- Sleep disorders are conditions that disrupt normal sleep patterns, affecting health and daily functioning.
- Maintaining a regular sleep schedule and bedtime routine helps regulate the body’s internal clock, reducing the risk of sleep disruptions.
- Avoiding stimulants, managing stress, and creating a comfortable sleep environment promote better rest and help prevent sleep-related issues.
 Sleep disorders refer to conditions that disrupt regular sleep patterns, affecting overall health and quality of life 1. Healthy sleep hygiene practices are essential for preventing the onset of sleep disorders, which are increasingly prevalent in modern society. Research shows that poor sleep hygiene—such as inconsistent sleep schedules, exposure to blue light before bed, and unhealthy bedtime habits—can lead to insomnia, sleep apnea, and other sleep disturbances 2. Adopting consistent sleep schedules, creating a conducive sleep environment, and avoiding stimulants like caffeine before bedtime are some evidence-based strategies that help improve sleep quality and mitigate risks 3. Additionally, regular physical activity and mindfulness practices, such as meditation, have shown significant benefits in enhancing sleep efficiency source. Awareness and education on sleep hygiene play a crucial role, as studies highlight a lack of sufficient emphasis on these practices in healthcare settings 4. With lifestyle modifications and targeted interventions, individuals can address sleep issues early and prevent chronic conditions linked to poor sleep hygiene 5.
Sleep disorders refer to conditions that disrupt regular sleep patterns, affecting overall health and quality of life 1. Healthy sleep hygiene practices are essential for preventing the onset of sleep disorders, which are increasingly prevalent in modern society. Research shows that poor sleep hygiene—such as inconsistent sleep schedules, exposure to blue light before bed, and unhealthy bedtime habits—can lead to insomnia, sleep apnea, and other sleep disturbances 2. Adopting consistent sleep schedules, creating a conducive sleep environment, and avoiding stimulants like caffeine before bedtime are some evidence-based strategies that help improve sleep quality and mitigate risks 3. Additionally, regular physical activity and mindfulness practices, such as meditation, have shown significant benefits in enhancing sleep efficiency source. Awareness and education on sleep hygiene play a crucial role, as studies highlight a lack of sufficient emphasis on these practices in healthcare settings 4. With lifestyle modifications and targeted interventions, individuals can address sleep issues early and prevent chronic conditions linked to poor sleep hygiene 5.
Understanding Sleep Hygiene
Sleep hygiene refers to a collection of practices and habits that contribute to optimal nighttime sleep quality and full daytime alertness. These practices include maintaining a consistent sleep schedule, creating a conducive sleep environment, and avoiding stimulants before bedtime 6. Sleep hygiene is essential for regulating circadian rhythms and ensuring restorative sleep, which supports overall health and well-being 7.
Good sleep hygiene plays a pivotal role in maintaining healthy sleep patterns. Practices such as adhering to a regular sleep schedule and avoiding exposure to blue light before bedtime are scientifically proven to enhance sleep quality 8. Sleep hygiene also helps mitigate stress, improve cognitive function, and reduce the risk of chronic illnesses such as cardiovascular diseases 9. Moreover, these practices are particularly effective in preventing sleep disturbances during transitions, such as shift work or stressful life events 10.
Neglecting sleep hygiene is often associated with the development of sleep disorders such as insomnia, sleep apnea, and restless legs syndrome. Inconsistent sleep patterns, prolonged screen time, and consumption of caffeine late in the day are significant contributors to these conditions 11. Chronic poor sleep hygiene exacerbates mental health issues and increases the risk of metabolic disorders 12. Addressing poor sleep hygiene through targeted interventions can significantly reduce the prevalence of these disorders.
What practices in sleep hygiene help prevent sleep disorders?
“Discover simple sleep hygiene practices to improve your rest and prevent sleep disorders. Small changes can lead to better, healthier sleep!”
