- Cardiovascular health refers to the optimal functioning of the heart and blood vessels, ensuring effective circulation of blood and oxygen throughout the body.
- Scientific research identifies aerobic, HIIT, and resistance exercises as the most effective methods to improve heart strength, circulation, and overall cardiovascular fitness.
- Consistent exercise reduces the risk of heart disease, lowers blood pressure, improves cholesterol levels, and enhances overall well-being.
 Cardiovascular health refers to the overall health of the heart and blood vessels, including their ability to deliver oxygen and nutrients efficiently throughout the body. Engaging in regular physical activity is one of the most effective ways to enhance cardiovascular health. Aerobic exercises, such as running, swimming, and cycling, are highly beneficial as they improve heart efficiency and reduce risk factors for cardiovascular disease. Resistance training also supports heart health by improving blood pressure and vascular function (1). Emerging research highlights that even light-intensity exercises, like walking, contribute significantly to long-term cardiovascular benefits (2). Additionally, combining aerobic exercise with flexibility and balance routines enhances recovery post-cardiovascular events (3). Recent studies have shown that exercise not only strengthens the heart but also reduces inflammation, further protecting against cardiovascular disease (4). Resistance training, when integrated with aerobic workouts, proves effective in managing conditions such as hypertension and type 2 diabetes, which are closely linked to cardiovascular health (5). Finally, exercise provides unique cardiovascular benefits even in special populations, such as individuals living with HIV (6).
Cardiovascular health refers to the overall health of the heart and blood vessels, including their ability to deliver oxygen and nutrients efficiently throughout the body. Engaging in regular physical activity is one of the most effective ways to enhance cardiovascular health. Aerobic exercises, such as running, swimming, and cycling, are highly beneficial as they improve heart efficiency and reduce risk factors for cardiovascular disease. Resistance training also supports heart health by improving blood pressure and vascular function (1). Emerging research highlights that even light-intensity exercises, like walking, contribute significantly to long-term cardiovascular benefits (2). Additionally, combining aerobic exercise with flexibility and balance routines enhances recovery post-cardiovascular events (3). Recent studies have shown that exercise not only strengthens the heart but also reduces inflammation, further protecting against cardiovascular disease (4). Resistance training, when integrated with aerobic workouts, proves effective in managing conditions such as hypertension and type 2 diabetes, which are closely linked to cardiovascular health (5). Finally, exercise provides unique cardiovascular benefits even in special populations, such as individuals living with HIV (6).
Why Exercise is Crucial for Heart Health
Exercise plays a vital role in maintaining heart health by improving cardiovascular efficiency, lowering blood pressure, and reducing cholesterol levels. Aerobic activities such as walking and running enhance heart function and reduce the risk of heart disease. Resistance training further improves vascular health by reducing arterial stiffness (1). Regular physical activity also minimizes inflammation, a key factor in cardiovascular disease (4). Lastly, exercise significantly reduces mortality risks linked to heart conditions (7).
Best Exercises to Improve Cardiovascular Health
Regular exercise is vital for a healthy heart. Scientific research highlights specific activities that improve cardiovascular health, reduce disease risk, and enhance overall well-being.
 1. Aerobic (Cardio) Exercises
1. Aerobic (Cardio) Exercises
Aerobic exercises like walking, cycling, and swimming improve cardiovascular health by enhancing heart function, reducing blood pressure, and promoting healthy cholesterol levels. Studies confirm regular aerobic activities lower coronary artery disease risks. High-intensity interval training offers superior benefits for cardiac patients (8). Workplace aerobic programs also enhance fitness (9). Elderly individuals benefit greatly from consistent aerobic training. Furthermore, stroke patients achieve improved outcomes through aerobic therapy (10).
2. High-Intensity Interval Training (HIIT)
High-Intensity Interval Training (HIIT) improves cardiovascular health by alternating short bursts of intense activity with rest. Studies show HIIT enhances heart function in coronary artery disease patients (11). It reduces cardiometabolic risks more effectively than continuous training (12). HIIT safely benefits cardiovascular patients. Stroke patients also see improvements. Additionally, low-volume HIIT benefits Type 2 Diabetes patients (13).
