- Intermittent fasting is an eating pattern that alternates between periods of eating and fasting to support metabolic health.
- It improves blood sugar regulation by enhancing insulin sensitivity and reducing insulin resistance.
- Fasting triggers the body to utilize stored energy, stabilizing glucose levels and reducing inflammation linked to metabolic disorders.
 Intermittent fasting (IF) is an eating pattern that alternates between periods of fasting and eating, offering flexibility in timing without focusing on specific food restrictions (1). The growing interest in intermittent fasting is due to its profound impact on blood sugar regulation. Research shows that IF improves insulin sensitivity, lowers fasting glucose levels, and reduces fluctuations in blood sugar throughout the day (2; 3). Additionally, fasting promotes metabolic flexibility, helping the body transition efficiently between glucose and fat as energy sources (4). Studies further reveal that IF induces hormonal changes, such as increased growth hormone and reduced insulin-like growth factor 1, that contribute to better glucose homeostasis (5). Together, these mechanisms suggest that intermittent fasting is a promising non-pharmacological strategy for managing and potentially preventing diabetes (6).
Intermittent fasting (IF) is an eating pattern that alternates between periods of fasting and eating, offering flexibility in timing without focusing on specific food restrictions (1). The growing interest in intermittent fasting is due to its profound impact on blood sugar regulation. Research shows that IF improves insulin sensitivity, lowers fasting glucose levels, and reduces fluctuations in blood sugar throughout the day (2; 3). Additionally, fasting promotes metabolic flexibility, helping the body transition efficiently between glucose and fat as energy sources (4). Studies further reveal that IF induces hormonal changes, such as increased growth hormone and reduced insulin-like growth factor 1, that contribute to better glucose homeostasis (5). Together, these mechanisms suggest that intermittent fasting is a promising non-pharmacological strategy for managing and potentially preventing diabetes (6).
Understanding Blood Sugar Regulation
Blood sugar regulation is a critical physiological process governed by complex hormonal interactions involving insulin and glucagon, primarily produced by the pancreas. Insulin facilitates the uptake of glucose into cells, reducing blood sugar levels, while glucagon triggers glucose release from the liver to prevent hypoglycemia (7). Dysregulation of this system can result in metabolic disorders like diabetes, where insulin function is impaired, leading to persistent hyperglycemia (8). The enzyme glucokinase plays a pivotal role in glucose metabolism by acting as a glucose sensor in pancreatic β-cells (9). Environmental and lifestyle factors, including diet and exercise, significantly influence blood sugar regulation by modulating insulin sensitivity and cellular glucose uptake (10). Recent studies emphasize the integration of metabolic and behavioral factors in understanding and managing blood sugar levels effectively (11).
How does intermittent fasting regulate blood sugar levels?
Intermittent fasting (IF) has gained significant attention for its potential health benefits, including its ability to regulate blood sugar levels. By alternating periods of eating and fasting, IF influences the body’s insulin response, promotes better energy usage, and enhances overall metabolic health. Understanding how these processes work can shed light on why IF is a powerful tool for managing blood sugar, improving insulin sensitivity, and reducing the risk of conditions like diabetes. This article explores the science behind IF and its impact on blood sugar regulation.
