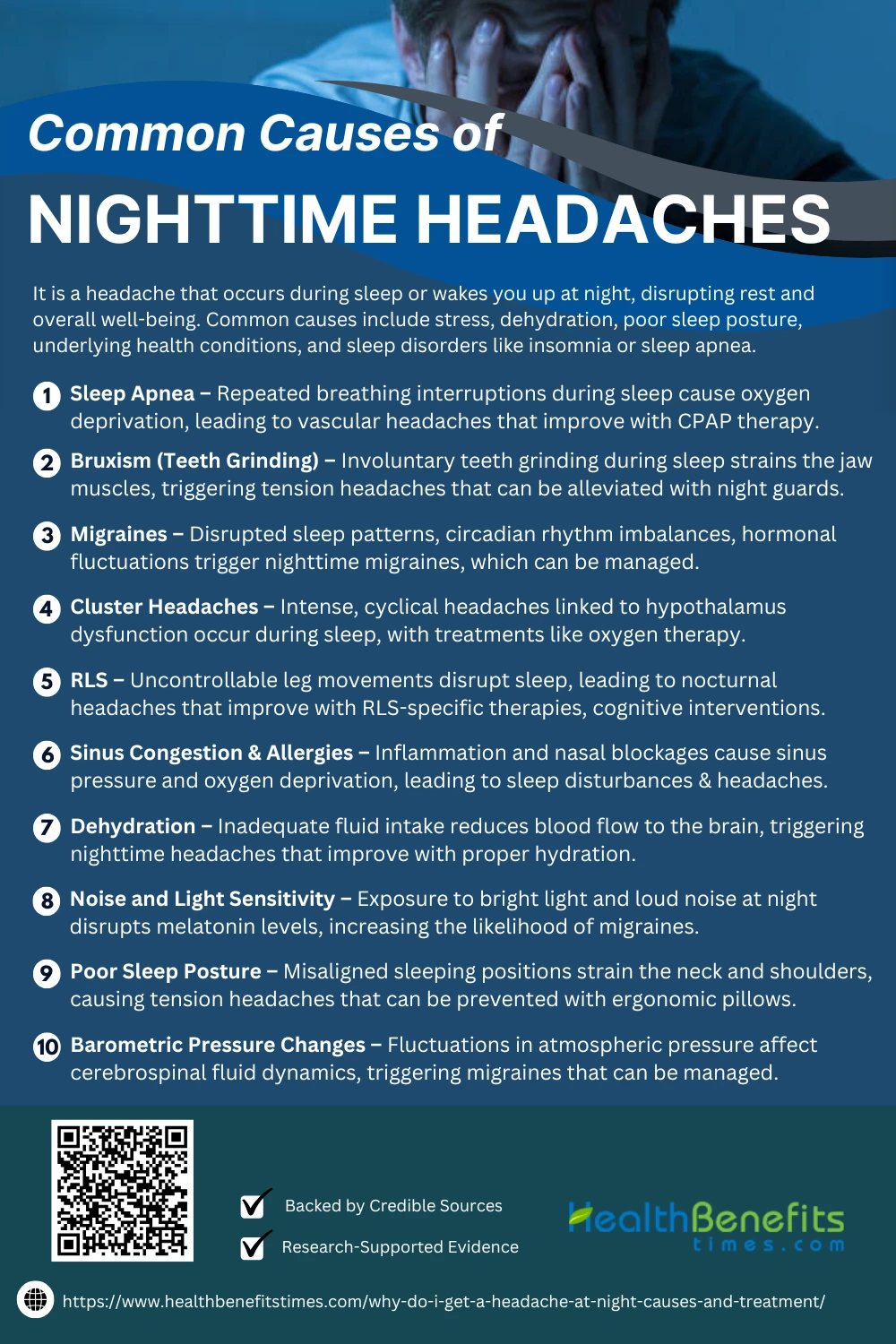
- It is a headache that occurs during sleep or wakes you up at night, disrupting rest and overall well-being.
- Common causes include stress, dehydration, poor sleep posture, underlying health conditions, and sleep disorders like insomnia or sleep apnea.
- Effective treatments involve identifying triggers, improving sleep hygiene, staying hydrated, managing stress, and seeking medical advice if headaches persist.
