- A kidney transplant is a surgical procedure that replaces a failing kidney with a healthy donor kidney to restore function.
- It is a preferred treatment for end-stage kidney disease, offering better quality of life compared to dialysis.
- Eligibility, risks, recovery, and lifelong medication are essential factors to consider before undergoing a kidney transplant.
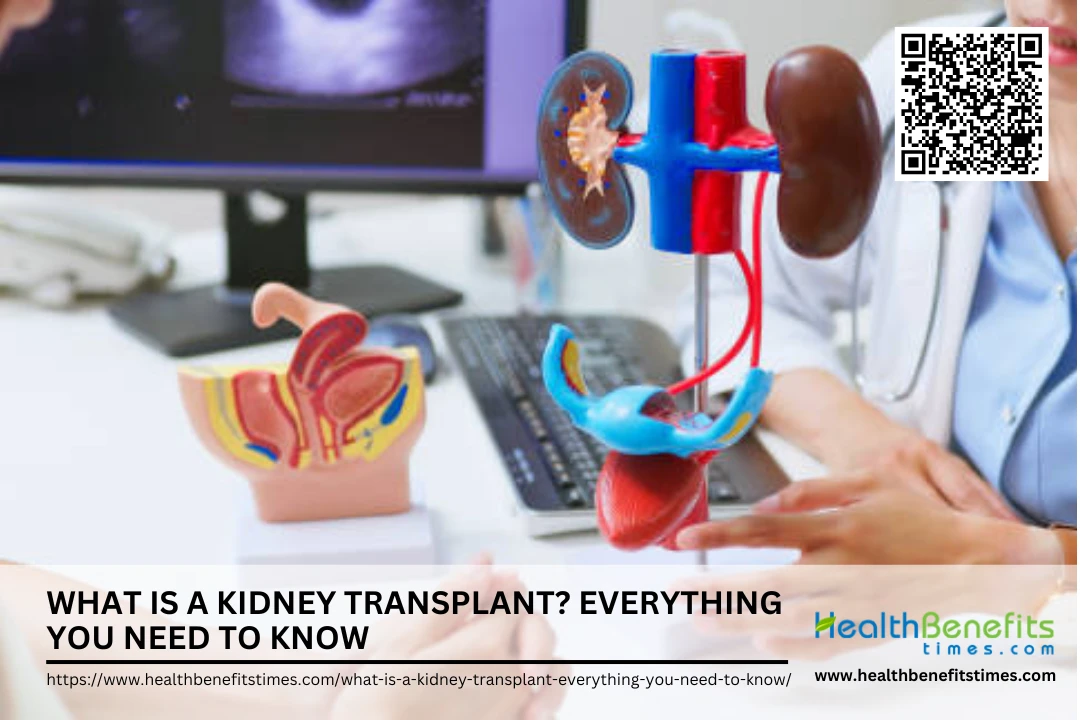 A kidney transplant is a surgical procedure in which a healthy kidney from a donor is placed into a person whose kidneys no longer function properly due to end-stage renal disease (ESRD) or other severe kidney conditions. Kidney transplantation is considered the best treatment option for patients suffering from chronic kidney disease (CKD) and ESRD, as it provides a better quality of life and longer survival compared to dialysis. The process involves receiving a kidney from either a deceased donor or a living donor, with living donor transplants offering better long-term outcomes. Despite the advantages, challenges such as organ rejection, long waiting lists, and the need for lifelong immunosuppressive medication exist. In this article, we will explore the kidney transplant process, eligibility criteria, risks, and life after transplantation.
A kidney transplant is a surgical procedure in which a healthy kidney from a donor is placed into a person whose kidneys no longer function properly due to end-stage renal disease (ESRD) or other severe kidney conditions. Kidney transplantation is considered the best treatment option for patients suffering from chronic kidney disease (CKD) and ESRD, as it provides a better quality of life and longer survival compared to dialysis. The process involves receiving a kidney from either a deceased donor or a living donor, with living donor transplants offering better long-term outcomes. Despite the advantages, challenges such as organ rejection, long waiting lists, and the need for lifelong immunosuppressive medication exist. In this article, we will explore the kidney transplant process, eligibility criteria, risks, and life after transplantation.
