Trauma is a complex and multifaceted concept that refers to a deeply distressing or disturbing experience that overwhelms an individual’s ability to cope. It can result from various events, including physical injuries, emotional abuse, natural disasters, or witnessing violence. Trauma affects people differently, with some experiencing immediate and severe reactions, while others may develop symptoms over time. The impact of trauma can be far-reaching, affecting a person’s mental health, physical well-being, and overall quality of life. In medical contexts, trauma often refers to physical injuries that require immediate attention, with major trauma typically defined by specific criteria such as the Injury Severity Score (ISS) or the Need For Trauma Intervention (NFTI). However, the definition of trauma is continually evolving as researchers and clinicians gain a deeper understanding of its various manifestations and long-term effects on individuals and communities.
Types of Trauma
Trauma can manifest in various forms, each with unique characteristics and impacts on an individual’s mental and physical health. Understanding these different types is crucial for effective diagnosis and treatment. Below is a list of various types of trauma:
1. Acute Trauma
Acute trauma refers to a single, isolated event that causes significant distress and disruption. This type of trauma can result from incidents such as natural disasters, accidents, or sudden loss of a loved one. Acute trauma is characterized by its sudden onset and the immediate psychological and physiological responses it triggers. Individuals experiencing acute trauma may develop symptoms of acute stress disorder, which can include intrusive thoughts, heightened anxiety, and emotional numbness. The impact of acute trauma can vary, with some individuals recovering quickly while others may develop long-term conditions such as posttraumatic stress disorder (PTSD).
2. Chronic Trauma
Chronic trauma results from prolonged and repeated exposure to distressing events. This type of trauma is often associated with ongoing situations such as domestic violence, child abuse, or living in a war zone. Chronic trauma can lead to complex psychological responses, including persistent anxiety, depression, and difficulties in forming healthy relationships. The cumulative effect of chronic trauma can severely impact an individual’s mental health and overall well-being. It is important to recognize and address chronic trauma early to prevent long-term psychological damage.
3. Complex Trauma
Complex trauma involves exposure to multiple traumatic events, often of an invasive, interpersonal nature. This type of trauma is typically experienced in childhood and can include prolonged abuse or neglect. Complex trauma can disrupt a child’s development and lead to severe emotional and psychological issues in adulthood. Symptoms may include difficulties with emotional regulation, dissociation, and impaired self-concept. Treatment for complex trauma often requires a comprehensive approach that addresses the multifaceted nature of the trauma and its pervasive impact on the individual’s life.
4. Vicarious Trauma
Vicarious trauma, also known as secondary traumatic stress, occurs when individuals are indirectly exposed to trauma through their work or relationships. This is common among mental health professionals, first responders, and caregivers who work closely with trauma survivors. Vicarious trauma can lead to symptoms similar to those experienced by direct trauma survivors, including emotional exhaustion, intrusive thoughts, and a diminished sense of safety. It is crucial for those at risk to engage in self-care practices and seek support to mitigate the effects of vicarious trauma.
5. Medical Trauma
Medical trauma arises from distressing medical experiences, such as invasive procedures, chronic illness, or life-threatening diagnoses. Patients may develop anxiety, depression, or PTSD as a result of their medical experiences. Medical trauma can also affect caregivers and family members who witness the suffering of their loved ones. Addressing medical trauma involves providing psychological support alongside medical treatment to help patients and their families cope with the emotional aftermath of their experiences.
6. Sexual Trauma
Sexual trauma encompasses any unwanted sexual activity that causes physical, emotional, or psychological harm. This type of trauma can have profound and lasting effects on an individual’s mental health, leading to conditions such as PTSD, depression, and anxiety. Survivors of sexual trauma may struggle with feelings of shame, guilt, and mistrust. Effective treatment for sexual trauma often includes trauma-focused therapy, support groups, and interventions aimed at restoring a sense of safety and empowerment for the survivor.
7. Family Trauma
Family trauma involves distressing events that occur within the family unit, such as domestic violence, divorce, or the death of a family member. This type of trauma can disrupt family dynamics and lead to long-term psychological issues for all members involved. Children are particularly vulnerable to the effects of family trauma, which can impact their development and emotional well-being. Addressing family trauma requires a holistic approach that considers the needs of each family member and promotes healing within the family system.
