Surgical Site Infections (SSIs) are a significant complication that can occur following surgical procedures. These infections develop at or near the site of a surgical incision within 30 days after surgery, or within 90 days if prosthetic material is implanted during the operation. SSIs affect approximately 2-4% of all in-hospital surgery patients and are a major contributor to postoperative illness and mortality. They can range from superficial incisional infections, which are limited to the skin and subcutaneous tissues, to deep incisional infections that extend into the deeper, softer tissues. SSIs are a leading cause of hospital readmissions following surgery and can result in increased healthcare costs, prolonged hospital stays, and in severe cases, patient death. Despite advancements in surgical techniques and the use of antibiotics, SSIs remain a persistent challenge in healthcare settings, particularly when associated with biofilm-forming bacteria that are resistant to conventional antibiotic treatments.
Common types of Surgical Site Infections
Surgical Site Infections (SSIs) are a significant concern in postoperative care, as they can lead to severe complications and prolonged hospital stays. SSIs are classified based on the depth and location of the infection. Below are the common types of SSIs, each requiring specific attention and treatment strategies:
1. Superficial Incisional SSI
Superficial incisional surgical site infections (SSIs) involve the skin and subcutaneous tissues and typically occur within 30 days post-surgery unless a foreign body is implanted, in which case the timeframe extends to one year. These infections are often associated with factors such as smoking, higher body mass index, and preoperative hospital admission. The management of superficial SSIs generally involves opening and draining the incision, which is usually sufficient without the need for extensive antimicrobial therapy. Preventative measures, including proper patient preparation and aseptic techniques, are crucial in reducing the incidence of superficial SSIs. The risk factors and preventative strategies for superficial SSIs highlight the importance of targeted interventions to minimize patient morbidity and healthcare costs.
2. Deep Incisional SSI
Deep incisional SSIs affect the deeper soft tissues, such as the fascial and muscle layers, and must occur within 90 days of the operation to be classified as an SSI, except when foreign materials are involved. These infections are more severe than superficial SSIs and often require urgent surgical debridement and antibiotic therapy. Risk factors for deep incisional SSIs include steroid use, smoking, and preoperative hospital admission. The incidence of deep incisional SSIs can be influenced by the type of surgery, with open surgeries posing a higher risk compared to laparoscopic procedures. Effective management and prevention strategies, including the use of antimicrobial prophylaxis and meticulous surgical techniques, are essential to reduce the occurrence and impact of deep incisional SSIs.
3. Organ or Space SSI
Organ or space SSIs involve any part of the body deeper than the fascial/muscle layer that is manipulated during surgery and must occur within 90 days post-operation to be considered an SSI. These infections are associated with significant morbidity and mortality, particularly in patients undergoing complex procedures such as solid organ transplants. Risk factors for organ or space SSIs include wound class, recent chemotherapy, and steroid use. The management of these infections often requires a combination of surgical intervention and antimicrobial therapy. Preventative measures, such as the use of oral antibiotic preparations preoperatively and adherence to aseptic techniques, are critical in reducing the risk of organ or space SSIs. Understanding the specific risk factors and implementing targeted prevention strategies can significantly improve patient outcomes and reduce healthcare burdens associated with these severe infections.
