A viral infection occurs when a virus enters the body, invades healthy cells, and begins to multiply, often causing disease. Viruses are tiny infectious agents that can infect all types of life forms, from animals and plants to microorganisms, including bacteria and archaea. Once inside the host, viruses hijack the host’s cellular machinery to reproduce, leading to cell damage or death. Viral infections can manifest in various forms, such as respiratory illnesses like the common cold, influenza, or more severe conditions like COVID-19. The body’s immune response plays a crucial role in combating viral infections, but some viruses have evolved mechanisms to evade the immune system, making them particularly challenging to treat. Vaccination and antiviral medications are common strategies for preventing and managing viral infections.
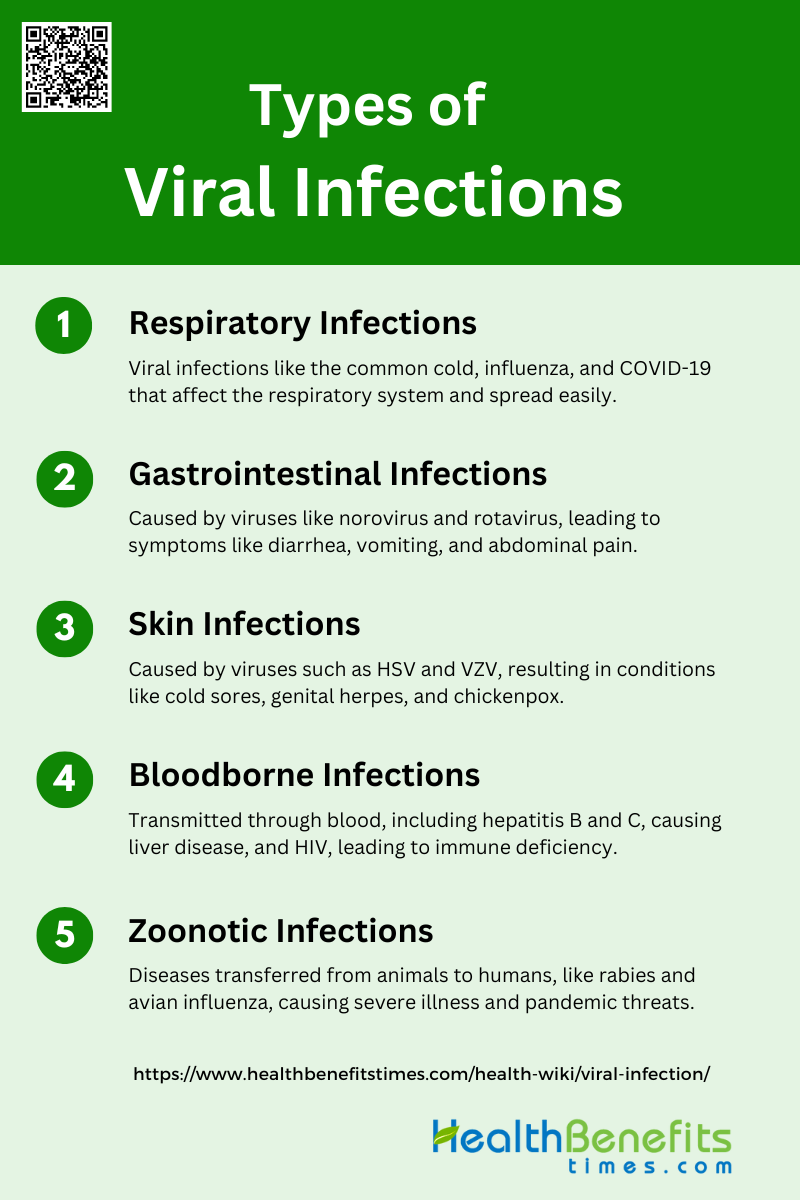
Types of Viral Infections
Viral infections are caused by viruses, which are microscopic pathogens that invade living cells to reproduce. These infections can affect various parts of the body and manifest in different forms. Understanding the types of viral infections is crucial for diagnosis, treatment, and prevention. Below are some common types of viral infections:
1. Respiratory Infections
Respiratory infections are caused by viruses that primarily affect the respiratory system, leading to illnesses such as the common cold, influenza, and COVID-19. These infections are highly contagious and can spread through respiratory droplets, causing widespread outbreaks and significant public health concerns.
- Common cold: A mild viral infection of the upper respiratory tract, primarily caused by rhinoviruses.
