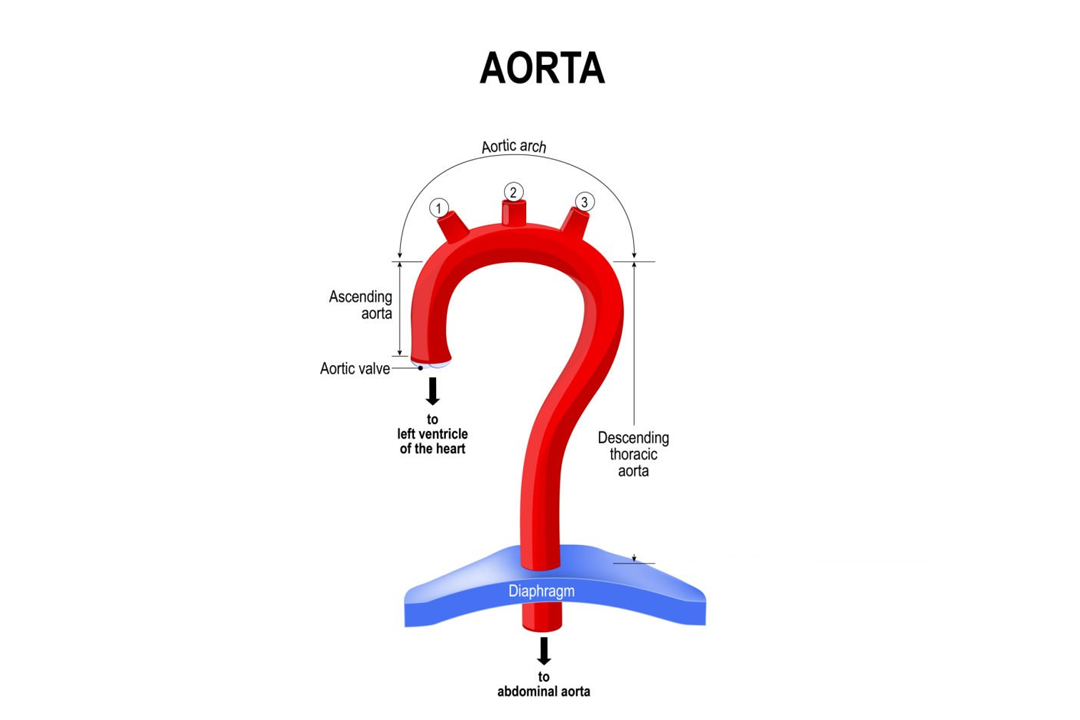
The aorta, known as the main artery in the human body, originates from the left ventricle of the heart and extends down to the abdomen, distributing oxygenated blood to all parts of the body through its branches, including the crucial coronary arteries. It is considered a dynamic structure, capable of maintaining optimal mechanical function through the continuous turnover of its internal structure, which is essential for the entire cardiovascular system’s functionality. Pathologically, an aortic aneurysm is diagnosed when there is a localized, pathological dilation of the aorta to more than 50% of its expected normal diameter, posing significant health risks. The health of the aorta is crucial, as conditions such as thoracic aortic calcification are linked to increased risks of cardiovascular and cerebrovascular events, presenting challenges to cardiac surgeons due to the potential for excessive aortic injury during procedures. Additionally, the aorta can be affected by diseases such as dissection, which requires prompt and accurate diagnosis for successful treatment, underscoring the importance of early detection. Abdominal aortic aneurysm (AAA), a multifactorial disease more common in men over 65, involves focal dilation of the abdominal aorta, with rupture being a feared complication necessitating emergency surgical intervention. The complexity of aortic pathologies requires a multidisciplinary approach for diagnosis and treatment, involving a team of specialists to ensure optimal outcomes. Furthermore, advancements in imaging and computational methods have enabled the precise calculation of the aorta’s geometry, aiding in the diagnosis and treatment of heart-related diseases. However, aortic calcifications can complicate or even prevent surgical interventions, emphasizing the need for careful preoperative assessment to avoid inoperable situations.
Causes of Aortic Disease
Aortic diseases, which encompass a wide range of disorders, are influenced by a complex interaction of genetic, environmental, and lifestyle factors. Risk factors for cardiovascular health such as hypertension, smoking, and hyperlipoproteinemia play a significant role in the development of aortic diseases, including aneurysms and dissections, which can result in sudden rupture and potentially fatal outcomes if not identified and treated promptly. Genetic predispositions are also crucial, particularly in diseases affecting the vasculature, specifically the aortic root and ascending aorta. Conditions such as Marfan syndrome, vascular Ehlers–Danlos syndrome, Loeys–Dietz syndrome, Turner syndrome, and familial thoracic aneurysm and dissection are genetic diseases with known mutations that have a significant impact on the structure and function of the aorta. The development of aortic dissection, a critical condition within the spectrum of aortic diseases, is associated with pathological conditions such as medial degeneration, characterized by a loss of elastic fibers and damage to the vasa vasorum, as well as mechanical wall stress induced by factors like shear stress from blood flow and hypertension. Lifestyle factors, particularly smoking, contribute to endothelial dysfunction through inflammation and oxidative stress, increasing the risk of aortic wall damage.