8. Traumatic Grief
Traumatic grief occurs when the loss of a loved one is sudden, unexpected, or violent, leading to an intense and prolonged grieving process. This type of grief can be complicated by feelings of shock, anger, and guilt, and may interfere with the individual’s ability to function in daily life. Traumatic grief can also exacerbate symptoms of PTSD and depression. Supportive interventions, such as grief counseling and support groups, are essential in helping individuals navigate the complex emotions associated with traumatic grief.
9. Disaster Trauma
Disaster trauma results from large-scale events such as natural disasters, terrorist attacks, or mass shootings. These events can cause widespread devastation and affect entire communities. Individuals exposed to disaster trauma may experience acute stress reactions, PTSD, and other mental health issues. The collective nature of disaster trauma often necessitates community-wide interventions and support systems to aid in recovery. Mental health professionals play a crucial role in providing immediate and long-term support to those affected by disaster trauma.
Common Causes of Trauma
Trauma can stem from various sources, each leading to significant emotional and psychological distress. Understanding these common causes is crucial for effective prevention and intervention. Below is a list of the most frequent causes of trauma:
1. Physical abuse or assault
Physical abuse or assault is a significant cause of trauma, often leading to long-term psychological and physical consequences. Victims of physical assault, such as those who sustain traumatic brain injuries (TBI), frequently experience post-traumatic stress disorder (PTSD) and other emotional sequelae. Studies have shown that individuals who suffer from assault-related TBI report worse outcomes in terms of quality of life and PTSD symptoms compared to those injured by other means. The intentionality behind the assault exacerbates the psychological impact, making it crucial to provide targeted support and early intervention for these victims.
2. Emotional or psychological abuse
Emotional or psychological abuse, including bullying and domestic violence, can lead to severe post-traumatic stress symptoms (PTSS). Research indicates that such forms of abuse are associated with higher levels of negative beliefs and emotions, avoidance behaviors, and difficulties with sleeping and concentrating. These symptoms can be more severe than those resulting from other types of trauma, such as accidents or sudden loss. The chronic nature of emotional abuse often leads to a pervasive sense of insecurity and mistrust in the world, significantly impacting the victim’s mental health and overall well-being.
3. Neglect or abandonment
Neglect or abandonment, particularly in childhood, can have profound and lasting effects on an individual’s psychological health. Children who experience neglect often develop PTSD and other mental health issues, such as depression and anxiety. The lack of a supportive and nurturing environment can lead to difficulties in forming healthy relationships and a disturbed belief system. The trauma from neglect is often complex, involving multiple incidents over time, which can result in long-term emotional and behavioral problems that persist into adulthood.
4. Natural disasters or accidents
Natural disasters and accidents are common causes of trauma that can lead to PTSD. Events such as hurricanes, floods, and severe car accidents expose individuals to sudden, life-threatening situations that can overwhelm their coping mechanisms. Studies have shown that the prevalence of PTSD among disaster victims can be as high as 30-40%, with rescue workers also at significant risk. The sudden and unpredictable nature of these events often leads to intense fear and helplessness, contributing to the development of PTSD and other stress-related disorders.
5. War or combat
War or combat is one of the most intense stressors known to man, often resulting in high rates of PTSD among military personnel. Veterans exposed to combat frequently experience a range of mental health issues, including depression, anxiety, and substance abuse. The traumatic experiences of war, such as witnessing death and destruction, can lead to chronic PTSD, which significantly impacts the individual’s ability to function in daily life. The prevalence of PTSD in armed forces underscores the need for effective mental health support and interventions for veterans.
6. Loss of a loved one or major life changes
The loss of a loved one or major life changes, such as divorce or job loss, can be significant sources of trauma. Such events often lead to complicated grief and PTSD, particularly if the loss is sudden or unexpected. The emotional impact of losing a loved one can result in severe negative emotions, avoidance behaviors, and difficulties in concentrating and sleeping. These symptoms can persist for an extended period, affecting the individual’s overall quality of life and mental health. Support systems and therapeutic interventions are crucial in helping individuals cope with such profound losses.
7. Witnessing violence or traumatic events
Witnessing violence or traumatic events, such as domestic violence or community violence, can lead to severe psychological harm, especially in children and adolescents. Exposure to such events is associated with a range of mental health issues, including PTSD, depression, and anxiety. Children who witness violence often exhibit externalizing behaviors, such as aggression, and internalizing behaviors, such as withdrawal and fear. The psychological impact of witnessing violence can be long-lasting, affecting the child’s development and ability to form healthy relationships. Early intervention and support are essential to mitigate these effects and promote resilience.
