- The endocrine system is a network of glands that produce hormones to regulate metabolism, growth, stress, and reproduction.
- Different exercises, including aerobic, strength, and restorative activities, uniquely impact hormonal health and balance.
- A well-rounded exercise routine, combined with proper rest and nutrition, optimally supports a healthy endocrine system.
 The endocrine system is a network of glands and organs that produce and regulate hormones, which are crucial for maintaining homeostasis, metabolism, and growth (1). Exercise plays a pivotal role in supporting endocrine health by influencing hormone secretion and balance. Resistance training, for example, has been shown to enhance anabolic hormone levels like testosterone and growth hormone, which are vital for muscle repair and metabolism (2). Similarly, aerobic exercise improves insulin sensitivity, reducing the risk of type 2 diabetes and other metabolic disorders (3). However, excessive or intense exercise without adequate recovery may lead to disruptions, such as menstrual dysfunctions or chronic stress hormone elevation (4). Combining moderate aerobic and resistance training is often recommended for a balanced endocrine response, supporting stress adaptation and overall hormonal health (5). Moreover, personalized exercise regimens tailored to individual needs can optimize the benefits of physical activity for endocrine function (6). Thus, regular and appropriately planned exercise acts as a cornerstone in maintaining endocrine health.
The endocrine system is a network of glands and organs that produce and regulate hormones, which are crucial for maintaining homeostasis, metabolism, and growth (1). Exercise plays a pivotal role in supporting endocrine health by influencing hormone secretion and balance. Resistance training, for example, has been shown to enhance anabolic hormone levels like testosterone and growth hormone, which are vital for muscle repair and metabolism (2). Similarly, aerobic exercise improves insulin sensitivity, reducing the risk of type 2 diabetes and other metabolic disorders (3). However, excessive or intense exercise without adequate recovery may lead to disruptions, such as menstrual dysfunctions or chronic stress hormone elevation (4). Combining moderate aerobic and resistance training is often recommended for a balanced endocrine response, supporting stress adaptation and overall hormonal health (5). Moreover, personalized exercise regimens tailored to individual needs can optimize the benefits of physical activity for endocrine function (6). Thus, regular and appropriately planned exercise acts as a cornerstone in maintaining endocrine health.
Connection between Exercise and the Endocrine System
Exercise plays a critical role in maintaining and enhancing the functions of the endocrine system. Physical activity stimulates hormone production, such as insulin, cortisol, and growth hormone, which regulate metabolism, stress response, and overall health (7). Regular exercise has been shown to improve the balance of the neuroendocrine system, supporting communication between the brain and hormone-producing glands (8). Additionally, it positively influences the secretion of myokines—hormones released by muscles during exercise—that contribute to reducing inflammation and supporting immune and endocrine functions (9). Evidence also suggests a strong relationship between exercise and the regulation of thyroid hormones, particularly in addressing modifiable risk factors for thyroid conditions (10). Lastly, the impact of exercise on circadian rhythm alignment underscores its role in synchronizing hormonal cycles for optimal physiological health (11).
Types of Exercises and Their Impact on the Endocrine System