3. Resistance Training (Strength Training)
Resistance training enhances cardiovascular health by improving blood pressure, cholesterol levels, and vascular function. Studies show that strength exercises like weightlifting reduce coronary heart disease risks by 23% (14). Combining resistance and endurance training further benefits obese adults (15.). It promotes endothelial health in adolescents (16). Additionally, resistance training improves heart function in chronic heart failure patients.
4. Flexibility and Balance Exercises
Flexibility and balance exercises enhance cardiovascular health by improving posture, reducing blood pressure, and enhancing joint function. Programs combining flexibility and balance training improve cardiovascular fitness in older adults (17). Activities like Tai Chi promote heart health by integrating flexibility and balance (18). Community-based programs improve balance and flexibility in patients with heart disease (19). Additionally, multicomponent training enhances flexibility and reduces hypertension (20). Tai Chi-based flexibility regimens significantly benefit cardiovascular aging (21).
5. Mind-Body Exercises
Mind-body exercises like yoga, Tai Chi, and meditation significantly improve cardiovascular health by reducing arterial stiffness and promoting heart rate variability. Systematic reviews highlight their effectiveness in reducing stress and improving cardiac function in patients with coronary artery disease (22). Tai Chi improves autonomic balance and blood pressure (23). Yoga enhances heart rate variability (24). Meditation programs also reduce stress in cardiac patients (25). Such exercises boost quality of life in heart failure patients (26).
Benefits of Exercise on Cardiovascular Health
Exercise plays a critical role in improving cardiovascular health by strengthening the heart, enhancing circulation, reducing disease risk, and promoting overall well-being through scientific-backed benefits.
 1. Improved Heart Function
1. Improved Heart Function
Regular exercise improves heart function by increasing cardiac output, enhancing oxygen delivery, and strengthening heart muscles. It lowers resting heart rate and boosts stroke volume. Aerobic exercise promotes vascular elasticity (27). Exercise also improves arterial function and reduces atherosclerosis (28). Lifelong exercise patterns significantly lower cardiovascular disease risks (29).
2. Reduce Blood Pressure
Regular exercise significantly reduces blood pressure and enhances cardiovascular health through improved vascular function and reduced arterial stiffness (28). Aerobic and resistance training effectively lower hypertension, contributing to decreased cardiovascular disease risk (30). Studies confirm that moderate physical activity improves overall heart health, especially in high-risk groups (31). Exercise decreases systolic and diastolic pressure even in hypertensive patients (32). Moreover, sustained physical activity improves cardiovascular function and mitigates comorbidities (33).
3. Lowered Cholesterol
Regular exercise is vital for reducing low-density lipoprotein (LDL) cholesterol while enhancing high-density lipoprotein (HDL) levels, effectively lowering cardiovascular disease risks (34). Aerobic and resistance training positively influence lipid profiles and overall vascular health (28). Evidence demonstrates that combining exercise with dietary modifications enhances cholesterol management (35). Additionally, long-term physical activity raises HDL cholesterol, protecting against coronary heart disease (4). Consistent exercise also lowers triglycerides, further benefiting lipid metabolism (36).
4. Reduced Risk of Heart Disease
Regular exercise significantly reduces the risk of heart disease by improving lipid profiles and lowering hypertension (34). Sustained physical activity mitigates cardiovascular mortality and prevents coronary artery disease (31). Additionally, aerobic exercise reduces heart failure risks and promotes vascular health (27). Higher fitness levels correlate with decreased coronary event rates and improved survival (37). Exercise also reduces inflammation and improves endothelial function, preventing atherosclerosis (38).
