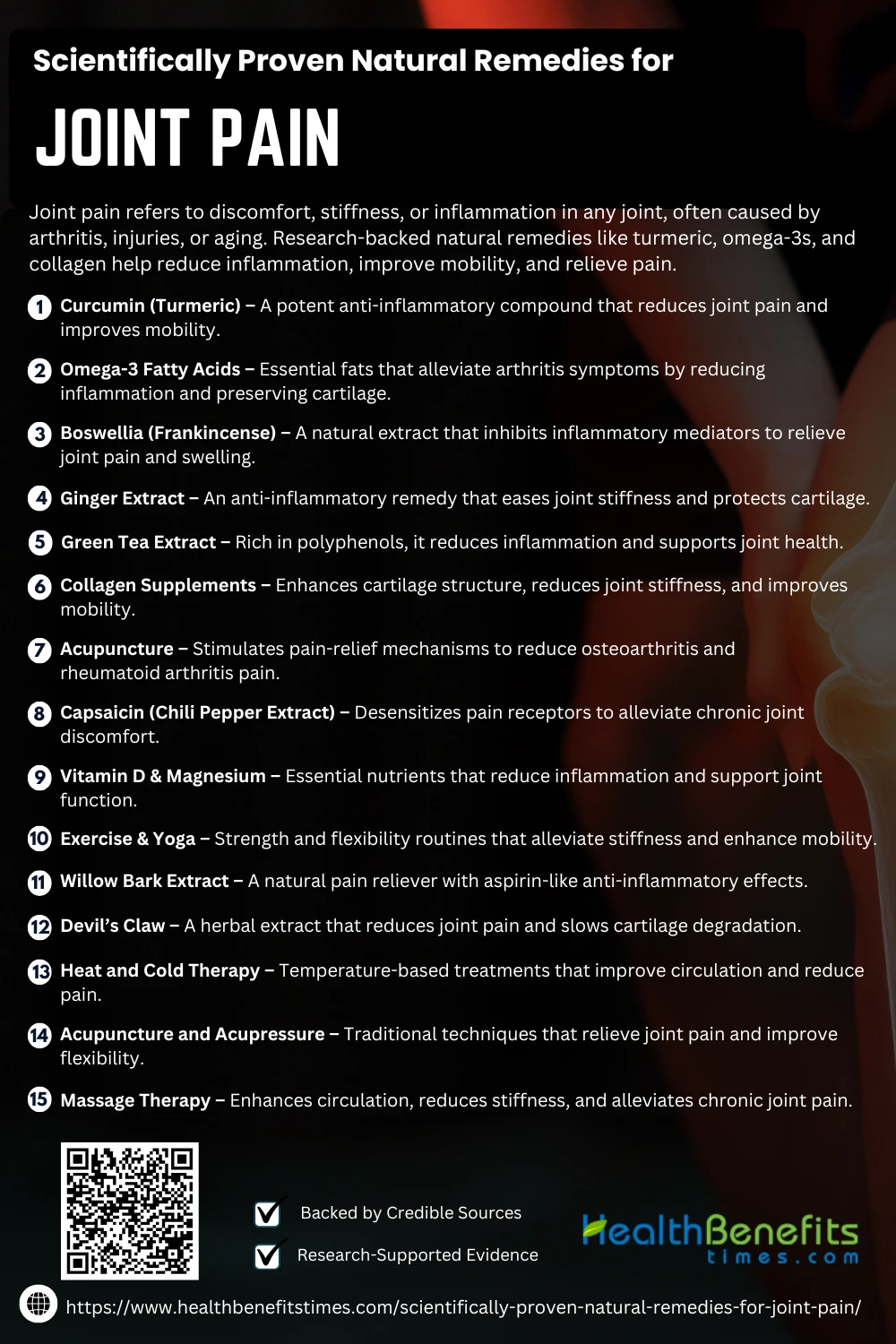
- Joint pain refers to discomfort, stiffness, or inflammation in any joint, often caused by arthritis, injuries, or aging.
- Research-backed natural remedies like turmeric, omega-3s, and collagen help reduce inflammation, improve mobility, and relieve pain.
- Lifestyle changes, including an anti-inflammatory diet, weight management, and regular exercise, enhance the effectiveness of natural treatments for long-term joint health.