- Influenza: A more severe respiratory infection caused by influenza viruses, leading to seasonal flu outbreaks.
- COVID-19: A novel coronavirus infection causing severe respiratory illness, first identified in 2019.
2. Gastrointestinal Infections
Gastrointestinal infections are caused by viruses that infect the stomach and intestines, leading to symptoms such as diarrhea, vomiting, and abdominal pain. Norovirus and rotavirus are the most common viral agents responsible for these infections, particularly in children and the elderly.
- Norovirus: A highly contagious virus causing acute gastroenteritis, often leading to outbreaks in communal settings.
- Rotavirus: A leading cause of severe diarrhea in young children, preventable by vaccination.
3. Skin Infections
Skin infections caused by viruses include those from the herpes simplex virus (HSV) and varicella-zoster virus (VZV). These viruses establish latent infections in nerve cells and can reactivate, causing recurrent skin lesions and other complications.
- Herpes Simplex Virus (HSV): Causes oral and genital mucocutaneous infections, with HSV1 leading to cold sores and HSV2 to genital herpes.
- Varicella-Zoster Virus (Chickenpox and Shingles): Causes chickenpox during primary infection and shingles upon reactivation, with potential complications such as postherpetic neuralgia and neurological disorders.
4. Bloodborne Infections
Bloodborne infections are transmitted through contact with infected blood and bodily fluids. Hepatitis B and C viruses and the human immunodeficiency virus (HIV) are the primary agents, leading to chronic liver disease and immune system compromise, respectively.
- Hepatitis B and C: Viruses causing chronic liver infections, potentially leading to cirrhosis and liver cancer.
- Human Immunodeficiency Virus (HIV): A virus that attacks the immune system, leading to acquired immunodeficiency syndrome (AIDS).
5. Zoonotic Infections
Zoonotic infections are diseases transmitted from animals to humans. Rabies and avian influenza are notable examples, with rabies being almost universally fatal once symptoms appear, and avian influenza posing significant pandemic threats.
- Rabies: A deadly viral infection transmitted through animal bites, affecting the central nervous system.
- Avian influenza: A viral infection from birds that can occasionally infect humans, leading to severe respiratory illness.
Common Symptoms of Viral Infections
Viral infections can present a wide range of symptoms, often depending on the type of virus and the part of the body affected. Recognizing these symptoms early can help in seeking timely medical intervention and preventing the spread of the infection. Below are some common symptoms of viral infections:
1. Fever: Fever is a prevalent symptom in many viral infections, including respiratory and gastrointestinal viruses. It is often a result of the body’s immune response to infection, where the hypothalamus in the brain increases body temperature to help fight off the virus.
2. Fatigue: Fatigue is a common symptom associated with viral infections, often due to the body’s immune response and the energy expended in fighting the infection. Chronic fatigue syndrome, which can follow viral infections, is characterized by prolonged and severe fatigue.
3. Muscle Aches: Muscle aches, or myalgia, are frequently reported in viral infections such as influenza and viral hemorrhagic fevers. These aches are typically due to the immune response and the release of inflammatory cytokines.
4. Coughing and Sneezing: Coughing and sneezing are hallmark symptoms of viral respiratory infections. These symptoms are caused by the virus triggering an inflammatory response in the respiratory tract, leading to irritation and the need to expel the virus.
5. Gastrointestinal Symptoms: Gastrointestinal symptoms like nausea and diarrhea are common in viral gastroenteritis caused by viruses such as rotavirus and norovirus. These symptoms are part of the body’s effort to expel the virus and are often accompanied by fever and vomiting.
6. Skin Rashes: Skin rashes can occur in viral infections such as COVID-19, where symptoms may include erythematous rash, urticaria, and chickenpox-like lesions. These rashes are often due to the immune response and inflammation in the skin.
7. Headache: Headaches are a frequent symptom in viral infections, including respiratory and gastrointestinal viruses. They are often caused by the body’s immune response and the release of inflammatory mediators.
8. Runny or Congested Nose: A runny or congested nose is a common symptom of viral respiratory infections. It results from the inflammation and increased mucus production in the nasal passages as the body attempts to trap and expel the virus.
9. Body Aches and Pains: General body aches and pains are common in many viral infections, including influenza and viral hemorrhagic fevers. These symptoms are typically due to the immune response and the release of inflammatory cytokines.