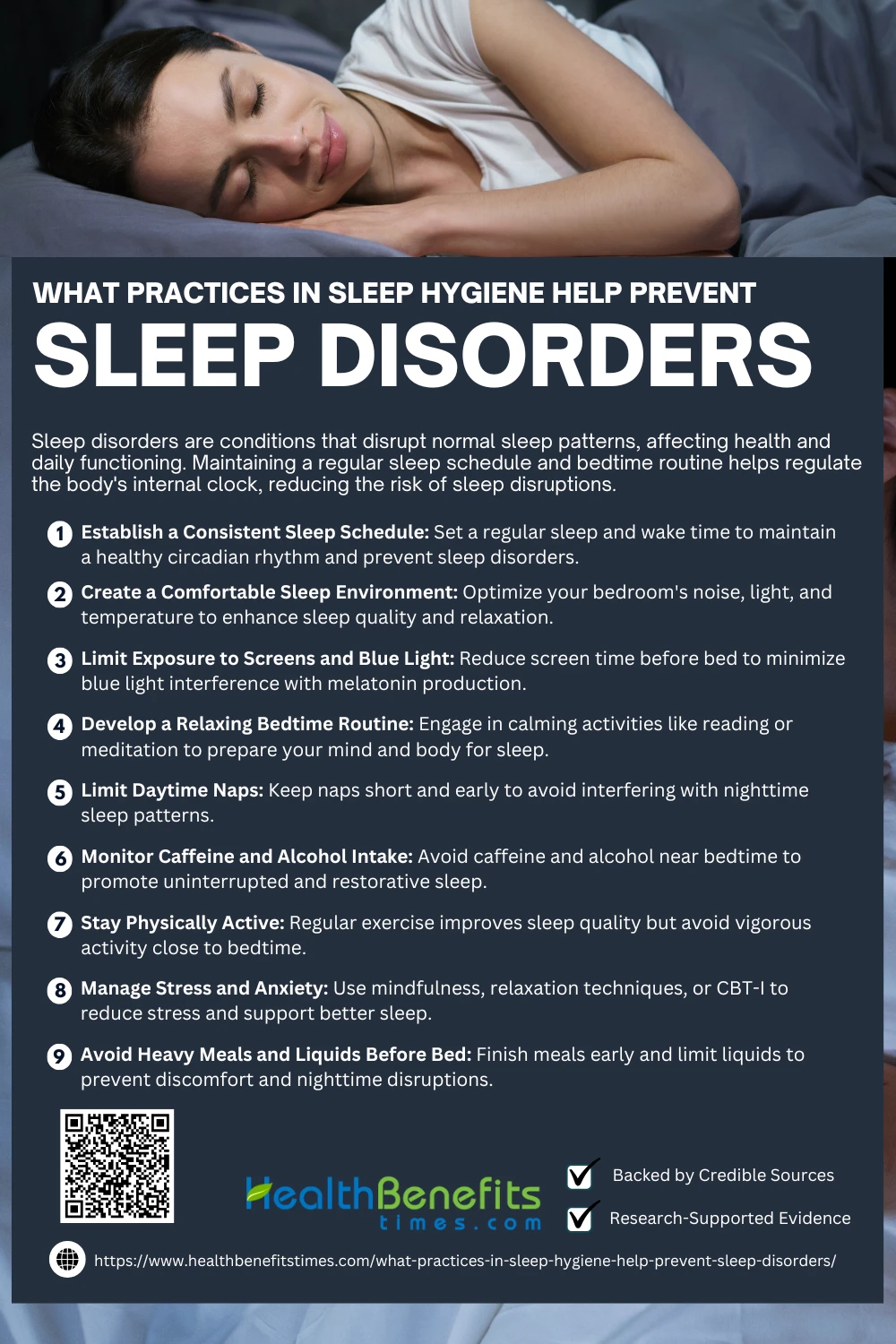 1. Establish a Consistent Sleep Schedule
1. Establish a Consistent Sleep Schedule
Maintaining a consistent sleep schedule is essential for regulating the body’s internal clock, improving sleep quality, and preventing disorders like insomnia. Research highlights the importance of sleeping and waking at the same time daily to reinforce circadian rhythms 13. Deviations can lead to disrupted sleep patterns, impacting mental and physical health 14. Studies have shown that consistent schedules enhance daytime alertness and reduce fatigue 15. This practice fosters long-term sleep stability 16 and prevents sleep-related health issues 17.
2. Create a Comfortable Sleep Environment
Creating a comfortable sleep environment is crucial for preventing sleep disorders. Reducing noise and ensuring a dark, cool room enhances sleep quality, as shown in studies emphasizing the impact of 18 on sleep. Similarly, comfortable bedding reduces physical discomfort and enhances restorative sleep (19). Consistency in maintaining a clutter-free, serene environment fosters relaxation (20). Moreover, avoiding blue-light exposure before bedtime creates optimal conditions for rest (21).
3. Limit Exposure to Screens and Blue Light
Reducing screen time before bedtime significantly enhances sleep quality, as blue light disrupts melatonin production, delaying sleep onset (22). Using blue light filters or wearing blue-light-blocking glasses mitigates these effects (23). Studies highlight that avoiding screens two hours before sleep improves overall restfulness (24). Adolescents benefit most from screen management strategies (25). Furthermore, dimming device brightness reduces circadian disruption (26).
4. Develop a Relaxing Bedtime Routine
Establishing a relaxing bedtime routine, such as reading or meditating, can significantly enhance sleep quality by preparing the mind and body for rest (27). Engaging in calming activities like light stretches or breathing exercises reduces anxiety (28). Consistency is key, as maintaining a regular sleep schedule fosters better sleep patterns (29). Warm baths or dim lighting also aid relaxation (30). Avoiding stimulating activities before bed prevents sleep disruptions (31).
5. Monitor Caffeine and Alcohol Intake
Limiting caffeine and alcohol intake is vital for better sleep hygiene, as caffeine disrupts sleep by blocking adenosine, a sleep-promoting chemical, and alcohol interferes with sleep cycles (32). Avoiding these substances close to bedtime improves sleep latency and quality (14). Studies recommend consuming caffeine only in the morning (33). Moderating alcohol ensures uninterrupted REM sleep (34). Monitoring intake promotes consistent sleep patterns (35).
6. Stay Physically Active
Engaging in regular physical activity supports healthy sleep by reducing sleep latency and improving sleep quality. Moderate aerobic exercises enhance slow-wave sleep, the most restorative phase (36). Physical activity also helps alleviate symptoms of insomnia and anxiety, which commonly disrupt sleep (37). Experts recommend avoiding vigorous exercise close to bedtime to prevent overstimulation (38).