 Joint pain is a common condition characterized by discomfort, inflammation, or stiffness in one or more joints, often resulting from arthritis, injury, or wear and tear over time. Millions of people worldwide experience joint pain, affecting mobility, daily activities, and overall quality of life. While conventional treatments such as non-steroidal anti-inflammatory drugs (NSAIDs) and corticosteroids provide temporary relief, they often come with significant side effects. Consequently, scientific research has increasingly focused on natural remedies that offer effective and safer alternatives. Studies have shown that omega-3 fatty acids from fish oil can reduce joint stiffness and inflammation, making them a viable dietary intervention. Similarly, curcumin, the active compound in turmeric, has demonstrated anti-inflammatory properties comparable to NSAIDs in clinical trials.
Joint pain is a common condition characterized by discomfort, inflammation, or stiffness in one or more joints, often resulting from arthritis, injury, or wear and tear over time. Millions of people worldwide experience joint pain, affecting mobility, daily activities, and overall quality of life. While conventional treatments such as non-steroidal anti-inflammatory drugs (NSAIDs) and corticosteroids provide temporary relief, they often come with significant side effects. Consequently, scientific research has increasingly focused on natural remedies that offer effective and safer alternatives. Studies have shown that omega-3 fatty acids from fish oil can reduce joint stiffness and inflammation, making them a viable dietary intervention. Similarly, curcumin, the active compound in turmeric, has demonstrated anti-inflammatory properties comparable to NSAIDs in clinical trials.
In addition to dietary interventions, herbal therapies such as Boswellia and willow bark extract have been studied for their pain-relieving effects, particularly in arthritis management. Furthermore, physical therapies, including acupuncture and massage, have been found to improve joint flexibility and reduce pain severity in osteoarthritis patients. Complementary treatments like collagen supplementation have also gained traction due to their role in cartilage regeneration and joint health. The integration of lifestyle modifications, such as weight management and structured exercise routines, has been widely endorsed by healthcare professionals to reduce joint stress and enhance mobility. Moreover, emerging research suggests that polyunsaturated fatty acids (PUFAs) can act as potent anti-inflammatory agents, aiding in the long-term management of joint disorders. With ongoing scientific advancements, natural remedies continue to gain recognition as effective adjuncts or alternatives to conventional joint pain treatments, paving the way for a more holistic and sustainable approach to musculoskeletal health.
Scientifically Proven Natural Remedies for Joint pain
Joint pain affects millions, often due to arthritis, aging, or inflammation. Fortunately, science-backed natural remedies like turmeric, omega-3s, and collagen offer relief. Discover proven, effective solutions to ease discomfort and improve mobility.
1. Curcumin (Turmeric)
Curcumin, the active compound in turmeric, has been widely studied for its anti-inflammatory properties and effectiveness in relieving joint pain. Clinical trials have shown that curcumin supplementation significantly reduces osteoarthritis symptoms, comparable to NSAIDs but without harmful side effects. (1) Research indicates that curcumin mitigates inflammation by inhibiting pro-inflammatory cytokines and oxidative stress. (2) Moreover, curcumin’s efficacy in managing rheumatoid arthritis and psoriatic arthritis has been confirmed in various studies. (3) Recent advancements in bioavailable curcumin formulations have improved its absorption, enhancing its therapeutic potential. (4) Additionally, turmeric combined with Boswellia extract has shown synergistic benefits in musculoskeletal pain relief. (5)
