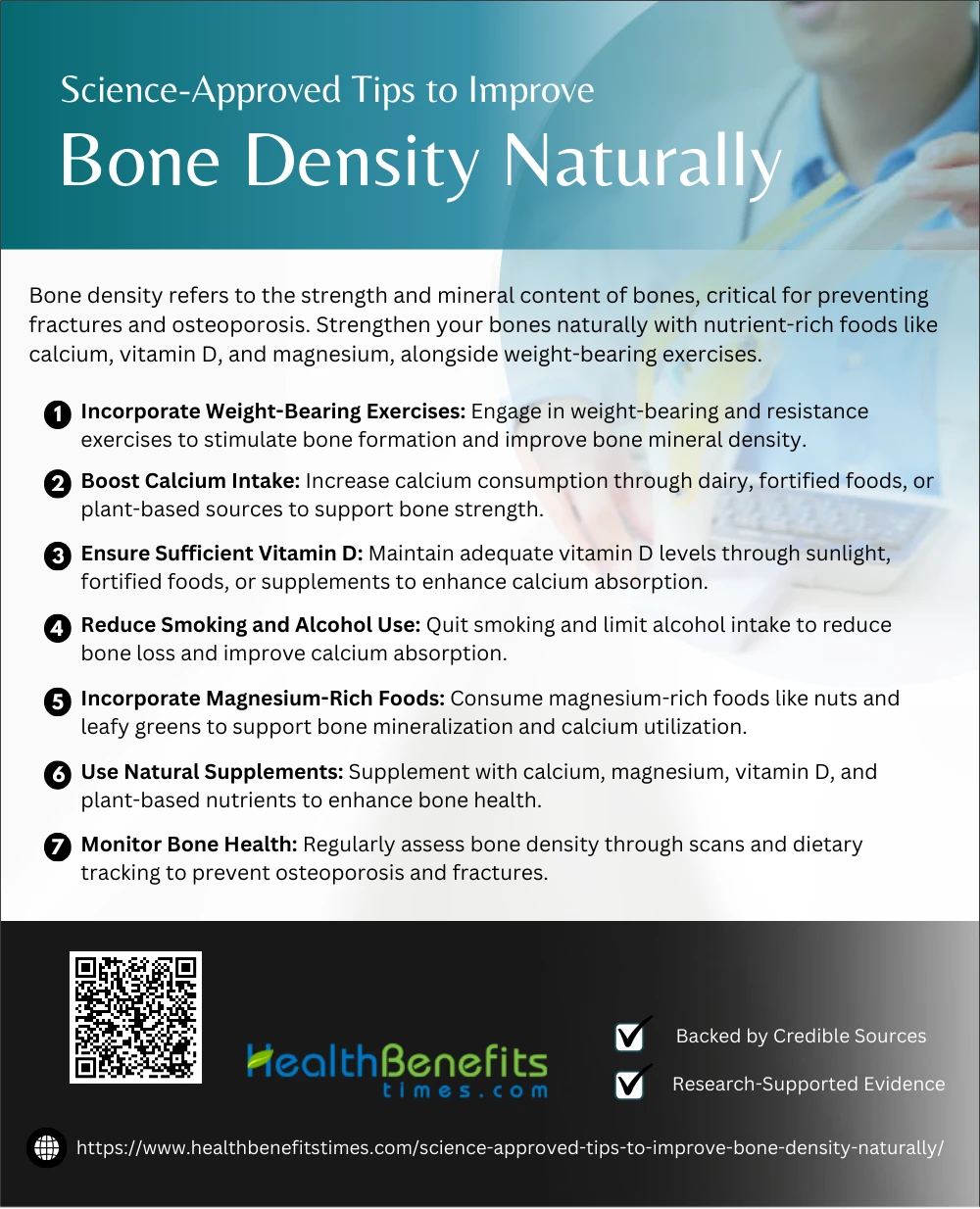
- Bone density refers to the strength and mineral content of bones, critical for preventing fractures and osteoporosis.
- Strengthen your bones naturally with nutrient-rich foods like calcium, vitamin D, and magnesium, alongside weight-bearing exercises.
- Adopt science-backed lifestyle changes, including reducing alcohol, quitting smoking, and maintaining a healthy weight, to improve bone health effectively.