Symptoms of Aortic Disease
Aortic diseases present with a range of symptoms that can be deceptive and varied, making timely diagnosis challenging. Classic symptoms include severe, sharp, or tearing chest or back pain, which is characteristic of acute aortic dissection. However, patients may also experience atypical symptoms such as epigastric pain, nausea, vomiting, and neurological symptoms like flaccid hemiplegia and slurred speech, which can mimic stroke or intracranial hemorrhage. The clinical presentation may be further complicated by symptoms that resemble other conditions, such as ischemic heart disease, hypertensive crisis, or pulmonary embolism, making differential diagnosis difficult. Neurological signs, including lower extremity pain, transient global amnesia, and acute cerebral ischemia, can be prominent, hindering accurate diagnosis of this life-threatening disease.
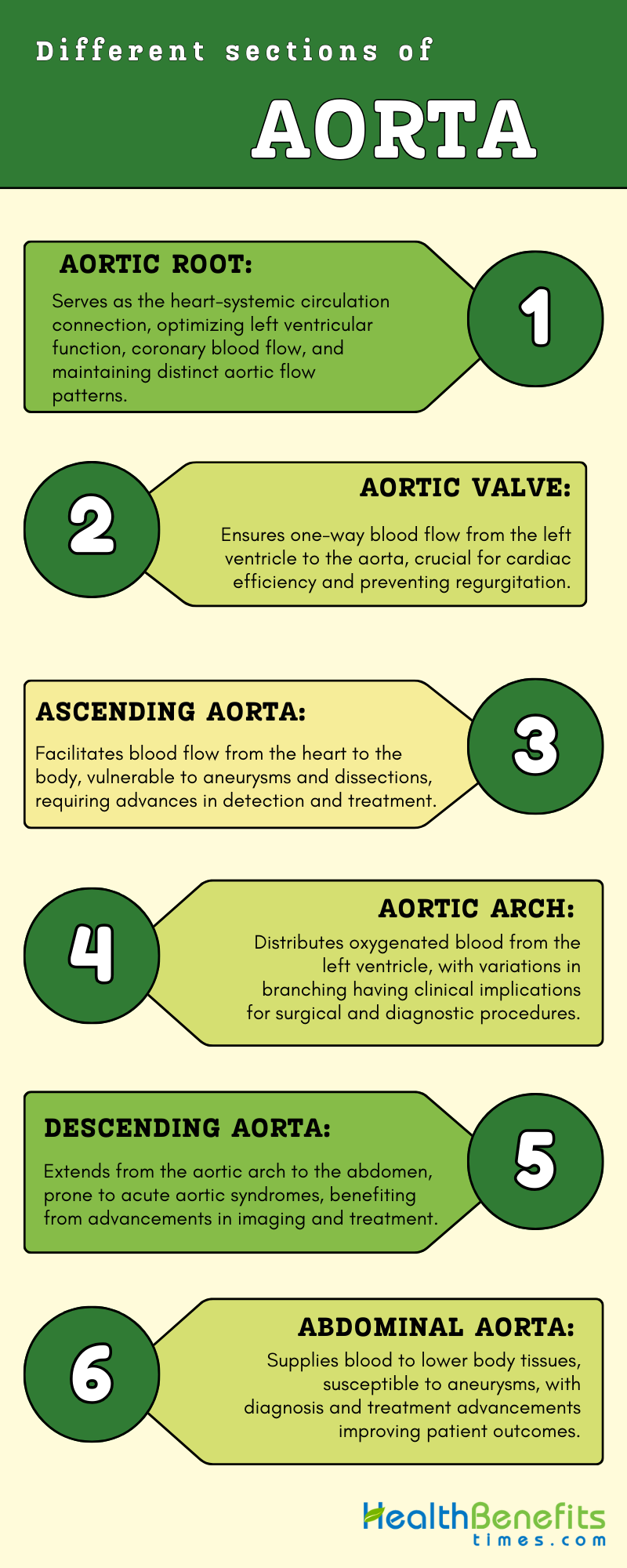
Different sections of Aorta
The aorta, a vital artery in the human body, displays significant variability across its different segments, which include the ascending aorta, aortic arch, thoracic, and abdominal segments. Each segment responds differently to physiological conditions and metabolic pathologies. This diversity is further highlighted by the unique cellular compositions and gene expression profiles within these segments, which undergo notable changes under conditions such as high blood glucose levels, dietary salt, or fat intake, particularly impacting the cellular makeup of the abdominal aorta. The abdominal aorta plays a crucial role in supplying blood to essential organs and is also prone to diseases like abdominal aortic aneurysm (AAA), which necessitates prompt diagnosis and treatment to prevent severe consequences.