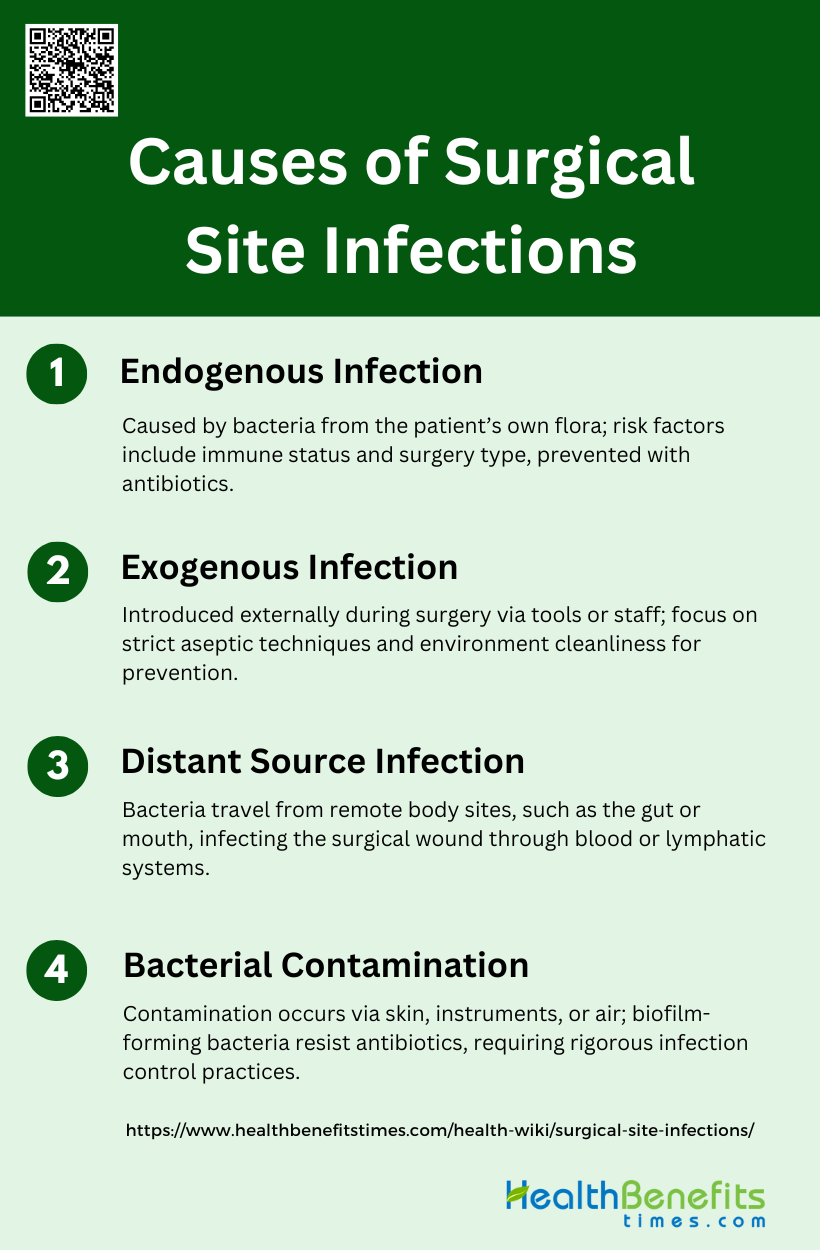
Causes of Surgical Site Infections
Surgical Site Infections (SSIs) can arise from various sources, each contributing to the complexity of preventing these infections. Understanding the causes is crucial for implementing effective preventive measures. Below are the primary causes of SSIs:
1. Endogenous Infection
Endogenous infections in surgical sites are primarily caused by the patient’s own flora. These infections occur when bacteria that normally reside on the skin or within the body enter the surgical wound. Common pathogens include Staphylococcus aureus, coagulase-negative staphylococci, Enterococcus spp., and Escherichia coli. The risk of endogenous infections is influenced by various patient-related factors such as immune status, presence of comorbidities, and the type of surgery performed. Preventive measures include proper patient preparation, aseptic surgical techniques, and the use of antimicrobial prophylaxis. Despite stringent preventive strategies, endogenous infections remain a significant challenge in surgical care.
2. Exogenous Infection
Exogenous infections are caused by pathogens introduced from external sources during or after surgery. These sources can include surgical instruments, the hands of the surgical team, or the hospital environment. Common exogenous pathogens include Klebsiella spp., Pseudomonas aeruginosa, and Acinetobacter baumannii. Preventive measures focus on minimizing contamination through strict aseptic techniques, proper sterilization of instruments, and maintaining a clean operating environment. Studies have shown that a significant proportion of surgical site infections (SSIs) are due to exogenous bacteria, highlighting the importance of environmental control and hygiene practices in preventing these infections.
