Vanilloid Receptor 1 (VR1), also known as Transient Receptor Potential Vanilloid 1 (TRPV1), is a nonselective cation channel predominantly expressed in sensory neurons. It plays a crucial role in the mediation of nociceptive signaling, which is the process by which painful stimuli are transmitted to the central nervous system. TRPV1 is activated by a range of physical and chemical stimuli, including capsaicin (the active component in chili peppers), heat, and protons, making it a key player in the sensation of pain and inflammatory thermal hyperalgesia. This receptor is involved in various pain pathways, including inflammatory and neuropathic pain, and is considered a potential target for developing analgesic drugs. Additionally, TRPV1 is implicated in cardiac nociception and modulating reflex responses to cardiac stress, highlighting its diverse physiological roles.
Structure and Location of Vanilloid Receptor 1
1. Description of VR1 Structure
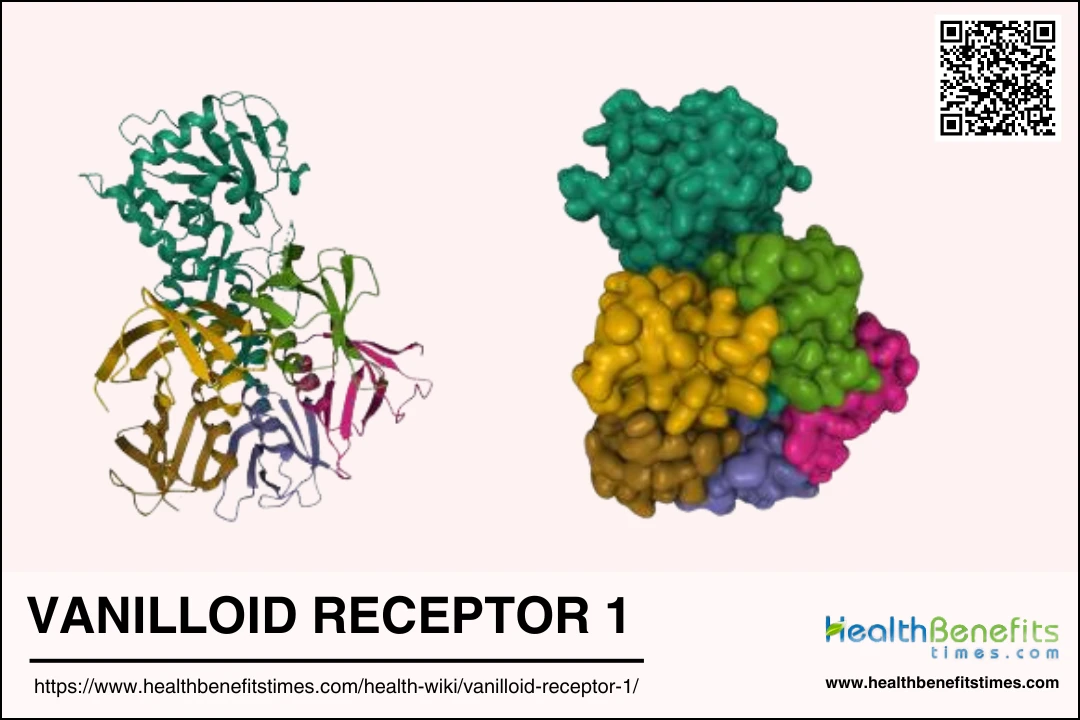
Vanilloid Receptor 1 (VR1), also known as TRPV1, is a ligand-gated ion channel that is activated by capsaicin, heat, and protons. Structurally, VR1 is a tetramer, with each subunit contributing to the formation of the ion channel pore. The receptor is glycosylated at the N604 site, which is located extracellularly, confirming its role as the exclusive site of glycosylation. The receptor’s quaternary structure predominantly forms homotetramers, as evidenced by co-immunoprecipitation and polyacrylamide gel electrophoresis studies. Key amino acids, Arg-114 and Glu-761, located in the N- and C-cytosolic tails respectively, are crucial for ligand binding.
2. Key Components and Functionalities
VR1 functions as a molecular integrator of various painful stimuli, including capsaicin, acid, and high temperature. It is a nonselective cation channel that allows the influx of calcium and sodium ions upon activation. The receptor’s glycosylation at N604 is essential for its proper folding and function. VR1 is involved in nociception, the sensory perception of pain, and is activated by endogenous ligands such as anandamide. The receptor’s ability to form multimers adds to its functional complexity, influencing its pharmacological properties. Additionally, VR1’s interaction with other proteins, such as the P2X3 purinoceptor, suggests a role in complex signaling pathways.
