Subserosal fibroids, a subtype of uterine fibroids, represent a prevalent yet frequently misunderstood health concern affecting countless women. Despite their widespread occurrence, these benign growths often remain in the shadows of medical awareness. In this comprehensive article, the answer to the question – what is subserosal fibroids, their origins, the diverse symptoms they may provoke, and the broad spectrum of available solutions and treatments will be discussed. This will throw light on the often-overlooked medical condition, empowering women with knowledge and clarity about their health.
What Are These Fibroids?
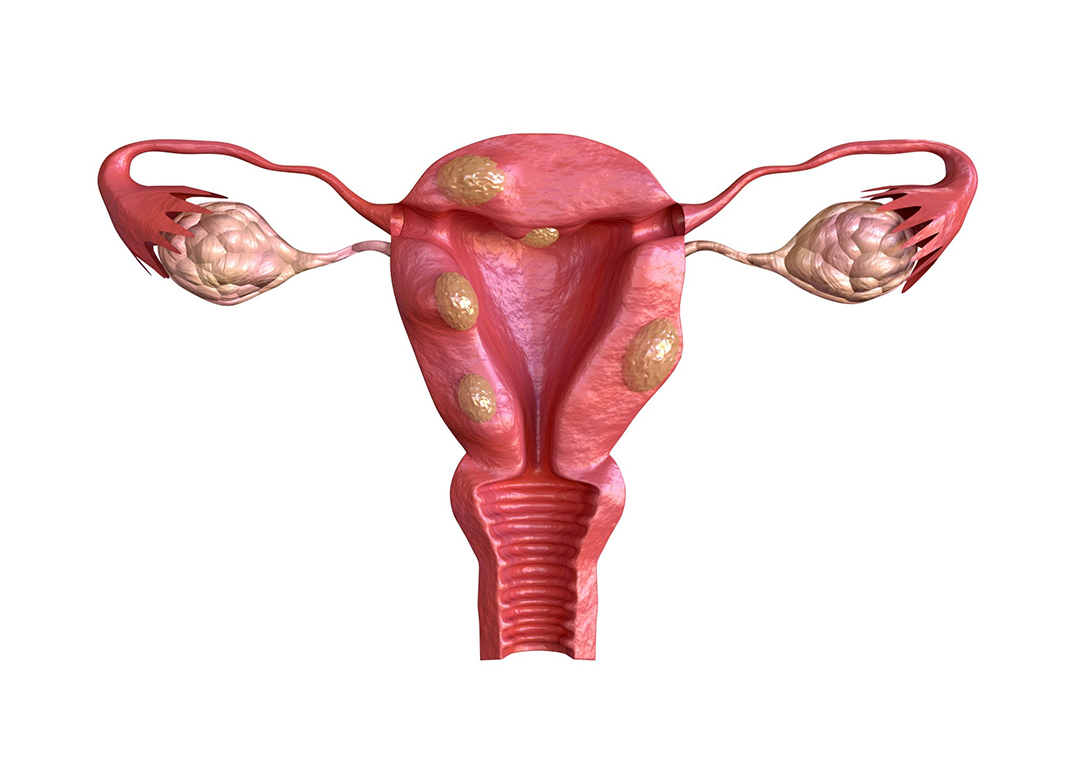
Subserous fibroids are a type of noncancerous growth that originates in the outermost layer of the uterus, medically known as the serosa. These fibroids are distinct from other uterine fibroids in terms of their location and growth pattern. Unlike their counterparts, which develop within the uterine wall or inside the uterine cavity, subserous fibroids project outward, often connecting to the uterus via a stalk-like structure.
The Anatomy of Subserous Fibroids
To gain a deeper understanding of subserous fibroids, it’s essential to explore their anatomy. These fibroids typically start as small, benign tumors that form on the outer surface of the uterus. Over time, they may grow and extend away from the uterine wall. This unique growth pattern sets subserous fibroids apart and influences their impact on a person’s health.
Characteristics and Variations
Subserous fibroids can vary in size, shape, and number. Some may remain relatively small and inconspicuous, while others can grow significantly, leading to noticeable protrusions on the uterine surface. Understanding the different characteristics and variations of subserous fibroids is crucial for healthcare professionals to provide accurate diagnosis and tailored treatment plans.
Common Symptoms and Effects
The presence of subserous fibroids can lead to various symptoms and effects, depending on their size and location. While some individuals with subserous fibroids may remain asymptomatic, others may experience discomfort, pain, or complications. Exploring the common symptoms and potential effects of these fibroids is essential for those seeking medical guidance and management.