Different types of exercise uniquely influence the endocrine system, improving hormone balance, stress management, metabolism, and overall health.
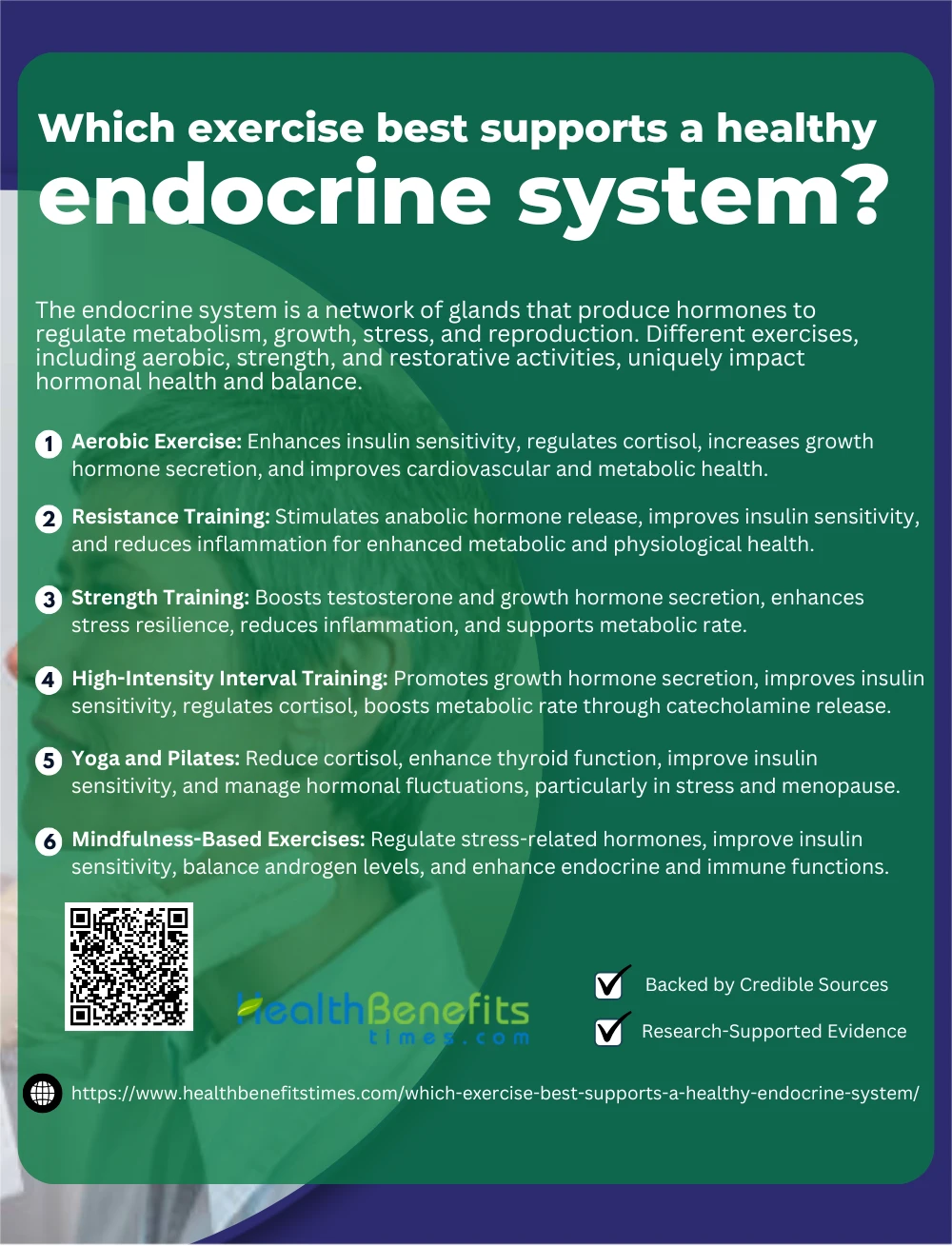 1. Aerobic Exercise
1. Aerobic Exercise
Aerobic exercise has been extensively studied for its profound impact on the endocrine system. Regular aerobic activity enhances insulin sensitivity, improving glucose metabolism and reducing the risk of type 2 diabetes (12). Additionally, it supports hormonal balance by regulating cortisol levels, which helps mitigate stress and promotes overall mental well-being (13). Furthermore, aerobic training increases growth hormone secretion, promoting muscle repair and metabolic health (14). Research also indicates that aerobic exercise can reduce inflammation and improve cardiovascular endocrine markers, reinforcing its role in comprehensive health management (15).
2. Resistance Training
Resistance training is a cornerstone of a healthy endocrine system, as it significantly influences the secretion of hormones essential for muscle growth, metabolism, and overall physiological health. This form of exercise stimulates the release of anabolic hormones like testosterone and growth hormone, which are crucial for muscle repair and protein synthesis (2). Additionally, it increases insulin sensitivity, improving glucose regulation and reducing the risk of metabolic disorders (3). Regular resistance training has been shown to optimize cortisol levels, aiding in the management of stress and preventing chronic fatigue (4). Furthermore, it enhances the production of myokines, cytokines released by muscles during exercise, which play a role in reducing inflammation and supporting metabolic health (5). The long-term endocrine benefits of resistance training also include improvements in bone health by influencing parathyroid hormone and calcitonin, which regulate calcium balance (16).
3. Strength Training
Strength training is highly beneficial for the endocrine system, promoting hormonal adaptations that support metabolic health, stress resilience, and muscle development. It enhances the secretion of testosterone and growth hormone, which are critical for muscle hypertrophy and tissue repair (2). Regular strength training improves insulin sensitivity, aiding in glucose metabolism and lowering the risk of type 2 diabetes (3). Additionally, it helps regulate cortisol levels, mitigating the effects of chronic stress and improving overall stress adaptation (17). Strength training also increases the production of myokines, which play a role in reducing systemic inflammation and enhancing endocrine health (5). Moreover, this type of exercise positively influences thyroid hormones, supporting metabolic rate and energy regulation (4).
4. High-Intensity Interval Training (HIIT)
High-Intensity Interval Training (HIIT) is an effective method to support a healthy endocrine system by promoting hormonal adaptations that enhance metabolism, stress response, and overall health. HIIT has been shown to significantly increase growth hormone secretion, which supports fat metabolism and muscle repair (2). Additionally, it improves insulin sensitivity, aiding in glucose regulation and reducing the risk of metabolic disorders like diabetes (3). This form of training also optimizes the balance of cortisol levels, helping the body better manage stress while preventing chronic hormonal dysregulation (17). HIIT stimulates the production of catecholamines like adrenaline and noradrenaline, which enhance fat oxidation and cardiovascular function (5). Furthermore, HIIT has been linked to positive thyroid hormone responses, boosting metabolic rate and energy balance (4).