Signs and Symptoms of Trauma
Trauma can manifest through a range of signs and symptoms, affecting an individual’s emotional, psychological, and physical well-being. Recognizing these indicators is essential for timely intervention and support. Below is a list of common signs and symptoms of trauma:
1. Emotional Symptoms
Emotional symptoms such as anxiety, fear, sadness, and anger are common responses to trauma. Individuals with post-traumatic stress disorder (PTSD) often experience strong negative emotions in response to trauma cues or reminders, which can significantly impact their daily lives. For instance, trauma-cued emotions like fear and sadness have been shown to decrease significantly following treatment, indicating their central role in PTSD symptomatology. Additionally, high levels of state anger have been associated with poorer treatment outcomes, particularly in adolescents with PTSD, suggesting that anger management may be crucial for effective therapy. These emotional responses are not only distressing but also contribute to the maintenance and exacerbation of PTSD symptoms, making them a critical focus for both research and clinical interventions.
2. Physical Symptoms
Physical symptoms such as fatigue, headaches, and difficulty sleeping are frequently reported by individuals who have experienced trauma. These symptoms can be particularly debilitating and are often linked to the body’s stress response mechanisms. For example, trauma-exposed individuals often report difficulties with sleeping and concentrating, which are common across various types of traumatic experiences. The cortisol response to traumatic stimuli has also been studied, revealing that higher cortisol levels post-trauma are associated with more adaptive emotional reactions, although they do not necessarily predict long-term PTSD symptoms. These physical manifestations of trauma can significantly impair an individual’s quality of life and are important indicators of the body’s ongoing struggle to cope with the traumatic event.
3. Behavioral Symptoms
Behavioral symptoms such as withdrawal, mood swings, and avoidance of reminders are common among trauma survivors. These behaviors are often coping mechanisms to manage the overwhelming stress and anxiety associated with trauma. For instance, avoidance of trauma-related cues is a well-documented symptom of PTSD and can lead to significant social and functional impairments. Trauma-focused rumination, or repetitive thinking about one’s distress, has been shown to exacerbate PTSD symptoms by increasing emotional reactivity to trauma reminders. Additionally, the severity of PTSD symptoms, including behavioral symptoms, can vary depending on the type of trauma experienced, with sexual trauma and domestic violence often leading to more severe avoidance behaviors. These behavioral symptoms not only affect the individual’s mental health but also their ability to engage in daily activities and maintain relationships.
4. Cognitive Symptoms
Cognitive symptoms such as confusion, trouble concentrating, and intrusive thoughts or flashbacks are hallmark features of trauma-related disorders like PTSD. Intrusive memories, which are involuntary and often emotionally charged, are a core feature of PTSD and can be highly distressing and disruptive. These cognitive disruptions can significantly impair an individual’s ability to function effectively in daily life. For example, trauma-exposed individuals often report difficulties with concentration and memory, which can affect their performance at work or school. Additionally, cognitive emotion regulation strategies, such as rumination and catastrophic thinking, have been linked to increased PTSD severity, highlighting the importance of addressing these cognitive processes in treatment. Understanding and targeting these cognitive symptoms are crucial for developing effective interventions to help trauma survivors manage their symptoms and improve their quality of life.