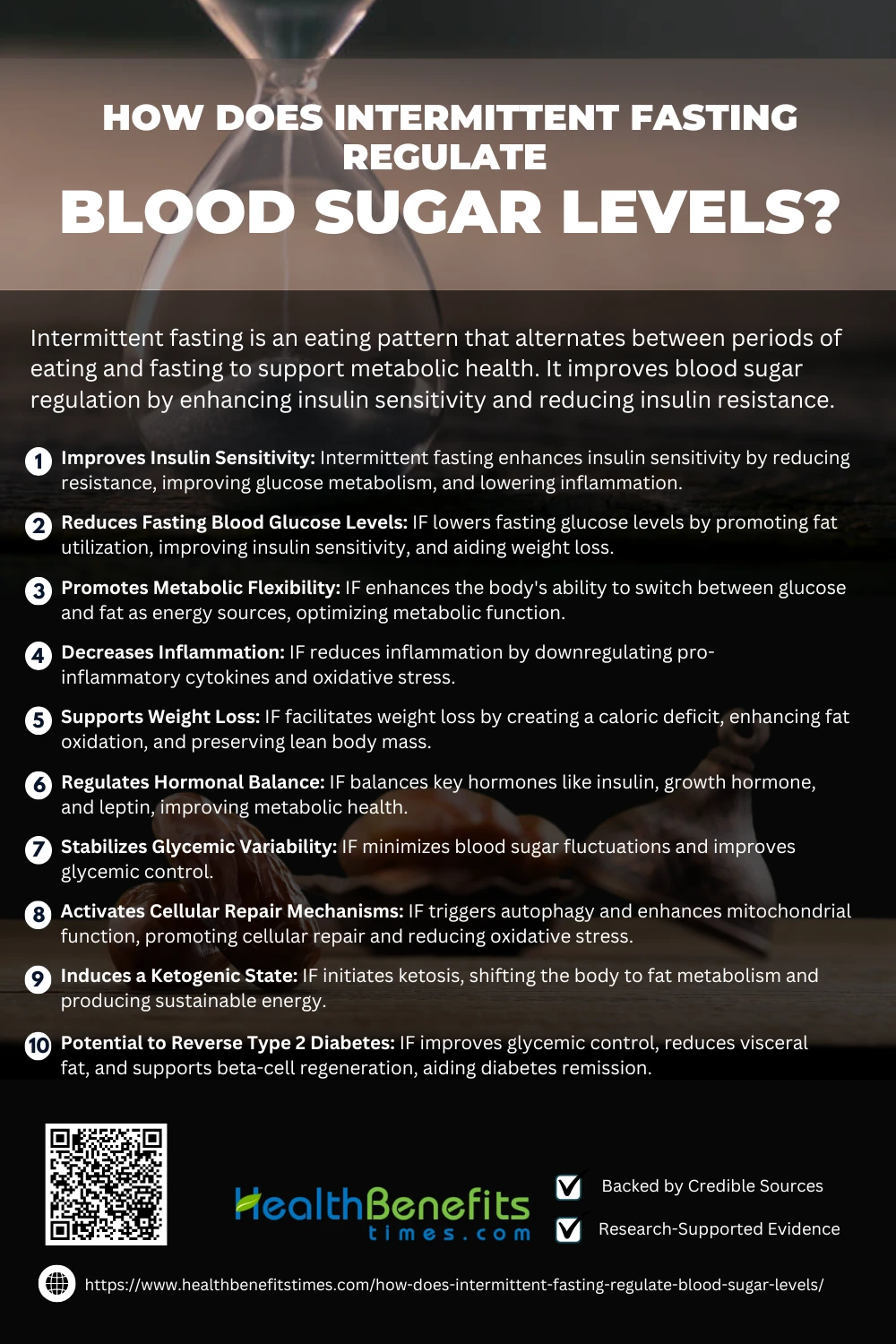 1. Improves Insulin Sensitivity
1. Improves Insulin Sensitivity
Intermittent fasting (IF) significantly enhances insulin sensitivity by reducing insulin resistance and improving glucose metabolism. It modulates key pathways in insulin signaling, such as the activation of AMP-activated protein kinase, enhancing cellular responsiveness to insulin (4). IF also decreases visceral fat, a major contributor to insulin resistance, further improving metabolic outcomes (13). Additionally, it regulates inflammatory markers that impair insulin action (12).
2. Reduces Fasting Blood Glucose Levels
Intermittent fasting (IF) effectively reduces fasting blood glucose levels by improving glucose metabolism and lowering insulin resistance. Studies demonstrate that IF promotes metabolic shifts, utilizing fat as a primary energy source and reducing glucose dependency (3). This process improves insulin sensitivity and decreases fasting glucose levels over time (2). Additionally, IF’s influence on weight loss and reduced visceral fat contributes to better glycemic control (12). Hormonal changes during fasting also enhance glucose utilization and reduce blood sugar variability (14).
3. Promotes Metabolic Flexibility
Intermittent fasting (IF) significantly enhances metabolic flexibility, the body’s ability to switch between glucose and fat as energy sources. Research indicates that IF stimulates mitochondrial efficiency and promotes the oxidation of stored lipids during fasting periods, improving energy balance (15). It facilitates a metabolic shift from carbohydrate reliance to fat mobilization, particularly through lipolysis (16). Additionally, IF optimizes insulin sensitivity and reduces systemic inflammation, further supporting metabolic adaptation (17).
4. Decreases Inflammation
Intermittent fasting (IF) has been shown to significantly reduce systemic inflammation by modulating key inflammatory pathways. Studies reveal that IF downregulates the activity of pro-inflammatory cytokines such as TNF-α and IL-6, which are associated with chronic diseases (18). Furthermore, it improves markers of oxidative stress, promoting cellular repair and reducing inflammation-induced tissue damage (19). IF also enhances mitochondrial function, helping to alleviate inflammation by reducing reactive oxygen species production (20). These effects make IF a promising strategy for managing inflammation-related disorders (21).
