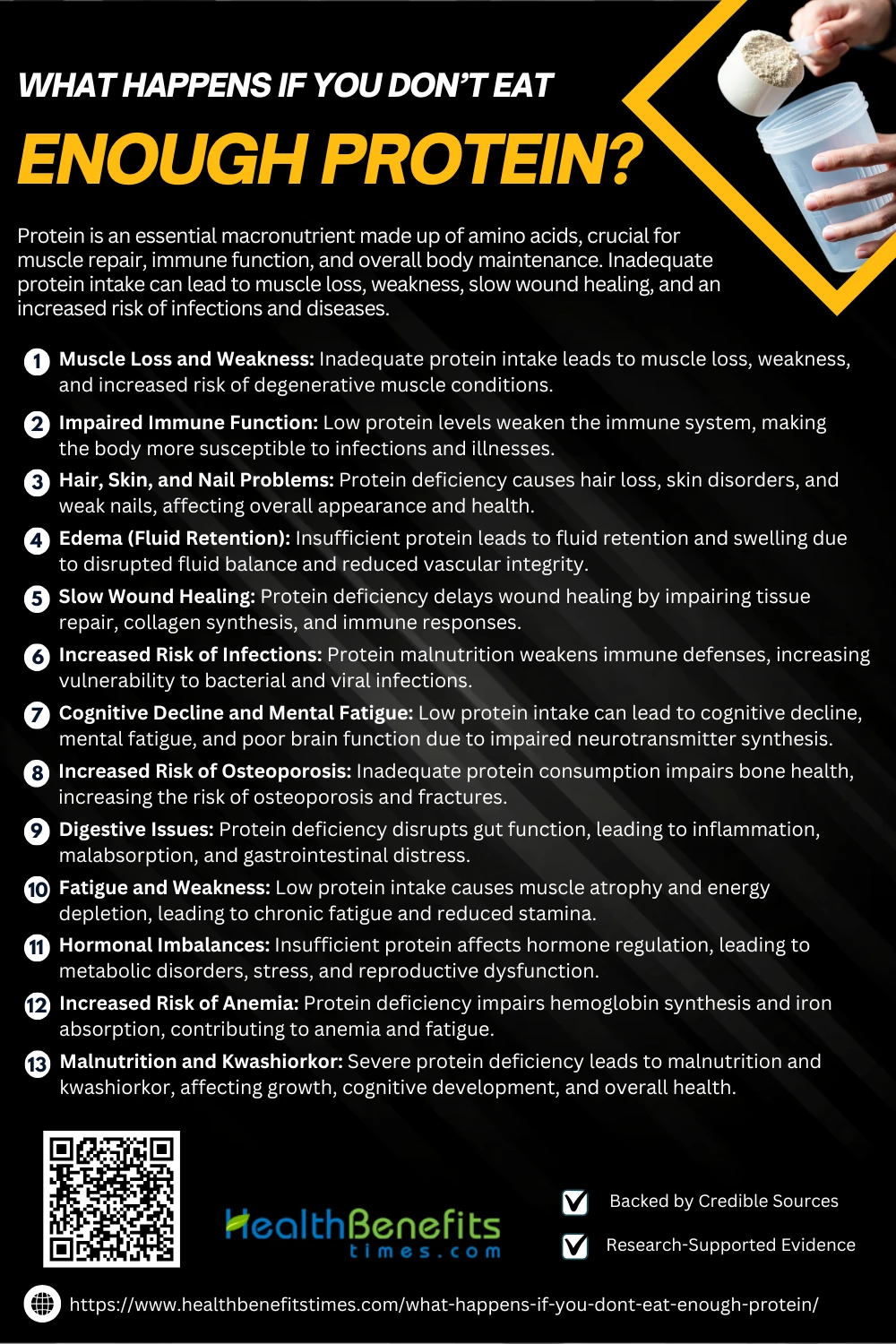
- Protein is an essential macronutrient made up of amino acids, crucial for muscle repair, immune function, and overall body maintenance.
- Inadequate protein intake can lead to muscle loss, weakness, slow wound healing, and an increased risk of infections and diseases.
- Chronic protein deficiency may cause hormonal imbalances, osteoporosis, cognitive decline, and severe malnutrition conditions like kwashiorkor.
 Protein is an essential macronutrient composed of amino acids that play a critical role in muscle growth, tissue repair, enzyme production, and immune function (1). A diet deficient in protein can have severe health consequences, affecting everything from muscle mass to metabolic function. Insufficient protein intake can lead to muscle wasting, impaired immune response, and increased susceptibility to infections (2). Research has shown that prolonged protein deficiency can compromise erythropoiesis, leading to reduced red blood cell production and anemia (3). Additionally, inadequate protein consumption is linked to weakened bone mineral density, increasing the risk of osteoporosis and fractures (4). Studies also indicate that protein deficiency negatively impacts cognitive function, impairing neurotransmitter activity and memory retention (5). The gut microbiome is also affected, as low protein intake can disrupt intestinal balance, leading to digestive issues (6). Furthermore, research suggests that inadequate dietary protein may exacerbate age-related muscle loss, or sarcopenia, significantly reducing mobility in older adults (7). Given these risks, maintaining a balanced diet with sufficient protein is essential for overall health and longevity (8).
Protein is an essential macronutrient composed of amino acids that play a critical role in muscle growth, tissue repair, enzyme production, and immune function (1). A diet deficient in protein can have severe health consequences, affecting everything from muscle mass to metabolic function. Insufficient protein intake can lead to muscle wasting, impaired immune response, and increased susceptibility to infections (2). Research has shown that prolonged protein deficiency can compromise erythropoiesis, leading to reduced red blood cell production and anemia (3). Additionally, inadequate protein consumption is linked to weakened bone mineral density, increasing the risk of osteoporosis and fractures (4). Studies also indicate that protein deficiency negatively impacts cognitive function, impairing neurotransmitter activity and memory retention (5). The gut microbiome is also affected, as low protein intake can disrupt intestinal balance, leading to digestive issues (6). Furthermore, research suggests that inadequate dietary protein may exacerbate age-related muscle loss, or sarcopenia, significantly reducing mobility in older adults (7). Given these risks, maintaining a balanced diet with sufficient protein is essential for overall health and longevity (8).