10. Swollen Lymph Nodes: Swollen lymph nodes are a common symptom of viral infections as the lymphatic system works to filter out the virus and produce immune cells to fight the infection. This swelling is a sign of the body’s active immune response.
11. Loss of Appetite: Loss of appetite is frequently observed in viral infections, particularly those affecting the gastrointestinal system. This symptom is often due to the body’s stress response and the release of inflammatory cytokines.
Causes of Viral Infections
Viral infections are caused by various factors that enable viruses to invade and multiply within the host’s body. These factors can range from direct contact with infected individuals to exposure to contaminated surfaces or vectors like insects. Understanding the causes of viral infections is essential for effective prevention and control. Below are some common causes of viral infections:
1. Person-to-person contact
Person-to-person contact is a significant mode of transmission for various viral infections. For instance, the hepatitis A virus (HAV) is primarily spread through direct contact with an infected person or by ingesting contaminated food or water. Similarly, respiratory syncytial virus (RSV) and rhinovirus, which cause respiratory infections, are often transmitted through direct contact with infected individuals or contaminated objects. The high infectivity of these viruses means that even asymptomatic individuals can contribute to the spread, leading to secondary infections and larger outbreaks. Effective prevention strategies include maintaining good personal hygiene and minimizing close contact with infected individuals.
2. Droplet transmission
Droplet transmission occurs when virus-laden droplets are expelled from an infected person through coughing, sneezing, or talking and are inhaled by a nearby individual. This mode of transmission is particularly relevant for respiratory viruses such as influenza and SARS-CoV-2. Studies have shown that droplets can travel short distances and deposit on mucosal surfaces, leading to infection. The COVID-19 pandemic has underscored the importance of droplet transmission, with measures such as mask-wearing and social distancing being crucial in mitigating the spread. Understanding the dynamics of droplet transmission helps in formulating effective public health interventions.
3. Contaminated food and water
Contaminated food and water are common sources of viral infections, particularly in resource-poor settings. Hepatitis E virus (HEV) and HAV are notable examples, often causing large-scale outbreaks through fecally contaminated water and food. Foodborne viruses like norovirus and HAV can be transmitted via ingestion of contaminated food items, especially those handled by infected individuals. Preventive measures include ensuring safe food handling practices, proper sanitation, and vaccination for at-risk populations. The role of food handlers in the transmission of these viruses highlights the need for stringent hygiene practices in the food industry.
4. Weakened immune system
Individuals with weakened immune systems are more susceptible to viral infections due to their reduced ability to mount an effective immune response. This increased vulnerability can result from underlying health conditions, immunosuppressive treatments, or age-related immune decline. For example, the severity of HAV infection increases with age and pre-existing liver disease. Similarly, immunocompromised individuals are at higher risk of severe outcomes from respiratory viruses like influenza and SARS-CoV-2. Protecting these populations involves targeted vaccination, prophylactic treatments, and minimizing exposure to potential sources of infection.
5. Poor hygiene practices
Poor hygiene practices significantly contribute to the spread of viral infections. Inadequate handwashing, improper food handling, and lack of sanitation facilities can facilitate the transmission of viruses like HAV and norovirus. The COVID-19 pandemic has highlighted the critical role of personal hygiene, including regular handwashing and surface disinfection, in preventing virus spread. Emphasizing good hygiene practices, especially in healthcare and food service settings, is essential for controlling outbreaks and reducing the burden of viral diseases.
6. Crowded living conditions
Crowded living conditions can exacerbate the spread of viral infections due to the increased likelihood of close contact and shared surfaces. Respiratory viruses such as RSV and influenza are more easily transmitted in densely populated environments, where maintaining physical distance is challenging. The rapid spread of SARS-CoV-2 in crowded settings has further demonstrated the impact of population density on viral transmission. Public health measures, including improving living conditions and reducing overcrowding, are vital for mitigating the spread of infections in such environments.
7. Insect bites
Insect bites are a less common but significant mode of transmission for certain viral infections. While not all viruses are transmitted this way, some, like the Zika virus and dengue virus, rely on insect vectors such as mosquitoes for their spread. These viruses are not covered in the provided data, but it is important to note that controlling insect populations and protecting against bites are crucial strategies for preventing these types of infections.