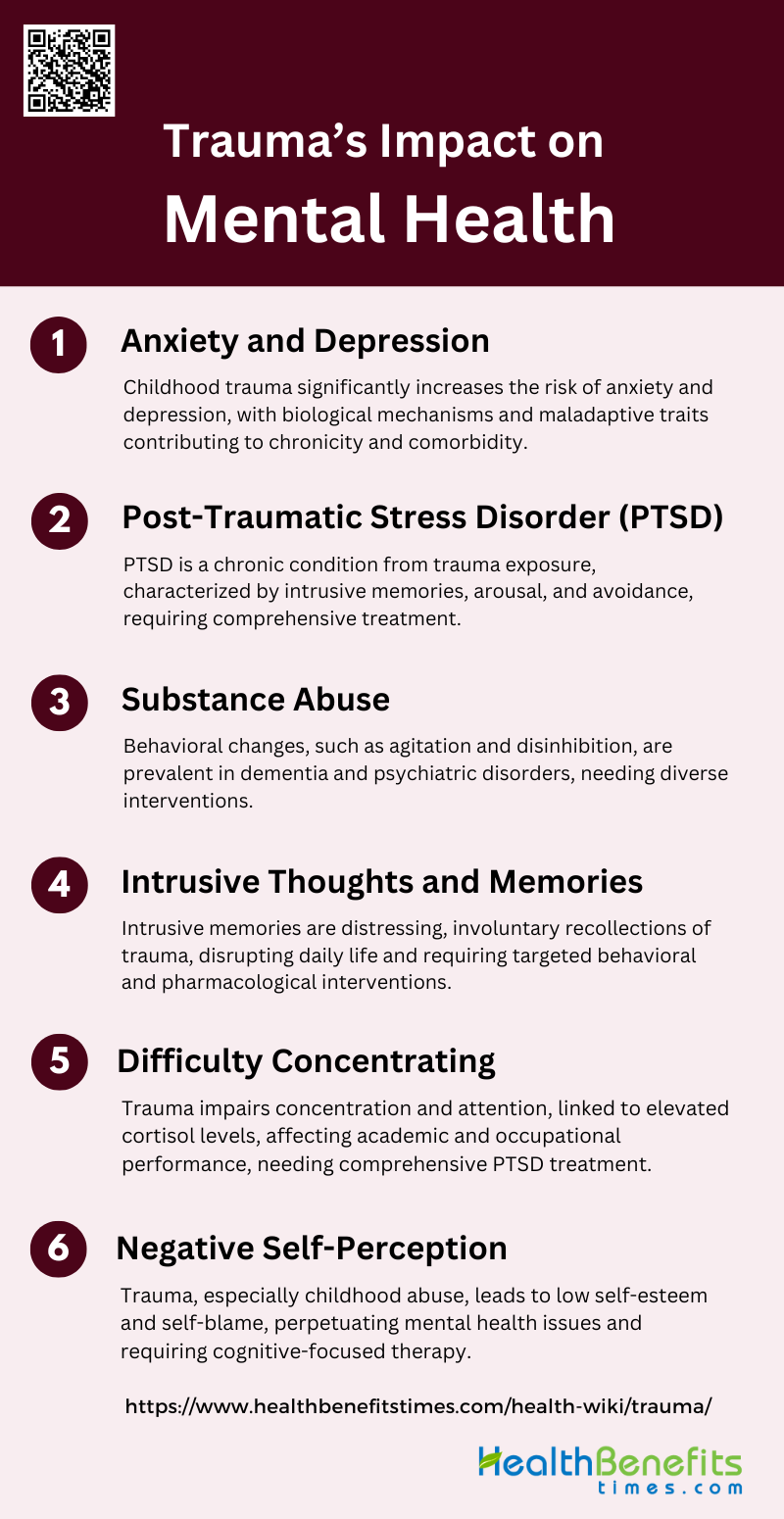
Trauma’s Impact on Mental Health
Trauma can have profound and lasting effects on an individual’s mental health, influencing various aspects of their emotional and psychological well-being. Understanding these impacts is essential for providing appropriate care and support. Below is a list of common mental health issues resulting from trauma:
1. Anxiety and Depression
Childhood trauma (CT) has been significantly linked to the development of anxiety and depressive disorders in adulthood. Studies from the Netherlands Study of Depression and Anxiety (NESDA) cohort reveal that individuals with a history of CT are at a higher risk of developing these disorders, with the strongest associations observed in those with comorbid conditions. CT not only predicts the onset of anxiety and depression but also contributes to their recurrence and poorer outcomes, including increased chronicity and comorbidity. Biological mechanisms such as heightened cortisol levels and inflammation, along with maladaptive personality traits, play a role in this increased vulnerability.
2. Post-Traumatic Stress Disorder (PTSD)
PTSD is a severe and often chronic condition that can develop following exposure to traumatic events. It is characterized by symptoms such as intrusive memories, heightened arousal, and avoidance behaviors. Research indicates that PTSD is prevalent among children and adolescents exposed to trauma, with about 16% developing the disorder. Predictors of PTSD include acute stress reactions, depression, anxiety, and insufficient psychological support. Effective treatment often involves a combination of psychoeducation, exposure therapy, coping skills training, and sometimes medication. Additionally, biological studies have shown that PTSD involves complex psychophysiological and neurobiological changes, further complicating its treatment and management.