 Nighttime headaches, also known as nocturnal headaches, refer to recurrent head pain that occurs during sleep or upon waking up, often disrupting rest and affecting overall well-being. (1) These headaches can be caused by various underlying factors, including sleep disorders, dehydration, and neurological conditions. One of the leading causes of nighttime headaches is sleep apnea, a condition where breathing repeatedly stops and starts during sleep, leading to oxygen deprivation and morning headaches. (2) Similarly, bruxism, or nighttime teeth grinding, can lead to tension headaches due to excessive jaw clenching. (1)
Nighttime headaches, also known as nocturnal headaches, refer to recurrent head pain that occurs during sleep or upon waking up, often disrupting rest and affecting overall well-being. (1) These headaches can be caused by various underlying factors, including sleep disorders, dehydration, and neurological conditions. One of the leading causes of nighttime headaches is sleep apnea, a condition where breathing repeatedly stops and starts during sleep, leading to oxygen deprivation and morning headaches. (2) Similarly, bruxism, or nighttime teeth grinding, can lead to tension headaches due to excessive jaw clenching. (1)
Other common triggers include hormonal imbalances, which can cause migraines and cluster headaches, particularly in women experiencing menopause or hormonal fluctuations. (3) Additionally, restless leg syndrome has been linked to nighttime headaches, as it affects sleep quality and increases stress levels. (4) Environmental factors such as poor air quality and barometric pressure changes also contribute to nocturnal headaches, particularly in individuals sensitive to weather fluctuations. (5) Moreover, lifestyle habits, including excessive screen time before bed, can lead to digital eye strain and tension headaches. (6) Effective treatment and prevention strategies depend on identifying the underlying cause. Solutions range from improving sleep hygiene and hydration to medical interventions like CPAP therapy for sleep apnea and medication for migraine relief. (3) By addressing these triggers, individuals can significantly reduce their risk of experiencing nighttime headaches and improve their sleep quality.
Common Causes of Nighttime Headaches
Nighttime headaches can be triggered by various factors, including sleep disorders, poor sleep environment, dehydration, stress, sinus issues, and medical conditions. Identifying the root cause is crucial for effective prevention and treatment.
1. Sleep Apnea
Sleep apnea is a major contributor to nighttime headaches due to repeated interruptions in breathing, leading to oxygen deprivation and increased carbon dioxide levels in the blood. This condition, commonly associated with obstructive sleep apnea (OSA), disrupts sleep cycles and contributes to morning headaches in affected individuals. (7) Studies show that sleep apnea-related hypoxia affects cerebral circulation, triggering vascular headaches that persist throughout the night. (8) Additionally, polysomnographic studies confirm a strong link between OSA and headaches, highlighting the role of nocturnal arousals in worsening head pain. (9) Sleep apnea can also be associated with cardiovascular risks, further intensifying symptoms like headaches and fatigue. (10) Effective treatment with continuous positive airway pressure (CPAP) therapy has been shown to significantly reduce headache frequency and severity in sleep apnea patients. (11)
2. Bruxism (Teeth Grinding)