Role of Protein in the Body
Proteins are vital macronutrients that contribute to various physiological functions, including structural support, enzyme activity, and immune defense. Collagen, the most abundant protein, maintains skin elasticity and tissue integrity (9). Proteins also play a crucial role in neurotransmission, influencing brain function and mental health (10). Additionally, they are essential for muscle repair and growth, facilitating post-exercise recovery (11). Proteins regulate cellular activities, including gene expression and metabolic processes (12). Their role in maintaining immune homeostasis further underscores their importance in overall health (13).
What Happens If You Don’t Eat Enough Protein?
Protein is essential for muscle growth, tissue repair, and overall health. Without enough protein, your body struggles with muscle loss, fatigue, weak immunity, and more. Here’s what happens when your intake is insufficient.
1. Muscle Loss and Weakness
Protein is essential for muscle maintenance and repair, and inadequate intake can lead to muscle loss and weakness. Research has shown that low protein consumption impairs muscle protein synthesis, leading to progressive atrophy and reduced physical strength (14). Studies indicate that insufficient protein can exacerbate conditions like sarcopenia and neuromuscular degeneration, particularly in aging individuals (15). Additionally, inadequate protein affects cellular metabolism and mitochondrial function, further contributing to muscle fatigue and dysfunction (16). Chronic protein deficiency has also been linked to spinal muscular atrophy, which results in progressive muscle weakness and mobility issues (17). Moreover, clinical findings highlight that protein deficiency disrupts histone deacetylase regulation, worsening muscle deterioration in degenerative disorders (18). Ensuring adequate protein intake is crucial for preserving muscle mass, overall mobility, and long-term health.
2. Impaired Immune Function
Protein is essential for immune function, and inadequate intake can severely impair immune responses, reducing the body’s ability to fight infections. Studies show that low protein consumption disrupts amino acid transport and weakens immune cell production, making individuals more vulnerable to diseases (1). Prolonged protein deficiency leads to reduced immunoglobulin synthesis, limiting the body’s ability to combat pathogens effectively (19). Research has also found that insufficient protein intake weakens checkpoint proteins involved in immune regulation, further compromising immune surveillance (20). Additionally, malnutrition-induced gut-lung axis dysfunction has been linked to respiratory illnesses due to immune suppression (6). Maintaining adequate protein intake is essential for supporting immune function and preventing chronic infections.
3. Hair, Skin, and Nail Problems
Protein is fundamental for healthy hair, skin, and nails, as it provides essential amino acids for keratin and collagen synthesis. Studies highlight that protein deficiency contributes to skin disorders such as hypohidrosis and discoloration, weakening the skin’s protective barrier (1). Moreover, inadequate protein impairs nail growth and strength, making them prone to splitting and breakage (19). Furthermore, chronic protein malnutrition results in alopecia and delayed wound healing, exacerbating dermatological problems (20). Maintaining sufficient protein intake is crucial for sustaining healthy hair, skin, and nails.
4. Edema (Fluid Retention)
Protein plays a critical role in maintaining fluid balance, and inadequate intake can cause edema (fluid retention) due to reduced oncotic pressure. Studies indicate that low serum protein levels contribute to fluid accumulation in tissues, leading to swelling in the extremities (21). Research also highlights that hypoalbuminemia disrupts vascular integrity, promoting leakage and retention of fluids (22). Additionally, protein deficiency can exacerbate nephrotic syndrome, causing the kidneys to leak protein, leading to severe water retention and swelling (23). Furthermore, malnutrition-induced fluid retention can result in pleural effusions and ascites, complicating respiratory function (24). Ensuring adequate protein intake is essential for regulating fluid distribution and preventing edema.
5. Slow Wound Healing
Protein is essential for wound healing, as it supports collagen synthesis and immune responses. Insufficient protein intake can delay wound closure by impairing cellular repair mechanisms and inflammatory responses (25). Studies show that protein deficiency reduces fibroblast proliferation, a crucial factor in tissue regeneration (26). Furthermore, low protein levels disrupt immune function, increasing the risk of wound infections and prolonging the healing process (27). Additionally, research indicates that protein supplementation accelerates recovery by enhancing angiogenesis and reducing inflammation (28). Ensuring adequate protein intake is vital for efficient tissue repair and overall recovery.
6. Increased Risk of Infections
Protein is crucial for immune function, and inadequate intake weakens immune defenses, increasing susceptibility to infections. Research shows that protein deficiency reduces antibody production and weakens immune responses, making individuals prone to bacterial and viral infections (27). Studies have linked low protein levels to impaired lung function, increasing the risk of respiratory infections (29). Additionally, protein malnutrition alters gut microbiota, weakening mucosal immunity and increasing vulnerability to gastrointestinal infections (30). Furthermore, insufficient protein intake reduces white blood cell production, impairing the body’s ability to fight off infections effectively (31). Ensuring adequate protein consumption is vital for robust immune function and disease prevention.
7. Cognitive Decline and Mental Fatigue
Protein is vital for brain function and cognitive health, and insufficient intake can contribute to mental fatigue and cognitive decline. Research indicates that low protein levels impair neurotransmitter synthesis, affecting memory, concentration, and decision-making (32). Studies also highlight that protein deficiency weakens mitochondrial function, leading to chronic fatigue and reduced brain energy metabolism (33). Furthermore, research on sleep-deprived individuals has shown that protein intake plays a role in preventing hippocampal neuronal damage, which is crucial for learning and memory (34). Additionally, inadequate protein consumption increases neuroinflammation, exacerbating cognitive impairment and mental exhaustion (35). Ensuring a protein-rich diet is essential for cognitive longevity and sustained mental energy.
8. Increased Risk of Osteoporosis
Protein is essential for bone health and density, and inadequate intake significantly increases the risk of osteoporosis. Studies show that low protein levels impair calcium absorption, leading to decreased bone mineralization and increased fracture risk (36). Additionally, insufficient dietary protein weakens collagen synthesis, which is crucial for bone structure and resilience (37). Research highlights that amino acid deficiency accelerates bone loss, particularly in aging populations, exacerbating osteoporosis progression (38). Furthermore, low protein intake has been linked to jawbone osteoporosis, indicating its impact on both skeletal and dental health (39). Ensuring adequate protein consumption is essential for maintaining bone integrity and reducing osteoporosis risk.