5. Enhance Vascular Function
Exercise enhances vascular function by improving endothelial health and nitric oxide (NO) production, reducing arterial stiffness, and increasing blood flow (39). Regular physical activity strengthens vascular walls and mitigates cardiovascular risks (40). Aerobic training significantly restores vascular structure, combating hypertension (27). Exercise also improves vascular reactivity, vital for managing coronary artery disease (28). Endothelial adaptation further enhances NO bioavailability for vascular relaxation (41).
6. Improve Blood Sugar Control
Exercise plays a crucial role in improving blood sugar control by enhancing insulin sensitivity and reducing glucose levels, thus lowering cardiovascular risks in diabetic patients (31). Regular physical activity boosts mitochondrial function and cardiovascular health (27). Aerobic training improves glycemic control, reducing dependency on pharmacotherapy (42). Combining exercise with lifestyle adjustments mitigates diabetes-related cardiovascular risks (43). Additionally, exercise aids lipid metabolism, enhancing vascular function (44).
7. Stress Reduction
Exercise reduces stress by improving cardiovascular resilience and lowering stress-induced markers in heart disease patients (45). It promotes relaxation and reduces anxiety through enhanced endorphin production (46). Regular physical activity mitigates the risks of chronic stress, improving overall heart health (47). Cardiovascular fitness programs also enhance self-confidence and mental well-being (34). Finally, stress reduction via exercise lowers inflammation, which benefits vascular health (4).
Evidence-Based Recommendations
Adopting evidence-based strategies is crucial for optimal cardiovascular health. Regular physical activity, such as 150 minutes of weekly aerobic exercise, reduces cardiovascular disease (CVD) risk (48). Consuming a heart-healthy diet emphasizing vegetables, fruits, whole grains, and lean proteins helps manage cholesterol (49). Statin therapy is effective in reducing LDL cholesterol and preventing CVD (50). Monitoring and maintaining blood pressure below 140/90 mmHg is key (51). Smoking cessation significantly lowers the risk of coronary heart disease (52). Stress management through mindfulness and physical activity also mitigates CVD risk (46). Regular risk assessments for cholesterol, blood sugar, and lifestyle factors are essential (53). Following antithrombotic therapy guidelines benefits patients with established coronary artery disease (54). Finally, addressing sedentary lifestyles through structured exercise programs reduces mortality in high-risk groups (47).