Understanding Kidney Transplants
A kidney transplant is a medical procedure where a diseased or non-functioning kidney is replaced with a healthy kidney from a donor to restore renal function. (1) The procedure involves connecting the new kidney to the recipient’s blood vessels and bladder, allowing it to filter waste and regulate body fluids. (2) Patients suffering from end-stage renal disease (ESRD) due to conditions like diabetes or hypertension are candidates for kidney transplants. (3) The surgery improves survival rates and enhances quality of life compared to dialysis. (4) However, challenges such as organ rejection and donor availability persist. (5)
Types of Kidney Transplants
Kidney transplants can come from living or deceased donors, each with unique benefits and challenges. Understanding the different types—living donor, deceased donor, and preemptive transplants—helps patients make informed decisions about their treatment.
 1. Deceased donor kidney transplant
1. Deceased donor kidney transplant
A deceased donor kidney transplant involves transplanting a kidney from a donor who has passed away due to brain death or circulatory death. These transplants make up a significant portion of kidney transplants worldwide, offering a vital solution for patients with end-stage kidney disease. (6) However, these kidneys may have a slightly higher risk of delayed function compared to living donor kidneys. (7) Despite this, deceased donor transplants are essential for increasing organ availability and saving lives. (8)
2. Living donor kidney transplant
A living donor kidney transplant is when a healthy individual donates a kidney to a recipient in need. This type of transplant offers better long-term outcomes and shorter waiting times compared to deceased donor transplants. (9) Living donors can be related or unrelated, as long as they are a good match for the recipient. (10) Additionally, paired kidney exchange programs allow incompatible donor-recipient pairs to swap kidneys with another pair, increasing the chances of a successful match. (11)
3. Preemptive kidney transplant
A preemptive kidney transplant is performed before a patient requires dialysis, offering better survival rates and reducing complications associated with kidney failure. Patients who receive a preemptive transplant have improved long-term outcomes compared to those who undergo dialysis before transplantation. (12) Research suggests that this approach minimizes cardiovascular risks and enhances post-transplant recovery. (13) Additionally, preemptive transplantation is linked to lower rejection rates and better graft function. (14)
4. Paired kidney donation (Kidney Exchange Program)
Paired kidney donation (kidney exchange) allows incompatible donor-recipient pairs to swap kidneys with another mismatched pair, increasing transplant opportunities. This program helps patients with immune or blood type incompatibilities receive a suitable kidney from another donor. (15) Studies show that paired kidney donation significantly improves access to transplantation, reducing wait times for recipients. (16) Moreover, it enhances graft survival rates and reduces rejection risks compared to deceased donor transplants. (17)
5. Simultaneous Kidney-Pancreas Transplant
A Simultaneous Kidney-Pancreas (SPK) Transplant is a procedure performed primarily for patients with Type 1 diabetes and end-stage kidney disease, offering the potential to cure diabetes and restore kidney function. This approach significantly improves long-term survival and quality of life by addressing both organ failures at once. (18) Studies suggest that SPK transplantation leads to better glycemic control and reduced cardiovascular complications compared to kidney transplant alone. However, it comes with increased surgical complexity and requires careful post-transplant monitoring.
Eligibility for a Kidney Transplant
Eligibility for a kidney transplant depends on medical, lifestyle, and psychological factors. Doctors assess overall health, organ compatibility, and potential risks to determine if a patient qualifies for this life-saving procedure.