1. Aortic root
The aortic root is a complex and highly sophisticated structure that serves as the connection between the heart and the systemic circulation. It plays a crucial role in optimizing the function of the left ventricular pump, ensuring normal coronary blood flow, and maintaining a distinctive flow pattern in the aorta. Its anatomy was described as early as by Leonardo da Vinci and later named by Antonio Maria Valsalva. This includes the sinuses of Valsalva, which are critical for its function, indicating the historical recognition of its complexity.
2. Aortic valve
The aortic valve is a crucial component of the cardiovascular system that ensures one-way blood flow from the left ventricle to the aorta, playing a key role in maintaining efficient cardiac function. Structurally, the valve consists of three cusps attached to a fibrous annulus, with its integrity dependent on the annulus geometry and the ratio of annulus to cusp area to prevent regurgitation and ensure valve competence. The valve’s complexity is further highlighted by its proximity to the esophagus, allowing for detailed visualization through transesophageal echocardiography (TEE), and the mechanical stresses it experiences, including shear, bending, tensile, and compressive forces, which can impact cellular responses and potentially lead to pathological changes. Advances in valve repair and replacement, such as percutaneous approaches for implanting bioprosthetic valves, demonstrate ongoing progress in treating aortic valve diseases. These diseases, often without medical cures, emphasize the importance of understanding the valve’s anatomy, pathology, and the mechanical and biological interactions within this intricate structure. The aortic root, which includes the lower part of the ascending aorta, sinotubular junction, annulus, cusps, and aortic sinus of Valsalva, plays a significant role in the valve’s function and is a focal point for surgical interventions. Diagnostic evaluations, including detailed echocardiographic examinations and Doppler imaging, are essential for assessing valve disease, with parameters such as transvalvular velocity, pressure gradients, and valve orifice planimetry providing crucial diagnostic information. Overall, these insights into the structure, function, and challenges in repairing and replacing the aortic valve highlight the complexity of this vital cardiac component and the importance of multidisciplinary approaches in managing aortic valve diseases.
3. Ascending aorta
The ascending aorta, a critical portion of the aortic artery, possesses distinct anatomical and physiological features that set it apart from other sections of the aorta. It originates from the aortic valve and extends to the aortic arch, playing a crucial role in the cardiovascular system by facilitating the flow of blood from the heart to the rest of the body. The ascending aorta is known for its high concentration of elastic fibers, which contribute to its compliance and the Windkessel effect, enabling it to efficiently absorb and redistribute the energy generated by the heart’s systolic function. This segment is vulnerable to various pathologies, such as ascending aortic aneurysms, characterized by a dilatation resulting in a cross-sectional diameter more than 1.5 times its normal value, and dissections, often linked to genetic abnormalities rather than atherosclerotic changes. The development of these conditions can be influenced by biomechanical alterations, leading to inefficiencies and potential structural failure of the aorta. Additionally, the ascending aorta can be impacted by atypical coarctations, typically secondary to conditions like vasculitis or genetic disorders, and is a potential site for thrombus formation, which can have serious clinical consequences if not promptly addressed. Advances in imaging and computational algorithms have significantly enhanced the detection, segmentation, and measurement of the ascending aorta, aiding in the diagnosis and monitoring of its diseases. These technological advancements, combined with a deeper understanding of the ascending aorta’s biomechanics and pathophysiology, are essential for developing targeted therapies and surgical interventions to effectively manage its disorders.
4. Aortic arch
The aortic arch is a crucial part of the aorta located between the ascending and descending aorta. It plays a key role in systemic circulation by distributing oxygenated blood from the left ventricle to the body. Structurally, it originates from the ascending aorta, arches backward and to the left of the trachea, and transitions into the descending aorta at the level of the fourth thoracic vertebra. The aortic arch gives rise to three major branches: the brachiocephalic trunk, the left common carotid artery, and the left subclavian artery, which supply blood to the head, neck, and arms. Variations in the branching pattern of the aortic arch are common, with differences in the distance between the origins of these branches and the number of branches. Some individuals may have variations such as a direct origin of the left vertebral artery from the arch. These anatomical variations have significant clinical implications, particularly in surgical and diagnostic procedures. The unique three-dimensional geometry and flow dynamics of the aortic arch are believed to contribute to the development of serious aortic diseases, including aneurysms. Pathologies involving the aortic arch, such as aneurysms and dissections, present complex surgical challenges, with evolving techniques and prostheses aimed at simplifying operations and reducing surgical time. Congenital variants and anomalies of the aortic arch, which may be associated with vascular rings, congenital heart disease, and chromosomal abnormalities, highlight the importance of recognizing these conditions for prognosis and management. Therefore, the anatomy, variations, and associated pathologies of the aortic arch emphasize its significance in cardiovascular health and disease.