8. Mother to child
Vertical transmission, or mother-to-child transmission, can occur during pregnancy, childbirth, or breastfeeding. For example, HEV can be transmitted from an infected mother to her fetus, leading to high fetal and perinatal mortality. Similarly, while the transmission of SARS-CoV-2 from mother to child is rare, it remains a concern, particularly during delivery and breastfeeding. Preventive measures include screening and treating pregnant women for infections and providing appropriate medical care during and after childbirth to minimize the risk of transmission.
9. Bodily fluids
Transmission through bodily fluids, such as blood, saliva, and semen, is a well-documented route for several viral infections. Bloodborne viruses like HEV can be transmitted through blood transfusions, necessitating the screening of blood donors for HEV RNA. Similarly, the presence of viral RNA in saliva highlights the potential for transmission through saliva-contaminated surfaces or direct contact. Ensuring the safe handling of bodily fluids and implementing rigorous screening protocols are essential for preventing the spread of these infections.
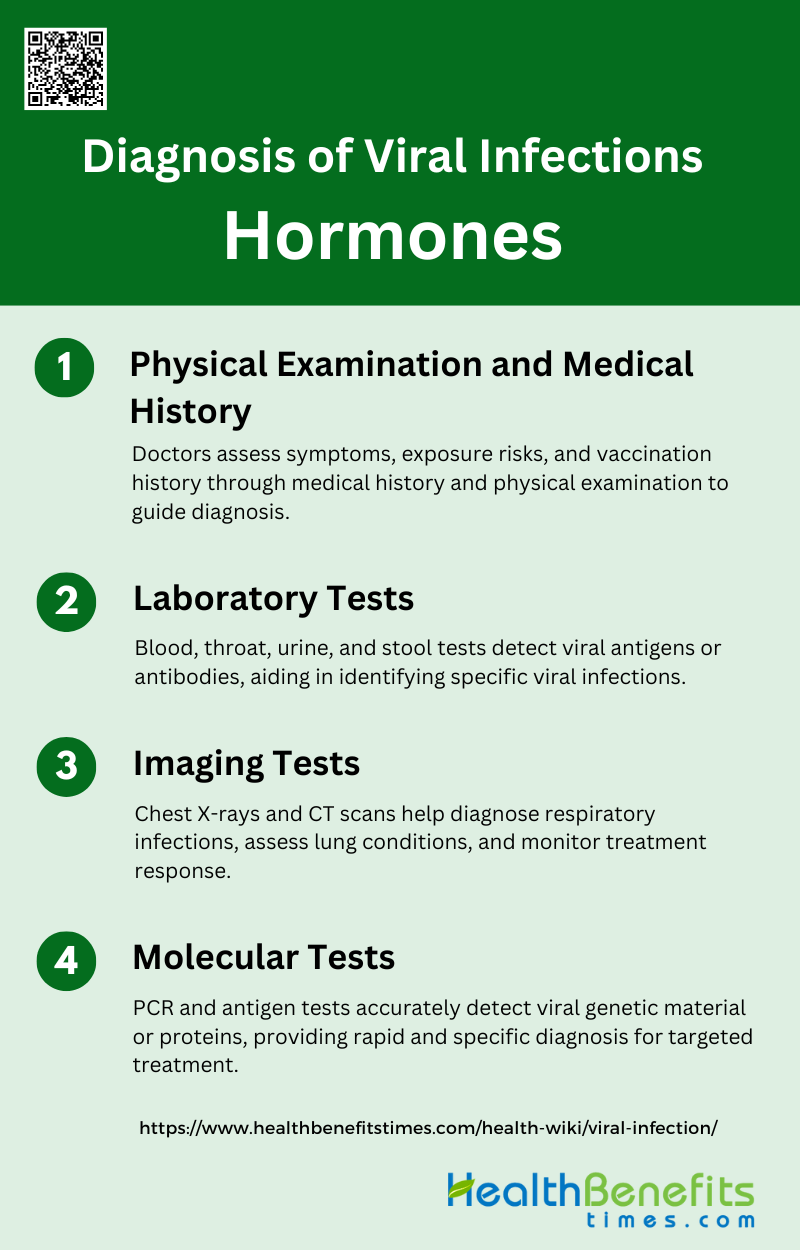
Diagnosis of Viral Infections
Diagnosing viral infections involves a combination of clinical evaluation, laboratory tests, and imaging studies. Accurate diagnosis is crucial for determining the appropriate treatment and managing the spread of the infection. Below are some common methods used for diagnosing viral infections:
1. Physical Examination and Medical History
When diagnosing viral infections, doctors start by taking a detailed medical history to understand the patient’s symptoms, their duration, and any potential exposure to infectious agents. They inquire about recent travel, contact with sick individuals, and vaccination history to assess risk factors. A thorough physical examination follows, during which doctors check vital signs and look for signs of infection, such as fever, rash, or respiratory distress. This comprehensive assessment helps in identifying the type of viral infection and guides further diagnostic testing, ensuring a targeted and effective approach to treatment.