5. Supports Weight Loss
Intermittent fasting (IF) has gained recognition for its effectiveness in supporting weight loss through various metabolic mechanisms. IF creates a caloric deficit by restricting eating windows, leading to reduced energy intake and increased fat oxidation (22). Studies demonstrate that IF reduces visceral fat, a major contributor to metabolic syndrome, while preserving lean body mass (4). It also lowers levels of insulin and enhances lipolysis, promoting the use of stored fats as an energy source (23). Furthermore, IF improves adherence to dietary regimens compared to continuous calorie restriction (24).
6. Regulates Hormonal Balance
Intermittent fasting (IF) has a profound effect on hormonal balance, particularly by modulating insulin, growth hormone, and leptin levels. Research highlights that fasting increases the secretion of growth hormone, which aids in fat metabolism and muscle preservation (25). Additionally, IF enhances insulin sensitivity, reducing overall insulin levels and preventing metabolic disturbances (26). Leptin, the hunger-regulating hormone, is also positively affected, reducing appetite dysregulation (27). Furthermore, IF promotes autophagy in hormonal pathways, improving cellular health and metabolic function (28).
7. Stabilizes Glycemic Variability
Intermittent fasting (IF) plays a vital role in stabilizing glycemic variability by reducing fluctuations in blood sugar levels and improving glucose regulation. Research highlights that IF reduces postprandial glucose spikes and promotes steady insulin secretion, which minimizes glycemic excursions (29). This dietary pattern also enhances metabolic flexibility, allowing the body to efficiently switch between glucose and fat as energy sources (30). Furthermore, IF reduces markers of inflammation that contribute to glycemic instability (31). These effects collectively improve glycemic control, particularly in individuals with type 2 diabetes.
8. Activates Cellular Repair Mechanisms
Intermittent fasting (IF) stimulates cellular repair processes, primarily through the activation of autophagy, a mechanism where cells degrade and recycle damaged components. This process is critical for maintaining cellular health and preventing disease (32). IF triggers pathways such as AMP-activated protein kinase (AMPK), enhancing mitochondrial function and reducing oxidative stress (33). Additionally, IF enhances DNA repair and the removal of harmful proteins linked to aging and neurodegenerative diseases (34). The reduction in insulin levels during fasting further aids in decreasing pro-inflammatory responses, which supports cellular regeneration (28).
9. Induces a Ketogenic State
Intermittent fasting (IF) triggers a ketogenic state by depleting glycogen stores, causing the body to shift from using glucose to fat as its primary energy source. This process, known as ketosis, results in the production of ketone bodies, which provide a more sustainable energy source for the brain and muscles (35). Studies show that IF activates pathways like AMPK and PPAR-alpha, enhancing mitochondrial efficiency and fat metabolism (36).
10. Potential to Reverse Type 2 Diabetes
Intermittent fasting (IF) is increasingly recognized as a promising intervention for reversing type 2 diabetes (T2D) by improving glycemic control and insulin sensitivity. Studies show that IF reduces fasting glucose and HbA1c levels, key markers of diabetes management (37). The reduction of visceral fat through fasting also plays a critical role in enhancing insulin action (38). Moreover, fasting triggers autophagy, which may support pancreatic beta-cell regeneration and improve insulin production (39). These mechanisms collectively make IF a potential therapeutic strategy for achieving diabetes remission (40).
Considerations and Potential Risks of intermittent fasting
While intermittent fasting offers numerous health benefits, it’s not a one-size-fits-all approach. Certain individuals, such as those with medical conditions, pregnant women, or people with a history of eating disorders, may need to avoid or modify fasting practices. Potential side effects like fatigue, irritability, or nutrient deficiencies can arise if fasting is not done correctly. Understanding these risks and consulting a healthcare professional can help ensure a safe and effective fasting experience tailored to individual needs.
 1. Risk of Hypoglycemia
1. Risk of Hypoglycemia
Intermittent fasting (IF) can increase the risk of hypoglycemia, particularly in individuals on antidiabetic medications. Studies highlight that fasting may cause blood sugar levels to drop below safe thresholds, especially during prolonged fasting periods (3). This risk is amplified in patients using glucose-lowering drugs, requiring careful monitoring (41). Advanced glucose monitoring technologies have been recommended to prevent hypoglycemic events while practicing IF (42).