Bruxism, or involuntary teeth grinding during sleep, is a leading cause of nighttime headaches due to excessive jaw muscle tension and strain on the temporomandibular joint (TMJ). Studies show that bruxism leads to tension headaches, often worsening in the morning due to prolonged jaw clenching. This condition is commonly linked to stress, anxiety, and sleep disorders, exacerbating headache severity. (12) Clinical research suggests that myofascial pain dysfunction syndrome (MPDS) often accompanies bruxism, intensifying headache symptoms. Studies also highlight that occlusal splints and night guards can significantly reduce headache frequency in bruxism sufferers by alleviating pressure on jaw muscles. (1) Additionally, pediatric bruxism has been found to contribute to sleep disturbances and frequent morning headaches in children. (12)
3. Migraines
Migraines are a common cause of nighttime headaches, often triggered by disrupted sleep patterns, hormonal fluctuations, and stress. Research shows that migraine attacks frequently occur during sleep, particularly in those with irregular sleep cycles. (13) Additionally, studies confirm a strong link between sleep disturbances and migraine frequency, suggesting that poor sleep quality may exacerbate migraine episodes. (14) Circadian rhythm disruptions have also been associated with an increased likelihood of nighttime migraines, with research showing that changes in melatonin levels impact headache severity. (15) Furthermore, studies indicate that migraine headaches can be worsened by nighttime awakenings and fragmented sleep, highlighting the role of sleep consistency in migraine management. (16) Treatment strategies focusing on improving sleep hygiene and regulating circadian rhythms have been found to reduce nighttime migraine occurrences and severity. (17)
4. Cluster Headaches
Cluster headaches are among the most severe forms of nighttime headaches, often characterized by intense, unilateral pain around the eye that occurs cyclically during sleep. Research suggests that cluster headaches are linked to disruptions in the hypothalamus, which regulates circadian rhythms, explaining why they frequently strike at night. ({% https://elibrary.ru/item.asp?id=63350943 trusted %}) Studies indicate that oxygen therapy and triptans are effective treatments, reducing the severity and frequency of attacks. Sleep studies reveal that REM sleep disturbances correlate with cluster headache onset, further highlighting their connection to circadian rhythm dysfunction. (18) Preventative measures, such as melatonin supplementation, have shown promise in regulating sleep patterns and reducing nighttime attacks. (19)
5. Restless Leg Syndrome (RLS)
Restless Leg Syndrome (RLS) is a neurological disorder that disrupts sleep by causing uncomfortable leg movements, which can lead to nocturnal awakenings and subsequent headaches. Research highlights a strong comorbidity between RLS and migraine, suggesting that sleep fragmentation from RLS increases headache frequency. (20) Furthermore, studies indicate that dopaminergic dysfunction, a key feature of RLS, plays a role in headache disorders, making individuals more susceptible to nighttime headaches. (4) Clinical trials show that herbal and pharmacological treatments targeting RLS symptoms reduce headache severity, improving sleep quality and overall health. (4) Cognitive-behavioral therapy and relaxation techniques have also been found effective in managing RLS-related sleep disturbances and headaches. (21)
6. Sinus Congestion and Allergies
Sinus congestion and allergies are major triggers of nighttime headaches, as inflammation and nasal blockages lead to increased sinus pressure and disrupted sleep. Research indicates that nasal congestion from allergic rhinitis significantly contributes to nocturnal headaches by causing oxygen deprivation and sleep disturbances. (22) Furthermore, studies highlight that patients with persistent allergic rhinitis are nearly twice as likely to experience sleep-related headaches, emphasizing the link between airway obstruction and headache disorders. (23) Sinus congestion is also associated with higher levels of inflammatory cytokines, which can trigger migraines and tension headaches during sleep. (24) Treatments like nasal corticosteroids and antihistamines have been shown to alleviate symptoms and reduce headache frequency. (25) Additionally, research suggests that steam inhalation and saline nasal irrigation effectively relieve sinus congestion and improve sleep quality, reducing nighttime headache occurrences. (26)