2. Omega-3 Fatty Acids
Omega-3 fatty acids, particularly EPA and DHA, have been extensively researched for their role in reducing joint inflammation and stiffness. Studies confirm that omega-3 intake alleviates arthritis symptoms by inhibiting inflammatory pathways and cytokine production. (6) Clinical findings suggest that flaxseed-derived alpha-linolenic acid (ALA) also supports joint health and improves mobility in arthritis patients. (7) Furthermore, omega-3 supplementation has been associated with decreased osteoarthritis progression and enhanced cartilage preservation. (8) Research on polyunsaturated fatty acids (PUFAs) has highlighted their role in modulating inflammatory responses in rheumatoid arthritis. (9) Additionally, Mediterranean diets rich in omega-3 sources like fish and nuts have been linked to improved joint function and reduced pain severity. (10)
3. Boswellia (Frankincense)
Boswellia, also known as frankincense, has been recognized for its potent anti-inflammatory properties, particularly in joint pain management. Research indicates that Boswellia serrata extract effectively reduces pain and swelling associated with osteoarthritis and rheumatoid arthritis by inhibiting inflammatory mediators such as leukotrienes. (11) Clinical studies show that long-term Boswellia supplementation improves joint function and mobility. (5) Moreover, its combination with turmeric enhances its efficacy in reducing musculoskeletal pain. (12) Evidence suggests that Boswellia is particularly beneficial for athletes suffering from high-impact joint pain. ({% https://eastmeetswest.com/tumeric-and-frankincense/?noamp=available trusted %}) Additionally, studies confirm its role in accelerating post-exercise recovery by reducing soreness and stiffness. (11)
4. Ginger Extract
Ginger extract has been widely studied for its anti-inflammatory and analgesic properties in joint pain relief. Clinical trials demonstrate that ginger supplementation reduces pain and stiffness in osteoarthritis patients by modulating inflammatory pathways. (13) Additionally, ginger compress therapy has been shown to alleviate chronic joint pain and improve mobility. (14) Studies highlight the effectiveness of ginger in combination with other anti-arthritic herbs, such as turmeric and clove, for enhanced relief. (15) Furthermore, evidence suggests that ginger extract not only reduces joint inflammation but also protects cartilage from degradation. (16) In a placebo-controlled clinical trial, steamed ginger extract demonstrated significant pain reduction in osteoarthritis patients. (13)
5. Green Tea Extract
Green tea extract, rich in polyphenols like epigallocatechin gallate (EGCG), has been found to reduce inflammation and slow the progression of joint diseases. Research shows that EGCG inhibits pro-inflammatory cytokines, alleviating pain in arthritis patients. (17) Studies indicate that green tea polyphenols can prevent cartilage degradation and promote joint health. (18) Additionally, a clinical trial highlighted the effectiveness of green tea extract in reducing oxidative stress and joint pain. (19) Athletes using green tea extract reported improved mobility and reduced post-exercise joint stiffness. (20) Further research suggests that a diet rich in green tea compounds may lower the risk of joint-related surgeries. (21)
6. Collagen Supplements
Collagen supplements play a crucial role in maintaining joint health by improving cartilage structure and reducing pain. Studies show that hydrolyzed collagen supplementation enhances joint flexibility and reduces osteoarthritis symptoms. (22) Clinical trials have confirmed that collagen peptides support cartilage regeneration and reduce inflammation in arthritis patients. (23) Athletes taking collagen supplements have reported significant improvements in knee function and post-exercise recovery. (24) Research also highlights the combined benefits of type II collagen and Boswellia serrata in reducing joint stiffness and pain. (25) Moreover, collagen supplementation has been linked to enhanced joint mobility and reduced inflammation in long-term osteoarthritis management. (26)
