White blood cells (WBCs), also known as leukocytes, are crucial components of the immune system, responsible for defending the body against infections and foreign invaders. They are produced in the bone marrow and circulate in the blood and lymphatic system. WBCs are categorized into various subtypes, including neutrophils, lymphocytes, monocytes, eosinophils, and basophils, each playing distinct roles in immune responses. The count and functionality of these cells are vital indicators of health, with abnormalities potentially signaling conditions such as leukopenia, autoimmune diseases, or infections. Together, these cells circulate in the blood and lymphatic system, constantly patrolling for signs of disease and orchestrating the body’s defense mechanisms.
Types of White Blood Cells
White blood cells (WBCs), also known as leukocytes, are a crucial component of the immune system. They help protect the body against infections and foreign invaders. There are several types of white blood cells, each with unique functions and characteristics. Below is a list of the main types of white blood cells:
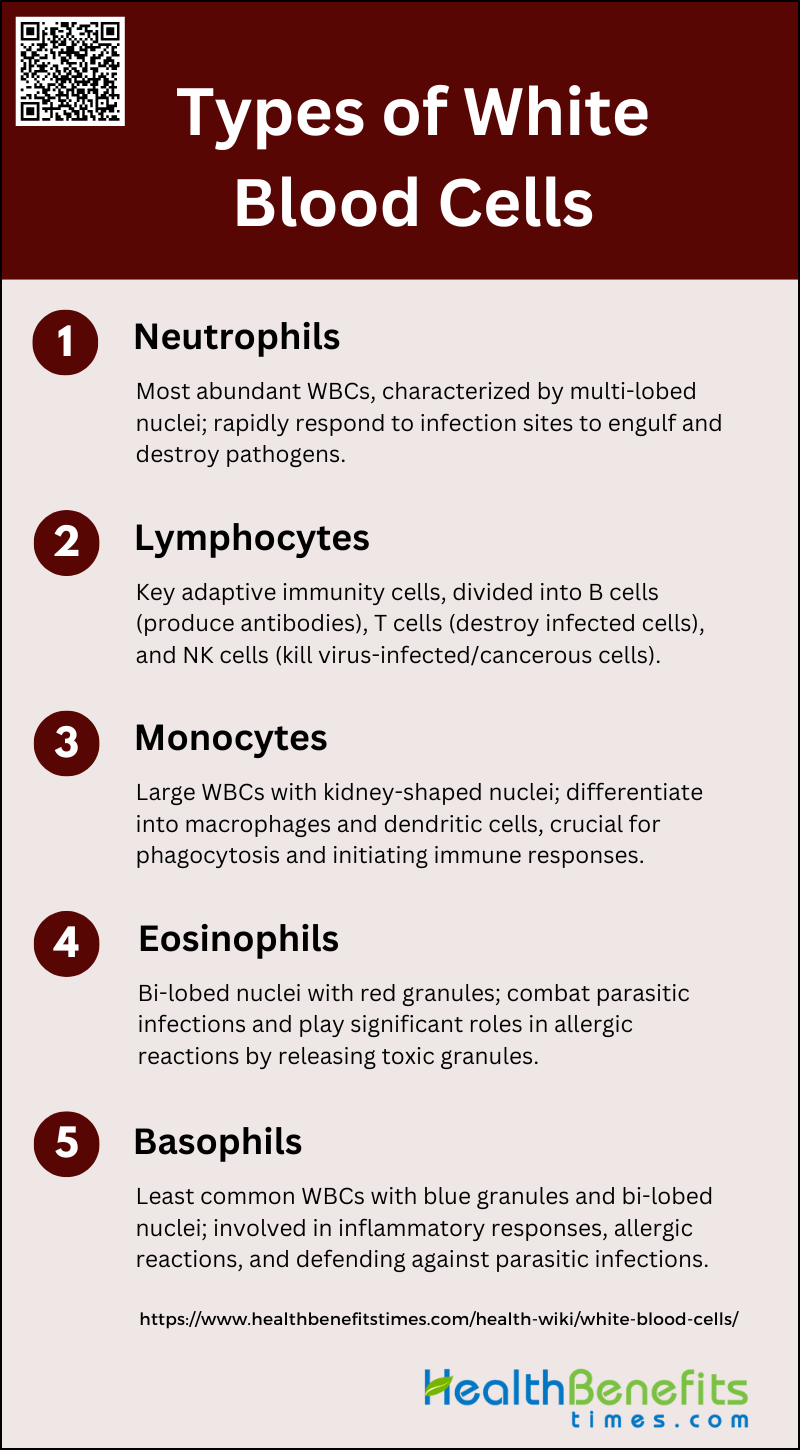
1. Neutrophils
Neutrophils are the most abundant type of white blood cells, characterized by their multi-lobed nucleus and granular cytoplasm. They play a crucial role in the innate immune response by rapidly migrating to infection sites, where they perform phagocytosis to engulf and destroy pathogens. Neutrophils also release enzymes and reactive oxygen species to kill microorganisms and form neutrophil extracellular traps (NETs) to trap and neutralize pathogens.