 Bone density refers to the amount of bone mineral in bone tissue, serving as an indicator of bone strength and health (1). Improving bone density naturally involves adopting lifestyle and dietary practices that enhance bone health while preventing conditions like osteoporosis. Regular weight-bearing exercises such as walking or resistance training have been shown to significantly increase bone mass and reduce fracture risk (2). Consuming foods rich in calcium, magnesium, and vitamin D, like leafy greens and fortified products, promotes optimal bone mineralization (3). Additionally, natural supplements such as resveratrol and omega-3 fatty acids can boost bone strength by enhancing bone microstructure and reducing inflammation (4). Incorporating balance and flexibility exercises further reduces fall-related risks, safeguarding against bone injuries (2). Avoiding bone-depleting habits, like excessive alcohol consumption and smoking, also plays a crucial role (5).
Bone density refers to the amount of bone mineral in bone tissue, serving as an indicator of bone strength and health (1). Improving bone density naturally involves adopting lifestyle and dietary practices that enhance bone health while preventing conditions like osteoporosis. Regular weight-bearing exercises such as walking or resistance training have been shown to significantly increase bone mass and reduce fracture risk (2). Consuming foods rich in calcium, magnesium, and vitamin D, like leafy greens and fortified products, promotes optimal bone mineralization (3). Additionally, natural supplements such as resveratrol and omega-3 fatty acids can boost bone strength by enhancing bone microstructure and reducing inflammation (4). Incorporating balance and flexibility exercises further reduces fall-related risks, safeguarding against bone injuries (2). Avoiding bone-depleting habits, like excessive alcohol consumption and smoking, also plays a crucial role (5).
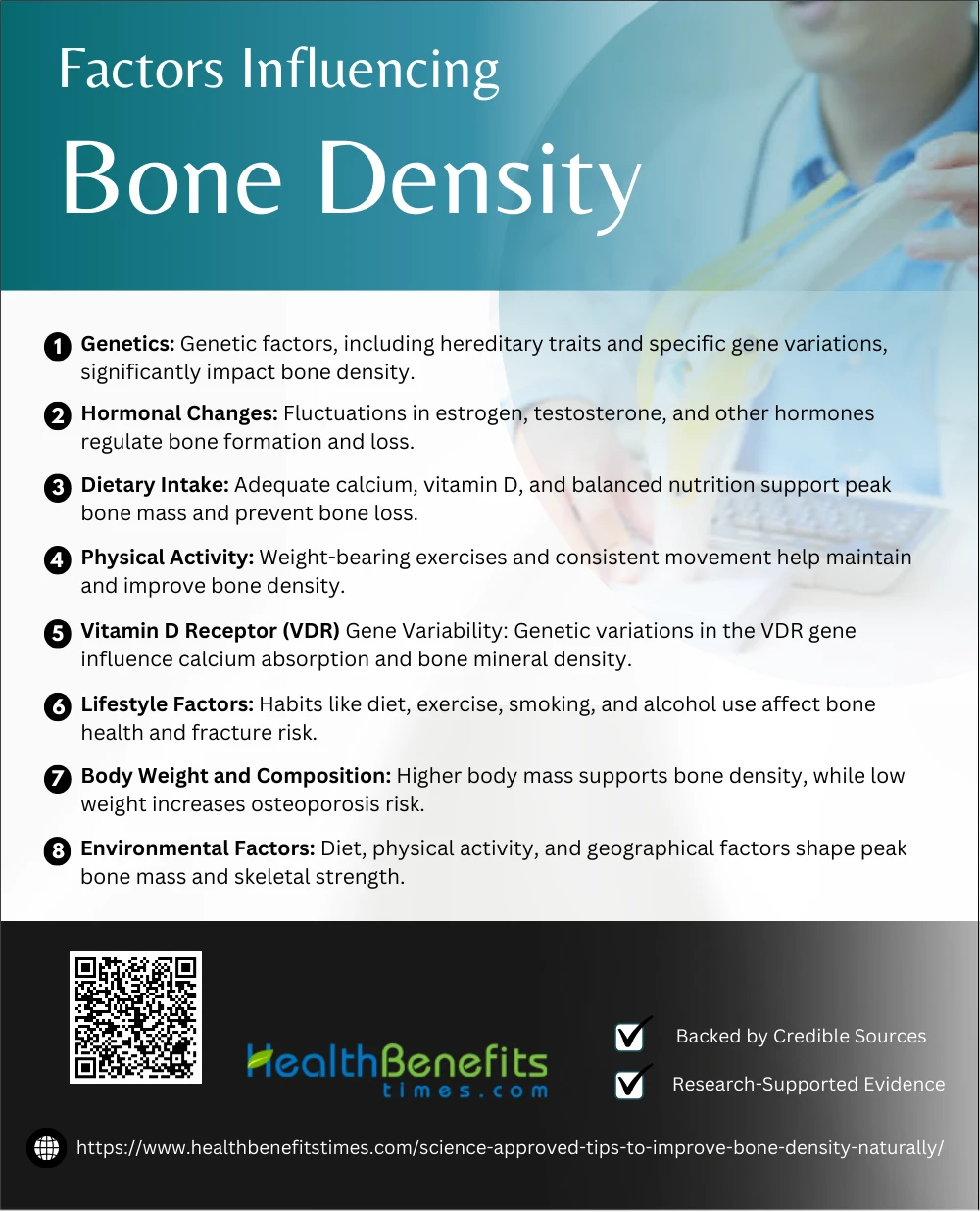
Factors Influencing Bone Density
Bone density is shaped by multiple factors, including age, genetics, nutrition, and lifestyle. Understanding these influences empowers you to take proactive steps for healthier, stronger bones.
1. Genetics
Genetics plays a pivotal role in determining bone density, with up to 85% of its variance attributed to hereditary factors (6). Specific genes, like the Vitamin D Receptor (VDR) gene, significantly influence bone mineral density (7). Family history of osteoporosis highlights genetic predisposition (8). Additionally, genetic factors influence peak bone mass during growth (9). Emerging research underscores polygenic interactions affecting bone health (10).
2. Hormonal Changes