7. Poor Sleep Posture
Poor sleep posture is a significant contributor to nighttime headaches, as improper spinal alignment puts strain on the neck, shoulders, and head muscles, leading to tension-type headaches. Research shows that cervicogenic headaches, caused by poor sleeping positions, often result in morning headaches due to muscle tension and restricted blood flow. (27) Studies also indicate that side sleeping with improper head support can lead to cervical misalignment, exacerbating headache symptoms. (28) Furthermore, prolonged use of high or flat pillows can strain the neck muscles, increasing the risk of headaches during sleep. (29) Correcting sleep posture through ergonomic pillows and proper spinal alignment techniques has been shown to significantly reduce headache frequency and improve sleep quality. (30)
8. Dehydration
Dehydration is a well-documented cause of nighttime headaches, as insufficient fluid levels lead to reduced blood volume and oxygen delivery to the brain. Studies confirm that mild to moderate dehydration can trigger headaches, particularly during sleep, when fluid intake is naturally restricted. (31) Additionally, fluid imbalances have been linked to increased nighttime headache frequency, as dehydration can cause electrolyte imbalances, further exacerbating head pain. (32) Pediatric research highlights that children experiencing dehydration-related headaches often wake up with morning headaches, emphasizing the role of hydration in sleep quality. (33) Increasing water intake and addressing chronic dehydration through proper hydration strategies has been shown to significantly reduce nighttime headaches. (34)
9. Noise and Light Sensitivity
Exposure to bright light and loud noise at night can trigger headaches and sleep disturbances, especially in individuals prone to migraines or tension headaches. Studies confirm that light sensitivity (photophobia) and noise sensitivity (phonophobia) contribute to sleep-related headaches, disrupting melatonin production and neurological stability. (35) Furthermore, excessive blue light exposure before bed has been shown to disrupt circadian rhythms, increasing the likelihood of nighttime migraines. (36) Individuals with neurological hypersensitivity disorders are more prone to experiencing nocturnal headaches triggered by light and sound exposure. (37) Reducing screen exposure, using blackout curtains, and maintaining a quiet sleep environment are effective in minimizing headache occurrences at night. (38)
10. Barometric Pressure Changes
Fluctuations in barometric pressure are a well-documented cause of nighttime headaches, particularly in individuals sensitive to weather changes. Research indicates that drops in atmospheric pressure can cause vascular changes in the brain, triggering migraine-like headaches during sleep. (39) Studies suggest that barometric pressure shifts can alter cerebrospinal fluid dynamics, leading to increased intracranial pressure and headache onset. Additionally, low pressure is linked to higher histamine levels, which may contribute to vascular headaches at night. (40) Managing these headaches involves stabilizing indoor air pressure, staying hydrated, and using preventive medications when pressure drops are expected. (41)
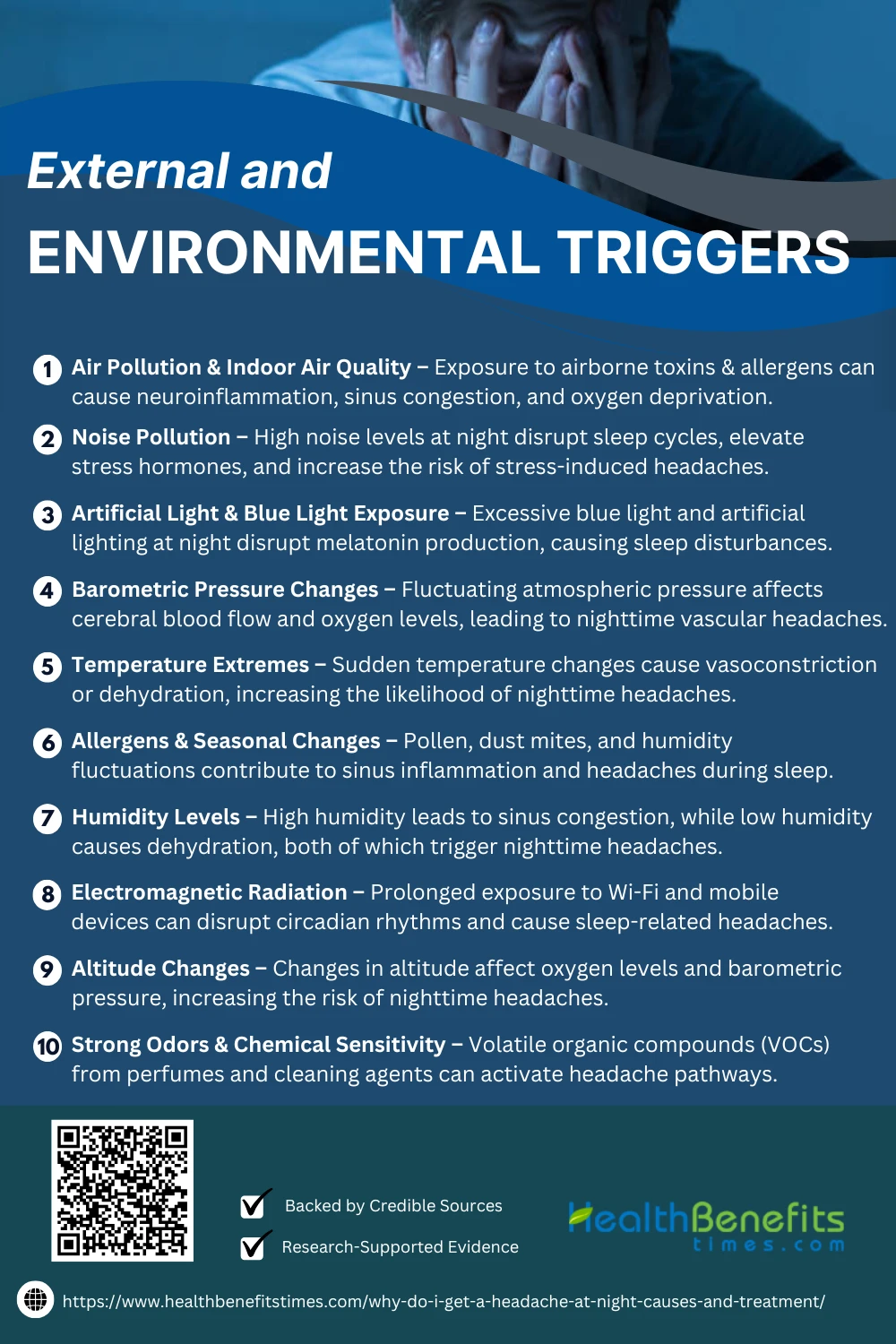
External and Environmental Triggers
External and environmental factors like noise, bright lights, poor air quality, and uncomfortable bedding can trigger nighttime headaches. Identifying these triggers can help improve sleep quality and prevent recurring headaches.