5. Descending aorta
The descending aorta is a vital component of the cardiovascular system, running from the aortic arch to the abdomen where it divides into the iliac arteries. Its anatomical path alongside the vertebral column is intricately detailed, with variations in diameter noted at different thoracic vertebrae levels, suggesting a complex relationship with surrounding structures and potential implications for gender-specific medical considerations. Acute aortic syndromes (AAS), such as aortic dissection, intramural hematoma, and penetrating aortic ulcer, are serious conditions affecting this region, with management options ranging from surgery to observation and medical treatment depending on the specific type and presence of complications. The descending aorta’s susceptibility to these conditions is further underscored by case studies demonstrating the life-threatening nature of penetrating ulcers and the risk of catastrophic rupture, highlighting the importance of prompt and effective intervention. Advances in imaging and segmentation techniques have greatly enhanced the diagnosis and measurement of the descending aorta, enabling early disease detection and accurate assessment of aortic size, crucial for treatment planning. The complexity of managing descending aorta conditions, such as aneurysms and traumatic injuries, is evident in the pathophysiology, diagnostic methods, and clinical outcomes associated with these diseases. Recent advancements in endovascular and hybrid treatment approaches offer less invasive options for addressing distal arch and descending aortic pathologies, with ongoing research into the hemodynamic effects of assist devices implanted in the descending aorta providing insights into potential future therapeutic strategies. Overall, these studies emphasize the critical role of the descending aorta in cardiovascular health and disease, highlighting the importance of multidisciplinary approaches to optimize patient outcomes.
6. Abdominal Aorta
The abdominal aorta is a critical part of the body’s main artery, extending from the diaphragm and bifurcating into the common iliac arteries in the lower abdomen. It plays a pivotal role in supplying oxygenated blood to various tissues. This segment is dynamic, adapting to respiratory mechanics, pulsatile hemodynamics, and musculoskeletal movement, highlighting the importance of understanding its geometric changes, especially after endovascular repair. Abdominal Aortic Aneurysm (AAA) is a significant pathology that affects this artery, characterized by a focal dilation exceeding 50% of its normal diameter, primarily in males over 65 years old, and is associated with risk factors such as smoking and hypertension. The disease’s multifactorial nature involves inflammation mediated by macrophages and T-lymphocytes, leading to aortic remodeling. Diagnosis often occurs incidentally due to the asymptomatic nature of most cases, with ultrasonography being the gold standard for screening. Surgical intervention, either open or endovascular, is recommended for aneurysms exceeding 5.5 cm in diameter due to the high risk of rupture, which can be a significant emergency. Anatomical knowledge of the abdominal aorta and its branches is crucial for surgical approaches, with cadaveric dissection providing valuable insights into various access strategies. Radiologists play a vital role in diagnosing AAA and its complications, using imaging to identify signs of instability or rupture. The evolution of treatment strategies, including the development of stents and endovascular repair, has been influenced by advancements in imaging technologies and a deeper understanding of the aorta’s morphology and hemodynamics.
Diseases related with Aorta
- Aortic Aneurysm
Aortic aneurysms are a serious complication of aortic disease, characterized by the localized widening of the aortic wall, which increases the risk of rupture. These aneurysms can occur in the abdomen or chest, with abdominal aneurysms being more common and often linked to atherosclerosis. Risk factors for aortic aneurysms include older age, male sex, smoking, high blood pressure, high cholesterol levels, and a family history of the condition. The development of aortic aneurysms involves inflammatory reactions, activation of proteases, and metalloproteinases that contribute to the weakening of the aortic wall. Early detection using imaging techniques such as ultrasonography is essential to prevent complications, as rupture can result in high mortality rates. Surgical procedures, including endovascular repair, are the main treatment options for aortic aneurysms, underscoring the importance of prompt diagnosis and management to reduce the risk of rupture and associated deaths.
- Aortic Dissection
Aortic dissection is a serious condition characterized by a longitudinal tear in the aorta, requiring emergency surgical intervention. It is a highly lethal disease with unpredictable outcomes, presenting a significant challenge in clinical settings. The global incidence of aortic dissection has not been extensively studied, focusing on in-hospital mortality and follow-up results. The disease is linked to various risk factors such as high blood pressure, abnormal lipid levels, and connective tissue disorders, which increase the risk of aortic dissection. Prompt diagnosis and advanced multidisciplinary treatment are essential for managing patients with aortic dissection, with treatment approaches varying depending on the severity and location of the tear. Aortic dissection remains a major public health issue, requiring targeted screening, prevention strategies, and efforts to reduce the medical burden.
- Aortic Coarctation
Aortic coarctation is a congenital heart defect characterized by a narrowing of the descending thoracic aorta, commonly located just distal to the left subclavian artery. It is often accompanied by other cardiac anomalies such as patent arterial duct, bicuspid aortic valve, ventricular septal defect, and mitral valve abnormalities. This condition affects approximately 3 out of 10,000 live births and can present at various ages, with a high mortality rate and a mean age of death at 34 years. Surgical interventions have advanced over time, from open lateral thoracotomy to techniques such as patch aortoplasty and subclavian flap aortoplasty, with extended end-to-end anastomosis now being the preferred method due to lower re-coarctation rates. In adults, endovascular approaches with covered stent placement have become the preferred treatment, especially in cases of atypical clinical onset, providing effective management and improved outcomes.