9. Digestive Issues
Protein is essential for maintaining digestive health, and inadequate intake can lead to gastrointestinal disorders. Studies show that low protein levels impair gut barrier function, making the intestines more susceptible to inflammation and malabsorption (40). Additionally, research indicates that protein deficiency alters gut microbiota composition, leading to digestive discomfort and nutrient absorption issues (41). Inadequate protein intake has also been linked to intestinal disorders and fat malabsorption, which can cause bloating, diarrhea, and chronic digestive distress (42). Furthermore, insufficient protein contributes to gut inflammation, increasing the risk of conditions such as colitis and irritable bowel syndrome (43). Ensuring adequate protein intake supports digestive health and reduces the risk of gastrointestinal complications.
10. Fatigue and Weakness
Protein is vital for muscle function and energy production, and insufficient intake can lead to fatigue and weakness. Research shows that low protein levels impair muscle regeneration, contributing to chronic fatigue and reduced physical endurance (44). Studies also highlight that inadequate protein intake weakens mitochondrial function, disrupting energy metabolism and leading to persistent tiredness (45). Additionally, protein deficiency decreases muscle mass and strength, worsening symptoms of frailty and fatigue (33). Furthermore, malnutrition-induced muscle atrophy can exacerbate muscle weakness and decrease overall stamina (16). Ensuring adequate protein consumption is essential for maintaining muscle function and reducing fatigue.
11. Hormonal Imbalances
Protein plays a crucial role in hormonal regulation, and insufficient intake can lead to endocrine dysfunction. Research shows that low protein consumption impairs insulin signaling, increasing the risk of metabolic disorders and hormone imbalances (46). Additionally, studies indicate that protein deficiency disrupts adrenal hormone production, which can lead to fatigue, stress, and reduced energy levels (47). Furthermore, inadequate protein affects steroid hormone pathways, leading to menstrual irregularities and reproductive dysfunction (48). Lastly, protein deprivation can lower estrogen and testosterone levels, increasing the risk of osteoporosis and muscle loss (49). Ensuring adequate protein intake is essential for hormonal balance and overall health.
12. Increased Risk of Anemia
Protein is essential for red blood cell production, and insufficient intake can contribute to anemia by impairing hemoglobin synthesis. Studies show that low protein levels hinder iron absorption, increasing the risk of iron deficiency anemia (50). Research also indicates that protein malnutrition exacerbates anemia in patients with gastrointestinal disorders, where nutrient absorption is already compromised (51). Furthermore, inadequate protein intake has been linked to chronic inflammation and oxidative stress, both of which impair red blood cell function and lifespan (52). Additionally, protein deficiency impacts bone marrow function, reducing erythropoiesis and leading to persistent fatigue and weakness associated with anemia (53). Ensuring adequate protein intake is crucial for maintaining healthy blood production and preventing anemia.
13. Malnutrition and Kwashiorkor
Protein is essential for growth, development, and metabolic function, and severe deficiency can lead to malnutrition and kwashiorkor. Research highlights that protein deficiency is a major contributor to malnutrition-related mortality, especially in regions with food scarcity (54). Additionally, kwashiorkor is associated with poor-quality protein diets, often exacerbated by famine and low socio-economic conditions (55). Furthermore, malnutrition-induced kwashiorkor affects cognitive development, leading to long-term neurological deficits (56). Ensuring adequate protein intake is crucial for preventing severe malnutrition and related health complications.
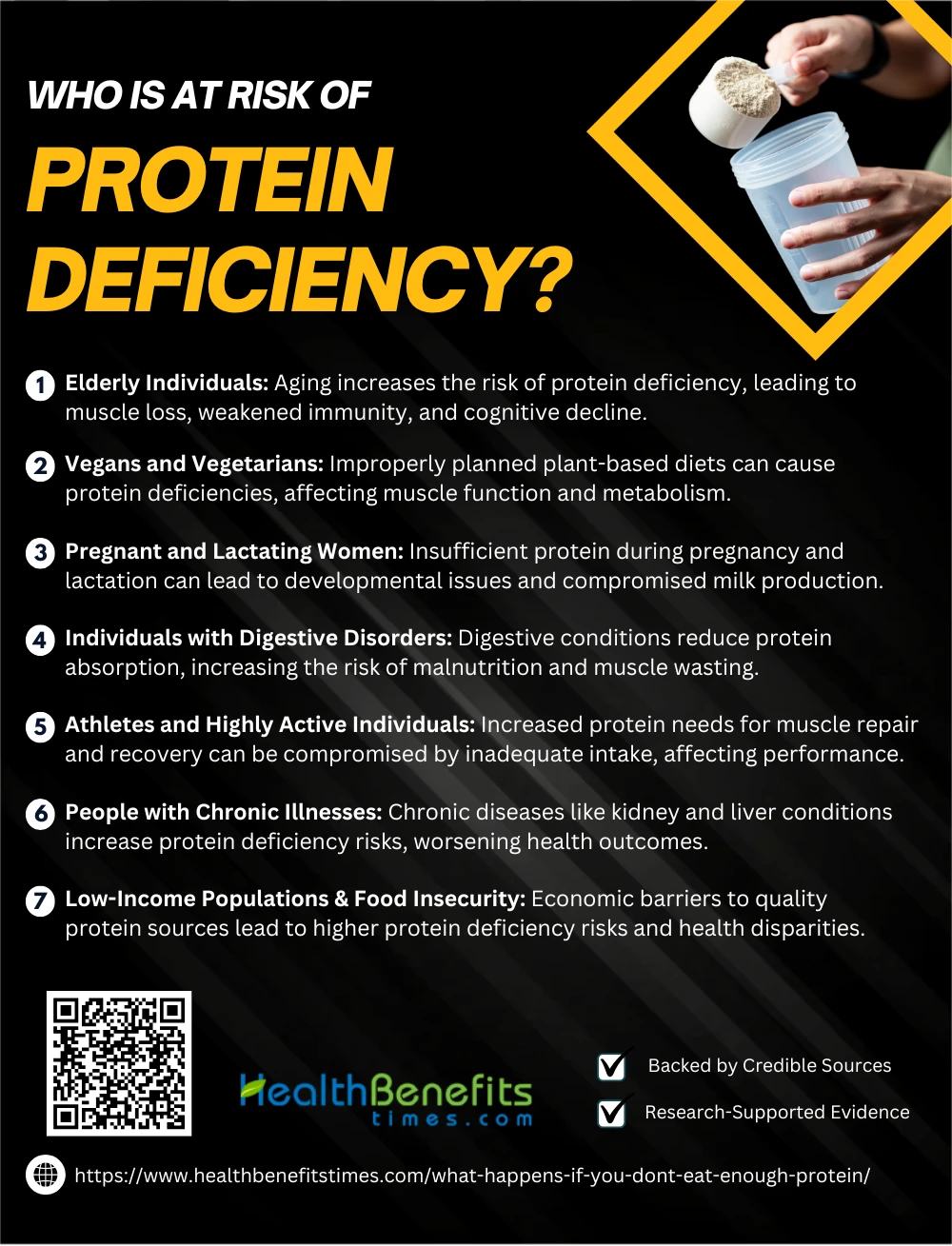
Who is at Risk of Protein Deficiency?