Diagnosis and Treatment Options
When faced with the possibility of subserous fibroids, timely diagnosis and appropriate treatment are essential. Healthcare providers employ various diagnostic methods, including imaging techniques, to confirm the presence and characteristics of these growths. Once diagnosed, individuals and their healthcare teams can explore suitable treatment options, which may range from conservative approaches to surgical interventions.
Potential Complications and Considerations
Subserous fibroids, like other types of uterine fibroids, can lead to complications that require careful monitoring and management. Understanding these potential complications and considering the associated risks is vital for individuals with subserous fibroids, as it informs their healthcare decisions and ensures proactive care.
Causes
The exact cause of subserosal fibroids is not fully understood, but several elements are believed to contribute to their development:
Hormonal Influences: Hormones, particularly estrogen and progesterone, play a significant role in the growth. These growths tend to enlarge during the reproductive years when hormone levels are at their most elevated.
Genetics: Family history may also increase the risk of developing. If your mother or sister has had them, you may be more prone to this condition.
Race and Ethnicity: Studies have suggested that African-American women are more likely to develop fibroids, including subserosal fibroids, than women of other racial or ethnic backgrounds.
Recognizing the Symptoms
These fibroids can vary in size, from small, barely noticeable growths to larger masses that can cause significant discomfort. The symptoms associated may include:
- Pelvic Pain and Pressure: Subserosal fibroids can cause pelvic pain or pressure in the lower abdomen.
- Backache: Some women with such fibroids experience lower back pain, which can be persistent and dull.
- Frequent Urination: As these grow, they can press against the bladder, increasing urinary frequency.
- Constipation or Difficulty with Bowel Movements: Large fibroids may exert pressure on the rectum, resulting in constipation or difficulty passing stool.
- Enlarged Abdomen: In some cases, subserosal fibroids can cause the abdomen to appear enlarged or distended.
- Infertility and Pregnancy Complications: While they may not always lead to infertility, they can interfere with fertility and are associated with a higher risk of pregnancy difficulties, such as miscarriage or preterm birth.
Diagnosis
In the event of suspicion regarding these fibroids or the manifestation of associated symptoms, the imperative course of action is to seek a professional medical evaluation. The diagnostic process typically unfolds systematically.
- A thorough physical assessment is conducted by a healthcare provider, focusing on a pelvic assessment to identify any uterine irregularities indicative of subserosal fibroids.
- Subsequently, diagnostic imaging techniques are valuable tools for confirming and localizing these fibroids. Ultrasound, magnetic resonance imaging (MRI), or pelvic computed tomography (CT) scans are often recommended to clearly represent the fibroids’ presence and positioning within the uterine structure.
- In specific scenarios where a more detailed assessment is required, a hysterosalpingography (HSG) procedure may be deemed necessary. This specialized test allows for an evaluation of not only the fibroids but also the uterine cavity’s shape and the condition of the fallopian tubes.
Together, these diagnostic steps form a comprehensive approach to identifying and characterizing these fibroids, enabling healthcare professionals to tailor appropriate treatment strategies based on the findings.
Treatment Options
Treatment options for these fibroids are determined by several factors, including the fibroids’ size and location, symptom severity, and the patient’s age and fertility aspirations. One approach is ‘Watchful Waiting,’ appropriate for smaller fibroids with mild or no symptoms, where healthcare providers advocate routine monitoring without immediate intervention.
Alternatively, ‘Medications’ such as birth control pills or progestin-releasing intrauterine devices (IUDs) may be prescribed to alleviate symptoms like heavy menstrual bleeding and pelvic pain. For more substantial or symptomatic fibroids, ‘Minimally Invasive Procedures’ like uterine artery embolization (UAE) or laparoscopic myomectomy can be employed, effectively removing or reducing fibroids while preserving the uterus.
In more severe cases, mainly when fibroids are large or causing debilitating symptoms, ‘Surgical Removal’ through a hysterectomy may be the recommended course of action. These treatment modalities provide women with various options tailored to their specific circumstances, emphasizing the importance of personalized care in addressing these fibroids.
Conclusion
Subserosal fibroids, while prevalent, can significantly diminish a woman’s quality of life. This article covered points that answer the query – what is subserosal fibroids and give awareness of their causes, early symptom recognition, and exploration of treatment alternatives are pivotal in addressing this condition. Consulting a healthcare provider for an accurate diagnosis and a tailored treatment plan is crucial if you suspect or experience related symptoms. Fortunately, with a well-informed approach, many women can discover effective relief and uphold their reproductive health, even in subserosal fibroids. It is essential to advocate for your well-being, as early intervention can prevent complications and enhance overall health and vitality.