- Aortic Stenosis
Aortic stenosis (AS) is a common valvular heart disease characterized by progressive fibro-calcific remodeling of the aortic valve cusps, resulting in obstruction and increased afterload on the left ventricle, ultimately leading to heart failure. The pathophysiology of calcific AS (CAS) is similar to atherosclerosis, involving lipid-protein complexes and potential diagnostic markers such as lipoprotein(a). Despite advancements in interventional treatments like transcatheter aortic valve implantation, determining the optimal timing for intervention remains a clinical challenge, particularly with the rising prevalence of AS due to demographic changes. Current guidelines recommend aortic valve replacement for symptomatic patients, while management of asymptomatic patients lacks proven pharmacotherapies to slow progression, underscoring the need for innovative approaches such as biomarker screening and early valve intervention guided by medical imaging.
- Aortic Regurgitation
Aortic regurgitation (AR) is a significant valvular heart disease characterized by the improper closure of the aortic valve cusps, resulting in the backflow of blood into the left ventricle. The causes of AR are varied, including acute conditions such as aortic dissection and chronic diseases like rheumatic heart disease and congenital anomalies. Various noninvasive cardiovascular imaging techniques, such as transthoracic echocardiography, cardiac magnetic resonance, and cardiac computed tomography, are essential for evaluating the mechanism, severity, and hemodynamic impact of AR on the cardiovascular system. Research has demonstrated that even mild-to-moderate AR in patients with heart failure and preserved ejection fraction can significantly worsen long-term outcomes, with AR serving as an independent predictor of major adverse cardiovascular events. Surgical advancements like transcatheter aortic valve replacement (TAVR) have transformed the treatment of AR, underscoring the importance of comprehending the underlying mechanisms and risk factors for AR development and recurrence following intervention.
- Marfan Syndrome
Marfan Syndrome (MFS) is a rare autosomal dominant connective tissue disorder caused by mutations in the FBN1 gene, resulting in multisystemic manifestations that do not show a preference for gender, race, or ethnicity. Patients with MFS are at risk of developing life-threatening cardiovascular complications, such as aortic root dilation, aortic dissection, mitral valve prolapse, and aortic insufficiency. Current evidence indicates that beta-blockers are the primary treatment for MFS, effectively slowing aortic enlargement, while angiotensin receptor blockers may be beneficial as an additional therapy to limit aortic growth. Aortic dissection involving the descending aorta in MFS patients poses a significant clinical challenge, with high rates of reintervention, redissection, and mortality, underscoring the importance of close monitoring and timely interventions in these individuals. Regular assessment, evaluation of genetic history, and comprehensive preventive therapeutic strategies are essential in the management of MFS to enhance patient outcomes.
- Giant Cell Arteritis