Tips for Staying Motivated
Staying motivated for cardiovascular health involves setting achievable goals, tracking progress, enjoying activities, finding support, and focusing on long-term benefits for heart health and overall wellness.
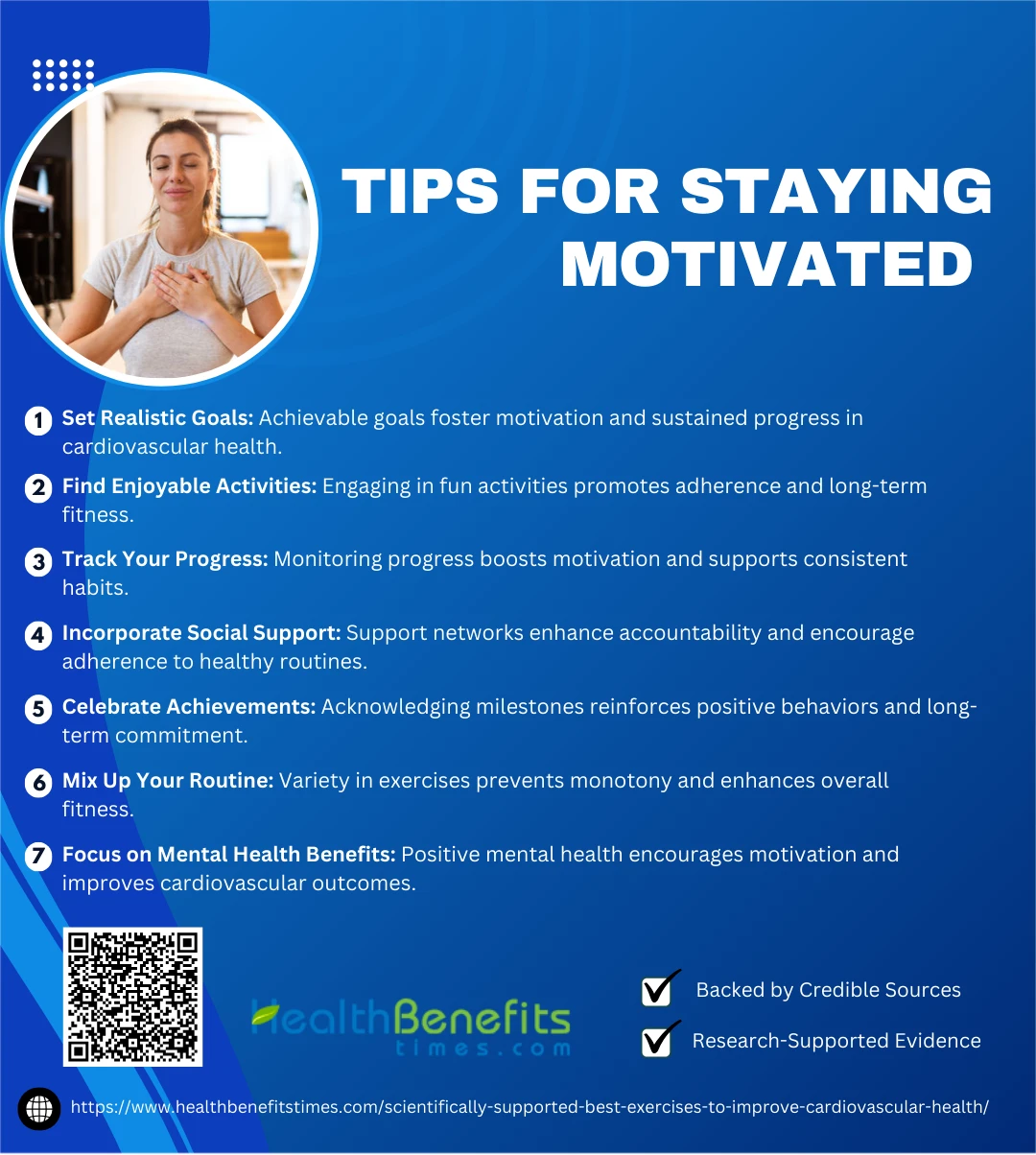 1. Set Realistic Goals
1. Set Realistic Goals
Setting realistic goals is critical for maintaining motivation and achieving cardiovascular health. Personalized goal-setting combined with motivational interviewing fosters sustained behavioral changes (55). Small, achievable milestones increase self-efficacy and adherence to healthy practices (56). SMART goals, which are specific, measurable, achievable, relevant, and time-bound, significantly enhance cardiovascular health outcomes (57). A structured approach emphasizing realistic progress fosters better engagement (58). Regularly reassessing goals ensures alignment with personal capacity and lifestyle (59).
2. Find Enjoyable Activities
Engaging in enjoyable physical activities is vital for sustaining motivation and improving cardiovascular health. Activities such as dancing, hiking, or sports help increase participation and adherence to fitness routines (60). Personalized options like exergaming enhance engagement and reduce monotony (61). Incorporating outdoor adventures further boosts intrinsic motivation and cardio benefits (62). Structured programs tailored to preferences ensure long-term consistency (63). Regular physical education fosters satisfaction and fitness, supporting sustained efforts (64).
3. Track Your Progress
Tracking progress is essential for maintaining motivation in cardiovascular health. Utilizing wearable devices and apps helps individuals monitor physical activity, heart rate, and overall progress (65). Self-monitoring improves adherence to fitness routines and health outcomes (66). Visual feedback on goals encourages sustained motivation (67). Personalized feedback fosters autonomy and engagement (68). Effective tools like pedometers enhance adherence in cardiac rehabilitation programs (69).