1. Air Pollution & Poor Indoor Air Quality
Exposure to air pollution and poor indoor air quality has been directly linked to nighttime headaches, as airborne toxins and allergens can cause neuroinflammation and vasodilation, leading to head pain. Studies suggest that prolonged exposure to fine particulate matter (PM2.5) increases the risk of developing chronic headaches and sleep disturbances. (42) Research also confirms that indoor pollutants such as volatile organic compounds (VOCs) and mold spores contribute to sinus congestion and headaches during sleep. (43) Additionally, studies reveal that carbon dioxide buildup from poor ventilation can trigger oxygen deprivation-related headaches in enclosed spaces. (44)
2. Noise Pollution
Exposure to high noise levels at night disrupts sleep cycles and triggers stress-related headaches, particularly in urban environments. Studies indicate that chronic exposure to traffic and industrial noise increases nighttime headache frequency due to elevated cortisol levels and vascular tension. (45) Research further suggests that rail noise pollution is linked to increased sleep disturbances and tension headaches, particularly in individuals living near railway tracks. (46) Additionally, constant low-frequency noise can contribute to neurological hypersensitivity, increasing headache severity during sleep. (47) Implementing soundproofing measures and using white noise machines has been shown to reduce noise-induced headaches and improve sleep quality. (48)
3. Artificial Light & Blue Light Exposure
Exposure to artificial light and blue light before bedtime can disrupt melatonin production and increase the risk of nighttime headaches. Studies show that prolonged blue light exposure can worsen migraines and tension headaches by overstimulating the brain and affecting circadian rhythms. (49) Research further suggests that LED and fluorescent lighting can cause visual strain and headaches, particularly in individuals sensitive to light flickering. (50) Additionally, excessive evening blue light exposure has been linked to neuroinflammation, a common trigger for chronic headaches. (51) Implementing blue light filters and dimming lights before bedtime has been shown to reduce light-induced headaches and improve sleep quality. (52)
4. Barometric Pressure Changes
Fluctuations in barometric pressure can trigger vascular headaches by affecting cerebral blood flow and oxygen levels, especially at night. Studies indicate that rapid pressure drops can dilate blood vessels, increasing headache intensity in individuals prone to migraines. (53) Preventive strategies, such as adjusting sleep environments and hydration levels, have been shown to mitigate barometric pressure-induced headaches. (41)
5. Temperature Extremes
Exposure to extreme temperatures has been identified as a significant environmental trigger for nighttime headaches. Studies indicate that sudden temperature drops can cause vasoconstriction, leading to migraine onset, whereas extreme heat increases dehydration and dilates blood vessels, exacerbating headache symptoms. Furthermore, research suggests that seasonal variations and rapid weather changes can influence headache frequency, particularly in individuals prone to migraines. A study published in the Journal of Headache and Pain (54) highlights the role of barometric pressure shifts in nocturnal headache occurrences. Additionally, findings from the American Headache Society (55) emphasize that cold exposure can trigger cluster headaches in susceptible individuals. Research conducted by Neurology & Therapy (56) suggests that heat waves contribute to an increased prevalence of tension-type headaches. Moreover, a systematic review in Cephalalgia associates temperature fluctuations with increased headache frequency, stressing the importance of maintaining a stable sleep environment for prevention.