Hormonal changes are a critical factor in bone density regulation. Estrogen plays a protective role, especially during menopause, where its decline accelerates bone loss (11). Lactation also temporarily decreases bone mineral density (12). Hormonal contraceptives may influence bone density through prolonged use (13). Testosterone has anabolic effects, enhancing bone strength in both genders (14).
3. Dietary Intake
Dietary intake significantly impacts bone density, with calcium and vitamin D being essential nutrients. Adequate calcium intake supports peak bone mass, particularly in young adults, as highlighted by 15. Environmental factors, including diet, also play a role in bone health, as noted by 6. Proper nutrition mitigates aging-related bone loss, per 16. Women’s adherence to dietary calcium recommendations improves bone mineral density (17). Nutritional factors profoundly influence bone metabolism (18).
4. Physical Activity
Physical activity is crucial for maintaining bone density, as regular exercise helps achieve peak bone mass and reduces bone loss. Physical activity’s role in bone health extends across ages, impacting men (19) and elderly women (20). It also interacts with genetic factors in determining bone mass (6). Moreover, consistent activity supports bone health in children (21).
5. Vitamin D Receptor (VDR) Gene Variability
Vitamin D receptor (VDR) gene variability significantly influences bone density, with specific polymorphisms linked to variations in bone mineral density (22). Allelic variations in the VDR gene can predict calcium absorption and bone health (23). Studies indicate VDR polymorphisms account for up to 75% of bone density variation (24). Meta-analyses reveal these genetic markers’ role in osteoporosis (25). The association is evident in girls’ growth and bone density (26).
6. Lifestyle Factors
Lifestyle factors such as diet, physical activity, and smoking significantly affect bone density. High calcium intake and regular weight-bearing exercises promote bone health (27). Conversely, smoking and alcohol consumption negatively impact bone mineral density (28). Young adults’ bone health depends on lifestyle choices like exercise and calcium intake (29). Adolescents benefit from lifestyle interventions (30), while gender-specific behaviors influence fracture risk (31).
7. Body Weight and Composition
Body weight and composition are critical determinants of bone density, with higher body mass correlating to increased bone mineral density (6). Fat mass contributes to skeletal health through mechanical loading (32). Low body weight, however, is associated with reduced bone density (33). Body composition affects bone health in both the elderly (34) and children (21).