Protein deficiency can affect various groups, especially those with inadequate dietary intake or higher nutritional needs. Below are the key populations at risk:
1. Elderly Individuals
Aging increases the risk of protein deficiency, leading to muscle loss, weakened immunity, and cognitive decline. Research shows that older adults often struggle with protein absorption and reduced appetite, leading to frailty and sarcopenia (25). Studies highlight that low protein intake in seniors contributes to cognitive impairment and neurodegenerative diseases, such as Alzheimer’s (57). Additionally, elderly individuals with protein malnutrition are at higher risk of cardiovascular diseases, as protein is essential for vascular health (58). Furthermore, chronic kidney disease in aging adults is exacerbated by insufficient protein intake, negatively impacting renal function and overall metabolism (59). Ensuring adequate protein consumption is crucial for maintaining mobility, cognitive function, and longevity in the elderly.
2. Vegans and Vegetarians
A well-planned vegetarian or vegan diet can be healthy, but improper planning may lead to protein deficiencies, affecting muscle function and metabolism. Studies show that vegans and vegetarians often have lower protein intake, which can impact overall health and recovery (60). Research highlights that insufficient protein in plant-based diets can slow wound healing and muscle repair, leading to fatigue and weakness (61). Additionally, vegans may lack essential amino acids, which are critical for maintaining immune function and preventing malnutrition (62). Furthermore, studies suggest that vegans and vegetarians are at higher risk of sarcopenia (muscle loss) due to lower protein bioavailability, requiring careful dietary supplementation (63). Ensuring adequate protein intake from diverse plant-based sources is essential for maintaining muscle mass and overall health.
3. Pregnant and Lactating Women
Protein is essential during pregnancy and lactation, as it supports fetal growth and milk production. Inadequate protein intake in mothers can lead to developmental issues in infants, increasing the risk of malnutrition (25). Studies indicate that plant-based diets during pregnancy may contribute to protein deficiency, affecting both maternal and fetal health (64). Additionally, protein malnutrition in expectant mothers has been linked to pregnancy complications, such as low birth weight and preterm labor (65). Furthermore, lactating mothers require increased protein intake, as insufficient protein can impair milk production and nutrient supply for the infant (66). Ensuring adequate protein consumption is vital for maternal and infant health.
4. Individuals with Digestive Disorders
Digestive disorders such as Crohn’s disease, celiac disease, and irritable bowel syndrome impair nutrient absorption, leading to protein deficiency. Studies show that gastrointestinal conditions reduce protein uptake, increasing the risk of malnutrition and muscle wasting (67). Research indicates that patients with inflammatory bowel disease (IBD) experience chronic protein depletion, which can weaken immune responses and slow recovery (68). Additionally, digestive disorders interfere with pancreatic enzyme function, hindering protein digestion and causing deficiencies in essential amino acids (69). Furthermore, malabsorption syndromes contribute to muscle loss and fatigue, worsening the health outcomes of individuals with chronic digestive diseases (70). Ensuring adequate protein intake through specialized diets and supplements is crucial for managing digestive disorders.
5. Athletes and Highly Active Individuals
Athletes and highly active individuals have increased protein needs due to higher muscle turnover and recovery demands. Inadequate protein intake can impair muscle repair, weaken immunity, and reduce endurance, leading to suboptimal performance (71). Research highlights that protein deficiency among athletes can lead to reduced lean muscle mass and strength loss, impacting overall athletic output (72). Additionally, low protein consumption may compromise post-exercise recovery, increasing the risk of injuries and delayed healing (73). Furthermore, very high-protein diets must be carefully monitored, as excessive protein intake can strain kidney function in some individuals (74). Ensuring adequate protein intake through balanced nutrition is crucial for optimizing athletic performance and recovery.
6. People with Chronic Illnesses
Chronic illnesses such as kidney disease, diabetes, and inflammatory conditions increase the risk of protein deficiency, which can worsen health outcomes. Research shows that patients with kidney disease often suffer from protein-energy wasting, leading to muscle loss and weakness (75). Additionally, chronic inflammation in conditions like Crohn’s disease depletes protein stores, impairing immune function and recovery (68). Studies also highlight that malnutrition in obese individuals with chronic illnesses affects protein metabolism, leading to poor health outcomes (41). Furthermore, liver diseases disrupt protein synthesis, exacerbating muscle atrophy and metabolic imbalances (76). Ensuring adequate protein intake is essential for managing chronic illnesses and maintaining overall well-being.
7. Low-Income Populations & Food Insecurity
Low-income populations and food-insecure individuals face higher risks of protein deficiency, leading to malnutrition, weakened immunity, and stunted growth. Studies indicate that economic barriers prevent access to high-quality protein sources, increasing health disparities (77). Research highlights that food insecurity is linked to iron and protein deficiencies, significantly impacting children and pregnant women (78). Additionally, protein deficiency in marginalized communities leads to muscle wasting and cognitive impairments, reducing productivity and quality of life (41). Furthermore, undernourished individuals are more prone to chronic diseases, exacerbating socio-economic challenges (79). Ensuring affordable and sustainable protein access is vital for addressing global malnutrition.