7. Manage Stress and Anxiety
Managing stress and anxiety is crucial for maintaining healthy sleep hygiene. Techniques like mindfulness meditation reduce cortisol levels, improving sleep quality (39). Cognitive Behavioral Therapy for Insomnia (CBT-I) addresses anxiety-related sleep issues effectively (40). Journaling before bed helps clear the mind, reducing intrusive thoughts. Progressive muscle relaxation alleviates physical tension, aiding sleep (41). Deep breathing exercises calm the nervous system, facilitating relaxation (42).
8. Avoid Heavy Meals and Liquids before Bed
Avoiding heavy meals and liquids before bedtime is essential for sleep hygiene. Heavy meals disrupt digestion, causing discomfort and reducing sleep quality (43). Limiting liquids prevents nocturnal awakenings for bathroom trips (44). Late-night eating can disturb circadian rhythms, worsening sleep disorders (45). Experts suggest finishing meals at least two hours before sleep to improve restfulness (46). Balanced evening meals promote digestive ease and better sleep onset (47).
9. Limit daytime Naps
Limiting daytime naps promotes healthier sleep patterns by preventing disruptions to the circadian rhythm (28). Short naps of 20–30 minutes earlier in the day are less likely to interfere with nighttime sleep (48). Long or late-afternoon naps can delay sleep onset, worsening insomnia (32). Proper nap management enhances alertness while minimizing sleep debt (47). Consistently avoiding naps altogether may improve overall sleep quality (46).
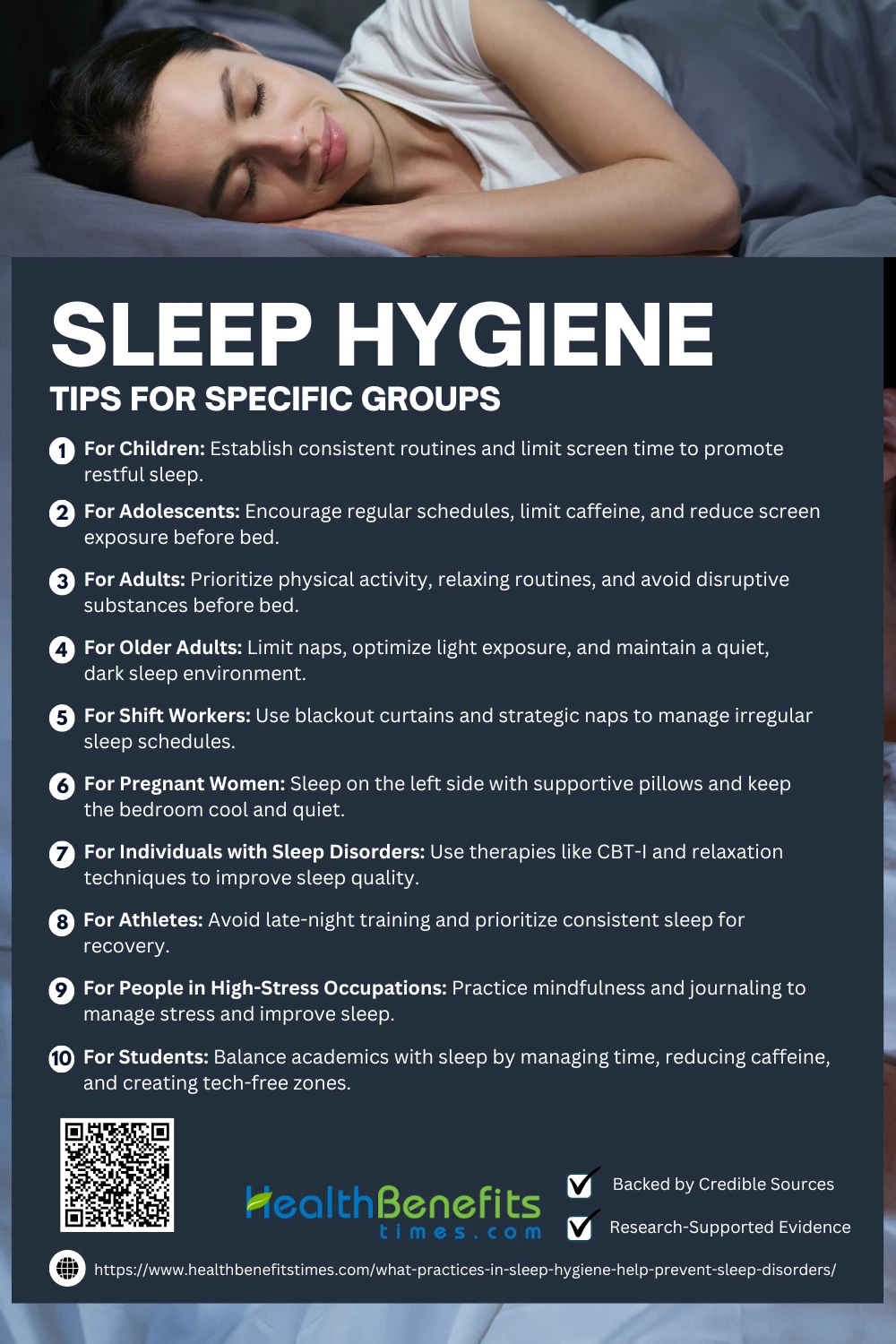
Sleep Hygiene Tips for Specific Groups
Sleep hygiene practices can vary based on individual needs, lifestyles, and challenges. Certain groups, such as students, shift workers, parents, and older adults, may face unique obstacles when it comes to maintaining healthy sleep routines. Tailoring sleep hygiene tips to these specific groups can help address their distinct needs and improve overall sleep quality. Here, we explore practical strategies to support better rest for everyone, no matter their circumstances.