8. Environmental Factors
Environmental factors significantly impact bone density, influencing peak bone mass development and maintenance. Factors like dietary calcium and physical activity play vital roles (35). Environmental variations, including demographic and ethnic characteristics, also contribute to differences in bone health (36). Mechanical forces and activity levels shape bone adaptation (37). Hereditary and environmental interactions influence bone formation (38), and studies confirm familial environmental impacts (39).
Science-Approved Tips to Improve Bone Density Naturally
Boosting bone density naturally is essential for long-term health. Discover science-backed strategies, from nutrition to exercise, to strengthen your bones and prevent future complications.
1. Incorporate Weight-Bearing Exercises
Incorporating weight-bearing exercises is a proven method to improve bone density. Activities like walking and resistance training stimulate bone formation (40). Exercises targeting major muscle groups enhance skeletal strength (41). High-intensity routines can further optimize bone mineral density (42). Resistance exercises, particularly in postmenopausal women, are especially beneficial (43). Even low-impact activities like mall walking can boost bone health significantly.
2. Boost Calcium Intake
Boosting calcium intake is essential for bone health, as it supports bone mineralization and reduces the risk of osteoporosis. Consuming dairy or fortified alternatives is highly effective (44). Calcium retention during growth significantly impacts bone density (45). Pairing calcium-rich foods with vitamin D enhances absorption (46). Even plant-based diets can provide adequate calcium (47). Balanced intake is critical for skeletal health (48).
3. Ensure Sufficient Vitamin D
Ensuring sufficient vitamin D is vital for bone density, as it enhances calcium absorption and bone mineralization (49). Vitamin D reduces bone loss in the elderly (50). Regular sun exposure boosts vitamin D levels (51). Fortified foods are critical in combating vitamin D deficiency (52). Subclinical vitamin D deficiency impacts bone health (53). Supplementation is often necessary for optimal levels (54).
4. Reduce Smoking and Alcohol Use
Reducing smoking and alcohol use significantly improves bone density by minimizing oxidative stress and preserving calcium absorption. Smoking is linked to increased bone resorption (55). Alcohol disrupts bone metabolism and impairs osteoblast function (56). Both habits increase the risk of osteoporosis (43). Quitting smoking reverses bone damage (57). Avoiding alcohol preserves skeletal strength (44). Healthy habits ensure long-term bone health (58).
5. Incorporate Magnesium-Rich Foods
Incorporating magnesium-rich foods like nuts, seeds, and leafy greens enhances bone density by supporting calcium absorption and bone mineralization. Magnesium influences bone health through its role in activating vitamin D (59). It also contributes to improved bone quality by regulating parathyroid hormone levels and reducing bone turnover. Consistent intake of magnesium, coupled with calcium, ensures better skeletal strength and resilience over time.
6. Use Natural supplements
Natural supplements like calcium, magnesium, and vitamin D significantly enhance bone density by improving mineral absorption and bone strength (44). Pomegranate seed oil supports anti-inflammatory pathways critical to bone health (60). Vitamin D supplementation boosts bone density, especially in deficient individuals (46). Enzymes like phytase aid nutrient utilization (61). Plant-based diets offer natural supplement alternatives for skeletal health (47). Antioxidants in pumpkin seeds protect bone tissues (45).
7. Monitor Bone Health
Monitoring bone health is critical for preventing fractures and osteoporosis. Regular bone density scans effectively track changes in bone mass (62). Vibration therapy assessments support bone strength improvement (40). Monitoring calcium and vitamin D intake ensures adequate bone support (46). Natural supplements, like nanohydroxyapatite, are measurable options (63). Weight-bearing exercises tracked with performance metrics benefit bone density (42). Long-term clinical assessments are crucial for overall bone health (64).
Myths and Misconceptions
- Drinking Milk Alone is Enough
- Many people believe consuming milk is all it takes to maintain healthy bones. While milk is a great source of calcium, bone health requires a combination of nutrients, including vitamin D, magnesium, and phosphorus. A diverse diet including leafy greens, nuts, seeds, and fortified foods is essential for building and maintaining bone density.