How Much Protein Do You Need?
Protein requirements vary based on age, activity level, and health conditions. The Recommended Dietary Allowance (RDA) suggests 0.8 grams per kilogram of body weight for healthy adults, though athletes and older adults may need higher intake for muscle maintenance and recovery (80). Research indicates that pregnant and lactating women require increased protein intake to support fetal growth and milk production (81). Additionally, individuals with chronic illnesses or recovering from surgery may benefit from higher protein intake to enhance immune function and healing (82). Studies also highlight that excessive protein intake can strain kidney function, particularly in individuals with pre-existing renal conditions (83). Furthermore, protein timing plays a role in muscle synthesis, with experts recommending protein intake throughout the day for optimal absorption and recovery (84). Ensuring balanced protein consumption is key to overall health and performance.
How to Prevent Protein Deficiency?
Ensuring an adequate protein intake is essential for maintaining overall health. Below are key strategies to prevent protein deficiency:
1. Consume a Balanced Diet
A balanced diet ensures an adequate protein intake, preventing malnutrition and associated health risks. Research highlights that a diet rich in diverse protein sources enhances amino acid availability and overall well-being (85). Studies indicate that plant-based and animal-based protein combinations improve nutrient absorption, preventing deficiencies (86). Additionally, dietary modeling supports a balanced approach to protein consumption, promoting long-term health (87). Furthermore, deficient diets during pregnancy may lead to complications, emphasizing the importance of balanced nutrition for vulnerable populations (88). Ensuring a well-rounded diet is key to preventing protein-related deficiencies.
2. Monitor Daily Protein Intake
Monitoring daily protein intake ensures optimal muscle function, immune health, and overall well-being. Studies highlight that tracking protein consumption improves nutrient balance, preventing deficiencies linked to fatigue and weakness (89). Research suggests that consistent monitoring of dietary protein intake is crucial for maintaining metabolic health and avoiding malnutrition (90). Additionally, dietary protein assessments help regulate blood glucose levels, particularly in individuals with metabolic disorders (91). Furthermore, women’s health studies emphasize the importance of protein monitoring, as deficiencies can increase the risk of pregnancy complications and osteoporosis (92). Ensuring adequate protein intake through dietary tracking is essential for long-term health.
3. Include Protein-Rich Snacks
Incorporating protein-rich snacks into daily diets helps prevent protein deficiency, supports muscle health, and maintains energy levels. Research highlights that snacks containing nuts, dairy, and legumes enhance protein intake, improving overall nutrition (93). Studies suggest that alternative protein sources like edible insects can also combat malnutrition, providing sustainable and nutrient-dense options (94). Additionally, underutilized crops such as lentils and chickpeas offer cost-effective, protein-rich snack options, helping address food insecurity (95). Furthermore, nutrient-dense protein snacks have been linked to improved health outcomes in women, reducing deficiencies during pregnancy and lactation (92). Ensuring protein-rich snacks in daily meals enhances overall health and prevents deficiencies.
4. Address Digestive Health
Maintaining digestive health is crucial for optimal protein absorption and preventing deficiency. Research shows that digestive enzyme supplementation enhances protein digestion, improving nutrient uptake in individuals with impaired gastrointestinal function (96). Studies indicate that malabsorption disorders, such as celiac disease and Crohn’s, contribute to protein deficiency, necessitating targeted nutritional interventions (97). Additionally, post-bariatric surgery patients are at higher risk of protein malabsorption, requiring continuous dietary monitoring and supplementation (98). Furthermore, gut microbiota balance plays a key role in nutrient metabolism, with research highlighting that prebiotic and probiotic intake supports protein digestion and absorption (99). Ensuring gut health optimization through balanced nutrition is essential for preventing protein deficiency.
5. Educate Vulnerable Populations
Educating vulnerable populations on protein-rich diets is crucial for preventing malnutrition and associated health risks. Research highlights that nutrition education programs improve dietary habits, reducing protein deficiency in at-risk communities (100). Studies show that community-based nutrition interventions promote sustainable food choices, increasing protein intake among low-income families (101). Additionally, educational programs tailored for pregnant women help reduce protein-related deficiencies, ensuring better maternal and fetal health (25). Furthermore, school-based nutrition initiatives improve children’s protein consumption, combating childhood malnutrition (102). Raising awareness and implementing targeted educational strategies can effectively reduce protein deficiency in vulnerable populations.
Conclusion
Not getting enough protein can lead to muscle loss, fatigue, weakened immunity, and long-term health issues like bone weakness and hormonal imbalances. To stay healthy, ensure a balanced diet with adequate protein from diverse sources. Whether through animal-based or plant-based options, meeting your protein needs is essential for maintaining energy, strength, and overall well-being. If you’re unsure about your intake, consult a healthcare professional or nutritionist for personalized guidance.
References:
- Hernández, G. et al. (2025). Defective Slc7a7 transport reduces erythropoietin compromising erythropoiesis. Springer.
- Norouzitallab, P. et al. (2025). A Pilot Field Evaluation of Dietary Ginger Effects on Immunity and Blood Metabolism in Fish. MDPI.
- Biancarosa, I. et al. (2025). Modulating the Nutritional Value of Acheta domesticus through Dietary Supplementation. ScienceDirect.
- Maillot, F. et al. (2025). Bone Mineral Density in French Adults with Early-Treated Phenylketonuria. ScienceDirect.
- Zhang, X. et al. (2025). Effects of Lipoic Acid on Serum Biochemistry and Antioxidant Function in Heat-Stressed Broilers. Springer.
- Brandão, I. et al. (2025). Exploring the Role of Diet and Nutrition in Respiratory Health through the Gut-Lung Axis. Frontiers in Nutrition.
- Andrade, M.J. et al. (2025). Microbial Safety of Animal-Based Food Products. Frontiers in Nutrition.