- For Children
Children thrive on routine. Establish a consistent bedtime and wake-up time, even on weekends. Activities like reading or a warm bath can signal bedtime. Avoid screen time, as exposure to blue light from devices can disrupt melatonin production, making it harder for children to fall asleep. - For Adolescents
Adolescents often struggle with delayed sleep patterns. Encourage them to maintain regular sleep schedules to align with their internal clock. Limit caffeine intake, especially in the evening, as it can delay sleep onset. Educate teens about the importance of avoiding screens before bed to ensure restful sleep. - For Adults
Adults should prioritize daily physical activity to promote deeper sleep and improve mood. Create a relaxing pre-sleep routine, such as meditation or light stretching. Avoid alcohol and heavy meals before bedtime, as they can disrupt sleep quality. - For Older Adults
Older adults often experience changes in sleep cycles. Limiting daytime naps to 20–30 minutes in the early afternoon can help maintain nighttime sleep. Exposure to natural light during the day and keeping the sleeping environment dark and quiet at night can support circadian rhythm regulation. - For Shift Workers
Shift workers face unique challenges due to irregular schedules. Using blackout curtains, eye masks, and noise-canceling tools can help create a night-like sleeping environment during the day. Strategically timed naps and light exposure can help regulate their circadian rhythm. - For Pregnant Women
Pregnancy can cause discomfort during sleep. Sleeping on the left side improves blood flow to the baby and mother. Use supportive pillows between the knees and under the abdomen for comfort. Keep the bedroom cool and quiet to minimize interruptions. - For Individuals with Sleep Disorders
Individuals with chronic sleep disorders benefit from behavioral therapies like Cognitive Behavioral Therapy for Insomnia (CBT-I). Progressive muscle relaxation and mindfulness meditation can reduce stress and anxiety, promoting better sleep. - For Athletes
Athletes need restorative sleep for recovery. Avoid late-night training sessions, as they can elevate heart rate and delay sleep. Include post-exercise relaxation techniques and maintain a consistent sleep schedule to support physical performance. - For People in High-Stress Occupations
High-stress jobs often lead to poor sleep due to racing thoughts or anxiety. Mindfulness meditation, deep breathing exercises, and journaling before bed can help calm the mind. Creating a bedtime routine can signal the brain to prepare for rest. - For Students
Students often sacrifice sleep for academics. Time management is key to avoid late-night cramming. Create a technology-free zone in the bedroom and limit caffeine to earlier in the day. A regular bedtime can help establish healthy habits that enhance focus and memory.
Warning Signs of Sleep Disorders
Recognizing warning signs of sleep disorders is crucial for maintaining health. Learn common symptoms, such as insomnia, snoring, or fatigue, and seek help for better sleep.
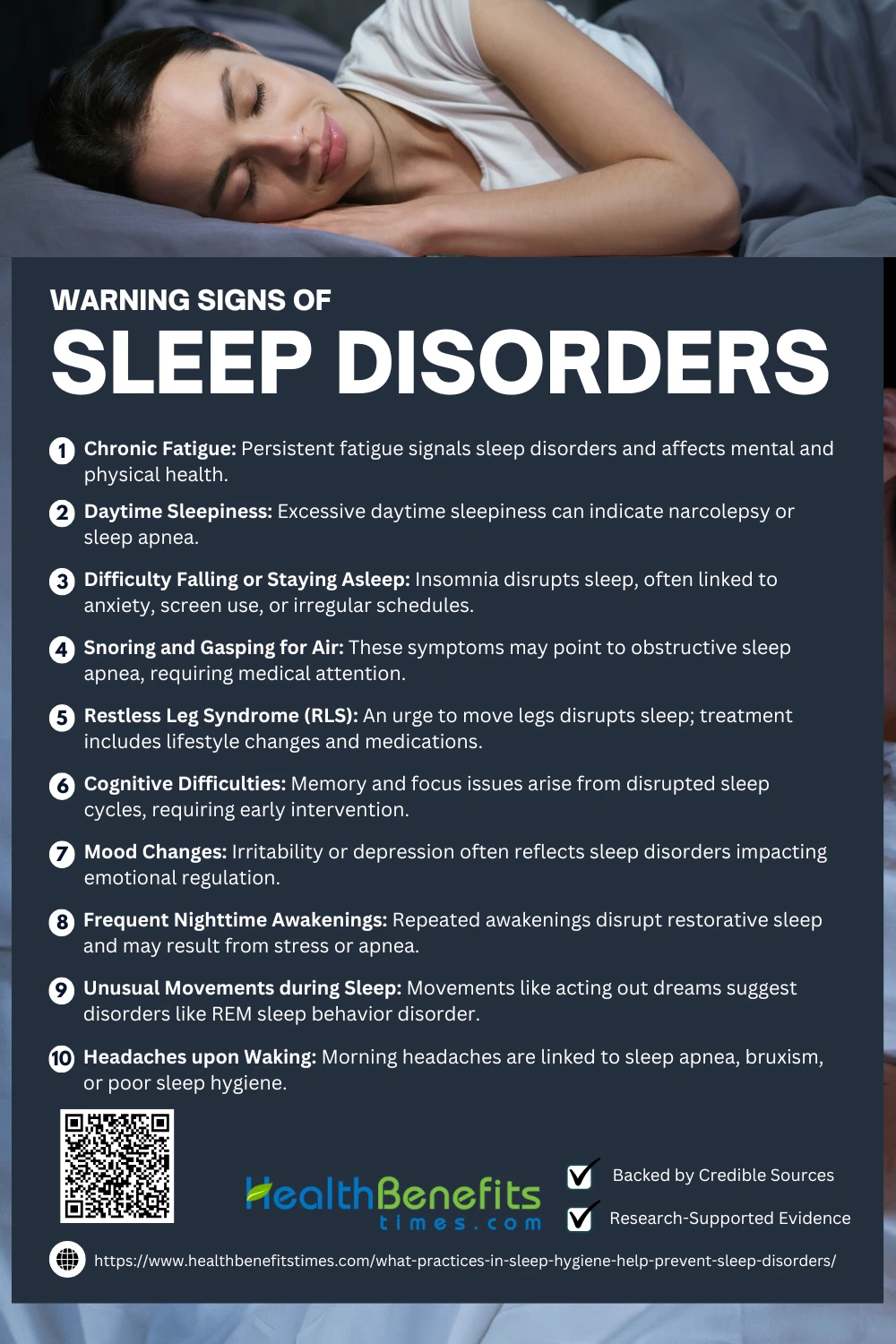 1. Chronic Fatigue
1. Chronic Fatigue