7. Acupuncture
Acupuncture has been extensively studied for its ability to reduce joint pain and improve mobility by stimulating the body’s natural pain-relief mechanisms. Clinical trials show that acupuncture alleviates osteoarthritis pain and enhances joint function by modulating inflammatory pathways. (27) Studies confirm that acupuncture therapy significantly reduces knee pain severity and stiffness in elderly patients. (28) Additionally, research highlights the effectiveness of acupuncture in managing polyarthritis by integrating traditional techniques with naturopathy. (29) A randomized controlled trial further demonstrated acupuncture’s ability to modulate brain activity and pain perception in knee osteoarthritis patients. (30) Moreover, acupuncture has been recommended as an alternative therapy for osteoarthritis-related pain relief and improved joint flexibility. (31)
8. Capsaicin (Chili Pepper Extract)
Capsaicin, the active compound in chili peppers, has been widely studied for its analgesic properties in managing joint pain. Research shows that capsaicin inhibits pain signals by desensitizing nerve receptors, making it an effective treatment for osteoarthritis and rheumatoid arthritis. (32) Clinical studies confirm that topical capsaicin application significantly reduces chronic joint pain and stiffness. (33) Additionally, capsaicin-containing creams have been shown to improve joint function and reduce inflammation in arthritis patients. (34) Research also suggests that dietary intake of capsaicin-rich foods may help regulate inflammation and pain sensitivity. (33) Furthermore, studies indicate that combining capsaicin with other natural anti-inflammatory compounds enhances its pain-relieving effects. (33)
9. Vitamin D & Magnesium
Vitamin D and magnesium play essential roles in maintaining joint health and reducing inflammation. Studies confirm that vitamin D deficiency is linked to increased joint pain and cartilage degradation, making supplementation crucial for osteoarthritis management. (35) Research also highlights the role of magnesium in improving calcium absorption and preventing joint stiffness. (36) A clinical trial demonstrated that vitamin D and magnesium together help reduce inflammatory markers in rheumatoid arthritis patients. (37) Additionally, studies suggest that magnesium supplementation improves joint mobility and muscle function in older adults. (38) Furthermore, research supports the combined use of these nutrients to prevent osteoporosis and joint degeneration. (39)
10. Exercise & Yoga
Exercise and yoga have been extensively researched for their benefits in joint pain relief and mobility enhancement. Clinical studies indicate that a combination of strength training and flexibility exercises can reduce joint stiffness and improve function in arthritis patients. (40) Yoga has been shown to reduce pain severity and inflammation by improving joint flexibility and reducing stress hormones. (41) Research further supports that yoga therapy enhances mobility and muscle strength, contributing to better pain management. (42) A systematic review suggests that targeted exercise programs can significantly decrease joint pain and improve quality of life in rheumatoid arthritis patients. (43) Additionally, yoga combined with breathing exercises has been found to regulate inflammatory markers, aiding in long-term joint health. (44)
11. Willow bark Extract
Willow bark extract has been traditionally used for pain relief and is now scientifically validated for joint health benefits. Research confirms that its active component, salicin, functions similarly to aspirin in reducing inflammation and relieving arthritis-related pain. (45) Clinical studies have demonstrated that willow bark significantly alleviates osteoarthritis symptoms, including pain and stiffness, when compared to placebo treatments. (46) Additionally, long-term use of willow bark extract has been associated with improved joint mobility and reduced inflammation without the gastrointestinal side effects of NSAIDs. (47) A randomized trial also found that combining willow bark with other anti-inflammatory herbs enhances its efficacy in managing chronic joint pain.