6. Allergens & Seasonal Changes
Allergens and seasonal changes are significant triggers for nighttime headaches, particularly in individuals with allergic rhinitis and sinus-related conditions. Studies suggest that increased pollen counts during spring and autumn can exacerbate inflammation in the sinuses, leading to nighttime migraine episodes. (57) Additionally, barometric pressure fluctuations and humidity shifts contribute to headache onset, as documented in research from the Headache Journal. (58) Indoor allergens, such as dust mites and mold spores, are linked to disrupted sleep and increased headache prevalence, as highlighted by Environmental Health Perspectives. (59) Furthermore, temperature variations between seasons can impact vascular function, affecting headache frequency, according to findings in The Journal of Neurology. (60)
7. Strong Odors & Chemical Sensitivity
Exposure to strong odors and chemical sensitivity are major external triggers of nighttime headaches, particularly in individuals prone to migraines. Research suggests that airborne chemicals such as volatile organic compounds (VOCs) from cleaning products and perfumes can activate the trigeminal nerve, leading to headache onset during sleep. (61) Additionally, studies have shown that multiple chemical sensitivity (MCS) is linked to disrupted sleep patterns and chronic headaches in affected individuals. (62) Prolonged exposure to environmental irritants has been associated with increased oxidative stress and neuroinflammation, which exacerbates headache frequency and intensity. Implementing air filtration and reducing chemical exposure have been found to significantly reduce headache episodes, improving overall sleep quality.
8. Humidity Levels
Humidity fluctuations, particularly high nighttime humidity, have been identified as a potential trigger for headaches due to their impact on sinus pressure and sleep quality. Research suggests that increased moisture in the air can lead to nasal congestion, promoting sinus headaches and migraines during sleep. (63) Additionally, variations in humidity levels influence barometric pressure, which has been linked to migraine onset and intensity. (64) A recent study found that individuals with chronic migraines reported heightened sensitivity to environmental humidity changes, leading to sleep disturbances and headache episodes. (65)
9. Electromagnetic Radiation (EMF Exposure)
Exposure to electromagnetic radiation (EMR) from electronic devices has been suggested as a potential trigger for nighttime headaches due to its impact on melatonin production and neurological function. (66) Research indicates that prolonged exposure to radiofrequency electromagnetic fields (RF-EMFs) from mobile devices can disrupt sleep patterns, leading to increased headache prevalence. Additionally, studies highlight that individuals with electromagnetic hypersensitivity (EHS) report more frequent headaches when exposed to Wi-Fi signals during sleep. (67) Further evidence suggests that blue light from screens can exacerbate headache symptoms by causing strain on the visual cortex and disrupting circadian rhythms.