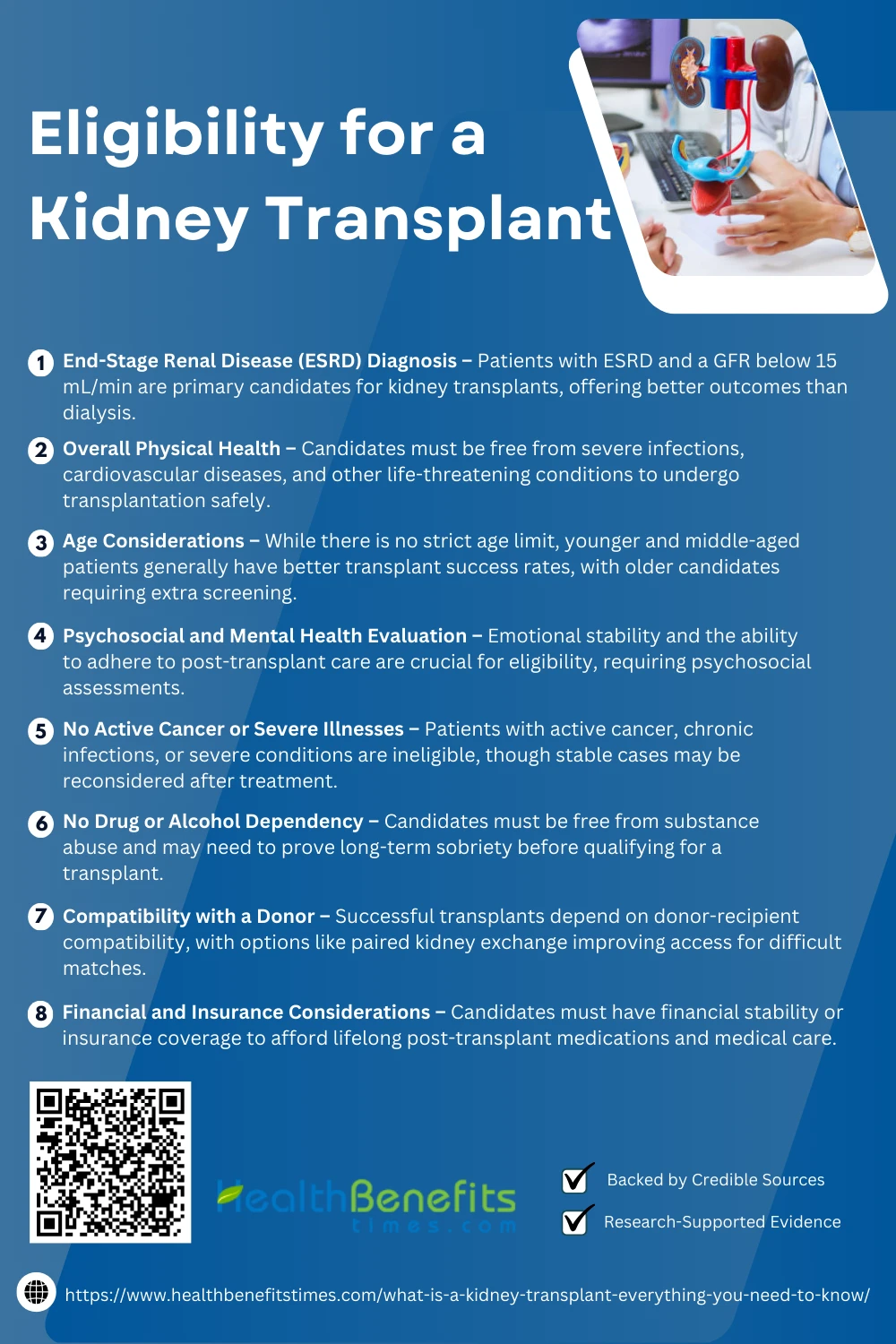 1. End-Stage Renal Disease (ESRD) Diagnosis
1. End-Stage Renal Disease (ESRD) Diagnosis
Patients with end-stage renal disease (ESRD), characterized by a glomerular filtration rate (GFR) below 15 mL/min, are the primary candidates for a kidney transplant. At this stage, the kidneys can no longer function effectively, requiring either dialysis or transplantation for survival. Studies highlight that kidney transplants offer better long-term health benefits compared to dialysis, improving quality of life and life expectancy. (19)
2. Overall Physical Health
A kidney transplant requires good overall health, meaning candidates must be free from active infections, severe cardiovascular diseases, or other life-threatening conditions. Patients with untreated diabetes, heart disease, or infections may face complications post-transplant. Evaluations include comprehensive health screenings to ensure that the patient is physically capable of undergoing surgery and managing recovery effectively. (20)
3. Age Considerations
There is no strict age limit for kidney transplants, but younger and middle-aged patients typically experience better transplant success rates due to their stronger immune response and ability to recover faster. While older patients can still receive a transplant, they must meet additional health requirements to ensure they can tolerate surgery and post-transplant medications. Studies indicate that elderly candidates require careful screening for complications like frailty, heart disease, and metabolic disorders. (21)
4. Psychosocial and Mental Health Evaluation
Mental and emotional stability is crucial for post-transplant success, as patients must adhere to strict medication regimens and lifestyle changes. Candidates undergo psychosocial evaluations to assess their ability to handle stress, medication adherence, and post-surgical care. Those with severe depression, anxiety, or cognitive impairments may require additional support or counseling to be considered for transplantation. (22)
5. No Active Cancer or Severe Illnesses