2. Nutritional Deficiencies
Intermittent fasting (IF) may lead to nutritional deficiencies, particularly in essential vitamins and minerals, due to reduced meal frequency and caloric intake. Studies highlight risks such as inadequate iron, calcium, and vitamin B12 levels, which can impact overall health (43). These deficiencies are more likely when fasting is combined with restrictive diets (44). Pregnant women and older adults are particularly vulnerable to the adverse effects of nutrient insufficiency during fasting (45).
3. Impact on Mental Health
Intermittent fasting (IF) can have mixed effects on mental health, potentially exacerbating anxiety and mood disorders in vulnerable populations. Additionally, IF may increase the risk of disordered eating behaviors, particularly in individuals with a history of eating disorders (46). On the other hand, short-term IF has been linked to increased neuroplasticity, suggesting potential cognitive benefits (47).
4. Potential Stress on Pregnant and Lactating Women
Intermittent fasting (IF) poses risks to pregnant and lactating women by potentially impacting fetal development and milk production. Research indicates that fasting may increase oxidative stress and disrupt nutrient availability crucial for fetal growth (48). Additionally, reduced caloric intake can affect maternal energy levels and lactation efficiency (41). These risks highlight the need for medical supervision for women considering fasting during these sensitive periods (49).
5. Sustainability Challenges
Intermittent fasting (IF) poses sustainability challenges due to its restrictive nature, which can lead to difficulties in long-term adherence. Research highlights that many individuals struggle to integrate IF into their lifestyle consistently, often leading to dropouts (2). Additionally, social eating norms and rigid schedules may further complicate adherence (50). Critics also point out that the psychological burden of fasting can reduce its feasibility as a lasting dietary strategy (51).
6. Risk of Bone Density Loss
Intermittent fasting (IF) may contribute to bone density loss due to reduced nutrient intake, particularly calcium and vitamin D. Research suggests that prolonged fasting or severe caloric restriction can negatively impact bone health, increasing the risk of fractures (52). A decrease in lean body mass during fasting can also exacerbate skeletal fragility (53). Moreover, older adults practicing IF are at a heightened risk, requiring close monitoring of bone health (54).
7. Interaction with Medications
Intermittent fasting (IF) can influence the effectiveness and metabolism of certain medications, particularly those for diabetes and hypertension. Research highlights that fasting alters drug pharmacokinetics, potentially leading to hypoglycemia or suboptimal therapeutic effects (4). Adjustments in dosing may be necessary, especially for individuals on insulin or glucose-lowering agents (55). Patients are advised to consult healthcare providers to mitigate risks, as improper fasting can exacerbate medication-related side effects (56).