- Hackney, A.C. et al. (2025). Appetite-Control and Eating-Behavior Traits in Weight-Cycling Athletes: The Wave Study. Human Kinetics.
- Fedorov, S. (2025). Collagen and Aging: A Scientific Perspective. ResearchGate.
- Peedicayil, J., & Santhosh, S. (2025). Histone Monoaminylation and Its Role in Psychiatric Disorders. Frontiers in Molecular Neuroscience.
- Vo-Nguyen, H., & Tran-Van, H. (2025). The Role of Disulfide Bridges in Recombinant Protein Interaction. Avicenna Journal of Medical Biotechnology.
- Romo-Vázquez, R. et al. (2025). Neuron Identity Switch and Its Impact on Cellular Function. Frontiers in Cellular Neuroscience.
- Martínez-García, G.G., & Suárez, M.F. (2025). Systemic Autophagy and Aging in Mice. bioRxiv.
- Chung, W. K., Lee, J. C., Pisapia, D. J., et al. (2024). Motor pool selectivity of neuromuscular degeneration in type I spinal muscular atrophy is conserved between human and mouse. Human Molecular Genetics.
- Lisco, G., Jo, H. G., Colaianni, G. (2025). Metabolic disorders as risk factors for osteoarthritis and targeted therapies for this pathology. Frontiers in Endocrinology.
- Belcher, D. (2025). Ribosome Biogenesis and Translational Control in Skeletal Muscle: Insights into Anabolic Deficits and Atrophy in Cancer Cachexia. Penn State University.
- Okada, S., Kakibuchi, D., Ishihara, S., et al. (2024). Robotic thymectomy for Morvan’s syndrome associated with thymoma: a case report. AME Groups.
- Osseni, A., & Schaeffer, L. (2025). Targeting histone deacetylase 6 (HDAC6) in Duchenne muscular dystrophy: New insights into therapeutic potential. Acta Physiologica.
- Liu, M., Wei, C., Xu, W., et al. (2025). Effect of prolonged starvation on nutrition utilization and transcriptional responses in Pacific oyster (Crassostrea gigas). Aquaculture Reports.
- Brom, V. C. (2025). Charakterisierung der Effekte agonistischer und antagonistischer Modulation von Immuncheckpoint-Molekülen auf die Osteoklastenbiologie. Bonn University.
- Anderson, M., & Dilip, M. (2024). Tapping into the Heart of a Diagnosis: A Case of Pleural Effusion with a Larger Story to Tell. UCLA Proceedings.
- Saad, O., & Rafiq, N. (2024). Unmasking posterior reversible encephalopathy syndrome: A hidden threat in juvenile lupus. Rheumatology Advances in Practice.
- Sheikh, J. A., Syed, U., & Osama, S. M. (2024). Nephrotic Syndrome Without Nephrotic Range Proteinuria.
- Lee, M., Channick, J., & Chan, V. (2024). Methimazole-Induced Hypothyroidism Presenting as Recurrent Thoracic Cavity Effusions and Ascites. ATS Journals.
- Sethi, V., & Murira, Z. (2025). Galvanizing and sustaining momentum are critical to improve maternal nutrition in South Asia. Frontiers in Nutrition.
- Subramaniam, S., Jose, A., Kenney, D., & O’Connell, A. K. (2025). Challenging the Notion of Endothelial Infection with Insights from the Current Scientific Evidence. Frontiers in Immunology.
- Liu, Z., Qing, L., Zhang, H., & Pan, X. (2025). Treatment of pediatric central nervous system infection caused by Carbapenem-resistant Klebsiella pneumoniae with Ceftazidime/Avibactam, two cases. Frontiers in Pharmacology.
- Kouw, I. W. K., Paulus, M. C., Boelens, Y. F. N., & Hermans, A. J. H. (2025). Feasibility Challenges in Protein Supplementation Research: Insights from the convalescence of functional outcomes after Intensive Care Unit Stay in a Randomised Study. Clinical Nutrition.
- Ebubechukwu, U., & Geraghty, P. (2025). Genesis of concurrent diseases: do diabetes mellitus and idiopathic pulmonary fibrosis have a direct relationship?
- Chen, J., Xue, W., Yao, Z., Wang, C., Zhu, W., & Wang, H. (2025). Epidemiological Investigation of Goose Circovirus Based on a Newly Developed Indirect ELISA Method. Frontiers in Veterinary Science.
- Aswani, Y., Aziz, H., Seda, P., Gosse, M. D., & Aparna, J. K. (2025). Cystic Echinococcus of the Liver. Journal of Obstetrics and Gynecology Science.
- Liu, Y. X., & Wang, J. (2024). Impact of comorbid subthreshold depressive symptoms on cancer-related fatigue and complications in adults with leukemia. World Journal of Psychiatry.
- Zabetakis, I., Booker, A., Teusch, N. E., & Dalby, A. (2025). Multisystem Inflammatory Syndrome observed Post-COVID-19: The Role of Natural Products, Medicinal Plants and Nutrients and the use of Prediction Tools. Frontiers in Pharmacology.
- Fu, X., Yan, S., Hu, Z., Sheng, W., Li, W., & Kuang, S. (2024). Guhan Yangsheng Jing mitigates hippocampal neuronal pyroptotic injury and magnifies learning and memory capabilities in sleep-deprived mice via the NLRP3 pathway. Journal of Ethnopharmacology.
- Wang, R., Liu, Y., Jiang, Y., Zhang, Y., & Zhang, Y. (2025). Shenling Baizhu San alleviates central fatigue through SIRT1-PGC-1α-Mediated mitochondrial biogenesis. Journal of Ethnopharmacology.
- Jooyandeh, H., & Aryamanesh, M. (2025). The effect of microbial transglutaminase enzyme treatment and Persian gum on the physicochemical and color characteristics of low-fat stirred yogurt. Journal of Food Science & Technology.
- Patel, B. L., Singh, P. K., & Singh, P. (2025). Heavy Metal Accumulation in Soybeans Cultivated in Singrauli Region.
- Bright, E., & ND, M. (2024). Thyroid Function and Genetics: Gene Mapping and Treatments to Change How Our DNA Manifests Itself. Eliz Bright.