3. Locations and Distribution in the Body
In the central nervous system, VR1-expressing neurons are found throughout the neuroaxis, including the cortex, hippocampus, hypothalamus, and cerebellum. In the peripheral nervous system, VR1 is predominantly expressed in primary sensory neurons, such as those in the dorsal root and trigeminal ganglia. VR1 is also present in non-neuronal tissues, including the sarcoplasmic reticulum of skeletal muscle, where it regulates calcium release. Additionally, VR1 is found in the gastrointestinal tract, particularly in vagal afferent neurons and the myenteric plexus. This widespread distribution indicates VR1’s involvement in various physiological processes beyond pain perception, such as emotion regulation and gastrointestinal function.
Mechanism Action of Vanilloid Receptor 1
1. How VR1 functions at the cellular level
Vanilloid Receptor 1 (VR1), also known as TRPV1, is a non-selective cation channel that plays a crucial role in the sensation of thermal and inflammatory pain. It is primarily expressed in small to medium-sized neurons within the dorsal root and trigeminal ganglia, and is transported to both central and peripheral processes of these neurons. VR1 is activated by various stimuli, including harmful heat, extracellular protons, and vanilloid compounds like capsaicin. Upon activation, VR1 allows the influx of cations, particularly calcium ions, which leads to depolarization of the neuron and the initiation of pain signals. Additionally, VR1 is involved in apoptotic pathways in thymocytes, indicating its broader role in cellular responses to harmful stimuli.
2. Interaction with stimuli (e.g., heat, capsaicin)
VR1 is a polymodal receptor that can be activated by multiple types of stimuli, including heat, acidic conditions, and capsaicin, the active component in chili peppers. Capsaicin binds to VR1 and induces conformational changes that open the channel, allowing cation influx and subsequent neuronal depolarization. Heat and protons also activate VR1, but the molecular mechanisms differ from those of capsaicin activation. For instance, mutations in the pore domain of VR1 affect its sensitivity to capsaicin but not to heat or acidic pH, suggesting distinct activation pathways. Additionally, endogenous ligands like N-arachidonoyl-dopamine (NADA) can activate VR1 with potency similar to capsaicin, further highlighting the receptor’s role in detecting various noxious stimuli.
3. Signal transduction pathways involving VR1
The activation of VR1 initiates several signal transduction pathways that contribute to its role in pain sensation and inflammation. Protein kinase C (PKC) is a significant modulator of VR1 activity. Activation of PKC enhances VR1’s response to capsaicin, heat, protons, and anandamide by increasing the probability of channel opening. This modulation is crucial for the receptor’s role in inflammatory pain, as PKC activation by pro-inflammatory peptides like bradykinin can potentiate VR1 activity. Additionally, VR1 activation leads to calcium influx, which can trigger downstream signaling cascades, including the release of neuropeptides such as substance P and calcitonin gene-related peptide (CGRP), further amplifying pain and inflammatory responses.
Functions of Vanilloid Receptor 1
Vanilloid Receptor 1 (VR1), also known as TRPV1, is a multifunctional receptor involved in various physiological and pathological processes. It plays a crucial role in pain and temperature sensation, synaptic plasticity, inflammatory responses, and several other bodily functions. Below are some of the key functions of VR1:
1. Pain and Temperature Sensation
The vanilloid receptor 1 (TRPV1) is crucial for detecting and integrating pain-producing chemical and thermal stimuli. It is predominantly expressed by sensory neurons and responds to noxious stimuli such as capsaicin, heat, and extracellular acidification. Studies involving TRPV1 knockout mice have shown that these mice lack the typical responses to capsaicin, acid, and heat, indicating that TRPV1 is essential for the sensation of pain and temperature. Additionally, TRPV1 is involved in inflammatory thermal hyperalgesia, where its activation leads to heightened sensitivity to painful thermal stimuli.
2. Synaptic Plasticity
TRPV1 is not only involved in peripheral pain sensation but also plays a significant role in synaptic plasticity within the central nervous system. It is expressed at various central synapses and can modulate neurotransmitter release and synaptic efficacy. TRPV1’s role in synaptic plasticity includes modifying the inducibility of other types of plasticity, thereby influencing activity-dependent synaptic changes. This receptor’s involvement in synaptic function is crucial for understanding its potential contributions to brain disorders and developing therapeutic treatments.