Practical Tips for Implementing IF for Blood Sugar Management
Successfully managing blood sugar with intermittent fasting (IF) requires a strategic approach. Selecting the right fasting schedule, consuming balanced meals during eating windows, and staying hydrated are key. Gradual adaptation and mindful tracking of blood sugar levels can help optimize IF benefits while minimizing potential risks for long-term metabolic health.
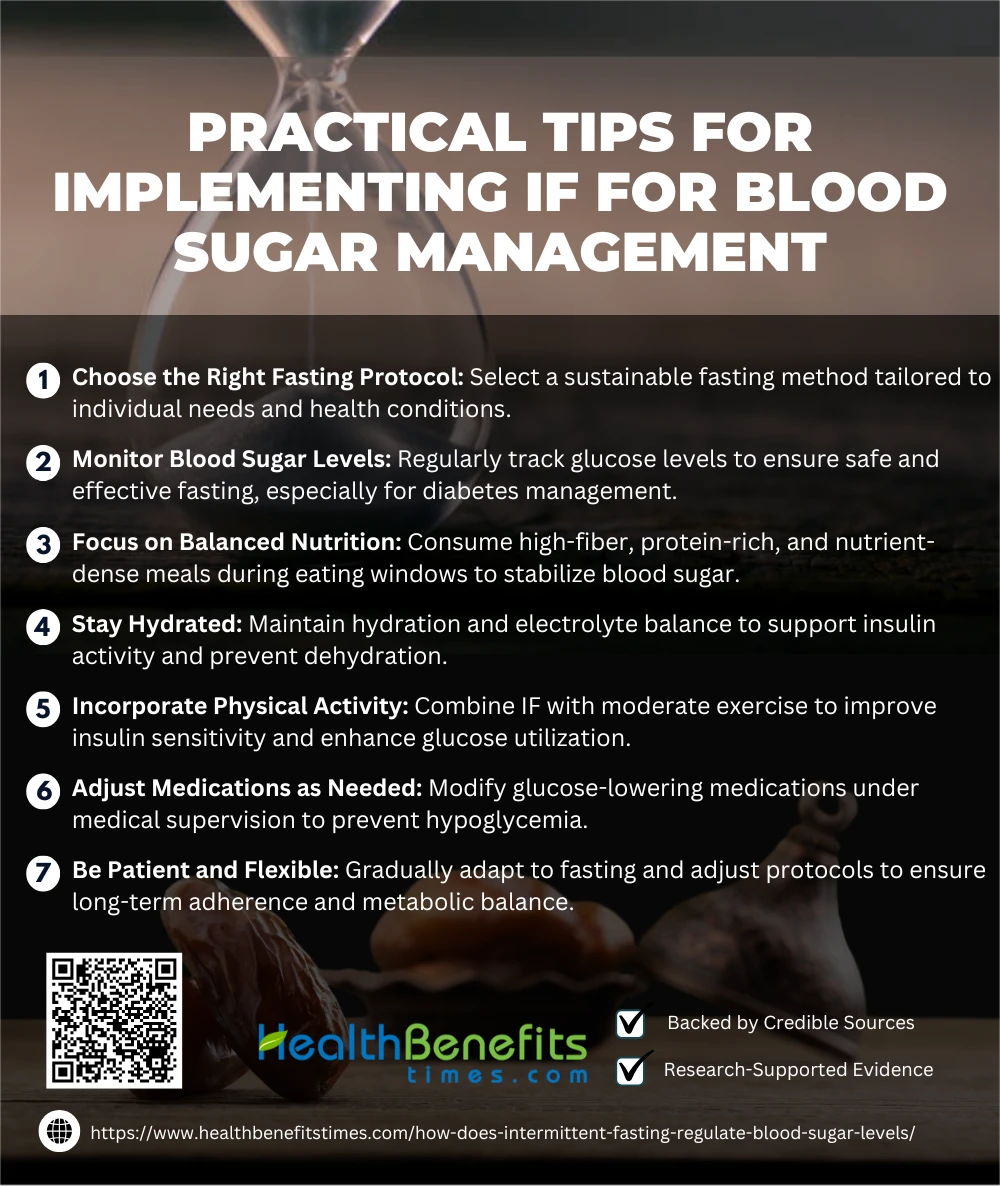 1. Choose the Right Fasting Protocol
1. Choose the Right Fasting Protocol
Selecting an appropriate fasting protocol is essential for effective blood sugar management. The 16:8 method, which involves fasting for 16 hours and eating during an 8-hour window, is widely recommended for beginners due to its sustainability and benefits on glycemic control (47). For individuals with type 2 diabetes, modified alternate-day fasting has been shown to improve insulin sensitivity while minimizing hypoglycemia risks (3). Incorporating physical activity during non-fasting hours enhances the benefits (57). Adherence to fasting schedules tailored to individual needs ensures safety and effectiveness (58).
2. Monitor Blood Sugar Levels
Monitoring blood sugar levels is crucial for safely implementing intermittent fasting (IF), particularly for individuals with diabetes or insulin resistance. Regular glucose monitoring ensures early detection of hypoglycemia or hyperglycemia, reducing associated risks (59). Continuous glucose monitoring (CGM) technologies offer real-time insights, making IF more manageable and safer (60). Additionally, studies emphasize the role of frequent monitoring in tailoring fasting regimens and medication adjustments (61).
3. Focus on Balanced Nutrition
Balanced nutrition is essential when practicing intermittent fasting (IF) to regulate blood sugar effectively. Incorporating high-fiber foods, lean proteins, and healthy fats can stabilize glucose levels and prevent energy crashes (62). Avoiding refined carbohydrates and sugary foods helps minimize glycemic spikes (59). Research emphasizes the role of micronutrient-rich meals in supporting insulin sensitivity during eating windows (63). Additionally, meal timing and nutrient density are critical for sustaining energy and metabolic health (64).
4. Stay Hydrated
Proper hydration is essential during intermittent fasting (IF) to maintain optimal blood sugar levels and prevent dehydration. Research highlights that drinking water throughout the fasting period helps regulate insulin activity and cellular functions (65). Including electrolyte-rich beverages during eating windows further aids hydration and glucose stability (59). Hydration strategies are particularly crucial for individuals managing diabetes to maintain consistent glycemic control (66).