Chronic fatigue, a persistent symptom of sleep disorders, often stems from disrupted circadian rhythms or poor sleep quality (49). It can exacerbate mood disorders, including depression and anxiety (50). Conditions like fibromyalgia frequently associate chronic fatigue with sleep disturbances (51). Early diagnosis and treatment of underlying sleep issues can mitigate fatigue and improve overall health (52).
2. Daytime Sleepiness
Excessive daytime sleepiness (EDS) is a key symptom of sleep disorders like narcolepsy or sleep apnea, characterized by an inability to stay alert during waking hours (53). EDS often impairs cognitive functions and increases accident risks (54). Regular monitoring of sleep patterns helps identify underlying issues (55). Early interventions such as therapy or CPAP devices can alleviate EDS and improve sleep quality (56).
3. Difficulty Falling or Staying Asleep
Difficulty falling or staying asleep, a hallmark of insomnia, disrupts sleep quality and contributes to fatigue and poor mental health (57). This condition often correlates with underlying issues such as anxiety or physiological disorders (58). Screen use and irregular sleep schedules exacerbate these challenges (59). Cognitive Behavioral Therapy (CBT-I) effectively addresses insomnia-related symptoms (60).
4. Snoring and Gasping for Air
Snoring and gasping for air during sleep are key signs of obstructive sleep apnea (OSA), a serious disorder affecting airway patency (61). These symptoms lead to fragmented sleep and reduced oxygen levels, increasing cardiovascular risks. Early detection through polysomnography is crucial for management.
5. Restless Leg Syndrome (RLS)
Restless Leg Syndrome (RLS) is characterized by an irresistible urge to move the legs, often disrupting sleep and causing significant discomfort (62). Nutritional deficiencies, such as low iron levels, may exacerbate symptoms (63). Early diagnosis and tailored treatments, like dopamine agonists, can alleviate RLS (64). Non-pharmacological approaches, including exercise and lifestyle changes, also prove effective (65).
6. Mood Changes
Mood changes, such as irritability, anxiety, and depression, often indicate sleep disorders like insomnia or sleep apnea (66). Sleep disruptions interfere with emotional regulation and brain function, exacerbating mood instability (67). Bipolar disorder patients frequently experience mood shifts triggered by poor sleep patterns (68). Early intervention, including cognitive-behavioral therapy, can improve sleep and stabilize mood (69).
7. Frequent Nighttime Awakenings
Frequent nighttime awakenings are a common symptom of sleep disorders like insomnia or sleep apnea, disrupting restorative sleep cycles (70). These awakenings often result from physiological issues such as obstructive breathing or stress-induced arousals (71). Addressing the underlying causes, such as stress management or medical conditions, can improve sleep continuity (72). Effective treatments include cognitive behavioral therapy and melatonin supplements (73).
8. Unusual Movements during Sleep
Unusual movements during sleep, such as acting out dreams, can indicate disorders like REM sleep behavior disorder (RBD) or periodic limb movement disorder (PLMD) (74). These conditions often correlate with neurological diseases like Parkinson’s (75). Early diagnosis is critical for managing symptoms effectively (76). Sleep studies help identify movement patterns and provide targeted treatments (77).
