
- Journal of Family Medicine. (2024). Hydration’s Role in UTI Prevention.
- (2024). Hydration and UTI Risk.
- (2024). Hydration Practices and UTI in Pregnant Women.
- (2024). Safety Profiles in Hydration Practices.
- org. (2024). Hydration for CAUTI Prevention.
- (2024). Community Health and Hydration Awareness.
- (2024). Hydration and Electrolyte Balance Study.
- Klarity Health. (n.d.). What is Sodium Deficiency?.
- Conscious Performance Nutrition. (n.d.). Hydration for Endurance Athletes.
- (n.d.). Pregnancy and Hydration Needs.
- Nutrition for Running. (2024). Bone Broth for Electrolyte Replenishment.
- (2024). Wearables in Hydration Monitoring.
- Savannah Journal of Science. (2024). Strategies for Hydration.
- Journal of Chemical Reviews. (2024). Hydration and Kidney Blood Flow.
- (2024). Hydration and Blood Purification.
- Taylor & Francis. (2024). Renal Function and Hydration.
- ATS Journals. (2024). Hydration in Hypercapnia Management.
- (2024). Comprehensive Therapy for Kidney Circulation.
- (2024). Pharmacometric Impacts of Hydration.
- (2024). Hydration and Kidney Complication Prevention.
- Kidney Research UK. (2024). Hydration and Waste Filtration.
- (2024). Kidney Study on Hydration.
- American Society of Nephrology. (2024). Role of Hydration in Filtration.
- Oxford Clinical Kidney Journal. (2024). Hydration’s Preventive Role in Kidney Health.
- Clinical Kidney Research. (2024). Hydration for Kidney Health.
- (2024). Hydration and Risk Reduction in CKD.
- Frontiers in Nutrition. (2024). Role of Hydration in Nutrition and CKD.
- BMC Medical Case Reports. (2024). Hydration for Diabetic and Hypertensive Patients.
- (2024). Kidney Health and Hydration Science.
- Oxford Clinical Kidney Journal. (2024). Electrolyte Balance and CKD.
- Springer Nature. (2024). Hydration Strategies for CKD Prevention.
- (2024). Dehydration and Cognitive Performance.
- Journal of Cellular Biochemistry. (2024). Dehydration and Oxidative Stress.
- (2024). Hydration and Athletic Performance.
- (2024). Hydration and Kidney Recovery.
- Taylor & Francis. (2024). Renal Protection via Hydration.
- (2024). Hydration in Dialysis Outcomes.
- Oxford Academic. (2024). Clinical Review on Kidney Therapies.
- American Society of Nephrology. (2024). Minimizing Kidney Damage Through Hydration.
- (2024). Hydration and Stress Regulation.
- (2024). Cellular Hydration and Hormonal Stability.
- (2024). Adrenal Function and Stress.
- (2024). Fertility and Hydration Study.
- (2024). Impact of Balanced Hydration on Electrolyte Balance.
- Oxford Academic. (2024). Risks of Chronic Hypervolemia.
- (2024). Overhydration and Electrolyte Imbalance Study.
- Environmental Medicine. (2024). Hydration Status and Physical Activity Risks.
- Springer Nature. (2024). Hydration and Physical Activities.
- (2024). Dehydration and Kidney Health.
- (2024). Renal Homeostasis and Dehydration.
- (2024). Chronic Kidney Damage from Dehydration.
- (2024). Dehydration and Acute Kidney Injury.
- (2024). Case Study on Dehydration-Related AKI.
- (2024). Effects of Dehydration on Electrolytes.
- (2024). Electrolyte Imbalances and Kidney Injury.
- (2024). Cholera and Electrolyte Disturbance.
- Taylor & Francis. (2024). Rehydration and Electrolyte Correction.
- (2024). Study on Cognitive Decline and Dehydration.
- Nature Reviews. (2024). Neurological Effects of Dehydration.
- (2024). Oxidative Stress Linked to Dehydration.
- Frontiers in Medicine. (2024). Impact of Aging and Dehydration on Cognition.
- (2024). Case Report on Dehydration and Cognitive Impairment.
- (2024). Cardiovascular Impacts of Dehydration.
- Frontiers in Medicine. (2024). Dehydration and Heart Function.
- Taylor & Francis. (2024). Hypertension and Chronic Dehydration.
- (2024). Oxidative Stress in Vascular Health.
- Acta Médica Portuguesa. (2024). Dehydration and UTI Risk.
- (2024). UTIs and Urine Concentration.
- Gavin Publishers. (2024). Cystinuria and Dehydration Impact.
- LWW Journal. (2025). Dehydration and UTI in Older Adults.
- The Lancet. (2024). Hydration and Urinary Health.
- Frontiers in Neurology. (2024). Hydration and Fatigue.
- (2024). Chronic Fatigue and Dehydration Study.
- (2024). Oxidative Stress and Fatigue.
- Nature Reviews. (2024). Neurological Impacts of Dehydration.
- Taylor & Francis. (2024). Strategies to Combat Fatigue Through Hydration.
- (2024). Stroke Risk and Dehydration Study.
- Frontiers in Neurology. (2024). Neurological Impacts of Dehydration.
- (2024). Oxidative Stress from Dehydration.
- Taylor & Francis. (2024). Hydration and Elderly Cerebrovascular Health.
- (2024). Cerebrovascular Health and Hydration.
- (2024). Hydration and Water Needs.
- (2024). Daily Water Intake Study.
- (2024). Hydration Risks and Benefits.
- Taylor & Francis. (2024). Personalized Hydration Plans.
- (2024). Seasonal Hydration Changes.
- (2024). Gaps in Kidney Stone Management.
- (2024). Hydration in Renal Health.
- Oxford Clinical Review. (2024). Electrolyte Balance and Kidney Disease.
- Frontiers in Medicine. (2024). Electrolyte Balance in Renal Health.
- (2024). Optimizing Kidney Filtration.
- Acta Nephrology. (2024). Hydration and Electrolyte Management.
- (2024). Clinical Approaches to Kidney Hydration.
- (2024). Caffeine and Kidney Health.
- Wiley Online Library. (2024). Caffeine’s Effect on Kidney Stones.
- (2024). Nutrition and Caffeine-Free Alternatives.
- (2024). Hydration Monitoring for Kidney Health.
- Frontiers in Pediatrics. (2024). Fluid Intake Strategies in Pediatrics.
- Oxford Clinical Kidney Study. (2024). Renal Function and Personalized Hydration.
- (2024). Hydration and Physical Activity.
- Frontiers in Physiology. (2022). Effects of Prehydration on Renal Health.
- (2019). Prehydration to Prevent Renal Stress.
- (2024). Vitamin C and Kidney Stone Therapy.
- (2024). Fluid Intake in Urolithiasis Prevention.
- (2024). Hydration and Crystal Formation.
- (2024). Sodium and Water Handling During Dialysis.
- Frontiers in Nutrition. (2024). Impact of High Sodium on Kidney Health.
- (2019). Dietary Salt and Chronic Kidney Disease.
- Frontiers in Nutrition. (2024). Isotonic Drinks for Kidney Health.
- (2024). Electrolyte Balance and Renal Function.
- (2024). Hydration Strategies for Physical Activity.
- Frontiers in Medicine. (2021). Risk Factors and Hydration for AKI.
- (2024). Hydration and Kidney Function Post-Procedure.
- (2015). Advanced Hydration for Contrast Imaging.