- Bone Loss is Only a Concern for Older Adults
- Bone density starts to decline in your 30s. This misconception often leads younger individuals to neglect bone health, missing the critical window for building peak bone mass. Habits like proper nutrition and regular exercise early in life can prevent issues like osteoporosis later on.
- Exercise Doesn’t Impact Bone Health
- This myth undermines the role of physical activity in strengthening bones. Weight-bearing exercises (e.g., walking, jogging, dancing) and resistance training stimulate bone remodeling, making them denser and more resilient. Without exercise, bones can weaken, regardless of diet.
- Supplements Can Replace a Healthy Diet
- While calcium and vitamin D supplements can be helpful, they are no substitute for a nutrient-rich diet. Whole foods provide synergistic nutrients that supplements lack, such as fiber, antioxidants, and trace minerals, which are crucial for overall health, including bones.
- Once You Lose Bone Density, It Can’t Be Rebuilt
- Bone remodeling is an ongoing process throughout life. While it’s easier to build bone mass earlier in life, proper care—including exercise, diet, and sometimes medication—can help regain and maintain bone density even after loss.
- Only Women Need to Worry About Osteoporosis
- Women are indeed at a higher risk due to hormonal changes after menopause, but men are not immune. Men over 50 are still at significant risk, particularly if they have poor nutrition, are sedentary, or have a family history of osteoporosis.
- Calcium-Fortified Foods are Always Beneficial
- Not all fortified foods provide bioavailable calcium, meaning the body may not absorb it effectively. Additionally, consuming excessive calcium without balancing it with other nutrients like magnesium can lead to issues like kidney stones or calcification of arteries.
- High Protein Diets Harm Bones
- It was once believed that high protein intake caused calcium loss through urine, weakening bones. Research now shows that protein is essential for bone health as it supports muscle strength and bone structure. The key is moderation and a balanced intake of calcium alongside protein.
- Vitamin D is Only Important in Winter
- Vitamin D helps the body absorb calcium, and its importance isn’t limited to any specific season. While sunlight is a natural source, many people have vitamin D deficiencies year-round due to limited sun exposure or inadequate intake through food. Consistent attention to vitamin D is necessary.
- Medications are the Only Solution for Bone Loss
- Although medications can treat severe osteoporosis, they aren’t the only option. Prevention and management through diet, exercise, and lifestyle changes are effective and often sufficient for many people. Medications should be a last resort or used in combination with lifestyle modifications.
Conclusion
Improving bone density naturally is a lifelong commitment to better health, but it doesn’t have to be overwhelming. By adopting science-backed strategies like a nutrient-rich diet, regular weight-bearing exercises, and healthy lifestyle habits, you can strengthen your bones and reduce the risk of fractures and osteoporosis. Small, consistent changes make a significant difference over time, proving that prevention is both simple and effective. Prioritize your bone health today to ensure a more active and resilient future.
References:
- Zeng et al., 2024 – “Bone aging and osteoporosis: recent evidence focusing on plant-based natural products.”
- Herlocker, HealthyCell – “Why Do People Lose Bone Density and Strength As They Age?”
- Kelly et al., 2024 – “Bones Plant-Based Nutrition Plan and Cookbook.”
- Stengler, 2009 – “Improve bone density: try natural supplements and strategies.”
- Simpson, 2014 – “Dr. Lani’s No-nonsense Bone Health Guide.”
- Jouanny et al., 1995
- Jakubowska-Pietkiewicz et al., 2012
- Stevenson et al., 1989
- Seeman & Tsalamandris, 1993
- Fujita et al., 1999
- Rannevik et al., 1995
- Kalkwarf, 1999
- Berenson et al., 2004
- Prakasam et al., 1999
- Fehily AM, Coles RJ, Evans WD, Elwood PC. (1992). Factors affecting bone density in young adults. Link.
- Tucker KL. (2003). Dietary intake and bone status with aging.
- French MR, Vernace-Inserra F. (2008). Adherence to calcium intake recommendations.
- New SA. (1995). Nutritional factors and bone metabolism.
- Atalar E, Aydin G, Keles I, et al. (2009). Factors affecting bone mineral density in men.
- Amiri AM, Hosseini SR. (2015). Relationship between bone mineral density and physical activity level in the elderly.