4. Incorporate Social Support
Incorporating social support is essential for staying motivated to improve cardiovascular health. Group exercise programs enhance accountability and foster a sense of community (70). Communication approaches that involve family and friends boost adherence to healthy habits (71). Social support predicts long-term physical activity adherence among cardiac patients (72). Support networks also enhance motivation by reinforcing self-efficacy (63). The ENRICHD study highlights improved outcomes when emotional support is provided post-myocardial infarction (73).
5. Celebrate Achievements
Celebrating achievements plays a critical role in maintaining motivation for cardiovascular health. Acknowledging small wins reinforces positive behaviors and promotes consistency in healthy habits (74). Marking milestones boosts self-efficacy and inspires perseverance (75). Recognizing progress fosters emotional resilience, supporting long-term adherence to healthy practices (76). Integrating celebrations within health programs enhances overall success (77). This approach aligns with evidence-based strategies for improving cardiovascular outcomes (78).
6. Mix Up Your Routine
Mixing up your routine is crucial for maintaining motivation and improving cardiovascular health. Incorporating diverse activities like resistance training and aerobic exercises prevents monotony and enhances engagement (79). Alternating routines helps target different muscle groups, ensuring holistic fitness (80). Diversifying exercises keeps workouts enjoyable and reduces the risk of plateaus (81). Additionally, combining motivational strategies ensures consistent participation (82). Regular variety fosters sustainable fitness habits for long-term cardiovascular benefits (83).
7. Focus on Mental Health Benefits
Focusing on mental health benefits can significantly motivate individuals to maintain cardiovascular health. Positive psychological well-being improves heart health by reducing stress and promoting healthy behaviors (84). Emotional well-being plays a crucial role in enhancing adherence to lifestyle changes, such as exercise (63). Self-determination boosts both mental and physical health through intrinsic motivation (85). Addressing depression can also improve cardiovascular outcomes (86). Promoting positive well-being reduces CVD risk and enhances long-term motivation (87).
Myths and misconceptions
- Myth: Only Intense Workouts Are Effective
Many believe that only high-intensity workouts, such as running or cycling at a fast pace, are beneficial for cardiovascular health. However, moderate-intensity exercises, such as brisk walking or gardening, can provide similar benefits. These activities help lower blood pressure and improve heart function without overwhelming the body. - Myth: Cardio Alone Is Sufficient
While aerobic exercises like jogging are vital, neglecting strength training is a common misconception. Resistance training not only builds muscle but also reduces fat, lowers cholesterol, and improves arterial stiffness, all of which enhance cardiovascular health. Combining both aerobic and strength exercises offers the most comprehensive benefits. - Myth: Exercise Can Weaken Your Immune System
The idea that regular exercise suppresses immunity is outdated. Research shows that moderate exercise enhances immune function and reduces the risk of cardiovascular disease. It boosts circulation, allowing immune cells to travel more efficiently throughout the body. - Myth: More Exercise Means Better Results
Some people think that exercising excessively leads to faster or better results. However, overtraining can cause physical fatigue, mental burnout, and even adverse effects on heart health, such as increased arterial stiffness. A balanced approach with rest days is crucial to avoid injuries and ensure consistent progress. - Myth: Spot Reduction Works
The belief that exercises targeting specific body areas (like sit-ups for belly fat) can reduce fat in those areas is widespread but untrue. Cardiovascular exercises, combined with a healthy diet, promote overall fat loss. The heart benefits from reduced overall fat mass, improving circulation and reducing strain.
Conclusion
Incorporating scientifically supported exercises like aerobic workouts, HIIT, resistance training, and stress-relieving activities into your routine can significantly improve cardiovascular health. These exercises enhance heart strength, circulation, and overall well-being while reducing the risk of chronic diseases. By staying consistent and tailoring your fitness plan to your abilities, you can enjoy long-term benefits for your heart and quality of life. Take the first step today and prioritize your cardiovascular health for a healthier future.
References:
- RJ Shephard et al.
- MFH Maessen et al.
- CM Perez-Terzic
- C Fiuza-Luces et al.