Patients with active cancer, chronic infections, or severe conditions such as advanced heart failure or liver disease are often ineligible for a kidney transplant. Transplantation requires a strong immune system, and ongoing illnesses can increase the risk of organ rejection or surgical complications. However, those who have successfully undergone cancer treatment or managed chronic illnesses for a stable period may be reconsidered after thorough evaluations. (23)
6. No Drug or Alcohol Dependency
Patients must be free from substance abuse, as addiction significantly affects medication adherence and overall health. Drug and alcohol dependency can lead to organ rejection, noncompliance with medications, and poor post-surgery outcomes. Candidates with a history of substance abuse must demonstrate long-term sobriety and may need to complete rehabilitation programs before being considered for a transplant. (24)
7. Compatibility with a Donor
A successful kidney transplant depends on donor-recipient compatibility, including blood type, tissue matching, and immune system response. A poorly matched kidney increases the risk of rejection, requiring stronger immunosuppressive medications. Modern techniques like paired kidney exchange and desensitization therapies help expand donor options for difficult-to-match patients. (25)
8. Financial and Insurance Considerations
A kidney transplant is a lifelong commitment, requiring expensive immunosuppressive medications, routine check-ups, and potential re-hospitalizations. Many transplant programs assess a candidate’s financial stability and insurance coverage to ensure they can afford the necessary treatments. Studies highlight that lack of financial resources is a major barrier to transplantation, and assistance programs may be available to help eligible patients. (26)
The Kidney Transplant Process
The kidney transplant process involves several key steps, from finding a compatible donor to preparing for surgery. Understanding each phase ensures patients are well-informed about what to expect during their transplant journey.