3. Distant Source Infection
Distant source infections occur when pathogens from a remote site within the body, such as the gums or intestines, migrate to the surgical site. This phenomenon, often referred to as the “Trojan Horse” mechanism, suggests that bacteria can travel through the bloodstream or lymphatic system to infect the surgical wound. Research indicates that the gut microbiome can play a significant role in these infections, even without a direct breach of the intestinal barrier. Understanding the dynamics of microbial movement within the body is crucial for developing new preventive strategies, such as genomic-based microbial tracking, to reduce the incidence of distant source infections.
4. Bacterial Contamination
Bacterial contamination of surgical wounds is a primary cause of SSIs. Contamination can occur during surgery from the patient’s skin, surgical instruments, or airborne particles in the operating room. The presence of biofilm-forming bacteria, which are highly resistant to antibiotics, further complicates the treatment of these infections. Preventive strategies include meticulous surgical techniques, proper skin preparation, and the use of antimicrobial agents. Despite these measures, bacterial contamination remains a significant risk factor for SSIs, necessitating continuous efforts to improve infection control practices and develop novel antimicrobial therapies.
Signs and Symptoms of Surgical Site Infections
Surgical Site Infections (SSIs) can manifest through various clinical signs and symptoms, indicating the presence of an infection at or near the surgical site. Early detection is essential for prompt treatment and to prevent complications. Below are the common signs and symptoms of SSIs:
1. Common Symptoms: Fever, pain at the surgical site, and local signs of inflammation such as redness, warmth, and swelling are frequently reported symptoms of SSIs.
2. Wound Discharge: Presence of wound discharge or drainage is a common indicator of SSIs.
3. Leukocytosis: Elevated white blood cell count (leukocytosis) is often observed in patients with SSIs.
4. Neurologic Deficits: In cases of spinal surgery, new neurologic deficits can be a rare but significant symptom of SSIs.
5. Back Pain: Persistent or worsening back pain, particularly after spinal surgery, is a common symptom of SSIs.
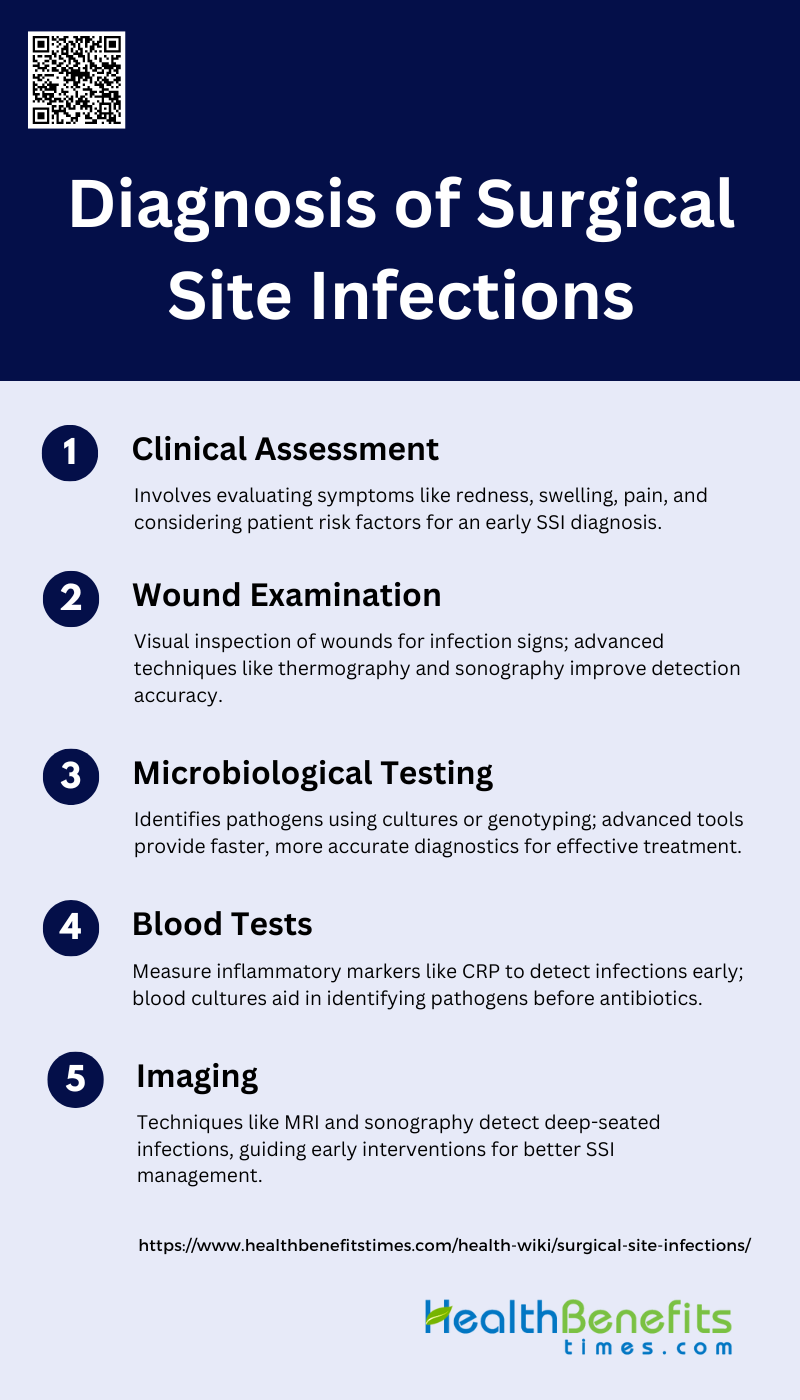
Diagnosis of Surgical Site Infections