- KJ Stewart
- C Ozemek et al.
- Perez-Terzic
- Rognmo, Ø., et al. (2004). High-intensity aerobic interval exercise. European Journal of Preventive Cardiology.
- Korshøj, M., et al. (2015). Worksite aerobic exercise. JSTOR.
- Pang, M.Y.C., et al. (2013). Aerobic exercise in stroke. Karger.
- Karlsen, T., et al. (2017). High-intensity interval training for maximizing health outcomes. ScienceDirect.
- Hussain, S.R., et al. (2016). HIIT vs continuous training for CVD prevention. Cardiology in Review.
- Way, K.L., et al. (2020). Low-volume HIIT benefits in diabetes. ScienceDirect.
- Liu, Y., et al. (2019). Resistance exercise and cardiovascular health. NCBI.
- Schjerve, I.E., et al. (2008). Combined training in obese adults. Portland Press.
- Yu, C.C.W., et al. (2016). Endothelial health in adolescents. NCBI.
- Seco, J., et al. (2013). Long-term activity and cardiovascular fitness. LWW Journals.
- Heckman, G.A., et al. (2008). Tai Chi and cardiovascular aging. LWW Journals.
- Segev, D., et al. (2019). Balance training in heart disease patients. Oxford Academic.
- Sobrinho, A.C.S., et al. (2023). Multicomponent training for cardiovascular health. Frontiers in Physiology.
- Taunton, J.E., et al. (1996). Tai Chi’s effect on aging. Karger Journals.
- Duan, F., et al. (2021). Mind-body exercises for coronary heart disease. MD Journals.
- Cai, L., et al. (2021). Tai Chi and cardiovascular benefits. ScienceDirect.
- Zou, L., et al. (2018). Yoga and heart rate variability. MDPI.
- Younge, J.O., et al. (2015). Meditation in cardiac disease. Oxford Academic.
- Shi, F., et al. (2024). Mind-body exercise impact on heart failure. ScienceDirect.
- Pinckard, K., et al. (2019). Aerobic exercise effects on cardiovascular health. Frontiers in Cardiovascular Medicine.
- Nystoriak, M.A., et al. (2018). Cardiovascular benefits of exercise. Frontiers in Cardiovascular Medicine.
- Maessen, M.F.H., et al. (2016). Lifelong exercise and cardiovascular health. ScienceDirect.
- Lavie, C. J., Stewart, M., & Ozemek, C. (2020). Benefits of exercise training on blood pressure.
- Agarwal, S. K. (2012). Cardiovascular benefits of exercise.
- Fagard, R. H., & Cornelissen, V. A. (2007). Effect of exercise on blood pressure.
- Sharman, J. E., & La Gerche, A. (2015). Exercise and cardiovascular risk.
- Myers, J. (2003). Exercise and cardiovascular health.
- Stefanick, M. L., Mackey, S., & Sheehan, M. (1998). Effects of diet and exercise on HDL cholesterol.
- Mann, S., Beedie, C., & Jimenez, A. (2014). Differential effects of exercise on cholesterol.
- Morris, C. K., & Froelicher, V. F. (1993). Cardiovascular benefits of improved exercise capacity.
- Paffenbarger Jr., R. S., & Hyde, R. T. (1984). Exercise in the prevention of coronary heart disease.
- Green, D. J., & Smith, K. J. (2018). Effects of exercise on vascular function, structure, and health in humans.
- Golbidi, S., & Laher, I. (2012). Exercise and the cardiovascular system.
- Yung, L. M., et al. (2009). Exercise, vascular wall, and cardiovascular diseases.
- Gulve, E. A. (2008). Exercise and glycemic control in diabetes.
- Pavlović, R., Solaković, S., & Simeonov, A. (2022). Physical activity in the prevention of diabetes and cardiovascular disorders.
- Colberg, S. R., Sigal, R. J., Yardley, J. E., & Riddell, M. C. (2016). Physical activity/exercise and diabetes.