12. Devil’s claw
Devil’s Claw, a herbal extract derived from Harpagophytum procumbens, has been extensively studied for its potent anti-inflammatory and analgesic effects in joint pain management. Research shows that Devil’s Claw significantly reduces pain and stiffness in osteoarthritis and rheumatoid arthritis by inhibiting inflammatory enzymes. (48) Clinical studies confirm its effectiveness in improving joint mobility and flexibility in arthritis patients. (45) A systematic review highlights its role in reducing the need for conventional painkillers by providing comparable relief with fewer side effects. (49) Moreover, Devil’s Claw has been found to slow cartilage degradation, making it a valuable natural therapy for degenerative joint diseases. (50) Additionally, research suggests that combining Devil’s Claw with other herbal anti-inflammatories enhances its therapeutic potential for long-term joint health. (49)
13. Heat and Cold Therapy
Heat and cold therapy are well-researched methods for alleviating joint pain by reducing inflammation and improving circulation. Clinical studies confirm that heat therapy relaxes muscles and enhances blood flow, relieving stiffness in osteoarthritis patients. (51) Cold therapy, on the other hand, reduces swelling and numbs nerve endings, effectively managing acute joint pain (Huang, 2024). Research highlights that alternating hot and cold treatments significantly improves pain tolerance and joint function in arthritis sufferers. (52) A study suggests that combining heat therapy with exercise can enhance joint flexibility and mobility. (53) Additionally, research supports the use of contrast therapy (hot and cold applications) for improved circulation and long-term pain management. (54)
14. Acupuncture and Acupressure
Acupuncture and acupressure have been extensively studied for their ability to alleviate joint pain by stimulating specific pressure points and enhancing energy flow. Research shows that acupuncture significantly reduces osteoarthritis pain by modulating inflammatory responses and increasing endorphin release. (55) Clinical trials confirm that acupressure helps in relieving joint stiffness and improving mobility in arthritis patients. (56) A systematic review suggests that acupuncture is particularly effective in post-operative knee rehabilitation, reducing swelling and pain. (57) Studies also highlight that auricular acupressure can enhance traditional pain management techniques by providing long-term relief. (57) Furthermore, research indicates that combining acupuncture with herbal medicine improves overall treatment outcomes for joint pain sufferers. (55)
15. Massage Therapy
Massage therapy has been widely recognized for its effectiveness in reducing joint pain and improving mobility. Research shows that regular massage sessions help decrease inflammation and muscle stiffness in arthritis patients. (58) Clinical studies confirm that massage therapy enhances circulation and reduces pain perception in osteoarthritis patients. (53) Additionally, a systematic review found that deep tissue massage effectively relieves chronic joint pain and improves flexibility. (59) Research also suggests that combining massage therapy with heat therapy may provide enhanced pain relief and muscle relaxation. (60) Furthermore, studies indicate that neuromuscular massage techniques play a crucial role in alleviating joint stress and stiffness. (61)
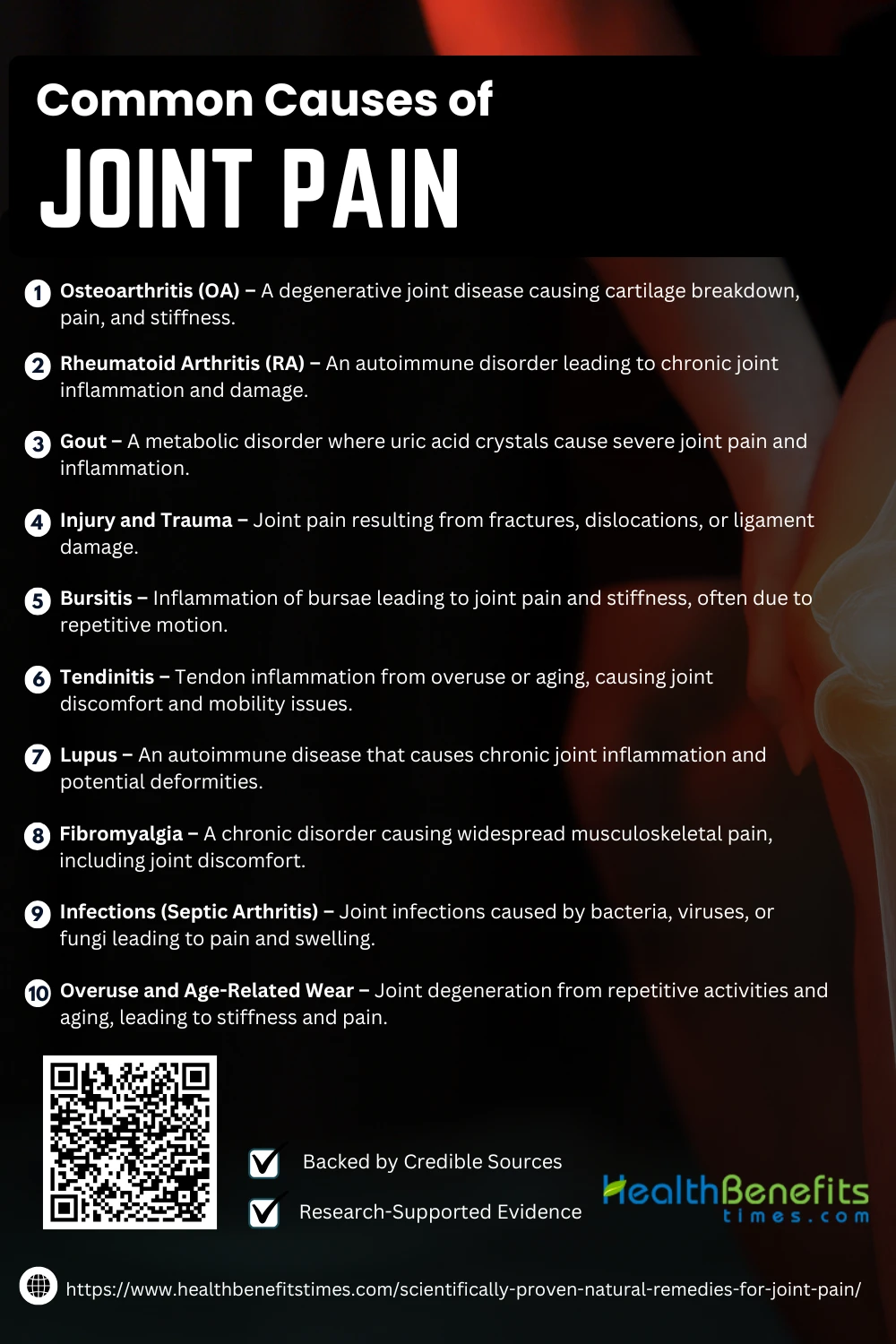
Common Causes of Joint Pain
Joint pain is a widespread issue caused by arthritis, injuries, aging, and inflammation. Factors like autoimmune diseases, overuse, and infections also contribute. Understanding these causes helps in managing and preventing discomfort effectively.