Giant Cell Arteritis (GCA) is a significant disease associated with the aorta, primarily affecting individuals over the age of 50, with a higher prevalence in women. This granulomatous vasculitis mainly targets large arteries, such as the aorta and its main branches, leading to inflammation and subsequent remodeling of the arterial wall. The pathophysiology of GCA involves the activation of dendritic cells, recruitment of CD4 T cells, and the production of inflammatory mediators such as IFN-γ and IL-17, ultimately resulting in destruction and remodeling of the vascular wall. GCA can present as cranial GCA, affecting the vessels in the head, or extracranial GCA, involving the aorta and its branches, potentially causing aneurysms and narrowing of affected vessels. Early diagnosis based on clinical signs, imaging, and inflammatory markers is essential to start appropriate treatment and prevent ischemic complications, particularly those affecting vision.
Methods to keep Aorta Healthy
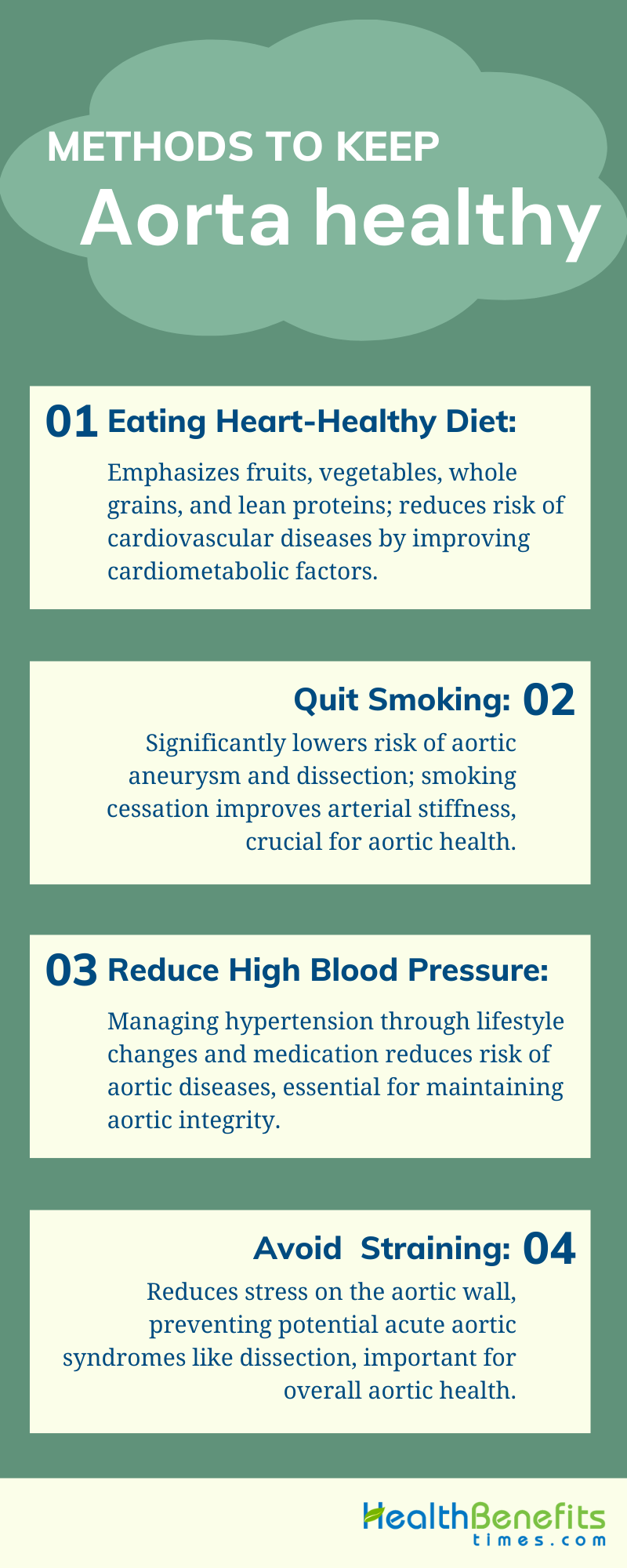
- Eating heart-healthy diet
Maintaining a healthy aorta and overall cardiovascular health is significantly influenced by dietary habits. A heart-healthy diet, as recommended by various studies, emphasizes the consumption of fruits, vegetables, legumes, whole grains, and lean protein sources while minimizing or avoiding processed foods, trans-fats, and sugar-sweetened beverages. Specific dietary patterns such as the Mediterranean, DASH, and plant-based diets have been identified as cardioprotective, reducing the risk of cardiovascular diseases (CVD). These diets not only help in managing cardiometabolic risk factors but also have a positive impact on the gut microbiome, which is linked to cardiovascular health. Moreover, the Healthy Eating Index-2015 (HEI-2015), which evaluates compliance with the Dietary Guidelines for Americans, has been associated with a lower risk of abdominal aortic calcification, indicating its role in preventing vascular calcification and CVD.
2. Quit smoking
Quitting smoking is a crucial strategy for maintaining aortic health, as supported by numerous research studies. Active smoking is strongly linked to an increased risk of aortic mortality, including deaths from aortic dissection and aneurysm, with the risk rising with the duration and intensity of smoking. Conversely, stopping smoking has been associated with a significant decrease in these risks, showing a dose-response relationship between the duration of smoking cessation and the risk of mortality from aortic aneurysm, although the link with aortic dissection mortality was weaker. The mechanisms behind smoking-induced damage to the aorta involve inflammation and oxidative stress-induced damage to the vascular wall, particularly endothelial dysfunction, which is a precursor to atherosclerosis and acute cardiovascular events. Quitting smoking is crucial for managing atherosclerotic vascular disease by addressing these mechanisms. Studies have also demonstrated that quitting smoking can lead to improvements in arterial stiffness, a marker of vascular health, although significant improvements may require prolonged cessation. Smoking is a major risk factor for abdominal aortic aneurysms (AAA), with quitting playing a key role in managing aortic disease. Long-term smoking is associated with increased risks of atherosclerosis and vascular calcification, highlighting the importance of quitting. Some studies have noted persistent vasomotor disturbances even after quitting, underscoring the importance of early cessation. Guidelines from cardiovascular scientific societies worldwide emphasize the importance of quitting smoking, along with controlling other cardiovascular risk factors, for the prevention and management of various aortic diseases. Overall, these findings emphasize the critical role of quitting smoking as a key approach to maintaining aortic health and preventing aortic diseases.