- Šoić, I. (2024). Hypovitaminosis and Oral Health. University of Zagreb Repository.
- Castañeda, S., & Ramírez, J. D. (2025). From Genes to Worms: A Deep Dive into Helminth Omics.
- Frias-Toral, E., Ceriani, F., Carriel, J., & Ramos, A. (2025). Understanding Obesity to Determine the Best Therapeutic Option: From Lifestyle Interventions to Therapies. Frontiers in Nutrition.
- Akcura, C., Alkan, S., Güney, S. C., & Sunbul, B. (2025). P-39 A Late Onset Case of Chylomicron Retention Disease. JCEM Case Reports.
- Sayed, I. M., & Das, S. (2025). Infection-Mediated Inflammation Promotes Cancer Initiation and/or Progression. Frontiers in Medicine.
- Hang, M., Pang, B. P. S., Iu, E. C. Y., Chan, W. S., & Tse, M. C. L. (2024). Deficiency of muscle-generated brain-derived neurotrophic factor causes inflammatory myopathy through reactive oxygen species-mediated necroptosis and weakness. Redox Biology.
- Andreasson, K. (2025). Physical activity, intensive exercise, and mechanisms for muscle impairment in patients with idiopathic inflammatory myopathies. Open Archive KI.
- Jeong, S. H., Kim, H. H., & Rodelas-Angelia, A. J. D. (2025). Inhibition of Melanogenesis via Passive Immune Targeted Alpha-MSH Binder Polypeptide.
- Glinicki, P., Sawicka-Gutaj, N., & Araujo-Castro, M. (2025). Advances in Diagnostics and Management of Adrenal Tumors. Frontiers in Endocrinology.
- Chang, X., MacIsaac, H. J., Zhang, J., & Zhou, Y. (2025). Cyanobacteria alter lipid metabolism in zooplankton via exudates of obesogens. Harmful Algae.
- Savage, C. H., Fox, S. N., Amireddy, N. R., & McMeekin, L. J. (2025). Estrogen-related receptor gamma is a regulator of mitochondrial, autophagy, and immediate-early gene programs in spiny projection neurons. Neurobiology of Disease.
- Khadse, P. M., & Chakre, S. (2024). Iron Deficiency and Nutritional Challenges in Low-Protein Diets. International Journal of Basic and Applied Sciences.
- Jabłońska, B. (2025). Nutritional Status and Nutritional Support in Patients with Gastrointestinal Diseases.
- Kontoghiorghes, G. J. (2024). New Insights into Aspirin’s Anticancer Activity: The Predominant Role of Its Iron-Chelating Antioxidant Metabolites.
- Alghanim, L. (2024). Design and Synthesis of Benzamide-Substituted Aromatic Aldehydes as Potential Therapeutics for Sickle Cell Disease. Virginia Commonwealth University.
- Moini, J., & Ferdowsi, K. (2024). Protein Deficiencies. Handbook of Nutritional Disorders.
- Hernandez, L., Hawash, A., & Schmidt, F. B. (2024). Kwashiorkor caused by a vegan diet. European Journal of Pediatric Dermatology.
- Ramadhani, D. H., Jumadi, J., & Sandi, G. (2024). Implementasi Algoritma K-Nearest Neighbors (KNN) Untuk Prediksi Gizi Buruk. SMATIKA JURNAL: STIKI.
- Li, X., Lin, Z., Chen, S., et al. (2025). Tiaogeng Decoction improves mild cognitive impairment in menopausal APP/PS1 mice through the ERs/NF-κ B/AQP1 signaling pathway.
- Kroon, J., Guillamat-Prats, R., et al. (2025). Vascular-and Immuno-Metabolism as Drivers of Cardiovascular Disease: Insights Obtained from Omics Approaches. Frontiers in Cell and Developmental Biology.
- Wang, Y. (2025). The significance of matrix remodeling associated 7 (MXRA7) in pathogenesis or management of renal diseases deserves more investigations. Renal Failure.
- Jurzak, N. (2024). Diety roślinne u dzieci, przegląd i bezpieczeństwo stosowania. Jagiellonian University Repository.
- Min, M., Tarmaster, A., Bodemer, A., & Sivamani, R. K. (2024). The Influence of a Plant-Based Diet on Skin Health: Inflammatory Skin Diseases, Skin Healing, and Plant-Based Sources of Micro-and Macro-Nutrients.
- Wolska, A. (2024). Ocena i porównanie spożycia wybranych składników pokarmowych w grupach wegan i wegetarian. Jagiellonian University Repository.
- Jang, W. Y., Kim, J. Y., Choi, E. J., et al. (2024). Evaluation of antioxidant activity and fermentation properties of potential probiotic strain Lactiplantibacillus plantarum HY7720 in plant-based materials. Discover Applied Sciences.
- Monge, M. F. E. (2024). Biological Value of Plant-Based Proteins for Children and Adolescent Development: A Review.
- Axelsson, P., Beermann, T., Hansen, H., et al. (2024). DSOG Guideline Bulletin: Vegetarian and Vegan Diets During Pregnancy. Danish Journal of Obstetrics and Gynecology.
- Pedrosa, L. F. C., Reis, B. Z., de Aquino Morais, S. L. S., et al. (2024). Vitamin D and Metabolic Syndrome.
- Marija, D. I., Velkova, S., Marija, K. I., Elena, S. J., & Sandeva, D. (2025). Acute Pancreatitis as an Uncommon Manifestation of Cystic Fibrosis? A Case Report. PESH Journal.
- Pinnuck, B., Su, W. K., Wilson, W., Pipicella, J., et al. (2025). Iron Deficiency, With or Without Anemia, in Inflammatory Bowel Disease Remains an Undermanaged Issue. Journal of Crohn’s and Colitis.
- Keser, I., Cvijetić, S., Trzija, M., & Ilich, Z. (2024). Assessment of Nutritional Status and Prevalence of Malnutrition in Nursing Home Residents. 9th International Congress of Nutrition.
- Hermann, R., Shovlin, C. L., Kasthuri, R. S., Serra, M., et al. (2025). Hereditary Hemorrhagic Telangiectasia and Gastrointestinal Impacts. Nature Reviews Disease Primers.