1. Osteoarthritis (OA)
Osteoarthritis (OA) is a degenerative joint disease characterized by cartilage breakdown, leading to pain, stiffness, and reduced mobility. Studies confirm that OA is the most common cause of chronic joint pain, affecting millions worldwide. (62) Research highlights the progressive nature of OA, with inflammation and joint deformities worsening over time. (63) Additionally, innovative therapies such as regenerative medicine are being explored to alleviate OA-related pain and improve joint function. (64)
2. Rheumatoid Arthritis (RA)
Rheumatoid arthritis (RA) is a chronic autoimmune disorder that primarily affects synovial joints, causing inflammation, pain, and long-term joint damage. Research indicates that RA is associated with persistent joint swelling and systemic complications. (65) Studies highlight that RA impairs proprioception and postural control, increasing fall risk among patients. (66) Additionally, recent advancements in polymer hydrogel therapies offer promising treatments to manage RA-induced pain and inflammation. (67)
3. Gout
Gout is a metabolic disorder caused by excess uric acid accumulation, leading to crystal formation in the joints, which triggers severe pain and inflammation. Research highlights that gout primarily affects the lower limbs, causing recurring flare-ups and joint degeneration. (68) Studies show that monosodium urate (MSU) crystals in synovial fluid are responsible for the characteristic swelling and stiffness. (69) Additionally, early diagnosis of gout through radiological markers can help in effective treatment and prevention of joint deformities. (70)
4. Injury and Trauma
Injury and trauma, including fractures, dislocations, and ligament tears, are major causes of joint pain and long-term mobility issues. Studies confirm that untreated anterior cruciate ligament (ACL) injuries accelerate joint degeneration and increase the risk of osteoarthritis. (71) Chronic inflammation after joint injuries often results in persistent knee pain and post-traumatic arthritis. (72) Additionally, misdiagnosed joint dislocations can lead to severe pain and long-term complications. (73)
5. Bursitis
Bursitis is a condition characterized by inflammation of the bursae, small fluid-filled sacs that cushion joints, leading to pain and stiffness. Research indicates that subacromial-subdeltoid bursitis is a common cause of shoulder pain, particularly in individuals with repetitive motion injuries. (74) Studies show that bursitis can result from infections, with periprosthetic joint infections affecting the shoulder bursae. (75) Additionally, research highlights a link between bursitis and conditions like gout, further exacerbating joint pain. (76)
6. Tendinitis
Tendinitis, the inflammation of tendons, is a leading cause of joint pain, often resulting from repetitive stress or aging. Studies confirm that Achilles tendinitis and tendinopathy contribute to knee osteoarthritis and reduced mobility in older adults. (77) Research suggests that tendinitis can be confused with other joint disorders, requiring precise clinical differentiation for effective treatment. (78) Additionally, evidence shows that supraspinatus tendinitis leads to chronic shoulder pain, significantly impacting joint function. (79)
7. Lupus
Lupus, an autoimmune disease, leads to chronic joint inflammation and musculoskeletal pain. Studies show that lupus-related joint pain can result in irreversible bone erosion and joint deformities. (80) Research confirms that lupus-induced arthritis often mimics rheumatoid arthritis, causing swelling and stiffness. (81) Additionally, studies highlight that juvenile lupus can lead to early-onset joint damage and long-term disability. (82)
8. Fibromyalgia
Fibromyalgia is a chronic disorder that causes widespread musculoskeletal pain, including joint discomfort. Research indicates that fibromyalgia is linked to microRNA dysregulation, which may contribute to increased pain sensitivity. Studies confirm that fibromyalgia coexists with other musculoskeletal diseases, worsening joint pain and disability. (83) Furthermore, research highlights that fibromyalgia often overlaps with inflammatory joint diseases, making diagnosis and treatment more complex. (84)