3. Substance Abuse
The co-occurrence of PTSD and substance use disorders (SUDs) is common and leads to more severe manifestations of both conditions. Intrusive memories associated with PTSD can trigger cravings, increasing the risk of relapse in individuals with SUDs. Studies have shown that PTSD symptoms significantly elevate craving levels for substances such as alcohol, cannabis, and cocaine. This dual disorder necessitates integrated treatment programs that address both PTSD and SUDs, incorporating strategies for emotion regulation and traditional craving management. Furthermore, childhood trauma has been linked to higher rates of substance abuse in adulthood, highlighting the long-term impact of early adverse experiences.
4. Intrusive Thoughts and Memories
Intrusive memories are a core feature of PTSD and involve involuntary, distressing recollections of the traumatic event. These memories are often vivid and emotional, disrupting daily functioning. Advances in cognitive science have improved our understanding of the development and treatment of intrusive memories. Behavioral and pharmacological interventions targeting the neural and hormonal processes involved in memory formation have shown promise in reducing the frequency and intensity of these intrusions. This focus on intrusive memories offers a more targeted approach to PTSD treatment, potentially leading to more effective and scalable interventions.
5. Difficulty Concentrating
Trauma can significantly impair cognitive functions, including concentration and attention. Individuals with PTSD often report difficulties in maintaining focus, which can affect their academic and occupational performance. Biological stress responses, such as elevated cortisol levels, have been linked to these cognitive impairments. Studies have shown that heightened stress during trauma encoding can lead to more intrusive memories, which in turn disrupt concentration. Addressing these cognitive symptoms is crucial in the comprehensive treatment of PTSD, as they contribute to the overall functional impairment experienced by affected individuals.
6. Negative Self-Perception
Negative self-perception is a common consequence of trauma, particularly in individuals with a history of childhood abuse. This can manifest as low self-esteem, feelings of worthlessness, and self-blame. Research indicates that CT is associated with maladaptive personality traits and negative self-associations, which contribute to the development of anxiety and depressive disorders. These negative self-perceptions can perpetuate a cycle of mental health issues, making recovery more challenging. Therapeutic interventions that focus on improving self-esteem and altering negative cognitive patterns are essential in addressing this aspect of trauma’s impact on mental health.
Trauma Assessment and Diagnosis
Accurate assessment and diagnosis of trauma are crucial for effective treatment and recovery. This process involves various diagnostic tools and the expertise of mental health professionals. Below is a list detailing the key components of trauma assessment and diagnosis:
1. Diagnostic Criteria
The assessment of trauma-related disorders, particularly posttraumatic stress disorder (PTSD), involves a variety of diagnostic tools and criteria. The DSM-5 and ICD-11 provide distinct sets of criteria for diagnosing PTSD, which can lead to challenges in clinical practice due to their differences. Additionally, the concept of Developmental Trauma Disorder (DTD) has been proposed to address the limitations of traditional PTSD criteria, especially in children and adolescents with complex trauma histories. However, the lack of validated assessment tools for DTD remains a significant gap. Symptom validity tests are also crucial in the medicolegal context to ensure accurate diagnosis and avoid malingering. Overall, the diagnostic process must consider the specific trauma type and its associated symptomatology to provide a comprehensive evaluation
2. Professional Assessment
Mental health professionals play a critical role in the assessment and diagnosis of trauma-related disorders. They are responsible for conducting thorough clinical evaluations, which include trauma-based screenings and structured diagnostic interviews. The ethical responsibility of incorporating trauma-informed care into practice is emphasized, given the high prevalence of trauma exposure among clients in public mental health services. Professionals must be adept at differentiating between PTSD and other overlapping disorders, such as complex PTSD and developmental trauma disorder, to avoid diagnostic overshadowing. Continuous education and training in trauma-informed practices are essential for mental health professionals to stay updated on the latest assessment tools and intervention strategies. This ensures that they can provide accurate diagnoses and effective treatment plans tailored to the unique needs of trauma-exposed individuals.
Trauma Treatment
Effective trauma treatment involves various therapeutic approaches and interventions designed to help individuals heal and recover. Understanding these treatments is essential for choosing the right path to recovery. Below is a list of common trauma treatments:
1. Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy (CBT) is a widely recognized and effective treatment for post-traumatic stress disorder (PTSD). It focuses on altering negative thought patterns and behaviors associated with trauma. CBT helps patients understand and change their thoughts about the trauma, which in turn reduces the emotional impact and symptoms of PTSD. Studies have shown that CBT, particularly when trauma-focused (TF-CBT), is highly effective in reducing PTSD symptoms in both adults and children. The therapy often includes techniques such as cognitive restructuring, exposure therapy, and stress management, which collectively help patients process and cope with their traumatic experiences.