The evaluation and testing process for a kidney transplant involves a comprehensive series of medical assessments. Initially, patients undergo a detailed medical history review, laboratory tests, and imaging studies to assess their kidney function, organ health, and overall suitability for surgery. Psychosocial evaluations also ensure that candidates can comply with the necessary post-transplant care regimen. (27) This process identifies any underlying conditions that could affect the success of the transplant, such as cardiovascular issues. (28) Comprehensive testing also helps evaluate tissue compatibility for potential donors, (29) and in some cases, it may include additional steps for high-risk patients, such as genetic testing. (30)
2. Waiting List and Matching Process
Once evaluated, patients are placed on the kidney transplant waiting list, where they are ranked based on medical urgency, compatibility, and waiting time. The matching process is primarily driven by blood type compatibility and tissue matching, with a national registry used to allocate available organs. (31) The UNOS system assigns priority to patients based on various medical factors, ensuring that organs are allocated fairly. (32) For patients with high sensitization (those with a previous transplant or antibodies against certain donors), advanced matching techniques such as desensitization protocols are utilized. (33) Additionally, patients may be eligible for paired kidney exchanges, where incompatible donor-recipient pairs can swap kidneys. (34)
3. Finding a Living Donor
Finding a living donor for a kidney transplant can significantly shorten waiting times and improve patient outcomes. Living kidney donors are typically family members or close friends, but altruistic donors (unrelated individuals) can also donate. (1) Potential donors undergo rigorous compatibility testing, including blood type and tissue matching to ensure the transplant’s success. (35) Living donor transplants offer better long-term outcomes and reduced risk of organ rejection compared to deceased donor transplants. (36) Donor safety is a top priority, and modern procedures, such as laparoscopic kidney donation, minimize recovery time. (37)
4. The Transplant Surgery
The kidney transplant surgery involves placing the donor kidney into the recipient’s abdomen, connecting it to blood vessels and the bladder. The surgery typically lasts 3 to 4 hours, with careful attention given to ureteral stent placement to ensure proper urine flow from the new kidney. (38) Surgeons use advanced techniques to minimize risks of bleeding and organ damage during the procedure. (39) After surgery, the patient is closely monitored in an intensive care unit for immediate recovery, with tests to assess kidney function and ensure there are no signs of rejection. (40) The procedure’s success depends on precise surgical techniques and post-operative care. (41)
5. Post-Transplant Care and Immuno-suppressants
After a kidney transplant, patients are closely monitored for organ rejection, infection, and proper kidney function. Immunosuppressant medications are critical to prevent the immune system from attacking the new kidney. These drugs include cyclosporine and tacrolimus, which must be carefully balanced to avoid toxicity and infections. (42) Regular blood tests are essential to monitor drug levels and kidney function, with adjustments to the regimen as needed (EBSCOhost). Post-transplant care also involves addressing side effects like high blood pressure and diabetes caused by immunosuppressants, and patients must adhere to a strict regimen for long-term success. (43) (44)
6. Follow-Up Care
Post-transplant follow-up care is essential for ensuring the success of the kidney transplant. Patients undergo frequent check-ups, including blood tests, to monitor kidney function and detect signs of rejection. Adjustments to medications, including immunosuppressants, are made based on test results. (45) Follow-up visits also include psychosocial support to manage emotional challenges. (41) Vaccination schedules and infection prevention strategies are vital as immunosuppressant use increases susceptibility to infections. (46) Regular monitoring and care contribute to long-term success and better outcomes. (47)
Post-Transplant Recovery and Care
Successful post-transplant recovery requires comprehensive medical monitoring, psychological support, and strict adherence to immunosuppressant therapy. Routine follow-up visits and blood tests help detect early signs of rejection, ensuring optimal kidney function. (48) Psychological factors also play a crucial role, as emotional well-being significantly impacts post-transplant adherence and recovery outcomes. (49) Additionally, rehabilitation programs that include lifestyle adjustments, dietary plans, and physical activity contribute to long-term health improvements. (50)
Benefits of a Kidney Transplant
A kidney transplant offers life-changing benefits, including improved kidney function, freedom from dialysis, and enhanced quality of life. Successful transplants can significantly increase lifespan and overall well-being for recipients.