Accurate diagnosis of Surgical Site Infections (SSIs) is crucial for effective treatment and prevention of complications. Various diagnostic methods are employed to identify and confirm the presence of an infection. Below is the primary Diagnosis of Surgical Site Infections:
1. Clinical Assessment
Clinical assessment is crucial for the early detection of surgical site infections (SSIs). It involves a thorough evaluation of the patient’s symptoms and risk factors. For instance, a high level of suspicion is necessary to attain an early definitive diagnosis, especially in cases like spine surgery where SSIs can be superficial or deep-seated. Common presenting symptoms include pain, redness, and swelling around the surgical site. Additionally, factors such as diabetes, smoking, and the use of steroids can increase the risk of SSIs. Regular follow-up visits, particularly between 2 to 4 weeks post-surgery, are essential for early detection and management of SSIs.
2. Wound Examination
Wound examination is a vital component in diagnosing SSIs. Visual inspection of the wound can reveal signs of infection such as redness, swelling, and discharge. Studies have shown that features like granulation degree, exudate amount, and the presence of nasogastric tubes are significantly associated with subsequent SSI diagnosis. Advanced techniques like sonography can also be employed to detect fluid collections around the wound, which are predictive of SSIs. Moreover, infrared thermography has shown promise in predicting SSIs by identifying temperature differences between the wound site and surrounding tissue. These methods enhance the accuracy of wound examination and facilitate early intervention.
3. Microbiological Testing
Microbiological testing is essential for identifying the pathogens responsible for SSIs and guiding appropriate antibiotic therapy. Traditional methods include Gram staining and culturing bacteria from wound swabs or deep tissue biopsies. However, these methods can be time-consuming and sometimes yield false-negative results. Recent advancements in molecular microbiology, such as genotyping, allow for quicker and more accurate identification of pathogens, even those that are difficult to culture. Devices like the MolecuLight i:X Imaging Device can visualize bacteria in real-time, improving the speed and accuracy of diagnosis. These innovations are crucial for timely and effective management of SSIs.