10. Altitude Changes
Changes in altitude have been recognized as a significant external trigger for nighttime headaches, primarily due to fluctuations in barometric pressure and oxygen levels. (68) Studies indicate that higher altitudes can lead to hypoxia, which increases cerebrovascular dilation and intracranial pressure, contributing to headache onset during sleep. Furthermore, rapid altitude shifts can disturb sleep patterns and cause dehydration, both of which are closely associated with headache development. Individuals prone to migraines are particularly susceptible to altitude-induced headaches due to heightened vascular sensitivity. (69)
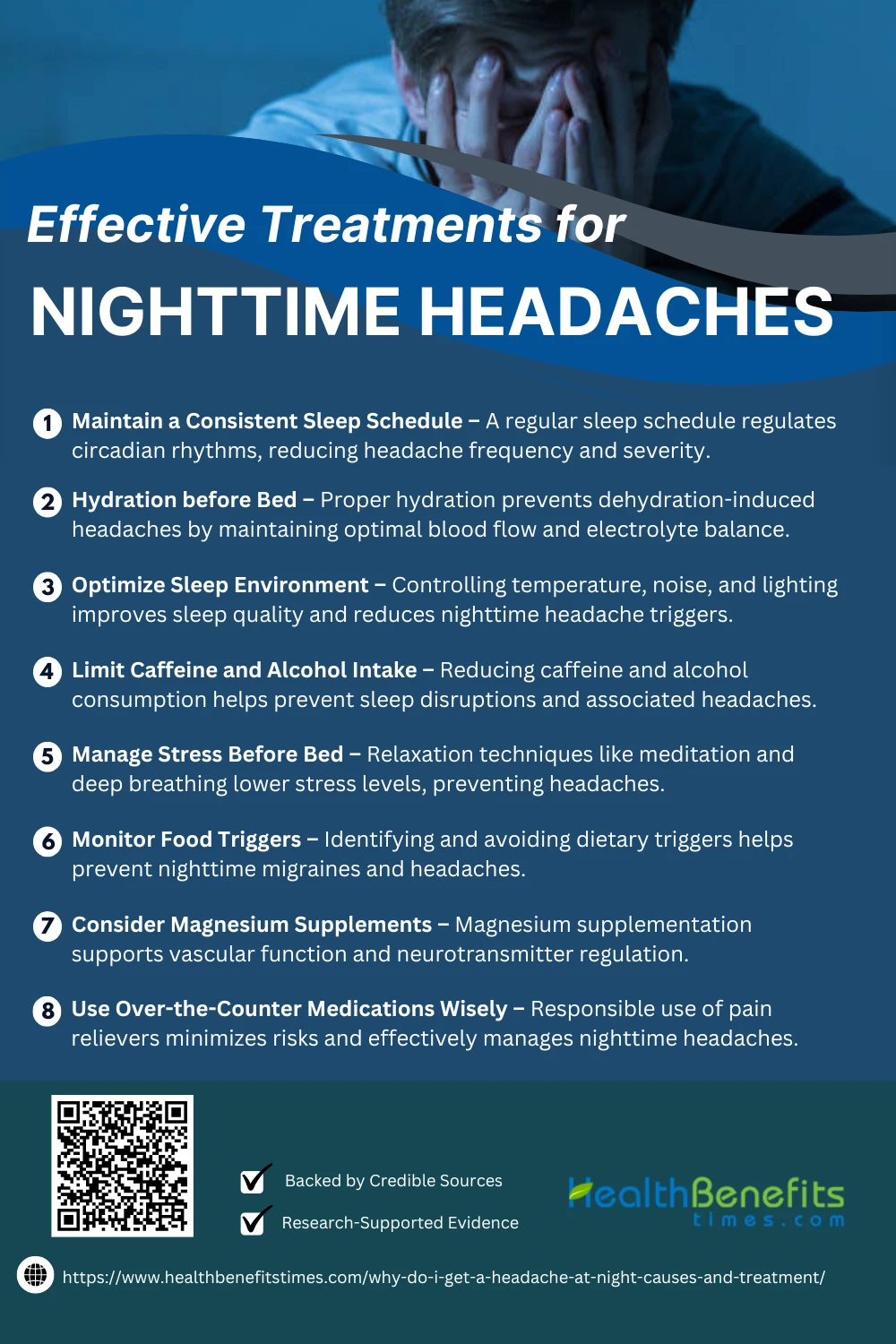
Effective Treatments for Nighttime Headaches
Waking up with a headache at night can disrupt sleep and affect your well-being. Understanding the causes and exploring effective treatments can help you manage nighttime headaches and enjoy restful sleep.
1. Maintain a Consistent Sleep Schedule
Maintaining a consistent sleep schedule has been shown to reduce the frequency and severity of nighttime headaches by regulating the body’s circadian rhythms. (70) Research suggests that irregular sleep patterns contribute to stress and hormonal imbalances, which can trigger headaches during the night. Studies also indicate that stable sleep habits improve melatonin production, promoting deeper sleep and reducing headache risk. Furthermore, individuals with chronic headaches who follow a structured sleep routine report fewer disruptions and lower headache intensity. (71)
2. Hydration before Bed
Hydration before bed plays a critical role in preventing nighttime headaches by maintaining optimal electrolyte balance and preventing dehydration, a common headache trigger. (72) Research indicates that insufficient water intake can lead to increased blood viscosity, reducing oxygen flow to the brain and contributing to headache onset. Furthermore, studies suggest that proper hydration improves sleep quality, reducing the likelihood of sleep disturbances that may cause headaches. Drinking enough fluids, especially electrolyte-rich beverages, before bedtime has been shown to reduce the frequency and severity of headaches in individuals prone to nocturnal migraine attacks. (73)
3. Optimize Sleep Environment
Optimizing the sleep environment is an effective treatment for nighttime headaches, as research suggests that temperature regulation, noise reduction, and light control significantly improve sleep quality and reduce headache frequency. (74) Studies indicate that exposure to artificial light before bedtime suppresses melatonin production, leading to poor sleep and headache onset. Additionally, maintaining a room temperature between 60-67°F (15-19°C) has been shown to prevent headaches by promoting deeper sleep cycles.