3. Inflammatory Responses
TRPV1 is activated by various endogenous inflammatory mediators, such as bradykinin, which sensitizes the receptor through second messenger signaling cascades. This sensitization leads to increased intracellular calcium levels and enhanced receptor activity, contributing to inflammatory hyperalgesia. The receptor’s activation by protein kinase C (PKC) and other signaling pathways further underscores its role in mediating inflammatory pain. These mechanisms highlight TRPV1’s importance in the body’s response to inflammation and its potential as a target for anti-inflammatory therapies.
4. Cardiovascular and Respiratory Systems
TRPV1 is also involved in cardiovascular and gastrointestinal protection. It can be activated by endogenous ligands like anandamide and exogenous agonists such as capsaicin, leading to beneficial effects on cardiovascular function. Activation of TRPV1 in sensory nerves can result in hypotensive effects and protection against cardiac and gastrointestinal injury through the release of neurotransmitters like calcitonin gene-related peptide and substance P. These findings suggest that TRPV1 is a valuable target for developing drugs to treat cardiovascular and gastrointestinal diseases.
5. Neurological Disorders
TRPV1’s expression in the brain and its role in synaptic plasticity suggest its involvement in various neurological disorders. The receptor’s ability to modulate synaptic function and neurotransmitter release indicates that it could contribute to the pathophysiology of conditions such as epilepsy, depression, and neurodegenerative diseases. Understanding TRPV1’s mechanisms in the central nervous system could lead to new therapeutic approaches for these disorders.
6. Wound Healing and Autophagy
TRPV1 is expressed in non-sensory tissues, including the epidermis, where it functions as a sensor for noxious chemical stimuli. Its activation in keratinocytes by capsaicin and acidification suggests a role in skin physiology and wound healing. Additionally, TRPV1’s involvement in calcium signaling pathways may influence cellular processes such as autophagy, which is essential for maintaining cellular homeostasis and responding to stress. These functions highlight TRPV1’s broader physiological roles beyond pain sensation.
VR1 and Capsaicin
Explanation of Capsaicin and its Relationship with VR1
Capsaicin, the active component in chili peppers, is known for its ability to produce a burning sensation. This compound specifically targets the vanilloid receptor 1 (VR1), also known as the transient receptor potential vanilloid 1 (TRPV1). VR1 is a sensory neuron-specific ion channel that detects various pain-producing stimuli, including heat, acid, and vanilloids like capsaicin. When capsaicin binds to VR1, it activates the receptor, which is primarily located on nociceptive primary afferent neurons. This activation leads to the sensation of burning pain, making VR1 a crucial player in the pain pathway.
How Capsaicin Activates VR1 and Induces the Sensation of Heat/Pain
Capsaicin activates VR1 by binding to specific sites on the receptor, causing it to open and allow the influx of cations, particularly calcium ions (Ca2+). This influx leads to depolarization of the neuron and the subsequent transmission of pain signals to the brain. The activation of VR1 by capsaicin is characterized by multiple open states of the channel, which can be influenced by the concentration of capsaicin. Additionally, VR1 can be sensitized by other factors such as protons and heat, which lower the activation threshold and enhance the pain response. This complex interaction between capsaicin and VR1 results in the characteristic sensation of heat and pain.
Use of Capsaicin in Topical Pain Relief Treatments
Capsaicin is widely used in topical formulations for pain relief, particularly in conditions like neuropathic pain and arthritis. High-concentration capsaicin patches, such as the 8% capsaicin patch, have been shown to provide effective pain relief for up to 12 weeks after a single application. The mechanism involves the defunctionalization of nociceptive nerve fibers, leading to a temporary reduction in their ability to transmit pain signals. This defunctionalization is achieved through the prolonged activation and subsequent desensitization of VR1, which can result in the degeneration and eventual regeneration of nociceptive terminals. The use of capsaicin in topical treatments offers a non-opioid alternative for managing chronic pain with minimal systemic side effects.
VR1 in Health and Disease
Vanilloid Receptor 1 (VR1) is a multifunctional receptor implicated in various health conditions and diseases. Its role extends from modulating pain and inflammatory responses to influencing cancer progression and neurodegenerative diseases. Below are some key areas where VR1 plays a significant role:
1. Chronic Pain
The vanilloid receptor 1 (VR1), also known as TRPV1, plays a significant role in chronic pain. VR1 is a cation-selective ion channel expressed on primary sensory neurons and is upregulated following inflammation and nerve damage. Studies have shown that VR1 antagonists, such as 6-aryl-7-isopropylquinazolinones, are effective in models of chronic nociceptive and neuropathic pain, indicating the potential for VR1 blockers in chronic pain treatment. Additionally, the administration of the potent TRPV1 agonist resiniferatoxin (RTX) selectively ablates nociceptive neurons, effectively blocking experimental inflammatory hyperalgesia and neurogenic inflammation, which suggests a promising therapeutic approach for managing chronic pain.