4. Blood Tests
Blood tests are valuable tools in the diagnosis of SSIs, particularly through the measurement of inflammatory markers. C-reactive protein (CRP) is a strong rule-in and rule-out marker for SSIs, providing a reliable indication of infection. Other markers, such as serum amyloid A, have also shown potential in expediting the diagnosis of SSIs. Comparing pre-operative and post-operative levels of these markers can help in early detection. Blood cultures, although having a low yield, should be collected before initiating antibiotic therapy to identify the causative organisms. These tests complement clinical assessment and wound examination in diagnosing SSIs.
5. Imaging
Imaging techniques play a significant role in diagnosing SSIs, especially when clinical signs are ambiguous. Magnetic resonance imaging (MRI) is the diagnostic modality of choice for detecting deep-seated infections, particularly in spine surgeries. Computed tomography (CT) scans can also be used for guided aspiration of paraspinal collections when there is a high suspicion of SSI. Additionally, sonography has been shown to detect peri-incisional fluid collections, which are predictive of SSIs. Infrared thermography is another promising tool that can identify temperature differences indicative of infection. These imaging modalities provide valuable insights that aid in the early and accurate diagnosis of SSIs.
Prevention Strategies of surgical site infections (SSIs)
Preventing Surgical Site Infections (SSIs) involves a combination of meticulous hygiene, sterilization practices, and comprehensive preoperative and postoperative care. Implementing these strategies can significantly reduce the risk of infections. Below are the key prevention strategies for SSIs:
1. Hygiene and Sterilization Practices
Hand hygiene and the sterilization of instruments and the operating environment are critical components in preventing surgical site infections (SSIs). Proper hand hygiene by surgical staff, including thorough washing and the use of antiseptic solutions, significantly reduces the risk of introducing pathogens into the surgical site. Sterilization of surgical instruments and the operating environment is equally important. Instruments must be sterilized using methods such as autoclaving, and the operating room should be cleaned with appropriate disinfectants to eliminate potential contaminants. Additionally, the use of alcohol-based skin preparations for both patients and surgical staff has been shown to be effective in reducing microbial load, thereby lowering the risk of SSIs.
2. Preoperative and Postoperative Care
Preoperative and postoperative care is essential in minimizing the risk of SSIs. The administration of prophylactic antibiotics before surgery, particularly timed to ensure bactericidal concentrations at the time of incision, is a well-established practice that significantly reduces SSI rates. Proper wound care and monitoring post-surgery are also crucial. This includes the use of sterile dressings, regular inspection of the wound for signs of infection, and maintaining optimal conditions such as normothermia and glycemic control. Advanced wound care techniques, such as the use of silver-impregnated dressings and vacuum-assisted closure, have shown promise in further reducing infection rates. Continuous education and adherence to evidence-based guidelines are vital for the effective prevention of SSIs.
Treatment Options for surgical site infections (SSIs)
Surgical site infections (SSIs) are a significant concern in postoperative care, requiring prompt and effective treatment to prevent complications. The treatment options for SSIs can be broadly categorized into medical treatments and surgical interventions. Below are the key approaches to managing SSIs:
1. Medical Treatments
1. Antibiotic Therapy
Antibiotic therapy is a cornerstone in the treatment of SSIs. The choice of antibiotics depends on the suspected or identified pathogens, with Staphylococcus aureus being a common culprit. Treatment usually begins with broad-spectrum antibiotics and may be adjusted based on culture results. In some cases, prolonged antibiotic courses may be necessary to fully eradicate the infection.
2. Drainage and Debridement
Drainage and debridement are crucial components of SSI management. This involves removing infected or necrotic tissue and draining any accumulated pus. Negative pressure wound therapy (NPWT) has shown promising results in treating SSIs by promoting wound healing, reducing hospital stays, and accelerating wound closure. Vacuum sealing drainage (VSD) is another effective technique, particularly for intracranial neurosurgery SSIs, with studies showing full recovery in 70% of patients.