4. Limit Caffeine and Alcohol Intake
Reducing caffeine and alcohol intake has been shown to alleviate nighttime headaches by minimizing their stimulant and vasodilatory effects. Studies highlight that excessive caffeine consumption disrupts sleep patterns, leading to increased headache susceptibility. (75) Furthermore, alcohol consumption is linked to heightened morning headache risk due to its impact on sleep quality. (76) Research suggests that people with migraines benefit significantly from avoiding alcohol and caffeine, as these substances can act as dietary triggers. (77) Additionally, caffeine dependency may lead to rebound headaches, necessitating careful intake regulation. (78)
5. Manage Stress Before Bed
Using supportive pillows and mattresses significantly reduces nighttime headaches by improving spinal alignment and sleep quality. Research shows that latex pillows help control waking headaches by minimizing cervical strain. (79) Proper pillow conditions promote high-quality sleep, reducing headaches and neck stiffness. (80) Integrating pillow and mattress design optimizes spinal support, alleviating nocturnal pain and headache symptoms. (81) Sleep ergonomics research confirms that head support alignment reduces pressure points, preventing morning headaches. (82)
6. Monitor Food Triggers
Monitoring food triggers is an effective approach for managing nighttime headaches by reducing dietary-induced migraine occurrences. Studies suggest that tracking triggers in a headache diary helps identify patterns and improve treatment outcomes. (83) Research indicates that common dietary culprits, such as alcohol and processed foods, contribute to nighttime headache frequency. (84) Additionally, personalized dietary modifications can help mitigate nocturnal headaches by addressing food sensitivities. (85)
7. Consider Magnesium Supplements
Magnesium supplements effectively reduce nighttime headaches by regulating neurotransmitters and vascular function. Studies indicate that magnesium deficiency contributes to nocturnal migraines, and supplementation helps alleviate symptoms. (86) Clinical trials confirm that magnesium intake significantly reduces migraine frequency and intensity. (87) Furthermore, magnesium oxide supplementation has been shown to improve sleep quality and prevent nocturnal leg cramps, which may be linked to headaches. (88) A systematic review highlights magnesium’s role in reducing chronic headaches and improving sleep health. (89)
8. Use Over-the-Counter Medications Wisely
Using over-the-counter medications wisely can effectively treat nighttime headaches while minimizing risks. Research highlights the importance of choosing appropriate pain relievers and avoiding caffeine-containing formulations before bed. (90) A review emphasizes proper timing for sleep-impacting medications to enhance efficacy. (91) Studies suggest that OTC drugs remain a common first-line treatment for migraine-related nocturnal headaches. (83) However, self-medicating with sleep aids can lead to dependency and decreased melatonin levels, exacerbating sleep disturbances. (92)
When to Seek Medical Help
Seeking medical help for nighttime headaches is essential if they persist, worsen, or disrupt sleep. Studies suggest headaches triggered by sleep disturbances may indicate underlying neurological conditions. (93) Cluster headaches with nocturnal onset require specialist evaluation. (94) Sleep disorders, including REM-related arousals, may exacerbate migraines and should be diagnosed early. (95) Additionally, older adults with frequent nighttime headaches should rule out conditions like sleep apnea. (96)
Conclusion
Nighttime headaches can stem from various causes, including stress, dehydration, sleep disorders, or underlying health conditions. Identifying triggers and adopting proper treatments—such as hydration, stress management, and sleep hygiene—can significantly reduce their occurrence. If headaches persist despite lifestyle changes, consulting a healthcare professional is essential to rule out serious conditions and find effective solutions. Prioritizing good sleep habits and addressing potential medical issues can help you achieve restful, pain-free nights.