- Popovic, D., et al. (2022). Defining the importance of stress reduction in managing cardiovascular disease.
- Blumenthal, J. A., et al. (2005). Effects of exercise and stress management training on cardiovascular risk markers.
- Franklin, B. A., et al. (2021). Chronic stress, exercise, and cardiovascular disease.
- Zachariah, G., & Alex, A. G. (2017). Exercise for prevention of cardiovascular disease.
- Mosca, L., et al. (2004). Evidence-based guidelines for cardiovascular disease prevention.
- McAlister, F. A., et al. (2007). Recommendations in evidence-based guidelines.
- Thomas, S. G., & Goodman, J. M. (2011). Physical activity clearance for cardiovascular risk.
- Ferket, B. S., et al. (2010). Cardiovascular risk assessment.
- Pearson, T. (2015). Risk assessments for cardiovascular health.
- Vandvik, P. O., et al. (2012). Antithrombotic therapy in coronary artery disease.
- Swoboda, C. M., et al. (2016). Setting single or multiple goals for cardiovascular health.
- Xu, L., et al. (2023). Motivational skills in cardiovascular prevention.
- White, N. D., et al. (2013). SMART goals for cardiovascular risk reduction.
- Kris-Etherton, P. M., et al. (2021). Strategies for promoting cardiovascular health.
- Fleury, J., & Sedikides, C. (2007). Wellness motivation in cardiac rehabilitation.
- Marcus, B. H., & Pekmezi, D. (2024). Motivating people to be physically active.
- Cacciata, M. C., et al. (2022). Facilitators and challenges to exergaming.
- Mackenzie, S. H., et al. (2018). Using outdoor adventure to enhance physical activity.
- Breeman, L. D., et al. (2025). Motivation for lifestyle changes in cardiac rehabilitation.
- Gao, Z. (2009). Motivation and engagement in physical education.
- Salvi, D., et al. (2018). An m-Health system for education and motivation in cardiac rehabilitation.
- Mayo, N. L., et al. (2022). Implementation of a self-determination based clinical program.
- Dennison, C. R., & Hughes, S. (2011). Motivating patients to adopt healthy lifestyles.
- Williamson, T. M., et al. (2021). Behavioral counseling for cardiovascular health.
- Rosneck, J., & Waechter, D. (2006). Exercise motivation: Pedometer use in cardiac rehabilitation.
- Clayton, C., Motley, C., & Sakakibara, B. (2019). Enhancing social support among people with cardiovascular disease.
- Duffy, E. Y., et al. (2021). Communication approaches to enhance cardiovascular health.
- Teleki, S., et al. (2022). Role of social support in physical activity for heart patients.
- Writing Committee for the ENRICHD Investigators (2003). Social support post-myocardial infarction.
- Kumar, D. R. S. (2023). The Power of Self-Care.
- Bradford, T. W., & Grier, S. A. (2017). Virtual support communities and motivation.
- Feeney, B. C., & Collins, N. L. (2015). A theoretical perspective on thriving through relationships.
- Spahn, J. M., et al. (2010). Behavioral change strategies in nutrition counseling.
- Rosamond, W., & American Heart Association. (2022). Life’s essential 8.
- Williams, M. A., et al. (2007). Resistance exercise in cardiovascular health.
- O’Donovan, G., et al. (2010). The ABC of Physical Activity for Health.
- Kashyap, N. (2023). The Power of Aerobic Exercises.
- Milne, S., et al. (2002). Promoting exercise using Protection Motivation Theory.
- Artinian, N. T., et al. (2010). Interventions for cardiovascular risk reduction.
- Boehm, J. K., & Kubzansky, L. D. (2012). Positive well-being and cardiovascular health.
- Sheldon, K. M., et al. (2008). Self-determination theory in physical and mental health.
- Elderon, L., & Whooley, M. A. (2013). Depression and cardiovascular disease.
- Sin, N. L. (2016). Positive well-being and CVD prevention.