2. Role of Surgical Intervention
In some cases, additional surgery may be necessary to effectively treat SSIs. This is particularly true for deep infections or those involving implanted devices. The debridement-irrigation, antibiotic therapy, and implant retention (DAIR) protocol has shown effectiveness in treating deep SSIs, especially when performed within 3 months of the initial surgery. Early second-look surgery (within 7 days) for iterative debridement may also be beneficial in some cases. However, the need for reoperation should be carefully evaluated, as it can lead to increased medical costs and longer hospital stays.
How to Reduce Your Risk of Surgical Site Infections as a Patient
Reducing the risk of surgical site infections (SSIs) is crucial for a smooth recovery and overall health. Patients can take several proactive steps to minimize their risk. Below are key measures to consider:
1. Personal Hygiene before Surgery
Maintaining personal hygiene before surgery is crucial in reducing the risk of surgical site infections (SSIs). Preoperative measures such as antiseptic showers and the use of chlorhexidine bathing cloths have been shown to potentially decrease the risk of SSIs. Screening and decolonization protocols for methicillin-sensitive and methicillin-resistant Staphylococcus aureus (S. aureus) are also recommended, as nasal carriers of S. aureus are more likely to develop nosocomial infections and SSIs. The World Health Organization (WHO) emphasizes the importance of preoperative measures, including proper skin antisepsis, to minimize infection risks. Therefore, patients should adhere to prescribed hygiene protocols, including thorough washing with antiseptic solutions, to lower the chances of postoperative complications.
2. Follow Post-Surgery Care Instructions Strictly
Strict adherence to post-surgery care instructions is vital for preventing SSIs. Postoperative infection prophylaxis can include the use of silver-impregnated or vacuum dressings, extended intravenous antibiotics, and supplemental oxygen therapy. Proper wound care, including keeping the surgical site clean and dry, and following the healthcare provider’s guidelines on dressing changes and activity restrictions, are essential steps in minimizing infection risks. Additionally, the use of antiseptic surgical dressings and negative pressure wound therapy has shown promise in reducing SSIs. By meticulously following these instructions, patients can significantly reduce their risk of developing infections and promote faster, complication-free recovery.
3. Importance of Reporting Any Unusual Symptoms to Your Doctor Immediately
Promptly reporting any unusual symptoms to your doctor is critical in the early detection and treatment of SSIs. Symptoms such as increased redness, swelling, pain, or discharge at the surgical site should be communicated to healthcare providers without delay. Early intervention can prevent the progression of infections and reduce the associated morbidity and healthcare costs. Studies have shown that timely management of SSIs, including the use of appropriate antibiotics and wound care, can significantly improve patient outcomes. Therefore, patients should be vigilant and proactive in reporting any signs of infection to ensure timely and effective treatment.
Impact on Healthcare Systems in surgical site infections
Surgical site infections (SSIs) pose a significant challenge to healthcare systems, leading to increased costs and resource utilization. Understanding the various impacts of SSIs can help in developing effective strategies to mitigate these issues. Below are key areas affected by SSIs:
1. Financial Implications
Surgical site infections (SSIs) impose a significant financial burden on healthcare systems. Studies have shown that SSIs lead to increased costs due to prolonged hospital stays, additional treatments, and readmissions. For instance, SSIs can extend hospital stays by an average of 9.7 days and increase costs by approximately $20,842 per admission. In the UK, the additional cost per patient with an SSI was found to be around £3,776, including antibiotic costs. Moreover, hospitals face a substantial financial impact, with one study estimating nearly $1.6 billion in excess costs due to SSIs. These financial implications highlight the need for effective prevention strategies to mitigate the economic burden on healthcare systems.