9. Headaches upon Waking
Morning headaches can signal sleep disorders like obstructive sleep apnea or bruxism, caused by interrupted breathing or teeth grinding (67). Poor sleep hygiene and insomnia are common culprits (57). Studies show treating underlying conditions, such as sleep apnea with CPAP, significantly reduces headaches (78). Melatonin therapy can also help by regulating sleep cycles (73).
10. Cognitive Difficulties
Cognitive difficulties, such as memory lapses or reduced attention span, are warning signs of sleep disorders like sleep apnea and insomnia (80). These symptoms often result from disrupted restorative sleep cycles (81). Research links oxidative stress in sleep disorders to cognitive decline (82). Early intervention and therapies, such as cognitive-behavioral approaches, can mitigate these effects (83).
Modifying Sleep Hygiene to Individual Needs
Modifying sleep hygiene to meet individual needs is crucial for optimizing rest and addressing diverse sleep challenges. Personalized approaches, such as aligning routines with lifestyle and cultural contexts, improve sleep outcomes (84). Stress management strategies and cognitive-behavioral therapy help individuals address barriers to quality sleep (85). Tailoring light exposure and temperature adjustments can also aid specific groups (86). Furthermore, addressing unique adolescent sleep challenges supports long-term health (87). Integration of mindfulness practices complements these efforts (79).
When to Seek Professional Help
- Persistent Insomnia: Difficulty falling or staying asleep for weeks may require professional intervention to address underlying causes like anxiety or hormonal imbalances.
- Excessive Daytime Sleepiness: Feeling excessively sleepy during the day, even after a full night’s rest, could signal conditions like narcolepsy or sleep apnea.
- Loud Snoring or Gasping: If snoring is accompanied by gasping for air or pauses in breathing, a sleep specialist should evaluate for obstructive sleep apnea.
- Frequent Nighttime Awakenings: Regularly waking up multiple times at night without apparent reason may require assessment for sleep disorders like restless leg syndrome.
- Unexplained Mood Changes: Chronic irritability, anxiety, or depression linked to sleep disruptions is a strong reason to consult a professional.
- Morning Headaches: Waking up with headaches could indicate sleep apnea or bruxism, conditions that need medical evaluation.
- Leg Discomfort at Night: Persistent leg discomfort or urges to move during sleep may suggest Restless Leg Syndrome, which a specialist can diagnose and treat.
- Sleepwalking or Acting Out Dreams: Unusual behaviors during sleep, such as sleepwalking or violent movements, could point to REM sleep behavior disorder.
- Cognitive Difficulties: Memory issues or reduced concentration due to poor sleep may require a sleep study to identify treatable disorders.
- Sleep Paralysis: Experiencing frequent episodes of sleep paralysis can be associated with narcolepsy and should prompt professional evaluation.
Common Myths about Sleep Hygiene
- Myth: Everyone Needs Eight Hours of Sleep
While eight hours is often cited as the standard, sleep requirements vary widely depending on individual factors such as age, activity level, and genetics. Young adults may need more sleep than older adults, and highly active individuals may require additional rest to recover. Studies show some individuals can function well on seven hours, while others may need nine or more. - Myth: Drinking Alcohol Helps You Sleep Better
Alcohol may initially help you fall asleep due to its sedative effects, but it disrupts the natural sleep cycle. It reduces the amount of restorative REM sleep and often causes frequent awakenings, leaving you feeling tired the next day. Regular alcohol use before bed is linked to poor overall sleep quality. - Myth: Watching TV Before Bed Is Relaxing
Many believe watching TV or scrolling on phones helps them unwind, but the blue light emitted from screens suppresses melatonin production, a hormone critical for sleep. This delay in sleep onset can lead to reduced sleep quality and duration. Experts recommend avoiding screens at least an hour before bed. - Myth: You Can “Catch Up” on Sleep During Weekends
Sleep debt accumulated during the week cannot be fully recovered by sleeping longer on weekends. This practice can also disrupt your circadian rhythm, making it harder to establish a consistent sleep schedule. Regular sleep patterns are more effective for maintaining good sleep health. - Myth: Snoring is Harmless
While occasional snoring may not be problematic, chronic snoring can indicate underlying conditions like obstructive sleep apnea. This disorder leads to pauses in breathing during sleep, increasing the risk of cardiovascular issues and daytime fatigue. Persistent snoring should prompt medical evaluation. - Myth: A Hot Room Is Conducive to Sleep
A cooler sleeping environment is more conducive to quality rest. The body’s core temperature naturally drops during sleep, and a cool room supports this process. Ideal temperatures for sleep range between 60–67°F (15–19°C). Overly warm environments can lead to discomfort and restless sleep. - Myth: Exercising at Night Hampers Sleep
While vigorous activity right before bed can delay sleep onset, moderate exercise in the evening can improve sleep quality and duration. Physical activity helps regulate circadian rhythms and promotes deep sleep. Timing and intensity matter, so individuals should find what works best for them. - Myth: Older Adults Need Less Sleep
It is a common misconception that aging reduces the need for sleep. Older adults typically require the same 7–9 hours of sleep as younger adults. However, sleep patterns may shift, with lighter and more fragmented sleep being common, often requiring adjustments to sleep hygiene. - Myth: Sleeping Pills Are Always Safe
While sleeping pills can be effective for short-term use, prolonged reliance can lead to dependency and mask underlying sleep disorders. Side effects such as daytime drowsiness and cognitive impairment are also concerns. Behavioral therapies and lifestyle changes are preferred for addressing chronic sleep issues. - Myth: Napping Always Reduces Fatigue
Napping can be beneficial, but its effectiveness depends on duration and timing. Short naps of 20–30 minutes in the early afternoon can boost alertness. Long or late naps, however, may interfere with nighttime sleep, worsening fatigue and disrupting sleep cycles.