5. Incorporate Physical Activity
Combining intermittent fasting (IF) with physical activity amplifies its benefits for blood sugar management by improving insulin sensitivity and enhancing glucose uptake in muscles. Studies reveal that moderate exercise, such as walking or resistance training, during non-fasting periods optimizes glucose utilization (67). Additionally, resistance training during IF boosts fat oxidation while preserving muscle mass (68). Tailoring activity intensity and timing to individual needs is key to minimizing risks such as hypoglycemia (69). Hydration and nutritional strategies further complement exercise benefits (70).
6. Adjust Medications as Needed
Adjusting medications is critical when practicing intermittent fasting (IF) for blood sugar management, particularly for individuals on glucose-lowering agents. Research shows that fasting alters glucose metabolism, necessitating careful adjustments in insulin and oral hypoglycemic drugs to avoid hypoglycemia (59). Continuous monitoring helps tailor dosage modifications to fasting patterns (60). Collaboration with healthcare providers ensures safe implementation of IF, minimizing risks while optimizing glucose control (71). Periodic reassessment of medication regimens is essential for achieving long-term success (72).
7. Be Patient and Flexible
Patience and flexibility are key to successfully managing blood sugar while implementing intermittent fasting (IF). Adapting fasting protocols to individual needs helps mitigate adverse effects and enhances long-term adherence (67). Regular monitoring allows for adjustments in fasting windows, preventing glucose imbalances (59). Embracing a gradual transition into fasting, rather than abrupt changes, supports metabolic adaptation (68). Combining flexibility in dietary choices during eating windows ensures sustainability and minimizes psychological stress (64).
Conclusion
Intermittent fasting offers a powerful approach to regulating blood sugar levels by improving insulin sensitivity, promoting fat utilization, and reducing inflammation. Its ability to stabilize glucose levels makes it a promising strategy for managing and preventing metabolic disorders like diabetes. However, personalized guidance and mindful implementation are essential for safe and effective results.
References:
- Liu, K., Liu, B., & Heilbronn, L. K. (2020). Intermittent fasting: what questions should we be asking? Physiology & Behavior.
- Patterson, R. E., Laughlin, G. A., & Sears, D. D. (2015). Intermittent fasting and human metabolic health. Journal of Clinical Endocrinology and Metabolism.
- Arnason, T. G., Bowen, M. W., & Mansell, K. D. (2017). Effects of intermittent fasting on health markers in those with type 2 diabetes. World Journal of Diabetes.
- Mattson, M. P., Longo, V. D., & Harvie, M. (2017). Impact of intermittent fasting on health and disease processes. Ageing Research Reviews.
- Vitale, R., & Kim, Y. (2020). Effects of intermittent fasting on glycemic control and body composition. Metabolic Syndrome and Related Disorders.
- Albosta, M., & Bakke, J. (2021). Intermittent fasting: is there a role in diabetes management? Clinical Diabetes and Endocrinology.
- Schwarz, P. E. H., Timpel, P., & Harst, L. (2018). Blood sugar regulation as a key focus for cardiovascular health promotion and prevention: an umbrella review. Journal of the Endocrine Society.
- Singh, H., Aggarwal, J., & Pasha, E. H. (2023). Beyond blood sugar: Unraveling the complexities of liver and kidney health in type 2 diabetes mellitus. South University Journal of Health Sciences.
- Gloyn, A. L., Odili, S., & Buettger, C. (2004). Glucokinase and the regulation of blood sugar. Diabetes and Glycemic Disease Management.
- Lesiak, A. J., & Griswold, J. C. (2023). Blood sugar balance: A glucose metabolism web game for diabetes education. The American Biology Teacher.
- Ackerman, E., Gatewood, L. C., & Rosevear, J. W. (1965). Model studies of blood-glucose regulation. The Bulletin of Mathematical Biophysics.
- Malinowski, B., Zalewska, K., & Węsierska, A. (2019). Intermittent fasting in cardiovascular disorders—an overview.
- Hoddy, K. K., Unterman, T. G., & others. (2014). Intermittent fasting vs daily calorie restriction for type 2 diabetes prevention: a review of human findings. Translational Research.
- Kim, B. H., & Choe, H. K. (2021). Effects of intermittent fasting on circulating hormones and glucose regulation. Endocrinology and Metabolism.
- Palmer, B. F., & Clegg, D. J. (2022). Metabolic flexibility and its impact on health outcomes. Mayo Clinic Proceedings.
- Mishra, S., & Singh, B. (2020). Intermittent fasting and metabolic switching: a brief overview. Biomedical and Pharmacology Journal.