2. Length of Hospital Stay and Patient Recovery
SSIs significantly prolong the length of hospital stays and delay patient recovery. On average, SSIs extend hospital stays by 9.7 days, and in some cases, the length of stay can increase by up to 92%. This extended hospitalization not only delays patient recovery but also increases the risk of further complications and readmissions. For example, patients with deep SSIs had a median length of stay of 7 days compared to 5 days for those without SSIs. Additionally, SSIs are associated with higher readmission rates, further complicating patient recovery and increasing healthcare costs. These findings underscore the critical need for effective infection control measures to improve patient outcomes and reduce hospital stays.
3. Strategies to Reduce the Burden on Healthcare Systems
To reduce the burden of SSIs on healthcare systems, several strategies can be implemented. Adherence to prevention guidelines, such as antibiotic prophylaxis, screening, and decolonization of MRSA, has shown economic benefits. Early discharge (ED) programs and the use of antibiotics that allow for ED can also be cost-effective and improve patient quality of life. In low-resource settings, innovative solutions like solar-powered autoclaves for sterilization can help reduce SSIs. Additionally, implementing bundled prevention practices, including proper sterilization and wound care, can mitigate the risk of SSIs. These strategies highlight the importance of comprehensive infection control measures to reduce the incidence and financial impact of SSIs on healthcare systems.
FAQs
1. Can lifestyle changes before surgery help prevent SSIs?
Yes, certain lifestyle changes, such as quitting smoking, managing diabetes, and maintaining a healthy weight, can reduce the risk of SSIs. Smoking cessation programs and proper glycemic control are especially important as they reduce complications related to wound healing.
2. Are there any preoperative tests or screenings to assess SSI risks?
Screening for bacteria like methicillin-resistant Staphylococcus aureus (MRSA) is common in some hospitals. If patients are found to be carriers, decolonization treatments like nasal ointments or antiseptic baths may be used before surgery to reduce the risk of infection.
3. What role does nutrition play in preventing SSIs?
Proper nutrition before surgery can enhance immune function and promote better wound healing. Nutrients such as vitamin C, zinc, and protein are crucial in supporting tissue repair and reducing infection risks.
4. How do biofilms contribute to SSIs, and why are they difficult to treat?
Biofilms are clusters of bacteria that adhere to surfaces and form protective layers. They can form on surgical implants or in wounds, making the bacteria more resistant to antibiotics and harder to treat. Specialized treatments, such as biofilm-targeting therapies, may be necessary for infections involving biofilms.
5. Can SSIs occur after minimally invasive surgeries?
Yes, while the risk of SSIs is generally lower in minimally invasive procedures, they can still occur. Proper aseptic techniques and postoperative wound care are essential to minimize infection risks, even for small incisions.
6. What are the long-term effects of SSIs on patient health?
SSIs can have lasting impacts, including chronic pain, reduced mobility, scarring, and in severe cases, permanent organ damage. They may also increase the risk of future infections, particularly if prosthetic materials are involved.
7. Are there alternative wound closure techniques that reduce the risk of SSIs?
Some advanced wound closure techniques, such as the use of antimicrobial sutures, staples, or adhesives, may reduce the risk of SSIs. Negative pressure wound therapy (NPWT) is another option that helps improve healing by reducing infection risks in high-risk patients.
8. How can patients care for surgical drains to reduce infection risk?
Proper care of surgical drains, including keeping the area clean and following the surgeon’s instructions on drainage and dressing changes, is crucial in preventing infections. Patients should be vigilant about signs of infection around the drain site.
9. What innovations are being developed to combat antibiotic-resistant SSIs?
Research is exploring novel therapies like bacteriophages (viruses that target specific bacteria) and advanced antimicrobial dressings infused with nanoparticles to treat SSIs caused by resistant bacteria.
10. Can environmental factors in the hospital contribute to SSIs?
Yes, poor air quality, contaminated surfaces, and lack of proper sterilization procedures can contribute to exogenous SSIs. Maintaining a sterile environment in the operating room and ensuring hospital cleanliness are critical for preventing infections.