2. Lymphocytes
Lymphocytes are key players in adaptive immunity and are divided into B cells, T cells, and Natural Killer (NK) cells. B cells produce antibodies that neutralize pathogens, while T cells destroy infected cells and regulate immune responses. NK cells, part of the innate immune system, target and kill virus-infected and cancerous cells without prior sensitization. Together, these cells ensure a robust and specific immune response to various pathogens.
3. Monocytes
Monocytes are large white blood cells with a kidney-shaped nucleus. They circulate in the blood and migrate into tissues, where they differentiate into macrophages and dendritic cells. Macrophages are essential for phagocytosis, engulfing pathogens and cellular debris, while dendritic cells present antigens to T cells, initiating adaptive immune responses. Both cell types play pivotal roles in maintaining immune surveillance and orchestrating immune responses.
4. Eosinophils
Eosinophils are characterized by their bi-lobed nucleus and large, red-staining granules. They are primarily involved in combating parasitic infections and play a significant role in allergic reactions. Eosinophils release toxic granules and inflammatory mediators that can kill parasites and modulate the immune response during allergic conditions, such as asthma.
5. Basophils
Basophils are the least common type of white blood cells, identifiable by their large, blue-staining granules and bi-lobed nucleus. They are crucial in inflammatory responses and allergic reactions, releasing histamine and other mediators that contribute to inflammation and vasodilation. Basophils also play a role in defending against parasitic infections and modulating the immune response.
Functions of White Blood Cells
White blood cells (WBCs) play a vital role in the body’s immune response. They are responsible for identifying and neutralizing pathogens such as bacteria, viruses, and other foreign substances. Below is a list of the primary functions of different types of white blood cells:
1. Defending Against Infection
White blood cells (WBCs) play a crucial role in defending the body against infections by identifying and attacking pathogens such as viruses, bacteria, parasites, and fungi. Neutrophils, a type of WBC, are often the first responders to infection sites, where they engulf and destroy pathogens through a process called phagocytosis. Lymphocytes, another type of WBC, are involved in recognizing specific antigens presented by pathogens and initiating an adaptive immune response. Monocytes, which differentiate into macrophages, also contribute by phagocytosing pathogens and presenting antigens to lymphocytes, thereby bridging innate and adaptive immunity.
2. Producing Antibodies
Lymphocytes, particularly B cells, are essential for the production of antibodies, which are proteins that specifically target and neutralize pathogens. When B cells encounter an antigen, they differentiate into plasma cells that secrete large quantities of antibodies. These antibodies bind to antigens on the surface of pathogens, marking them for destruction by other immune cells or neutralizing their harmful effects directly. This process is a critical component of the adaptive immune response, providing long-term protection and immunological memory against specific pathogens.
3. Removing Dead Cells
Phagocytosis is a process by which certain WBCs, such as neutrophils and macrophages, engulf and digest dead cells and cellular debris. This function is vital for maintaining tissue homeostasis and preventing the accumulation of potentially harmful cellular waste. Macrophages, which originate from monocytes, are particularly adept at clearing dead cells and are often found in tissues where they continuously monitor and clean up cellular debris. This process not only helps in tissue repair but also in the resolution of inflammation.
4. Fighting Allergies and Inflammation
Eosinophils and basophils are WBCs that play significant roles in allergic reactions and inflammation. Eosinophils are involved in combating parasitic infections and are key players in allergic responses, where they release cytotoxic granules that can damage tissues and contribute to inflammation. Basophils, although less abundant, are crucial for initiating and propagating allergic inflammation. They release histamine and other mediators that increase vascular permeability and attract other immune cells to the site of inflammation. Both cell types are essential for the body’s response to allergens and in the regulation of immune responses.