2. Prolonged Exposure (PE) Therapy
Prolonged Exposure (PE) Therapy is a specific type of cognitive-behavioral therapy that involves repeated, detailed imagining or recounting of the trauma in a safe, controlled environment. This process helps patients gradually confront their trauma-related memories, thoughts, and feelings, reducing their power over time. Prolonged Exposure has been shown to be particularly effective for PTSD, with robust evidence supporting its use. The therapy typically involves both in vivo exposure (confronting feared situations in real life) and imaginal exposure (revisiting the trauma memory). PE helps patients reduce avoidance behaviors and improve their overall functioning.
3. Cognitive Processing Therapy (CPT).
Cognitive Processing Therapy (CPT) is another form of cognitive-behavioral therapy specifically designed for PTSD. It focuses on helping patients understand and reframe their negative thoughts about the trauma. CPT involves writing about the traumatic event and discussing its impact on beliefs about oneself, others, and the world. This therapy has been shown to be highly effective in reducing PTSD symptoms, particularly in survivors of rape and sexual assault. CPT helps patients challenge and modify their maladaptive beliefs, leading to a reduction in PTSD symptoms and an improvement in overall mental health.
4. Eye Movement Desensitization and Reprocessing (EMDR)
Eye Movement Desensitization and Reprocessing (EMDR) is a psychotherapy treatment designed to alleviate the distress associated with traumatic memories. EMDR involves recalling traumatic events while simultaneously focusing on an external stimulus, such as the therapist’s finger moving back and forth. This process is believed to help reprocess traumatic memories and reduce their emotional impact. EMDR has been shown to be effective in treating PTSD, with studies indicating significant reductions in symptoms . It is particularly useful for patients who may not respond well to traditional talk therapies.
5. Trauma-Focused Cognitive Behavioral Therapy (TF-CBT)
Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) is a specialized form of CBT designed to help children and adolescents overcome the impact of traumatic experiences. TF-CBT combines trauma-sensitive interventions with cognitive-behavioral, family, and humanistic principles. It has been shown to be highly effective in reducing PTSD symptoms in youth, with individual forms of TF-CBT demonstrating large effects compared to waitlist controls. The therapy typically involves psychoeducation, cognitive processing, and gradual exposure to trauma reminders, helping young patients and their families process and cope with the trauma.
6. Medications
Medications are often used as an adjunct to psychotherapy in the treatment of PTSD. Selective serotonin reuptake inhibitors (SSRIs) and other antidepressants are commonly prescribed to help manage symptoms such as anxiety, depression, and insomnia. While pharmacological treatments can be effective, their effect sizes are generally lower compared to psychological therapies. Emerging evidence also suggests the potential of pharmacologically assisted psychotherapies, such as MDMA-assisted psychotherapy, which has shown promise in treating PTSD. Medications can provide symptom relief and improve the overall effectiveness of psychotherapy, but they are typically not considered a standalone treatment for PTSD.
Preventing Trauma
Preventing trauma involves proactive measures and strategies aimed at reducing the risk and impact of traumatic events. By fostering supportive environments and promoting resilience, we can mitigate the effects of trauma. Below is a list of key strategies for preventing trauma.
1. Community-based Interventions
Community-based interventions play a crucial role in preventing trauma by fostering resilience and providing essential resources. For instance, the Los Angeles County Department of Mental Health funded community partnerships to build capacity for addressing trauma. These partnerships focused on trauma-informed education, community outreach, and linking community members to resources. The initiative conducted over 7800 events with more than 250,000 attendees, resulting in nearly 14,000 successful linkages to various resources. Despite the challenges posed by the COVID-19 pandemic, the community members reported improvements in stress tolerance and community connectedness, demonstrating the effectiveness of these interventions.
2. Education and Awareness
Education and awareness are fundamental in preventing trauma and its long-term effects. Trauma-informed education and training can significantly enhance the ability of individuals and communities to recognize and address trauma. For example, systematic trauma-informed attachment-focused interventions are recommended to prevent intergenerational trauma. These interventions target multiple levels, including individual, familial, and community, to resolve parental trauma and support parent-infant attachment. Such comprehensive educational strategies are essential for preventing the transmission of trauma across generations and promoting mental health.