3. Reduce high blood pressure
Maintaining a healthy aorta involves various strategies to manage and reduce high blood pressure, a critical factor in preventing aortic diseases. Surgical or transcatheter repair is recommended for conditions like coarctation of the aorta to mitigate the risk of severe aortopathy and hypertension, with medical therapy paralleling that for essential hypertension, including beta blockers and angiotensin-converting enzyme inhibitors as first-line treatments. Despite the scarcity of data on specific antihypertensive agents for aortic disease, the combination of an ACE inhibitor or angiotensin receptor blocker with a calcium channel blocker and a diuretic is strongly recommended, especially for patients with resistant hypertension. Endovascular stenting has also shown promise in reducing hypertension in adults with coarctation of the aorta, demonstrating safety and effectiveness in lowering blood pressure. Innovative methods like electrical stimulation of the heart to control blood pressure have been explored, offering an alternative approach by adjusting stimulation patterns based on the patient’s needs. Lifestyle interventions, including dietary modifications to reduce salt intake and increase consumption of high-potassium fruits and vegetables, alongside targeted weight loss, have been identified as effective measures for hypertension prevention. A Mediterranean-style diet, particularly a green-Mediterranean diet enriched with plant-based foods and green tea, has been associated with significant reductions in proximal aortic stiffness, indicating its potential for aortic health improvement. Beta blockers remain the antihypertensive agents of choice for preventing aortic dissection, especially in individuals with inherited aortic wall weaknesses. Additionally, nutritional interventions like saffron extract have shown potential in preventing blood pressure increases and aortic remodeling in hypertensive rats. Comprehensive management strategies, including lifestyle interventions and pharmacotherapy, are crucial for maintaining aortic health and reducing the risk of atherosclerotic cardiovascular diseases.
4. Avoid heavy lifting or straining
Maintaining a healthy aorta is essential for cardiovascular health, as it serves as the main artery that carries oxygenated blood from the heart to the body. One important way to keep the aorta healthy is to avoid heavy lifting or straining, which can increase stress on the aortic wall and potentially lead to acute aortic syndromes, such as dissection. High-intensity strength training, in particular, has been linked to acute dissection of the ascending aorta, even in individuals without known aneurysms or a history of hypertension or collagen vascular disease. Additionally, engaging in strenuous sports or occupations that involve repetitive extreme physical activity can raise the risk of aortic aneurysm due to intense hemodynamic stress on the aorta. Dietary changes, specifically adopting a Mediterranean-style diet rich in plants, have shown potential in reducing proximal aortic stiffness, a marker of arterial aging and cardiovascular risk, highlighting the importance of lifestyle modifications for aortic health. Furthermore, avoiding manipulation of the aorta during medical procedures, as demonstrated by the no-touch aorta technique in coronary artery bypass grafting, can lower the risk of cerebrovascular accidents, underscoring the need for gentle handling of the aorta in clinical settings. Individuals with aortic enlargement should approach regular, vigorous exercise cautiously to prevent worsening aortopathy. Adhering to dietary patterns associated with low aortic stiffness may help in both primary and secondary prevention of cardiovascular diseases, emphasizing the comprehensive approach required to maintain aortic health. Overall, these strategies stress the significance of lifestyle changes, dietary modifications, and careful clinical practices in preserving aortic health and preventing aortic diseases.
Treatment and managements
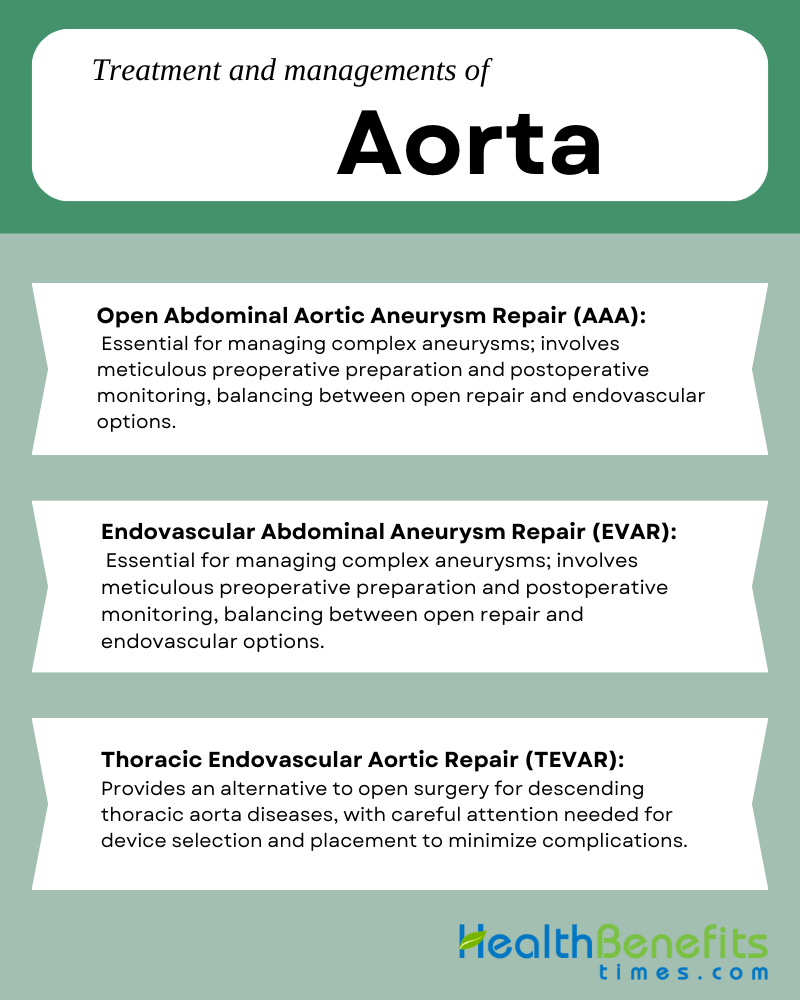
1. Open Abdominal Aortic Aneurysm Repair (AAA)
Open abdominal aortic aneurysm repair (AAA) remains a crucial procedure for managing aortic aneurysms, especially in cases where endovascular repair is not suitable or in the presence of specific conditions such as essential thrombocythemia. Careful perioperative management is necessary to prevent complications like thrombosis and bleeding. Despite advancements in endovascular technologies, open surgical repair continues to be the primary treatment for thoracoabdominal aortic aneurysms, requiring thorough preoperative preparation and a collaborative team effort to minimize perioperative risks. The open abdominal management technique, particularly in cases of ruptured AAA, has demonstrated the effectiveness of negative pressure therapy systems and the components separation technique in improving abdominal wall closure rates and outcomes. The choice between open surgical repair and the less invasive endovascular aortic aneurysm repair (EVAR) depends on various factors, including aneurysm size and