5. Yoga and Pilates
Yoga and Pilates are highly effective practices for supporting endocrine health through stress reduction, hormone regulation, and enhanced physical well-being. Yoga, with its emphasis on controlled breathing and relaxation, activates the parasympathetic nervous system, reducing stress-related cortisol levels and promoting a balanced hormonal state (18). Similarly, Pilates has been shown to improve thyroid function, supporting metabolism and energy balance, particularly in sedentary women (19). Both practices are linked to improved insulin sensitivity, contributing to better glucose metabolism and reducing the risk of metabolic disorders (20). Additionally, regular Pilates sessions help regulate cortisol and reduce systemic inflammation, further enhancing endocrine system health (21). Yoga and Pilates are also effective in managing hormonal fluctuations, such as those experienced during menopause, by reducing visceral fat and enhancing hormonal balance (22).
6. Mindfulness-Based Exercises
Mindfulness-based exercises, such as meditation and yoga, significantly contribute to endocrine health by regulating stress-related hormones and improving overall physiological function. These practices are particularly effective in modulating the hypothalamic-pituitary-adrenal (HPA) axis, reducing cortisol levels, and enhancing resilience to stress. Mindfulness-based stress reduction (MBSR) programs have been shown to improve cortisol and dehydroepiandrosterone sulfate (DHEAS) levels, enhancing mental and physical health (23). Furthermore, mindfulness techniques positively impact insulin sensitivity, contributing to better glucose metabolism and reducing the risk of diabetes (24). Studies also highlight the benefits of mindful yoga in balancing androgen levels and improving reproductive health in conditions like polycystic ovary syndrome (25). Additionally, MBSR programs are associated with enhanced endocrine and immune function, leading to improved quality of life in chronic conditions (26).
Lifestyle Factors Supporting Exercise and Hormonal Health
Balanced nutrition, quality sleep, stress management, and regular exercise are key lifestyle factors that support optimal hormonal health.
 1. Balanced Diet
1. Balanced Diet
A balanced diet plays a critical role in optimizing hormonal health and enhancing the benefits of exercise. Proteins, as the building blocks of muscles, support anabolic hormone production, including growth hormone and testosterone, aiding in muscle repair and recovery (1). Healthy fats, particularly omega-3 fatty acids, contribute to the synthesis of steroid hormones, which regulate metabolism and stress responses (16). Micronutrients such as zinc and magnesium are vital for the regulation of insulin and thyroid hormones, directly impacting energy balance and metabolic efficiency (3). Additionally, adequate carbohydrate intake replenishes glycogen stores and mitigates the elevation of cortisol after intense physical activity (2). Finally, hydration paired with an adequate intake of electrolytes ensures optimal cellular function and hormonal signaling during exercise (6).
2. Quality Sleep
Quality sleep is essential for maintaining hormonal balance and optimizing the benefits of exercise. During deep sleep, the body releases growth hormone, which supports muscle repair and tissue regeneration after exercise. Sleep also regulates cortisol levels, preventing the stress hormone from disrupting recovery and metabolic processes (27). Insufficient sleep, on the other hand, can impair glucose metabolism and reduce insulin sensitivity, counteracting the positive hormonal effects of physical activity (28). Research highlights that even partial sleep deprivation alters the secretion of hormones like testosterone, critical for muscle strength and endurance (29). Moreover, exercise itself can improve sleep quality by enhancing the secretion of serotonin, which promotes relaxation and regulates sleep cycles (30).
3. Stress Management
Effective stress management is vital for maintaining hormonal balance and enhancing exercise outcomes. Chronic stress triggers excessive cortisol release, disrupting the hypothalamic-pituitary-adrenal (HPA) axis and impairing recovery and metabolism. Practices like mindfulness meditation reduce cortisol levels and improve insulin sensitivity, which supports overall metabolic health (24). Yoga and other mindfulness-based exercises have been shown to regulate stress-related hormones and improve resilience, promoting better exercise adaptation (25). Regular physical activity itself is a natural stress reliever, enhancing the release of endorphins and reducing the perception of stress (16). Furthermore, engaging in relaxation techniques post-exercise, such as deep breathing, helps restore parasympathetic function and balance hormonal responses (23).
4. Hydration
Proper hydration is critical for maintaining hormonal balance and optimizing exercise performance. Dehydration can impair the release of growth hormone during physical activity, reducing its anabolic effects and hindering muscle repair (31). Adequate hydration helps regulate cortisol levels, mitigating the stress response and supporting recovery after exercise (32). Additionally, hydration status influences the secretion of vasopressin, a hormone essential for fluid balance and thermoregulation during physical activity (33). Furthermore, consistent hydration reduces the risk of heat-related illnesses and ensures optimal cardiovascular function during intense physical exertion (34).
5. Exercise Variety
Incorporating a variety of exercise types enhances hormonal health by activating multiple endocrine pathways, promoting overall balance and adaptation. Resistance training increases anabolic hormones like testosterone and growth hormone, which are critical for muscle repair and recovery (35). Aerobic exercises, on the other hand, improve insulin sensitivity and reduce cortisol levels, enhancing metabolic and stress regulation (1). Combining these modalities with flexibility or balance exercises, such as yoga, supports parasympathetic activation, which mitigates stress-related hormonal imbalances (36). This approach also boosts hippocampal plasticity through increased production of neurotrophic factors influenced by varied exercise routines (37).