- Lemon, P. W. R. (2000). Beyond the Zone: Protein Needs of Active Individuals. Journal of the American College of Nutrition.
- Bilsborough, S., & Mann, N. (2006). A Review of Issues of Dietary Protein Intake in Humans. International Journal of Sport Nutrition and Exercise Metabolism.
- Poortmans, J. R., Carpentier, A., et al. (2012). Protein Turnover, Amino Acid Requirements, and Recommendations for Athletes and Active Populations. Brazilian Journal of Medical and Biological Research.
- Tipton, K. D. (2011). Efficacy and Consequences of Very-High-Protein Diets for Athletes and Exercisers. Proceedings of the Nutrition Society.
- Rosenblum, N., Qubisi, S., & Kwak, J. (2025). KMT2D, a Kabuki Syndrome Disease Gene and Epigenetic Regulator, Functions Within Nephrogenic Cells in a Cell Model of Kidney Disease. Kidney International Reports.
- Suarez, A. A. R., Jühling, F., Moehlin, J., & Others. (2025). Protein Tyrosine Phosphatase Delta is a STAT3-Phosphatase and Suppressor of Metabolic Liver Disease. BMJ Gastroenterology.
- Abdolkhani, D., & Mohammadi, B. (2024). Food Security and Its Challenges in Global Societies.
- Shukla, Y. R., Bhardwaj, R. K., & Shraddha, S. (2024). Underexploited Tropical and Subtropical Vegetable Crops for Diversification and Nutritional Security: A Review. Taylor & Francis.
- Sajic, T. (2025). Next Generation of Omics Analysis to Study Lipid-Rich Tissues. Frontiers in Endocrinology.
- Karras, G. I., Colombo, G., & Kravats, A. N. (2025). Hsp90: Bringing It All Together. Cell Stress and Chaperones.
- Bulut, M., Kıratlı, K., Ali, M. A., Aysin, M., & Ali, A. M. (2025). Lymphadenopathies: A Retrospective Study of Epidemiology, Characteristics, Diagnosis, and Treatment Outcomes of Patients in a Tertiary Hospital in Mogadishu. Infection and Drug Resistance.
- Castaño, B. (2025). DNA Damage Tolerance Pathway Choice: A Decision Orchestrated by Fine-Tuned p53 Levels. University of Ulm.
- Erdemci-Evin, S. (2025). Antiretroviral Function of Primate and Murine PYHIN Proteins and Evasion by HIV-2. University of Ulm.
- Li, J. G., Ying, Y. L., & Long, Y. T. (2025). Aerolysin Nanopore Electrochemistry. Accounts of Chemical Research.
- Oluyemi, G., Fasakin, E., Johnson, O. V., & Adetumbi, O. A. (2024). Digestibility of Non-conventional Protein Sources Blend in African Catfish Using Novel Aquafeed Formulation Software.
- Tosun, A. Ö. (2025). Development of Textile-Based Resistive Pressure Sensing Socks in Diabetes Mellitus for Early Detection of DFU. ITU Repository.
- Alhumaidan, O. A., Alkhunein, S. M., Alakeel, S. A., & Fallata, G. A. (2025). Saudi Healthy Plate-2024: Framework for Developing, Modeling, and Evaluating Saudi Arabia’s Dietary Guidelines.
- Magryś, J., & Bronowicka-Adamska, P. (2025). Impact of Vegan Diet on Pregnancy Outcome. Nutrition Clinique et Métabolisme.
- Fernando, M. G., Castro, C. B., Gardener, S. L., et al. (2025). Baseline Energy and Nutrient Intakes of AU‐ARROW Participants Using a Food Frequency Questionnaire—Preliminary Findings.
- Barkovskaya, I. A., Kruchinin, A. G., & Rozhkova, I. V. (2024). Iodine Deficiency in Russia: Current State of the Problem, Global Practice and New Approaches to Therapy. Food Systems Journal.
- Schönenberger, K. A. (2024). Advances in Medical Nutrition: Strategies and Innovations in Dietetics, Obesity Management, and Nutritional Support. University of Basel.
- León-Guereño, P., Krupa-Kotara, K., et al. (2024). Women’s Health in an Interdisciplinary Dimension—Determinants of Nutritional Disorders. Frontiers in Nutrition.
- Egger, L., Portmann, R., Herrmann, M., & Mehner, E. (2024). A Comparative Nutritional Life Cycle Assessment of Protein-Rich Foods. Wageningen University & Research.
- Borah, D., Kumar, M. N., Mishra, R., & Chutia, M. (2024). Eri Silkworm Pupae: An Alternative Source of Protein in Changing Climate.
- Chimwaza, G., Egbadzor, K. F., & El-Graoui, M. (2024). How Do Neglected and Underutilized Crops (NUCS) in Africa Contribute to Food Security, Nutrition, and Climate Change Outcomes? CABI Digital Library.
- Zhou, Z., Liu, Y., Ishigaki, Y., et al. (2025). Microbial protease supplementation improves gastric emptying and protein digestive fate of beef for the elderly under dynamic in vitro digestion. Food Research International.
- Amin, N., Ahmed, S., & Shah, Z. (2024). Intestinal Protozoa Incidence and Risk Factors in Muhajir Residential ARC-1 & ARC II District Dir Lower. Insights Journal of Health and Research.
- Hassan, M., Bekova, K., & Abdullah, N. (2024). Adherence to Nutritional Supplementation, Follow-Up Care, and Lost to Follow-Up in Post-Bariatric Surgery Patients. Journal of Ayub Medical College.
- Sadhu, S., Barghavi, V., Swain, L., & Gurudeo, S. (2024). Microbial Production of Water-Soluble Vitamins.
- Mukamurera, P. N. (2024). Prevalence and Interconnection of Diabetes and Malnutrition in Rural Uganda.
- Mahara, M. B., Bist, B. S., & Jaisee, L. (2024). Nutritional Status and Its Associated Factors among Elderly Lacto-Vegetarians of Budhanilkantha Municipality of Bagmati Nepal. South Asian Research Journal.
- Krishnan, V. (2024). Millets: Superfood of the Century—Challenges and Opportunities. Frontiers in Nutrition.