3. Building Resilience
Building resilience is a key strategy in trauma prevention, as it equips individuals with the ability to cope with and recover from traumatic events. Resilience training programs, such as the Mental Agility and Psychological Strength (MAPS) training for firefighters, aim to enhance mental agility and psychological strength. Although the MAPS program did not show significant effects on mental health issues or coping strategies, it did improve trauma knowledge among participants. This highlights the importance of resilience training in increasing awareness and preparedness, which are critical components of trauma prevention.
4. Developing Coping Strategies
Developing effective coping strategies is essential for mitigating the impact of trauma. Early interventions, particularly those delivered via the internet, have shown promise in helping individuals exposed to traumatic events. Indicated interventions, which are targeted at individuals showing signs of post-traumatic distress, have been found to significantly improve mental health outcomes. These interventions provide accessible and timely support, helping individuals develop coping mechanisms that can prevent the progression of trauma-related symptoms.
5. Mental Health Support
Providing robust mental health support is vital for preventing trauma and its associated disorders, such as PTSD. Cognitive-behavioral therapy with a trauma focus (CBT-T) has been identified as an effective intervention for individuals with acute stress disorder, reducing the severity of PTSD symptoms. Additionally, collaborative care models have shown promise in decreasing PTSD symptom severity post-injury. These findings underscore the importance of targeted mental health interventions in preventing the onset of PTSD and other trauma-related conditions.
FAQs
1. How does trauma affect different age groups?
Trauma impacts children, adolescents, and adults differently. Children may show behavioral changes such as regression, while adolescents might exhibit risk-taking behavior. Adults often have more well-defined coping mechanisms but may experience deeper emotional or physical symptoms. Understanding age-specific responses helps in tailoring effective support and treatment.
2. Can trauma be passed down through generations?
Yes, trauma can be intergenerational. Known as transgenerational or intergenerational trauma, the effects of traumatic events experienced by one generation can impact the mental and emotional health of subsequent generations. This often occurs through learned behaviors, unresolved grief, and emotional patterns within families.
3. What is the difference between trauma and stress?
Stress is a common and often temporary response to challenges, while trauma is a more intense, overwhelming experience that affects long-term mental, emotional, and physical well-being. While stress might pass with time, trauma often requires more in-depth intervention to heal.
4. What are some common myths about trauma?
Some myths include the belief that trauma only affects people who experience extreme violence, that it’s purely a psychological issue, or that people should “just get over it” with time. In reality, trauma can result from a wide variety of experiences, affects both mental and physical health, and often requires professional treatment.
5. Can trauma cause physical health problems?
Yes, trauma can lead to physical health problems. Chronic trauma is linked to conditions such as cardiovascular disease, autoimmune disorders, and chronic pain. The body’s prolonged stress response can weaken the immune system and exacerbate existing physical conditions.
6. How do people with trauma respond to triggers?
Triggers are specific stimuli that remind individuals of their trauma and can cause intense emotional and physical reactions. These triggers may not be obvious to others and can include smells, sounds, places, or even emotions that were present during the traumatic event.
7. Is it possible to fully recover from trauma?
While trauma may have long-lasting effects, many people can recover with the right support. Full recovery may involve reducing symptoms to a manageable level, achieving emotional regulation, and rebuilding a sense of safety and trust. Some people may find that they grow stronger and more resilient after working through their trauma, a process known as post-traumatic growth.
8. How does trauma affect relationships?
Trauma can cause difficulties in forming and maintaining relationships. Trust issues, emotional detachment, and fear of vulnerability are common challenges. People with unresolved trauma may also struggle with boundaries and communication, making relationships more difficult to navigate.
9. What is trauma-informed care?
Trauma-informed care is an approach in health and social services that acknowledges the widespread impact of trauma and strives to create environments of healing and support. It involves understanding trauma’s effects and implementing practices that avoid re-traumatization, empowering individuals in their recovery.
10. How does trauma affect the brain?
Trauma can alter the brain’s structure and function, particularly in areas like the amygdala, hippocampus, and prefrontal cortex. These changes may result in heightened fear responses, memory difficulties, and problems with emotional regulation. In severe cases, these brain alterations can contribute to the development of PTSD and other mental health conditions.