2. Laboratory Tests
Laboratory tests play a crucial role in diagnosing viral infections. Blood tests can detect the presence of viral antigens or antibodies, providing evidence of an active or past infection. Throat swabs are often used to collect samples from the respiratory tract, which can be analyzed for viral pathogens. Urine tests may be conducted to identify viruses that affect the urinary tract, while stool samples can help detect gastrointestinal viruses. These tests provide valuable information about the viral load and the specific virus involved, aiding in accurate diagnosis and informing treatment decisions.
3. Imaging Tests
Imaging tests are essential tools for diagnosing respiratory viral infections. Chest X-rays are commonly used to visualize the lungs and detect abnormalities such as pneumonia or fluid accumulation, which may indicate a viral infection. CT scans offer a more detailed view, allowing for the assessment of lung tissue and the identification of complications like lung inflammation or damage. These imaging techniques help doctors evaluate the severity of the infection and monitor the patient’s response to treatment, providing a comprehensive understanding of the impact of the virus on the respiratory system.
4. Molecular Tests
Molecular tests, such as PCR (Polymerase Chain Reaction) tests, are highly sensitive and specific methods for detecting viral infections. PCR tests amplify viral genetic material, allowing for the identification of even small amounts of virus in a sample. Antigen tests, on the other hand, detect specific proteins from the virus, providing rapid results. These tests are crucial for diagnosing infections with high accuracy and are especially valuable for detecting viruses that are difficult to culture in the laboratory. Molecular tests enable precise identification of the virus, facilitating timely and appropriate treatment decisions.
Treatment of Viral Infections
Treating viral infections involves various approaches aimed at alleviating symptoms, reducing viral load, and preventing complications. The choice of treatment depends on the type of virus and the severity of the infection. Below are some common methods used for treating viral infections:
1. Antiviral Medications
Antiviral medications are crucial in the treatment of viral infections, particularly for respiratory viruses such as influenza, respiratory syncytial virus (RSV), and coronaviruses. Historically, M2 inhibitors like amantadine and rimantadine were used for influenza A, but resistance has rendered them ineffective. Currently, neuraminidase inhibitors are the primary antiviral class for treating influenza. For RSV, the monoclonal antibody palivizumab and the antiviral ribavirin are available, though their efficacy is limited. Emerging therapies, including novel antiviral agents and combination therapies, are being developed to enhance treatment efficacy and address drug resistance.
2. Stay Hydrated
Staying hydrated is a fundamental aspect of managing viral infections, particularly those affecting the respiratory tract. Adequate hydration helps maintain mucosal moisture, which is essential for the proper functioning of the respiratory system and the immune response. For instance, in the treatment of RSV, supportive care including hydration and oxygenation is critical, especially in severe cases involving infants and the elderly. Hydration supports overall health and can alleviate symptoms such as sore throat and congestion, making it a simple yet effective measure in the management of viral infections.
3. Get Plenty of Rest
Rest is a vital component in the recovery from viral infections. It allows the body to allocate energy towards the immune response, facilitating the fight against the virus. During rest, the body can repair tissues and produce immune cells more efficiently. For example, in the case of RSV, supportive care that includes rest is essential for recovery, particularly in vulnerable populations like infants and the elderly. Ensuring adequate rest can help reduce the severity and duration of symptoms, contributing to a quicker recovery.
4. Use Over-the-Counter Medications for Symptom Relief
Over-the-counter (OTC) medications play a significant role in alleviating symptoms of viral infections. These medications can help manage fever, pain, congestion, and cough, providing symptomatic relief. For instance, black elderberry (Sambucus nigra) has been shown to effectively reduce upper respiratory symptoms, offering a safer alternative to prescription drugs for common colds and influenza. While OTC medications do not cure the infection, they can significantly improve the quality of life during the illness and help manage discomfort.