patient compliance with EVAR requirements, which may not be met in all cases. Monitoring for EVAR complications using biomarkers from peripheral-blood-circulating extracellular vesicles offers a noninvasive method for early identification, underscoring the importance of postoperative care in both EVAR and open repair. While endovascular management has shown lower morbidity and better short-term prognosis, open surgery remains necessary in specific scenarios, highlighting the importance of individual evaluation for optimal AAA management. Studies have shown that open repair is safe and effective, particularly in specialized high-volume centers, despite the prevalence of endovascular procedures. The COVID-19 pandemic has presented unique challenges for emergent vascular surgeries, including open repair for ruptured AAA in COVID-positive patients, emphasizing the need for special considerations. Open surgery is recommended for various AAA conditions, including degenerative, mycotic, and those with significant accessory renal arteries, highlighting its essential role alongside EVAR.
2. Endovascular Abdominal Aneurysm Repair (EVAR)
Endovascular Abdominal Aneurysm Repair (EVAR) has become a key treatment for abdominal aortic aneurysms (AAAs), providing a less invasive option compared to open surgical repair, with the potential for lower postoperative mortality and shorter hospital stays. Originally intended for patients unsuitable for open repair, EVAR has expanded to be considered the primary treatment for thoracic and abdominal aortic conditions due to its association with improved morbidity and mortality rates. Despite its benefits, EVAR presents unique challenges, including the risk of endoleaks that require prompt identification and management for successful outcomes. The technique continues to evolve with the development of fenestrated and branch stent grafts to address more complex aneurysms. However, the effectiveness of the procedure can be influenced by patient-specific factors, such as sex, with studies suggesting that women may have worse outcomes than men, possibly due to anatomical differences. Customized aortic stent-grafts show promise in overcoming limitations of standard stents through personalized designs. While EVAR may not increase overall life expectancy in patients ineligible for open repair, it can reduce aneurysm-related mortality. In Taiwan, the widespread use of EVAR has shown effectiveness in short-term outcomes, despite a higher rate of reintervention. Comparative studies between EVAR and open repair suggest an early survival advantage for EVAR, which may diminish over time. Even in cases of giant AAAs, EVAR has been successful, demonstrating its adaptability and potential for treating challenging aneurysms. Despite differing opinions on the best treatment approach, the decision between EVAR and open surgery should be based on anatomical, clinical, and logistical factors. Additionally, the study of peripheral-blood-circulating extracellular vesicles (pbcEVs) provides a new method for monitoring EVAR-treated patients and potentially identifying biomarkers for complications like endoleaks.
3. Thoracic Endovascular Aortic Repair (TEVAR)
Thoracic Endovascular Aortic Repair (TEVAR) has become a crucial treatment option for various thoracic aortic conditions, providing a less invasive option compared to traditional open surgery with promising results in the medium to long term. While TEVAR is mainly used for diseases of the descending thoracic aorta, such as aneurysms, dissections, and intramural hematomas, advancements in device technology and techniques have expanded its use to certain cases involving the ascending aorta, particularly in patients with significant health issues or those not suitable for open surgery. Despite its advantages, TEVAR can lead to complications like endoleak, limb ischemia, and stent movement, highlighting the need for a thorough understanding of the disease process, careful selection of landing zones, and precise attention to anatomical details to minimize risks. Strategies for managing complications include addressing endoleaks with additional grafts or bypass procedures, and preventing stent migration with aortic arch repair and debranching techniques. TEVAR has been shown to be more effective than open surgery in reducing rates of illness and death, although outcomes can be affected by patient characteristics such as body mass index, with underweight patients facing higher risks of complications and endoleak. The success of the procedure also depends on thorough preoperative assessment, appropriate device selection, and accurate deployment to ensure proper sealing and anchoring within the aorta. In cases of acute aortic dissection, TEVAR can be a suitable alternative to open surgery, potentially preventing the progression to retrograde Type A dissection and reducing the complications associated with more invasive procedures. Overall, these findings emphasize the importance of tailoring TEVAR to individual patients, considering specific factors and procedural details to achieve optimal outcomes and effectively manage complications.