- Ausili E, Rigante D, Salvaggio E, et al. (2012). Determinants of bone mineral density, bone mineral content, and body composition in children.
- Klich I, Fendler W, Chlebna-Sokół D. (2012). Vitamin D receptor gene variability in pediatric bone health.
- Gong G, Stern HS, Cheng SC, et al. (1999). Bone mineral density and VDR gene polymorphisms.
- Vandevyver C, Wylin T, Cassiman JJ. (1997). VDR gene alleles’ influence on bone density.
- Cooper GS, Umbach DM. (1996). Meta-analysis of VDR polymorphisms and bone density.
- Tao C, Yu T, Garnett S, et al. (1998). VDR alleles predict growth and bone density in girls.
- Mohammadi F, Hamid TA, Yazid MN, Othman Z. (2011). Lifestyle factors influencing bone mineral density.
- Krall EA, Dawson-Hughes B. (1993). Heritable and lifestyle determinants of bone density.
- Hammad LF, Benajiba N. (2017). Lifestyle and bone health in young adults.
- Okayama T, Kinouchi K, Watanabe H. (2021). Lifestyle factors in adolescent bone mass.
- Nieves JW. (2021). Impact of lifestyle factors on bone density and fractures.
- Reid IR. (2002). Relationships among body mass and bone density.
- Shapses SA, Cifuentes M. (2015). Effects of body weight/composition on bone health.
- Blain H, Vuillemin A, Teissier A, et al. (2001). Muscle strength, body weight, and bone density in older women.
- Baudoin C, Cohen-Solal ME. (2002). Genetic and environmental factors affect bone density variances.
- Avdagić S, Barić I, Keser I, Rumbak I. (2012). Influence of heredity and environment on peak bone density.
- Gkiatas I, Lykissas M, Kostas-Agnantis I. (2015). Mechanical forces influencing bone growth.
- Seeman E, Hopper JL. (1997). Genetic and environmental components of bone density variance.
- Magarey AM, Boulton TJC, Chatterton BE. (1999). Familial and environmental influences on bone growth.
- Annino G. (2009). Vibration energy and neuromuscular assessment.
- Okorokov D. (2012). Quadriceps strength and landing kinematics.
- Zielińska P, Soroko-Dubrovina M, Dudek K. (2023). High-intensity laser therapy and muscle tone.
- Owens BB. (2004). Postmenopausal walking programs for bone density.
- Onyeike EN. (2012). Food, Nutrition, and Toxicology.
- Auti KS. (2024). Development of Milkshake Blended with Pumpkin Seed.
- Bollman L. (2008). Cholecalciferol Supplementation in Hemodialysis Subjects.
- Mansouri F, Shateri Z, Jahromi SE. (2024). Pro-Vegetarian Diet and Bone Health.
- Ahmed N. (2017). Clinical Biochemistry.
- Ahmadieh H, Arabi A. (2011). Vitamins and bone health: beyond calcium and vitamin D.
- Bonjour JP, Guéguen L, Palacios C. (2009). Minerals and vitamins in bone health.
- Holick MF. (2006). Role of vitamin D in fracture prevention.
- Laird E, Ward M, McSorley E. (2010). Vitamin D and bone health.
- Shearer MJ. (1997). Roles of vitamins D and K in osteoporosis prevention.
- Shinchuk L, Holick MF. (2007). Vitamin D and rehabilitation.
- Ghazanfarpour M, Najafi MN, Sharghi NB. (2018). Fennel and menopausal symptoms.
- Taheri E, Pourhoseingholi MA, Moslem A. (2022). Alcohol and bone metabolism.
- Halldorson M. (2013). Smoking cessation and healing.
- Markussen RA. (2014). Policy and habits affecting bone health.
- Foley DC. (1978). Magnesium and bone health mechanisms.
- Khajebishak Y, Payahoo L, Hamishehkar H. (2019). Pomegranate seed oil and bone health.
- Zhang BZ. (1999). Phytase enzymes for nutrient optimization.
- Uklejewski R, Winiecki M, Patalas A. (2024). Micro-CT assessment of bone density.
- Sarfi S, Azaryan E, Hanafi-Bojd MY. (2024). Nanohydroxyapatite applications in bone health.
- Ahmed N. (2017). Clinical biochemistry for bone monitoring.