5. Use a Humidifier to Ease Respiratory Symptoms
Using a humidifier can be beneficial in easing respiratory symptoms associated with viral infections. Humidifiers add moisture to the air, which can help soothe irritated nasal passages and throat, reduce congestion, and make breathing easier. This is particularly useful in conditions like RSV, where maintaining airway moisture is crucial for symptom management. By keeping the respiratory tract moist, humidifiers can help prevent complications and promote comfort during the course of the infection.
6. Vaccines
Vaccines are a cornerstone in the prevention of viral infections. They work by stimulating the immune system to recognize and combat specific viruses. For instance, vaccines for influenza and the development of vaccines for RSV are critical in reducing the incidence and severity of these infections. Despite the challenges in developing vaccines for rapidly mutating viruses like influenza, ongoing research and advancements in vaccine technology hold promise for more effective prevention strategies. Vaccination remains one of the most effective public health measures to control viral infections.
7. Emerging Therapies
Emerging therapies for viral infections are focused on improving treatment efficacy and overcoming resistance. Novel antiviral agents, combination therapies, and immunomodulatory drugs are being developed to target various stages of viral replication and enhance the immune response. For example, ALX-0171, a trivalent Nanobody, has shown promise in reducing RSV viral load in hospitalized children, although clinical outcomes need further improvement. Additionally, the re-emergence of natural remedies and the exploration of medicinal plants with antiviral properties offer potential new avenues for treatment. These innovative approaches are essential in addressing the unmet medical needs in viral infection management.
Preventive measures of Viral Infections
Preventing viral infections requires a combination of personal hygiene, vaccination, and public health measures. These strategies are essential to reduce the spread of viruses and protect vulnerable populations. Below are some common preventive measures for viral infections:
1. Vaccinations
Vaccinations are a cornerstone in the prevention of viral infections. They work by stimulating the immune system to recognize and combat pathogens, such as viruses and bacteria, without causing the disease itself. Vaccines have been instrumental in controlling and even eradicating diseases like smallpox and polio. In the context of respiratory viruses, such as influenza and COVID-19, vaccines have shown to significantly reduce the incidence and severity of infections. For instance, the rapid development and deployment of COVID-19 vaccines have been crucial in controlling the pandemic and reducing mortality rates. Vaccinations not only protect the individual but also contribute to herd immunity, thereby protecting the community at large.
2. Wash Hands Frequently
Frequent hand washing is a simple yet highly effective measure to prevent the spread of viral infections. The World Health Organization (WHO) recommends regular hand washing with soap and water as a primary defense against pathogens, including the SARS-CoV-2 virus responsible for COVID-19. Hand washing removes germs, including viruses, from the skin, thereby reducing the likelihood of transmission through contact with contaminated surfaces or direct person-to-person contact. This practice is particularly important in public spaces and healthcare settings where the risk of infection is higher. Hand sanitizers with at least 60% alcohol can be used as an alternative when soap and water are not available.
3. Stay Away from Sick People
Maintaining physical distance from individuals who are sick is another crucial preventive measure. Respiratory viruses, such as the flu and COVID-19, are primarily spread through droplets expelled when an infected person coughs, sneezes, or talks. These droplets can travel several meters and infect others who are in close proximity. By staying away from sick individuals, one can significantly reduce the risk of inhaling these infectious droplets. This measure is particularly important in indoor environments where ventilation may be limited, and the virus can linger in the air for extended periods. Social distancing, along with other measures like wearing masks, can effectively reduce the transmission of viral infections.
4. Don’t Share Personal Items
Avoiding the sharing of personal items such as utensils, towels, and toothbrushes is essential in preventing the spread of viral infections. Many viruses can survive on surfaces for varying periods, making it possible for them to be transmitted through shared items. For example, the SARS-CoV-2 virus can remain viable on surfaces like plastic and stainless steel for up to 72 hours. By not sharing personal items, individuals can minimize the risk of indirect transmission. This practice is particularly important in communal living settings, such as dormitories and nursing homes, where the close quarters can facilitate the spread of infections.
5. Maintain a Healthy Diet
A balanced diet rich in essential nutrients is vital for maintaining a robust immune system, which is the body’s primary defense against viral infections. Nutrients such as vitamins A, C, D, and trace elements like zinc and selenium have been shown to enhance immune function. For instance, vitamin D plays a crucial role in modulating the immune response, and its deficiency has been linked to increased susceptibility to infections. Similarly, zinc is essential for the normal development and function of immune cells. Consuming a diet that includes a variety of fruits, vegetables, lean proteins, and whole grains can provide the necessary nutrients to support immune health and reduce the risk of viral infections.