- Dedual, M. A., Wueest, S., & Borsigova, M. (2019). Intermittent fasting improves metabolic flexibility in short-term high-fat diet-fed mice. American Journal of Physiology-Endocrinology and Metabolism.
- Haasis, E., Bettenburg, A., & Lorentz, A. (2024). Effect of Intermittent Fasting on Immune Parameters and Intestinal Inflammation.
- Marinho, T. S., Ornellas, F., & Barbosa-da-Silva, S. (2019). Beneficial effects of intermittent fasting on liver inflammation.
- Zouhal, H., Bagheri, R., & Wong, A. (2020). Effects of Ramadan intermittent fasting on inflammatory biomarkers. Physiology & Behavior.
- Wang, X., Liao, Q., & Santos, H. O. (2020). Effects of intermittent fasting diets on inflammatory biomarkers.
- Silverii, G. A., Cresci, B., & Benvenuti, F. (2023). Effectiveness of intermittent fasting for weight loss in individuals with obesity. Nutrition, Metabolism & Cardiovascular Diseases.
- Jospe, M. R., Roy, M., & Brown, R. C. (2020). Exploratory secondary analyses of intermittent fasting and weight-loss trials. The American Journal of Clinical Nutrition.
- Torres, L., Lee, J. L., & Park, S. (2022). Retention, fasting patterns, and weight loss with an intermittent fasting app. JMIR mHealth and uHealth.
- Zouhal, H., Bagheri, R., & Wong, A. (2020). Effects of Ramadan intermittent fasting on gut hormones and body composition. International Journal of Environmental Research and Public Health.
- Tagde, P., & Bhattacharya, T. (2022). Multifaceted effects of intermittent fasting on treatment and prevention of chronic diseases. Current Diabetes Reviews.
- Fink, J., Tanaka, M., & Horie, S. (2024). Effects of fasting on metabolic hormones and functions. Juntendo Medical Journal.
- Salvadori, G., Mirisola, M. G., & Longo, V. D. (2021). Intermittent fasting and its effects on hormonal balance.
- Halberg, N., Henriksen, M., & Osterberg, K. L. (2005). Effect of intermittent fasting and refeeding on insulin action in healthy men. Journal of Applied Physiology.
- Mindikoglu, A. L., Abdulsada, M. M., & Jain, A. (2020). Intermittent fasting from dawn to sunset stabilizes glycemic markers. Journal of Clinical Endocrinology.
- Lee, S. H., Min, K. W., & Lee, B. W. (2021). Glycemic variability in intermittent fasting patterns. Diabetes & Metabolism.
- Mattson, M. P., Longo, V. D., & Harvie, M. (2017). Impact of intermittent fasting on health and disease processes. Ageing Research Reviews.
- Longo, V. D., & Panda, S. (2016). Fasting, circadian rhythms, and time-restricted feeding in healthy lifespan. Cell Metabolism.
- Madeo, F., Carmona-Gutierrez, D., Hofer, S. J., & Kroemer, G. (2019). Caloric restriction mimetics against age-associated disease. Aging.
- Neudorf, H., & Little, J. P. (2024). Impact of fasting and ketogenic interventions on the NLRP3 inflammasome: A narrative review. Biomedical Journal.
- Stepan, M. D., & Surugiu, R. (2024). Molecular mechanisms of healthy aging: The role of caloric restriction, intermittent fasting, Mediterranean diet, and ketogenic diet—a scoping review. Nutrients.
- Ali, M., Saeed, M., & Zaidi, S. A. H. (2021). Intermittent fasting: A user-friendly method for type 2 diabetes mellitus. Cureus.
- Lichtash, C., Fung, J., & Ostoich, K. C. (2020). Therapeutic use of intermittent fasting and ketogenic diet for T2D treatment. BMJ Case Reports.
- DiNicolantonio, J. J., & McCarty, M. (2019). Autophagy and beta-cell neogenesis in intermittent fasting. Open Heart.
- Shazman, S. (2023). Understanding T2D risk parameters through intermittent fasting. Nutrients.
- Grajower, M. M., & Horne, B. D. (2019). Clinical management of intermittent fasting in patients with diabetes mellitus. Nutrients.
- Muñoz-Hernández, L., Márquez-López, Z., & Mehta, R. (2020). Intermittent fasting as part of the management for T2DM: From animal models to human clinical studies. Current Diabetes Reports.
- Gudden, J., Arias Vasquez, A., & Bloemendaal, M. (2021). The effects of intermittent fasting on brain and cognitive function. Nutrients.