Conclusion
Adopting consistent sleep hygiene practices is key to preventing sleep disorders. Prioritizing a regular sleep schedule, creating a comfortable sleep environment, limiting screen time before bed, and managing stress can significantly enhance sleep quality. Healthy habits like avoiding caffeine and heavy meals close to bedtime, staying physically active, and practicing relaxation techniques further support restorative sleep. By integrating these practices into daily routines, individuals can reduce the risk of sleep disorders and promote long-term physical and mental well-being.
References:
- Kawabe, K., et al. (2024). Sleep Awareness of Japanese Outpatients. MDPI.
- Tangwijitsakul, H., et al. (2024). Sleep problems and executive dysfunctions in pre‐school children. Wiley Online Library. Retrieved from
- Herrera, G.F., et al. (2024). Fibromyalgia Diagnosis and Treatment Receipt. Military Medicine.
- Dietz, M. (2024). Ongoing Education of Sleep Hygiene Among Adolescents. ProQuest.
- Ferini-Strambi, L., et al. (2024). Psychological sleep studies: new insights. Frontiers in Psychology.
- Yavuz Akçay, Y., et al. (2024). General Hygiene Training Impact. Kent University Repository.
- Saha, S., et al. (2024). Evaluate First-Year Nursing Students’ Understanding of Sleep Hygiene. Saudi Journals.
- Hernández, T. L. (2024). Neurocognitive Foundations of Sleep Hygiene. Scientific Medical Data.
- Khan, I., et al. (2024). Determinants of Sleep Quality among Nursing Students. Social Science Review.
- Fogacci, F., et al. (2025). The Prognostic Value of Sleep Hygiene in Cardiovascular Health. Metabolism Journal.
- Sambhu, P. (2024). Multifaceted Exploration of Sleep Hygiene Determinants. JSTAGE.
- Carvalho, G. S., et al. (2024). Health Promotion Through Sleep Hygiene Practices. Frontiers in Public Health.
- Weiss, M.D., et al. (2008). Sleep hygiene for children with neurodevelopmental disabilities. Pediatrics.
- Stepanski, E.J., & Wyatt, J.K. (2003). Use of sleep hygiene in the treatment of insomnia. Sleep Medicine Reviews.
- Brown, F.C., et al. (2002). Relationship of sleep hygiene awareness and sleep quality. Behavioral Medicine.
- Drake, C.L., et al. (2005). Sleep hygiene practices in a population-based sample of insomniacs. Sleep.
- Riedel, B.W. (2000). Sleep hygiene. Treatment of Late-Life Insomnia.
- Ishiki, A., Kurosawa, E., Narai, D., et al. (2024). Best medical practices for older adults after a disaster: A narrative review. Frontiers in Medicine.
- National Sleep Foundation. (n.d.). Sleep hygiene tips for better rest. National Sleep Foundation.
- Sleep Health Journal. (n.d.). Optimizing bedroom environment for sleep quality. Sleep Health Journal.
- PubMed Central. (n.d.). Blue-light exposure and sleep disturbances. PubMed Central.
- Hale, L., Kirschen, G. W., et al. (2018). Youth screen media habits and sleep. ScienceDirect.
- Bigalke, J. A., Greenlund, I. M., et al. (2021). Blue-light blocking glasses in sleep hygiene. Sleep Health.
- Perrault, A. A., Ghisletta, P., et al. (2019). Impact of reducing evening screen use. PubMed.
- Silvani, M. I., Werder, R., et al. (2022). Effects of blue light on sleep. Frontiers in Physiology.
- Janků, K., Šmotek, M., et al. (2020). Evening screen exposure and sleep. Taylor & Francis.
- Tomopoulos, S., Bathory, E. (2017). Sleep regulation and hygiene in children. ScienceDirect.
- Irish, L. A., Kline, C. E., et al. (2015). Role of sleep hygiene in public health. NCBI.
- Mindell, J. A., Williamson, A. A. (2018). Bedtime routine and sleep. PubMed.
- Riedel, B. W. (2000). Sleep hygiene practices. SAGE.
- Halal, C. S. E., Nunes, M. L. (2014). Education in sleep hygiene. SciELO.
- Kloss, J. D., Nash, C. O., et al. (2016). Effects of caffeine and alcohol on sleep. Taylor & Francis.
- Winegar, R. (2024). Enhancing sleep quality with caffeine moderation. LWW Journals.
- Zhou, E. S., et al. (2020). Sleep health behaviors. NIH.
- Shriane, A. E., et al. (2020). Monitoring sleep hygiene in shift workers. Elsevier.