6. Consistent Physical Activity
Consistent physical activity is crucial for maintaining hormonal balance and enhancing exercise outcomes. Regular resistance training elevates anabolic hormones such as testosterone and growth hormone, which play essential roles in muscle repair, growth, and overall metabolism (38). Endurance exercises, on the other hand, improve insulin sensitivity, reducing the risk of type 2 diabetes and promoting energy efficiency (39). Research also highlights that consistent exercise mitigates premenstrual distress and stabilizes ovarian steroid hormones in women, contributing to better reproductive health (40). Moreover, consistent activity helps regulate cortisol levels, reducing stress and enhancing recovery (41). Finally, sustained exercise optimizes substrate utilization, improving the body’s ability to convert energy efficiently through better hormonal signaling (42).
7. Minimizing Toxins
Minimizing exposure to toxins is critical for maintaining hormonal health and maximizing the benefits of exercise. Environmental toxins, such as endocrine disruptors found in plastics and pesticides, can interfere with hormone balance, including the regulation of sex hormones like estrogen and testosterone (43). Persistent exposure to mitochondrial toxins can reduce energy production, impairing exercise performance and metabolic health (44). Detoxification strategies, including a clean diet and exercise, have been shown to support the removal of harmful substances and improve cellular sensitivity to thyroid hormones (45). Exercise-induced hormesis can further enhance the body’s resilience to low-dose toxins by promoting adaptive stress responses (46). Lastly, avoiding hormone-disrupting chemicals in food and water, such as bisphenol A (BPA) and phthalates, helps prevent metabolic imbalances and supports endocrine health (47).
8. Proper Recovery
Proper recovery is essential for maintaining hormonal balance and optimizing the benefits of exercise. After resistance training, key anabolic hormones such as testosterone, growth hormone, and IGF-1 are activated, facilitating muscle repair and growth during recovery (48). Post-exercise recovery also helps regulate cortisol levels, reducing stress-induced hormonal imbalances (1). Recovery practices like adequate hydration and nutrition optimize the removal of blood fatigue factors and restore energy stores, which are critical for hormonal homeostasis (49). Women experience unique recovery patterns influenced by hormonal fluctuations, highlighting the importance of tailored recovery strategies (50). Furthermore, biomarkers like testosterone and cortisol during recovery phases provide valuable insights into overall endocrine health and exercise adaptation (51).
9. Avoiding Excessive Exercise
Avoiding excessive exercise is essential for maintaining hormonal balance and preventing negative health outcomes. Overtraining can disrupt the hypothalamic-pituitary-adrenal (HPA) axis, leading to chronic elevations in cortisol levels and reduced anabolic hormones like testosterone, which are critical for muscle repair and overall health (1). Excessive exercise in women is particularly linked to menstrual irregularities and decreased bone density due to suppressed estrogen levels (52). Additionally, overtraining can lead to adrenal insufficiency, compromising recovery and increasing the risk of injury (53). To prevent these effects, balancing physical activity with adequate rest and nutrition is vital for long-term hormonal health (54).
Tips for Creating an Exercise Routine to Support Hormonal Health
Creating an effective exercise routine for hormonal health involves balancing aerobic, strength, and restorative activities, ensuring consistency and gradual progression.
- Incorporate Variety in Exercise
Combining resistance training, aerobic exercises, and flexibility workouts ensures balanced hormonal responses. Resistance training boosts testosterone and growth hormone levels, while aerobic exercise improves insulin sensitivity and reduces cortisol - Maintain Moderate Intensity
Avoid prolonged, high-intensity workouts to prevent overtraining and excessive cortisol release, which can disrupt hormonal balance. - Prioritize Recovery
Incorporate rest days and practices like stretching or yoga to reduce stress and restore hormonal equilibrium. - Schedule Exercise Wisely
Exercise at consistent times each day to support your body’s circadian rhythm and hormonal cycles. - Hydrate Properly
Staying hydrated is crucial for optimal cellular function and hormone regulation during and after exercise. - Balance Exercise with Nutrition
Ensure adequate calorie and nutrient intake to fuel workouts and prevent hormonal disruptions caused by energy deficiencies. - Limit High-Impact Sessions
For women, avoid frequent high-impact or excessive endurance exercises that can negatively affect estrogen levels and reproductive health. - Incorporate Stress-Reducing Activities
Include mindfulness practices, such as yoga or tai chi, to counteract cortisol spikes and promote relaxation. - Listen to Your Body
Adjust your exercise intensity and volume based on how your body feels, ensuring you’re not overtraining or neglecting recovery. - Seek Professional Guidance
Work with a fitness or health professional to tailor an exercise routine that aligns with your hormonal health needs and personal goals.
Potential Risks and Considerations
Excessive exercise or improper routines can disrupt hormonal balance, increase cortisol, and strain the endocrine system, emphasizing moderation and recovery.