- Roslin, M., Becker, A., & Gaballa, D. (2021). Novel nutritional and dietary approaches to weight loss. Current Cardiology Reports.
- Faris, M. A. I. E., & Al-Holy, M. (2014). Implications of intermittent fasting on maternal health. Mediterranean Journal of Nutrition and Metabolism.
- Harding, S. (2021). Intermittent fasting: Clinical considerations for mental health. The Journal for Nurse Practitioners.
- Laughlin, G. A., Sears, D. D., & Patterson, R. E. (2015). Intermittent fasting and human metabolic health. Journal of the Endocrine Society.
- Jahrami, H. A., Obaideen, A. A., & Mo’ez Al-Islam, E. F. (2019). Impact of diurnal intermittent fasting during Ramadan on oxidative stress markers. Journal of Nutrition & Metabolism.
- Brewer, S. (2020). Fasting during pregnancy and lactation: Effects on health and development. London School of Hygiene & Tropical Medicine.
- Longo, V. D., & Mattson, M. P. (2021). Intermittent fasting and longevity: Mechanisms and challenges. Nature Aging.
- Bienko, M., Rutkowska, M., & Toborek, M. (2024). Sustainability of intermittent fasting in sports and metabolic health. Quality in Sport.
- Anton, S., Ezzati, A., Witt, D., & McLaren, C. (2021). The effects of intermittent fasting regimens in middle-age and older adults: Current state of evidence. Experimental Gerontology.
- Veronese, N., & Reginster, J. Y. (2019). The effects of calorie restriction, intermittent fasting, and vegetarian diets on bone health. Aging Clinical and Experimental Research.
- Fallata, R. M., Nassar, S. M. S., & Almuabbiri, M. A. (2019). Exploring the impact of intermittent fasting on metabolic health in adults. SJR Publishing.
- Horne, B. D., Anderson, J. L., & May, H. T. (2023). Intermittent fasting and changes in clinical risk scores: Secondary analysis. Journal of Cardiovascular Risk Management.
- Garza-González, S., & Nieblas, B. (2022). Intermittent fasting as a treatment for cardiometabolic conditions. Current Vascular Pharmacology.
- Davies, M. J., Ahmad, E., & Ibrahim, M. (2022). Intermittent fasting and diabetes: Clinical considerations. Diabetes Care.
- Varady, K. A., & Cienfuegos, S. (2022). Clinical application of intermittent fasting for weight loss and metabolic health. Nature Reviews Endocrinology.
- Franz, M. J., Bantle, J. P., & Beebe, C. A. (2008). Nutrition recommendations and interventions for diabetes: 2008. American Diabetes Association.
- Nathan, D. M., Buse, J. B., & Davidson, M. B. (2009). Management of hyperglycemia in type 2 diabetes. Diabetes Care.
- Sacks, D. B., Bruns, D. E., & Goldstein, D. E. (2002). Guidelines for laboratory analysis in diabetes management. Clinical Chemistry.
- Reynolds, A., & Mitri, J. (2024). Dietary advice for individuals with diabetes. Endotext.
- Evert, A. B., Dennison, M., & Gardner, C. D. (2019). Nutrition therapy for adults with diabetes or prediabetes. PMC.
- Lichtenstein, A. H., & Appel, L. J. (2006). Diet and lifestyle recommendations for cardiovascular health. Circulation.
- Smart, C. E., Annan, F., Higgins, L. A., & others. (2018). Nutritional management in children and adolescents with diabetes. Pediatric Diabetes.
- Gray, A., & Threlkeld, R. J. (2015). Nutritional recommendations for individuals with diabetes. Europe PMC.
- Piercy, K. L., Troiano, R. P., & Ballard, R. M. (2018). Physical activity guidelines for Americans. JAMA Network.
- Colberg, S. R., Sigal, R. J., & Fernhall, B. (2010). Exercise and type 2 diabetes. Diabetes Care.
- Heron, K. E., & Smyth, J. M. (2010). Ecological momentary interventions. British Journal of Health Psychology.
- Thompson, P. D., Buchner, D., & Piña, I. L. (2003). Exercise training and diabetes management. Circulation.
- Evert, A. B., Boucher, J. L., & Cypress, M. (2014). Nutrition therapy recommendations for diabetes. Diabetes Care.
- Umpierrez, G. E., & Hellman, R. (2012). Management of hyperglycemia in hospitalized patients. The Journal of Clinical Endocrinology & Metabolism.