A kidney transplant significantly enhances a patient’s quality of life by reducing fatigue, improving overall well-being, and restoring normal kidney function. Research shows that transplant recipients experience fewer dietary restrictions and greater mobility, enabling them to resume daily activities and work. (20) Compared to dialysis, transplants lead to better psychological and social outcomes. (51) Post-transplant care and rehabilitation further improve health and reduce stress. (52) Studies highlight that kidney transplants lead to better mental well-being and life satisfaction, (53) with lower risks of depression and anxiety. (54)
2. Increased Life Expectancy
A kidney transplant substantially increases life expectancy compared to remaining on dialysis. Studies indicate that transplant recipients live significantly longer, with improved survival rates due to restored kidney function and reduced cardiovascular complications. (55) Transplants also lower the risk of infections and other dialysis-related complications, leading to better long-term health outcomes. (56) Reports suggest that younger patients undergoing transplantation can gain decades of life compared to dialysis patients. (57) Additionally, transplantation reduces the risk of kidney failure recurrence, improving overall longevity. (58) Long-term follow-ups demonstrate that kidney transplants extend lifespan while maintaining a better quality of health. ({% trusted %})
3. Greater Freedom and Convenience
A kidney transplant restores independence and improves the overall quality of life by eliminating the need for frequent dialysis sessions, allowing patients to resume work, travel, and engage in daily activities without restrictions. (59) Transplant recipients report greater psychological well-being and social engagement compared to dialysis patients. (60) Research also indicates that transplantation reduces stress related to managing chronic kidney disease, enhancing emotional freedom. (61) Furthermore, adolescent transplant recipients experience increased energy levels and fewer physical limitations. (62) Studies confirm that renal transplantation improves personal autonomy, making life more convenient and fulfilling. (63)
4. Reduced Risk of Cardiovascular Disease
Kidney transplant patients experience a lower risk of cardiovascular disease compared to those on long-term dialysis, as transplantation reduces hypertension, inflammation, and vascular complications. (64) Studies indicate that transplant recipients have a significantly lower likelihood of developing coronary artery disease and heart failure compared to dialysis patients. (5) Research shows that long-term survival is enhanced as cardiovascular risk factors stabilize post-transplant. (16) Additionally, a kidney transplant improves lipid metabolism and glucose regulation, reducing metabolic syndromes linked to heart disease. (65) A recent meta-analysis supports that kidney transplant patients have better long-term cardiovascular outcomes than those undergoing continuous dialysis. (66)
5. Fewer Dietary Restrictions
A kidney transplant allows recipients to enjoy a more balanced and less restrictive diet compared to dialysis patients. Unlike those on dialysis, transplant patients do not have to severely limit potassium, phosphorus, and fluid intake, which improves nutritional quality and overall well-being (The Lancet). Research highlights that post-transplant patients experience better digestion and metabolism, reducing food-related health concerns. (67) Transplant recipients are encouraged to maintain a healthy, diverse diet to prevent complications such as obesity and hypertension. (68) Studies suggest that proper nutritional balance post-transplant enhances kidney function and recovery. (69) Additionally, fewer dietary restrictions contribute to a higher quality of life and better patient satisfaction. (70)
Risks of a Kidney Transplant
A kidney transplant, while life-saving, carries certain risks. These include organ rejection, infection, complications from surgery, and side effects from immunosuppressant medications. Long-term monitoring is essential to prevent and manage potential complications.
One of the primary risks of a kidney transplant is organ rejection, where the recipient’s immune system attacks the new kidney despite immunosuppressant therapy. Acute rejection can occur within weeks, while chronic rejection may develop over time, leading to transplant failure. (71) To mitigate this risk, patients require continuous monitoring, and adjustments to medications are often necessary to maintain long-term kidney function. (72)
2. Side Effects of Immuno- suppressants
Immunosuppressants, essential for preventing kidney rejection, come with various side effects, including increased infection risk, high blood pressure, diabetes, and osteoporosis. Long-term use may also elevate the risk of cancer due to reduced immune surveillance. (73) Regular health monitoring and lifestyle modifications are necessary to balance the benefits of these medications while minimizing complications. (20)
3. Higher Risk of Infections
Kidney transplant recipients face an increased risk of bacterial, viral, and fungal infections due to the long-term use of immunosuppressants, which weaken the immune system. Opportunistic infections such as cytomegalovirus (CMV) and tuberculosis are more common in transplant patients, requiring strict monitoring and preventive measures. (74) Proper vaccination schedules and antiviral prophylaxis help reduce infection risks post-transplant. (75)