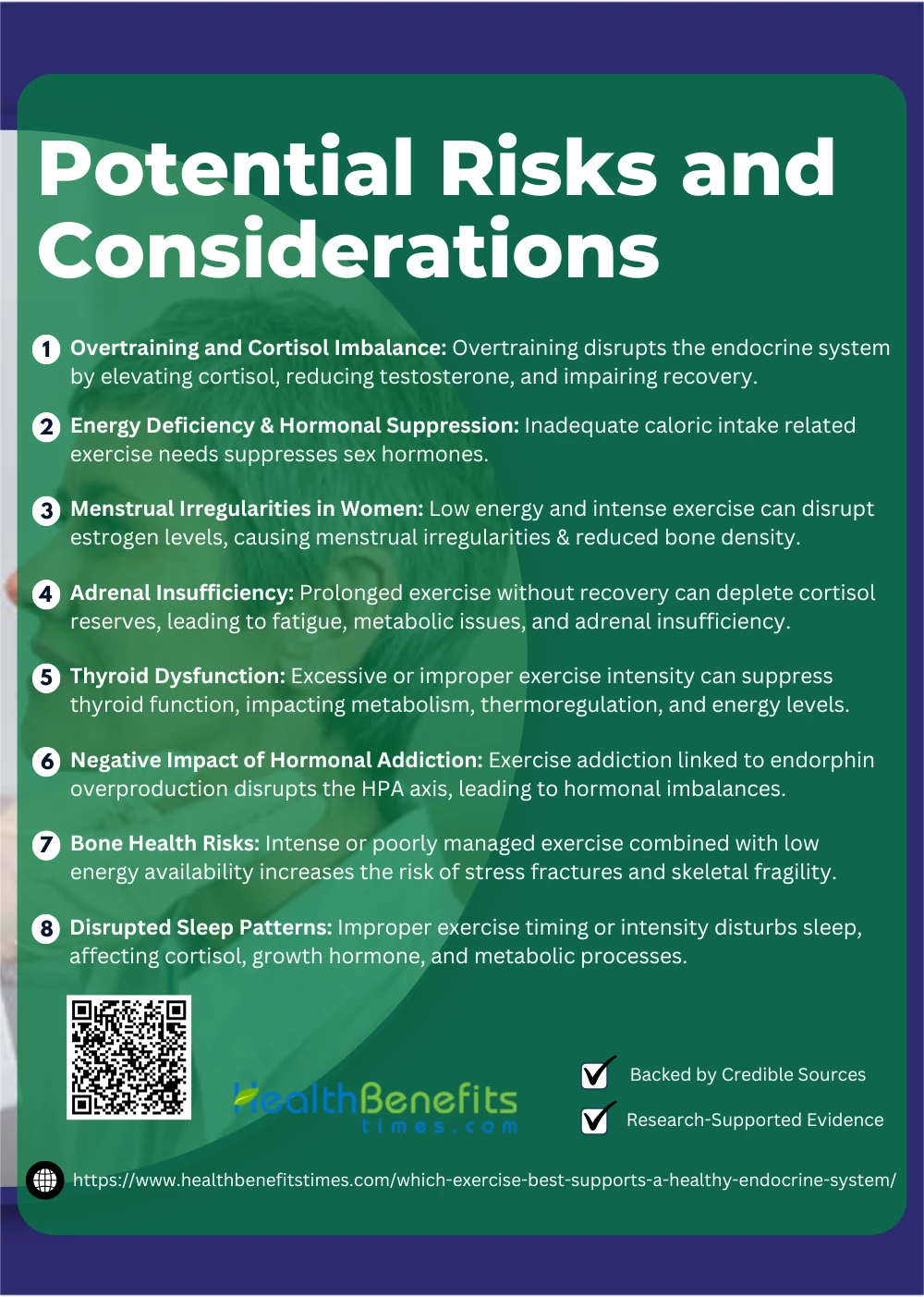 1. Overtraining and Cortisol Imbalance
1. Overtraining and Cortisol Imbalance
Overtraining can severely disrupt the endocrine system, leading to chronic cortisol imbalance and hormonal dysregulation. Prolonged and excessive physical activity elevates cortisol levels, resulting in a catabolic state that hinders muscle repair and adaptation (55). This imbalance affects the hypothalamic-pituitary-adrenal (HPA) axis, with studies showing impaired hormonal responses and adrenal insufficiency in overtrained individuals (53). Overtraining syndrome has also been linked to decreased testosterone levels and impaired gonadal function, exacerbating the negative effects of elevated cortisol (56). Furthermore, diurnal cortisol rhythms are often disrupted, reducing recovery efficiency and overall resilience (57). Maintaining a balance between exercise intensity and recovery is essential to avoid these adverse hormonal effects and promote long-term endocrine health (58).
2. Energy Deficiency and Hormonal Suppression
Energy deficiency caused by inadequate caloric intake relative to exercise demands can lead to significant hormonal suppression, particularly in women. Low energy availability (LEA) disrupts the hypothalamic-pituitary-gonadal (HPG) axis, suppressing the release of sex hormones like estrogen, which is crucial for reproductive health and bone density (59). This condition, often linked to functional hypothalamic amenorrhea, results in menstrual irregularities and exacerbates bone metabolism issues (60). Energy deficits also affect the growth hormone-IGF axis, leading to decreased muscle repair and growth potential (61). Chronic energy deficits can suppress bone turnover markers, further heightening the risk of stress fractures in active populations (62). Additionally, hormonal adaptations to energy deficiency include suppressed testosterone levels in men, affecting overall vitality and metabolic health (63).