Normal Ranges of White Blood Cells
The normal range of WBCs can vary based on age, sex, and overall health. Below is a list of the typical normal ranges for white blood cells:
1. Explanation of WBC Count
White blood cell (WBC) count is a critical clinical measure obtained from complete blood count assays, which helps in assessing the immune system’s status and detecting various medical conditions. WBCs are essential components of the immune system, responsible for defending the body against infections and foreign invaders. The total WBC count includes several subtypes such as neutrophils, lymphocytes, monocytes, eosinophils, and basophils, each playing distinct roles in immune response. The count can vary widely among healthy individuals and is influenced by genetic factors, as evidenced by studies identifying specific genomic loci associated with WBC phenotypes. Additionally, WBC count is a heritable trait, with different subtypes showing varying degrees of heritability.
2. Normal Range Values
The normal range for WBC count in healthy individuals typically falls between 4,000 and 10,000 cells per microliter of blood. However, these values can slightly differ based on demographic factors such as age, gender, and ethnicity. For instance, a large survey of Israelis without significant inflammation reported normal WBC ranges of 3.6-9.9 x10^3/µL for men and 3.4-10.0 x10^3/µL for women. Smokers tend to have higher WBC counts, with ranges extending up to 11.5 x10^3/µL for men and 11.2 x10^3/µL for women. These reference ranges are crucial for risk stratification and diagnosing conditions like infections, inflammatory diseases, and hematologic disorders.
3. Factors Influencing White Blood Cells Count
Several factors can influence WBC count, including genetic predispositions, lifestyle choices, and underlying health conditions. Genetic factors play a significant role, with specific loci associated with variations in WBC count and its subtypes. Lifestyle factors such as smoking have been shown to elevate WBC counts significantly. Additionally, metabolic conditions like diabetes and cardiovascular diseases are linked to variations in WBC count. For example, higher WBC counts within the normal range are associated with increased hemoglobin A1c levels, indicating a potential link to glucose metabolism and diabetes risk. Furthermore, WBC count and its subtypes can predict cardiovascular risk, with elevated neutrophil counts and high neutrophil-to-lymphocyte ratios being strong predictors of adverse cardiovascular events. These findings underscore the importance of considering multiple factors when interpreting WBC counts in clinical practice.
When to Worry About White Blood Cells Count
White blood cells (WBCs) are crucial for fighting infections and maintaining overall health. However, abnormal WBC counts can indicate underlying health issues. Below is a list of situations when you should be concerned about your white blood cell count:
1. High WBC Count (Leukocytosis)
Leukocytosis, or an elevated white blood cell (WBC) count, can arise from various causes, both malignant and nonmalignant. Common nonmalignant causes include infections, particularly bacterial infections, as well as physiological stressors such as surgery, trauma, and emotional stress. Medications like corticosteroids and conditions such as smoking, obesity, and chronic inflammatory diseases can also lead to leukocytosis. Symptoms of leukocytosis often include fever, weight loss, bruising, and fatigue, which may indicate a hematologic malignancy if no other cause is identified. Risks associated with high WBC counts include an increased likelihood of thrombosis, particularly in patients with myeloproliferative disorders like polycythemia vera and essential thrombocythemia. In severe cases, such as hyperleukocytosis in acute myeloid leukemia, there is a significant risk of complications like intracranial hemorrhage and leukostasis, which can be life-threatening.
2. Low WBC Count (Leukopenia)
Leukopenia, or a low WBC count, can result from a variety of conditions, including bone marrow disorders, autoimmune diseases, severe infections, and the use of certain medications such as chemotherapy drugs. Common causes also include viral infections and conditions that lead to bone marrow suppression or damage. Symptoms of leukopenia often include increased susceptibility to infections, fever, and fatigue, as the body’s ability to fight off pathogens is compromised. The risks associated with leukopenia are primarily related to the increased likelihood of infections, which can be severe and potentially life-threatening if not promptly treated. In the context of diseases like COVID-19, leukopenia has been associated with better prognoses, indicating a complex relationship between WBC counts and disease outcomes.