4. Increased Cancer Risk
Long-term immunosuppressant use in kidney transplant patients can lead to a higher risk of cancers, including skin cancer, lymphoma, and kidney tumors. The reduced immune response makes it difficult to detect and destroy malignant cells, increasing the risk of cancer development over time. (76) Regular oncological screening and sun protection measures are essential for reducing post-transplant cancer risks. (30)
5. Cardiovascular Complications
Patients undergoing kidney transplants face an increased risk of bacterial, viral, and fungal infections due to the lifelong use of immunosuppressant medications, which weaken the immune system. Conditions like tuberculosis (TB) and opportunistic viral infections are more common among transplant recipients, necessitating strict infection control measures. (75) Preventive treatments and routine screenings help minimize these risks, improving patient outcomes and long-term graft survival. (74)
Life after a Kidney Transplant
After a kidney transplant, patients experience a significant improvement in quality of life, with better energy levels, reduced dietary restrictions, and fewer hospital visits compared to dialysis. (77) However, lifelong use of immunosuppressants is required to prevent organ rejection, necessitating regular follow-up care. (57) Studies show that transplant recipients have increased life expectancy, with better long-term survival rates compared to dialysis patients. (28) Emotional well-being and social reintegration also improve significantly. (78) Post-transplant care focuses on managing medication side effects and reducing risks such as infections and cardiovascular diseases. (5) Regular monitoring of kidney function and healthy lifestyle choices ensure long-term transplant success. (79) Despite the challenges, kidney transplants offer greater freedom and the ability to return to work and daily activities. (80) Researchers emphasize the importance of mental health support to help recipients adapt to their new lifestyle. (81) With proper care, kidney transplants can provide long-lasting health benefits and a better future for patients. (82)
Alternatives to Kidney Transplants
If a kidney transplant isn’t an option, several alternative treatments can help manage kidney failure. Dialysis, medications, and lifestyle changes can support kidney function, improving quality of life and overall health.
1. Hemodialysis
Hemodialysis is a widely used alternative for patients with end-stage kidney disease who are unable to undergo a transplant. This process removes waste, excess fluids, and toxins from the blood through a dialysis machine, helping maintain stable kidney function. (83) While it is effective in sustaining life, long-term hemodialysis patients face challenges such as cardiovascular risks and dietary restrictions, making transplantation the preferred option when feasible. (84)
2. Peritoneal Dialysis
Peritoneal dialysis is another effective renal replacement therapy, allowing patients to filter waste through the peritoneal membrane in their abdomen. This home-based treatment offers greater flexibility and fewer dietary restrictions compared to hemodialysis. (83) Studies suggest that peritoneal dialysis patients experience better quality of life and independence, but infection risks like peritonitis require careful management. (85)
3. Bio-artificial Kidneys
Bioartificial kidneys are a promising alternative to traditional kidney transplants, aiming to mimic natural kidney functions without requiring immunosuppressive drugs. These devices combine cell-based filtration systems with artificial components to support long-term renal function. (86) Research suggests that bioartificial kidneys could provide a permanent solution for kidney failure patients, reducing reliance on dialysis and donor transplants. (57)
4. Xenotransplantation (Animal-to-Human Transplantation)
Xenotransplantation, the transplantation of genetically modified animal organs into humans, is being explored as a potential alternative for kidney transplants due to organ shortages. Recent breakthroughs in pig-to-human kidney transplantation show promise in overcoming immunological barriers. (87) However, concerns about long-term graft survival and cross-species infections remain key challenges in advancing xenotransplantation as a routine treatment. (88)
5. Wearable Artificial Kidneys
Wearable artificial kidneys (WAKs) are an emerging alternative to kidney transplants, designed to provide continuous blood filtration without the need for large dialysis machines. These portable devices allow greater mobility and flexibility, improving patient quality of life while reducing dialysis dependency. (89) Research suggests that WAKs could revolutionize kidney failure treatment, offering a sustainable and accessible alternative to transplantation. (90)
Conclusion
A kidney transplant is a life-changing procedure that can restore kidney function and improve quality of life for those with kidney failure. While it offers significant benefits, it also comes with risks, including potential complications and the lifelong need for immunosuppressive medications. Understanding the process, eligibility, and post-transplant care is crucial for making informed decisions. Whether considering a transplant or exploring alternative treatments, consulting with healthcare professionals can help determine the best path forward for long-term kidney health.