3. Menstrual Irregularities in Women
Intense or prolonged exercise can disrupt the hormonal balance necessary for regular menstrual cycles, leading to conditions such as amenorrhea or oligomenorrhea. These menstrual irregularities are often linked to low energy availability, which suppresses the hypothalamic-pituitary-gonadal (HPG) axis and reduces estrogen levels, negatively impacting reproductive and bone health (52). Research highlights that female athletes involved in sports emphasizing leanness are at higher risk of developing such disorders due to energy deficits and excessive training (64). Additionally, subtle menstrual disturbances are prevalent even among recreationally active women, further underscoring the complex interaction between exercise and hormonal health (65). Strenuous training can also impair bone mineral density over time, exacerbating the long-term risks associated with menstrual cycle suppression (66). To mitigate these risks, interventions such as adjusting training intensity and increasing caloric intake are recommended to restore hormonal and menstrual regularity (67).
4. Adrenal Insufficiency
Adrenal insufficiency, often linked to overtraining or stress, occurs when the adrenal glands fail to produce sufficient cortisol and other essential hormones, leading to impaired energy regulation and recovery. Prolonged exercise without adequate recovery can disrupt the hypothalamic-pituitary-adrenal (HPA) axis, decreasing cortisol response and contributing to fatigue and impaired metabolic adaptation (53). This condition, if not managed, may progress to adrenal crisis during high-intensity exercise, as cortisol reserves are insufficient to maintain homeostasis (68). In individuals with primary adrenal insufficiency, physical activity can exacerbate symptoms like hypoglycemia and reduced exercise tolerance due to impaired adrenal hormone production (69). Women with adrenal insufficiency may experience additional challenges in glucose regulation and cardiovascular adaptation during moderate exercise (70). To mitigate risks, strategies such as adjusting exercise intensity and incorporating hydrocortisone supplementation before physical activity have been shown to improve performance and endocrine stability (71).
5. Thyroid Dysfunction
Thyroid dysfunction, particularly hypothyroidism or subclinical hypothyroidism, can be influenced by exercise, highlighting the importance of appropriate intensity and duration in training regimens. Moderate exercise has been shown to enhance thyroid hormone levels, improving metabolism and energy regulation, but excessive intensity may suppress thyroid activity (72). Subclinical hypothyroid patients benefit from aerobic and resistance training, which supports metabolic health and reduces symptoms like fatigue (73). However, individuals with untreated thyroid conditions should avoid high-intensity or prolonged exercise, as it may exacerbate symptoms like decreased thermoregulation and fatigue (74). Thyroid dysfunction in women, particularly during pregnancy, requires careful exercise adjustments, as hormonal imbalances can affect both maternal and fetal health (75). Additionally, combining exercise with dietary and medical interventions, such as vitamin D supplementation, can enhance thyroid function and mitigate metabolic risks (76).
6. Negative Impact of Hormonal Addiction
Exercise addiction, characterized by a compulsive need to engage in physical activity, is linked to hormonal dysregulation and can negatively impact the endocrine system. The overproduction of endorphins and other hormones during prolonged or intense exercise may lead to a dependence on the “high” generated by these biochemical changes, fostering an addiction-like state. This dependency can exacerbate stress on the hypothalamic-pituitary-adrenal (HPA) axis, potentially leading to chronic cortisol elevation and adrenal exhaustion (77). Hormonal imbalance resulting from excessive exercise can also affect dopamine and serotonin levels, contributing to mood instability and further reinforcing the addictive behavior. In extreme cases, exercise addiction can impair reproductive hormones, reducing testosterone in men and disrupting estrogen cycles in women (78). To address these risks, monitoring exercise intensity and incorporating psychological support can help mitigate the adverse effects of hormonal addiction (79).
7. Bone Health Risks
While exercise is crucial for improving bone strength and density, excessive or improperly managed physical activity can pose risks to bone health through hormonal imbalances. Intense exercise in women, especially in combination with low energy availability, can suppress estrogen production, leading to a condition known as the Female Athlete Triad, which increases the risk of stress fractures (4). Prolonged overtraining can also impair bone metabolism by disrupting the endocrine and paracrine regulation of bone remodeling (80). These risks are not limited to athletes; improper exercise regimens in older adults with existing endocrine issues may exacerbate skeletal fragility, further increasing fracture susceptibility (81). Careful exercise planning, incorporating adequate nutrition and recovery, is essential to mitigate these risks and optimize the bone-strengthening benefits of physical activity (82).
8. Disrupted Sleep Patterns
Disrupted sleep patterns caused by improper exercise timing or excessive physical activity can significantly impact the endocrine system. Sleep deprivation impairs the hypothalamic-pituitary-adrenal (HPA) axis, resulting in elevated cortisol levels and reduced anabolic hormones like growth hormone, which are critical for recovery and tissue repair (83). Late-night or high-intensity workouts can disturb circadian rhythms, further disrupting the secretion of key hormones such as melatonin and insulin (84). Insufficient sleep exacerbates glucose metabolism issues, increasing the risk of insulin resistance and metabolic disorders (28). Prolonged sleep disruption also diminishes the body’s ability to regulate thyroid hormones, impacting energy balance and overall metabolic health (85). Regular moderate aerobic exercise, however, has been shown to improve sleep architecture and support endocrine stability, reducing the negative effects of sleep loss (86).