2. Inflammatory Diseases
VR1 is crucial in the context of inflammatory diseases, particularly in mediating inflammatory pain. VR1 activity is sensitized by inflammatory mediators such as protein kinase C (PKC), which enhances the receptor’s response to mild decreases in pH commonly encountered during inflammation. VR1 knockout mice exhibit reduced inflammatory hyperalgesia, underscoring the receptor’s role in inflammatory pain pathways. Furthermore, VR1 antagonists like capsazepine have been shown to reduce formalin-induced nocifensive behavior and CFA-induced mechanical hyperalgesia, highlighting VR1’s involvement in inflammatory pain and its potential as a therapeutic target.
3. Cancer
VR1 also has implications in cancer-related pain. The receptor is enriched in nociceptive neurons, and its activation can lead to calcium cytotoxicity, selectively ablating these neurons. This approach has been effective in blocking cancer pain in animal models without affecting other sensory modalities or motor functions. Additionally, VR1’s role in mediating pain through its response to noxious stimuli, such as capsaicin and heat, suggests that targeting VR1 could be a viable strategy for managing cancer pain, which is often resistant to conventional pain therapies.
4. Neurodegenerative Diseases
In neurodegenerative diseases, VR1’s role in pain perception and modulation is significant. For instance, in diabetic neuropathy, VR1 expression and function are altered, leading to increased pain sensitivity. Diabetic rats show increased capsaicin- and proton-activated currents in dorsal root ganglion neurons, which are mediated by VR1. This increased activity is associated with PKC-mediated phosphorylation and targeted expression of VR1 on the cell surface membrane, suggesting that VR1 modulation could be a therapeutic target for managing pain in neurodegenerative conditions. Additionally, VR1’s involvement in thermal hyperalgesia and its regulation by inflammatory mediators further highlight its potential role in neurodegenerative disease-related pain.
Therapeutic Implications of VR1
Vanilloid Receptor 1 (VR1) is a promising target for various therapeutic interventions due to its involvement in multiple physiological and pathological processes. Below are some key therapeutic implications of VR1:
1. Pain Management
The VR1 receptor, also known as TRPV1, has emerged as a significant target for pain management due to its role in nociceptive signaling. Activation of VR1 by agonists like capsaicin leads to an initial excitation followed by desensitization, which can effectively alleviate neuropathic pain. This desensitization mechanism is beneficial in treating various pain conditions, including diabetic neuropathy, postmastectomy pain, and herpes zoster-related neuropathic pain. Additionally, VR1 antagonists are being explored for their potential to treat chronic inflammatory pain and migraine, with several small-molecule antagonists currently in clinical trials. The dual approach of using both agonists and antagonists of VR1 offers a promising avenue for developing new analgesics that could improve the quality of life for patients suffering from chronic pain conditions.
2. Bladder Disorders
VR1 receptors are also implicated in the management of bladder disorders. Activation of VR1 by agonists such as capsaicin and resiniferatoxin (RTX) has shown promise in treating conditions like urinary bladder hyperreflexia and overactivity. These agents induce desensitization of sensory neurons, thereby reducing bladder overactivity and improving symptoms of urinary incontinence, which is particularly beneficial for elderly patients who often experience co-existing neuropathic pain and bladder disorders. The therapeutic potential of VR1 in bladder disorders is further supported by ongoing clinical trials of RTX, which has demonstrated improved tolerability compared to capsaicin. This highlights the potential of VR1-targeted therapies in providing relief for patients with bladder dysfunctions.
3. Inflammatory Diseases
VR1 receptors play a crucial role in inflammatory diseases by mediating pain and neurogenic inflammation. Increased expression of VR1 has been observed in inflamed tissues, such as the colonic nerve fibers in patients with inflammatory bowel disease, suggesting its involvement in inflammatory hyperalgesia. VR1 antagonists are being investigated for their ability to reduce inflammatory pain by blocking the receptor’s activation by endogenous agonists like protons and eicosanoids. Additionally, the downregulation of VR1 expression during vanilloid therapy may contribute to the therapeutic effects observed in inflammatory conditions. These findings underscore the potential of VR1-targeted therapies in managing inflammatory diseases and highlight the need for further research to develop effective VR1 antagonists for clinical use.