9. Infections (Septic Arthritis)
Septic arthritis is a severe joint infection caused by bacterial, viral, or fungal pathogens, leading to acute pain, swelling, and cartilage destruction. Research highlights that Haemophilus influenzae and Staphylococcus aureus are among the primary culprits of septic arthritis. ({% https://link.springer.com/article/10.1007/s11606-025-09362-4 trusted %}) Clinical reports confirm that untreated septic arthritis can lead to joint deformities and disability. (85) Additionally, postpartum septic arthritis has been identified as a rare but serious condition requiring immediate intervention. (86)
10. Overuse and Age-Related Wear
Overuse and age-related wear contribute to joint pain by accelerating cartilage degradation and inflammation. Studies indicate that mechanical stress from repetitive activities leads to early-onset osteoarthritis. (87) Research highlights that age-related biochemical changes impair joint lubrication, increasing friction and pain. ({% trusted %}) Furthermore, studies confirm that aging chondrocytes lose their regenerative ability, making joint damage irreversible. (88)
Differentiate between Conventional Treatments vs. Natural Remedies for joint pain
| Aspect | Conventional Treatments | Natural Remedies |
| Definition | Medical interventions involving pharmaceuticals and surgical procedures to manage joint pain. | Holistic approaches using dietary changes, supplements, herbs, and physical therapies to alleviate joint pain naturally. |
| Examples | NSAIDs (e.g., ibuprofen, naproxen), corticosteroids, disease-modifying anti-rheumatic drugs (DMARDs), physical therapy, joint replacement surgery. | Omega-3 fatty acids, turmeric (curcumin), ginger, Boswellia, acupuncture, yoga, heat & cold therapy, and collagen supplements. |
| Mechanism of Action | Targets inflammation and pain by blocking chemical pathways responsible for swelling and discomfort. | Works by reducing inflammation, improving joint lubrication, and strengthening cartilage through nutrition and lifestyle changes. |
| Effectiveness | Provides fast and potent relief but may require long-term use and professional supervision. | Often slower in onset but offers sustained relief and fewer long-term complications. |
| Side Effects & Risks | Potential gastrointestinal issues (ulcers, bleeding), cardiovascular risks, kidney damage, dependency (opioids), and surgical complications. | Generally safer, but may cause mild digestive issues or allergic reactions in sensitive individuals. |
| Cost | Prescription medications and surgeries can be expensive, requiring insurance coverage or long-term expenses. | More affordable in the long run, though quality supplements and therapies may have upfront costs. |
| Long-Term Impact | May alleviate symptoms but does not always address the root cause; chronic use can lead to organ damage. | Focuses on overall joint health, aiming to slow disease progression and enhance mobility. |
| Sustainability | Requires continued medication or interventions, which may lead to dependency. | Encourages a lifestyle-based approach, promoting self-care and preventative measures. |
| Suitability | Ideal for severe pain, advanced arthritis, or cases requiring immediate relief or surgical intervention. | Best suited for mild to moderate joint pain, prevention, and complementary therapy alongside medical treatment. |
Conclusion
Managing joint pain naturally is possible with scientifically proven remedies like curcumin, omega-3 fatty acids, collagen, and anti-inflammatory herbs. Research supports their effectiveness in reducing inflammation, improving mobility, and alleviating discomfort. Additionally, lifestyle changes, including a nutrient-rich diet, regular exercise, and weight management, enhance joint health. While these natural solutions provide significant relief, consulting a healthcare professional ensures the best approach for individual needs. Combining multiple remedies can offer long-term benefits for joint pain management.