Conclusion
In conclusion, no single exercise universally supports the endocrine system; rather, a combination of aerobic, strength, and restorative activities works best to promote hormonal balance and overall health. Aerobic exercises enhance metabolism and insulin sensitivity, strength training boosts growth hormone and muscle health, while restorative practices like yoga reduce stress and regulate cortisol levels. By adopting a balanced exercise routine tailored to individual needs and ensuring proper rest, nutrition, and stress management, one can effectively support a healthy endocrine system and improve overall well-being.
References:
- Hackney, A.C., & Lane, A.R. (2015). Exercise and the regulation of endocrine hormones.
- Kraemer, W.J. (1988). Endocrine responses to resistance exercise.
- Janssen, J.A. (2016). Impact of physical exercise on endocrine aging.
- Warren, M.P., & Goodman, L.R. (2003). Exercise-induced endocrine pathologies.
- Athanasiou, N., et al. (2023). Endocrine responses of the stress system to different types of exercise.
- Arslan, Ş. (2020). Endocrine Responses in Exercise.
- Finsterer, J. (2024). Sleep Deprivation and Vitamin B12 Deficiency.
- Pattanayak, S. (2024). Psycho-Neuro-Immuno-Endocrinology Interactions.
- López-Ojeda, W., & Hurley, R. A. (2025). Myokines and the Brain.
- Maleki, Z., et al. (2025). Modifiable Risk Factors for Thyroid Conditions.
- Brenna, A., et al. (2024). Chronobiology and Cardiometabolic Health.
- Gautam, R., et al. (2025). The Role of Lifestyle Interventions in PCOS Management.
- Bonilla, D. A., et al. (2024). New Insights in Body Recomposition.
- Fernández-Elías, V. E., et al. (2024). Training and Nutrition for Performance.
- Shah, M. Z., et al. (2024). Endocrine and Cardio-Metabolic Benefits of Exercise.
- Borer, K.T. (2013). Advanced exercise endocrinology.
- Borer, K.T. (2003). Exercise endocrinology.
- Fleming, K.M., & Herring, M.P. (2018). The effects of Pilates on mental health outcomes: A meta-analysis of controlled trials.
- Mehravar, M.R. (2018). The effect of eight-week Pilates exercise on thyroid function in sedentary women.
- Najafi, P., et al. (2023). Effects of tele-pilates and tele-yoga on biochemicals, physical, and psychological parameters of females with multiple sclerosis.
- Ahmadi, H., & Mehravar, M.R. (2019). The effect of an eight-week Pilates exercise regimen on stress management and cortisol levels in sedentary women.
- Malvini, A. (2022). The influence of regular Pilates practice on visceral adipose tissue in postmenopausal women.
- Carlson, L.E., et al. (2004). Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress and levels of cortisol, dehydroepiandrosterone sulfate (DHEAS).
- Priya, G., & Kalra, S. (2018). Mind-body interactions and mindfulness meditation in diabetes.
- Patel, V., et al. (2020). Regular mindful yoga practice as a method to improve androgen levels in women with polycystic ovary syndrome.
- Ardito, R.B., et al. (2017). Mindfulness-based stress reduction program on chronic low-back pain: A study investigating the impact on endocrine, physical, and psychologic functioning.
- Chennaoui, M., et al. (2015). Sleep and exercise: a reciprocal issue.
- Dolezal, B.A., et al. (2017). Interrelationship between sleep and exercise: a systematic review.
- Ritsche, K., et al. (2014). Exercise-induced growth hormone during acute sleep deprivation.
- Stutz, J., et al. (2019). Effects of evening exercise on sleep in healthy participants: a systematic review and meta-analysis.
- Peyreigne, C., et al. (2001). Effect of hydration on exercise-induced growth hormone response.
- Seal, A.D., et al. (2019). Hydration and health.
- Perrier, E.T., et al. (2021). Hydration for health hypothesis: a narrative review of supporting evidence.
- Marcos, A., et al. (2014). Physical activity, hydration and health.
- Uchida, M.C., et al. (2009). Hormonal responses to different resistance exercise schemes of similar total volume.
- Howlett, T.A. (1987). Hormonal responses to exercise and training: a short review.
- Triviño-Paredes, J., et al. (2016). The effects of hormones and physical exercise on hippocampal structural plasticity.
- Kraemer, W.J., & Ratamess, N.A. (2005). Hormonal responses and adaptations to resistance exercise and training.
- Consitt, L.A., et al. (2002). Endogenous anabolic hormone responses to endurance versus resistance exercise and training in women.
- Stoddard, J.L., et al. (2007). Exercise training effects on premenstrual distress and ovarian steroid hormones.
- Monninkhof, E.M., et al. (2007). Design of the sex hormones and physical exercise (SHAPE) study.