6. Get Adequate Sleep
Adequate sleep is essential for maintaining a healthy immune system. During sleep, the body undergoes various restorative processes, including the production of cytokines, which are proteins that help fight infections and inflammation. Chronic sleep deprivation can weaken the immune response, making individuals more susceptible to viral infections. Studies have shown that people who do not get enough sleep are more likely to catch common colds and other respiratory infections. Ensuring 7-9 hours of quality sleep per night can help bolster the immune system and improve overall health, thereby reducing the risk of viral infections.
7. Take Vitamins, Especially Vitamin C, D, and Zinc
Supplementing with vitamins and minerals, particularly vitamin C, vitamin D, and zinc, can enhance the immune system’s ability to fight off viral infections. Vitamin C is known for its antioxidant properties and its role in supporting various cellular functions of the immune system. Vitamin D is crucial for immune modulation, and its deficiency has been associated with increased susceptibility to infections. Zinc is essential for the normal development and function of immune cells. Clinical trials have shown that these micronutrients can be beneficial in preventing and managing viral respiratory infections, especially in populations with nutritional deficiencies.
8. Improve Indoor Air Quality
Improving indoor air quality is a critical measure in preventing the spread of airborne viral infections. Poor ventilation can lead to the accumulation of virus-laden droplets in indoor environments, increasing the risk of transmission. Strategies to enhance indoor air quality include regular ventilation, humidity control, and air filtration. Mechanical ventilation systems that incorporate air changes and filtration can effectively reduce the concentration of airborne viruses. Additionally, innovative approaches such as the use of antiviral treatments like propylene glycol can inactivate infectious bioaerosols, further reducing the risk of transmission. National authorities should acknowledge the importance of indoor air quality in infection control and implement appropriate measures.
FAQs
1. Can viral infections affect mental health?
Yes, viral infections can sometimes affect mental health. Some infections, like viral encephalitis or post-viral fatigue syndrome, may lead to symptoms such as confusion, depression, or anxiety. Additionally, the physical stress of fighting an infection and the social isolation due to contagious illnesses can impact mental well-being.
2. How long does a typical viral infection last?
The duration of a viral infection varies depending on the type of virus and the individual’s immune response. Some viral infections, like the common cold, may resolve within a few days, while others, such as mononucleosis, can last for weeks or even months.
3. Can viral infections be completely cured?
Not all viral infections can be completely cured. While many can be managed effectively with supportive care or antiviral medications, some, like HIV, result in chronic conditions that require ongoing treatment to manage symptoms and viral load.
4. Are viral infections always contagious?
While most viral infections are contagious, the degree and duration of contagiousness can vary. Some viruses are highly contagious through direct contact or respiratory droplets, while others may require specific conditions or vectors, such as mosquito bites, for transmission.
5. What role does genetic predisposition play in susceptibility to viral infections?
Genetic predisposition can affect an individual’s susceptibility to certain viral infections. Factors such as genetic variations in immune system genes can influence how effectively a person’s body responds to a virus, potentially making them more or less prone to infections.
6. Can you be reinfected with the same virus?
Yes, it is possible to be reinfected with the same virus, especially if the immune response from the initial infection was not strong or long-lasting. Some viruses, like the common cold, have multiple strains, making reinfection more likely.
7. Are there any specific dietary recommendations for people recovering from a viral infection?
While there are no universal dietary recommendations for all viral infections, consuming a balanced diet rich in vitamins, minerals, and antioxidants can support the immune system during recovery. Hydration and adequate protein intake are also important.
8. Can viral infections cause complications in pregnancy?
Yes, certain viral infections, such as rubella, cytomegalovirus (CMV), and Zika virus, can cause complications during pregnancy, including birth defects, miscarriage, or preterm birth. Pregnant women are often advised to take precautions to avoid exposure to these viruses.
9. How do antiviral medications differ from antibiotics?
Antiviral medications specifically target viruses, while antibiotics are designed to treat bacterial infections. Antivirals work by inhibiting viral replication, while antibiotics kill or inhibit the growth of bacteria. Using antibiotics for viral infections is ineffective and can contribute to antibiotic resistance.
10. Can lifestyle changes help prevent viral infections?
Yes, certain lifestyle changes, such as maintaining a healthy diet, exercising regularly, getting adequate sleep, and practicing good hygiene, can strengthen the immune system and reduce the risk of viral infections.