- National Institutes of Health. (2019). Physical activity and sleep quality. NIH.
- Stepanski, E., & Wyatt, J. (2019). Role of exercise in sleep hygiene. Elsevier.
- Kline, C. (2020). Exercise and circadian rhythms. PubMed.
- Adadzi, J., & Kerna, N. A. (2024). Role of mindfulness in reducing anxiety. Authorea.
- Perlis, M. L., et al. (2020). Effectiveness of CBT-I on anxiety and sleep. NIH.
- Espie, C. A., et al. (2017). Progressive muscle relaxation for insomnia. Elsevier.
- Brown, R. P., & Gerbarg, P. L. (2019). Deep breathing techniques for stress reduction. PubMed.
- Halson, S. L. (2008). Nutrition and its impact on sleep hygiene. Taylor & Francis.
- Bloom, H. G., et al. (2009). Hydration and sleep patterns. NCBI.
- Posner, D., & Gehrman, P. R. (2011). Behavioral insights on late-night eating. Elsevier.
- Yang, C. M., et al. (2010). Timing meals to optimize sleep. SAGE Journals.
- Nédélec, M., et al. (2015). Dietary habits for sleep hygiene. Springer.
- Stepanski, E., & Wyatt, J. K. (2014). The role of naps in sleep disorders. Elsevier.
- Fang, R., et al. (2024). Chronic fatigue and sleep problems. Research Square.
- Papapetropoulos, S., et al. (2024). Sleep disturbance and depression. NEJM Evidence.
- Ventriglia, G., et al. (2024). Sleep and chronic fatigue in fibromyalgia. Taylor & Francis.
- Galli, S., et al. (2024). Managing fatigue via sleep intervention. Springer.
- Fathi, M., et al. (2024). Excessive daytime sleepiness: A review. SBMU Journal.
- Wang, X., et al. (2024). Narcolepsy and daytime sleepiness. Wiley Online Library.
- McCullough, L., & Attarian, H. (2025). Health risks of sleep apnea. Journal of Clinical Sleep Medicine.
- Gökgöz, M., et al. (2025). Management of EDS in pediatric populations. Springer.
- Singhal, H. (2024). Insomnia and its impact. TJHMS.
- López García, R., et al. (2024). Prevalence of insomnia symptoms. MDPI.
- Reta, Y., et al. (2024). Predictors of insomnia. Frontiers in Psychiatry.
- Akca, A., et al. (2024). Coping strategies for insomnia. Wiley Online Library.
- Strenth, C., et al. (2024). Obstructive sleep apnea and cardiac risks. AHA Journals.
- Singh, H., et al. (2024). Efficacy of treatments for RLS. ScienceDirect.
- Martín-Núñez, J., et al. (2024). Nutritional influences on RLS. MDPI.
- Ferini-Strambi, L., et al. (2024). Tailored therapies for RLS. Springer.
- Falup-Pecurariu, C., et al. (2024). Managing RLS with non-pharmacological methods. Taylor & Francis.
- Jaworska, I., et al. (2024). Psychological impacts of sleep disturbances. Academia.
- Giannotta, G., et al. (2024). Chronobiology and mood disorders. MDPI.
- Ulrichsen, A., et al. (2024). Bipolar disorder and sleep patterns. ScienceDirect.
- Simas, K. R., et al. (2024). Therapy for sleep-induced mood changes. ResearchGate.
- Qu, L., et al. (2024). Sleep disturbances and their impact on health. PMC.
- Shah, J., et al. (2025). Causes of nighttime awakenings. Wiley Online Library
- Liliana, L. (2024). Impact of health conditions on sleep. MedEspera.
- Temirova, O. A. (2024). Role of melatonin in sleep improvement. MSU Journal.
- Boeve, B. F., & Ferman, T. J. (2024). REM sleep behavior disorder and its implications. Lancet Neurology.
- Taha, H. B. (2024). Parkinson’s and sleep disorders. Medical Literacy Initiative.
- Williams, G. K., et al. (2024). Neurological basis of sleep movement disorders. ACS Publications.
- Yunisova, G., et al. (2024). Diagnosing movement disorders through sleep studies. ScienceDirect.
- Drake, C., et al. (2024). Treatment effects on sleep disorders. Henry Ford Sleep Medicine.
- Bhattacharyya, D. (2024). Mindfulness in sleep hygiene. BMJ Paediatrics Open.
- Yusuff, A. S. (2025). Mechanisms of cognitive impairment in sleep disorders. Cureus.
- Bosak, M., & Kepińska-Wnuk, A. (2024). Neurological impacts of sleep disorders. Viamedica.
- Jing, Z., et al. (2024). Oxidative stress and cognitive dysfunction. JCMP.
- Calligaro, H., et al. (2024). Cognitive therapy approaches in sleep-related issues. Oxford Academic.
- Cai, D., Villanueva, P., et al. (2024). Postpartum practices and sleep. ScienceDirect.
- Bacia, J. (2023). Holistic strategies for sleep hygiene. ResearchGate.
- Noda, Y., Koga, Y., et al. (2024). Tailored sleep environments. Elsevier.
- Dietz, M. (2024). Sleep hygiene in adolescents. ProQuest.