- Isacco, L., et al. (2012). Influence of hormonal status on substrate utilization at rest and during exercise in the female population.
- Hyman, M. (2007). Systems biology, toxins, obesity, and functional medicine.
- Lee, Y.M., & Lee, D.H. (2019). Mitochondrial toxins and healthy lifestyle meet at the crossroad of hormesis.
- Trindade, F. (2020). Nutritional influences on hormonal health.
- Ji, L.L., et al. (2016). Exercise-induced hormesis and skeletal muscle health.
- Mason, R. (2002). Chemical Toxins and Obesity.
- Kraemer, W.J., & Ratamess, N.A. (2017). Recovery responses of testosterone, growth hormone, and IGF-1 after resistance exercise.
- Gu, P., et al. (2021). Effects of post-exercise recovery methods on exercise-induced hormones and blood fatigue factors: a systematic review and meta-analysis.
- Hausswirth, C., & Le Meur, Y. (2011). Physiological and nutritional aspects of post-exercise recovery: specific recommendations for female athletes.
- Lee, E.C., et al. (2017). Biomarkers in sports and exercise: tracking health, performance, and recovery in athletes.
- Huhmann, K. (2020). Menses requires energy: Disordered eating, excessive exercise, and high stress lead to menstrual irregularities.
- Brooks, K.A., & Carter, J.G. (2013). Overtraining, exercise, and adrenal insufficiency.
- Mastorakos, G., & Pavlatou, M. (2005). Exercise and the stress system.
- Cadegiani, F.A., & Kater, C.E. (2017). Hormonal aspects of overtraining syndrome: a systematic review.
- Delimaris, I. (2014). Potential adverse biological effects of excessive exercise and overtraining among healthy individuals.
- Anderson, T., & Wideman, L. (2021). Effects of overtraining status on the cortisol awakening response.
- Urhausen, A., Gabriel, H., & Kindermann, W. (1995). Blood hormones as markers of training stress and overtraining.
- De Souza, M.J., et al. (2008). The presence of both an energy deficiency and estrogen deficiency exacerbate alterations of bone metabolism in exercising women.
- Allaway, H.C.M., & Southmayd, E.A. (2016). The physiology of functional hypothalamic amenorrhea associated with energy deficiency.
- Hagobian, T.A., & Sharoff, C.G. (2009). Effects of exercise on energy-regulating hormones and appetite in men and women.
- Southmayd, E.A., & Williams, N.I. (2019). Energy deficiency suppresses bone turnover in exercising women with menstrual disturbances.
- Elliott-Sale, K.J., & Tenforde, A.S. (2018). Endocrine effects of relative energy deficiency in sport.
- Warren, M.P., & Perlroth, N.E. (2001). Hormones and sport-the effects of intense exercise on the female reproductive system.
- De Souza, M.J., et al. (2010). High prevalence of subtle and severe menstrual disturbances in exercising women.
- Arena, B., et al. (1995). Reproductive hormones and menstrual changes with exercise in female athletes.
- Eliakim, A., & Beyth, Y. (2003). Exercise training, menstrual irregularities, and bone development in children and adolescents.
- Bornstein, S.R., et al. (2016). Diagnosis and treatment of primary adrenal insufficiency: an endocrine society clinical practice guideline.
- Charmandari, E., et al. (2014). Adrenal insufficiency.
- Green-Golan, L., et al. (2007). Decreased epinephrine reserve and glycemic control during exercise.
- Simunkova, K., et al. (2016). Effect of a pre-exercise hydrocortisone dose on short-term physical performance.
- Ciloglu, F., et al. (2005). Exercise intensity and its effects on thyroid hormones.
- Ahn, N., et al. (2019). Exercise training-induced changes in thyroid function in women with subclinical hypothyroidism.
- Boelaert, K., & Franklyn, J.A. (2005). Thyroid hormone in health and disease.
- De Groot, L., et al. (2012). Management of thyroid dysfunction during pregnancy and postpartum.
- Greenspan, S.L., & Greenspan, F.S. (1999). The effect of thyroid hormone on skeletal integrity.
- Krivoschekov, S.G., & Lushnikov, O.N. (2011). Psychophysiology of sports addictions (exercise addiction).
- Çınaroğlu, M. (2024). Hormonal catalysts in the addiction cycle of muscle dysmorphia: A neuroendocrine perspective.
- Hamer, M., & Karageorghis, C.I. (2007). Psychobiological mechanisms of exercise dependence.
- Lombardi, G. (2019). Exercise-dependent modulation of bone metabolism and bone endocrine function.
- Kohrt, W.M., et al. (2004). Physical activity and bone health.
- Santos, L., et al. (2017). Exercise and bone health across the lifespan.
- Morrison, M., et al. (2022). Sleep, circadian biology and skeletal muscle interactions.
- Chennaoui, M., et al. (2015). Sleep and exercise: a reciprocal issue.
- Briançon-Marjollet, A., et al. (2015). The impact of sleep disorders on glucose metabolism.
- Bedrosian, T.A., & Fonken, L.K. (2016). Endocrine effects of circadian disruption.

