Staphylococcus epidermidis is one of the most abundant bacterial colonizers of healthy human skin and a prominent member of the normal skin microflora. However, it has also emerged as a significant opportunistic pathogen, particularly in hospital settings. S. epidermidis is the staphylococcal species most commonly associated with bacteremia and hospital-acquired infections, and it has become a leading cause of infections related to indwelling medical devices such as vascular catheters, prosthetic joints, and artificial heart valves. The prevalence of S. epidermidis in hospital-acquired infections is primarily due to its ability to adhere to and form biofilms on biomaterial surfaces, which is considered one of its most important virulence factors. In biofilm form, these bacteria are protected from antimicrobial agents and the host immune system, contributing to the persistence of biofilm infections and making treatment particularly challenging.
Characteristics of Staphylococcus epidermidis
Staphylococcus epidermidis is a Gram-positive bacterium commonly found on human skin and mucous membranes. It plays a dual role as both a harmless commensal and a potential pathogen. Below are the key characteristics of this microorganism:
1. Morphology and Structure
It has a spherical shape (cocci) and lacks flagella, making it non-motile. The cell wall structure is thick, composed of peptidoglycan, which is characteristic of Gram-positive bacteria. Additionally, S. epidermidis can produce a polysaccharide capsule that aids in evading the host immune system and contributes to biofilm formation on surfaces.
2. Growth Characteristics
It thrives at human body temperature (37°C) and can grow on various nutrient media, including blood agar, where it forms white, non-hemolytic colonies. The bacterium is known for its ability to form biofilms, particularly on medical devices, which is a critical factor in its pathogenicity. Biofilm formation is enhanced in the presence of glucose and other environmental factors.
3. Habitat and Distribution
It is part of the normal flora and plays a role in maintaining skin homeostasis. However, it can also be found in hospital environments, where it colonizes medical devices and surfaces. Its ability to adapt to different environmental conditions, including the hospital setting, makes it a common nosocomial pathogen.
4. Biochemical Properties
Biochemically, S. epidermidis is catalase-positive, meaning it can decompose hydrogen peroxide into water and oxygen. It is also coagulase-negative, distinguishing it from the more virulent Staphylococcus aureus. The bacterium can ferment glucose and other carbohydrates, producing acid but no gas. It possesses various enzymes, such as lipases and proteases, which contribute to its ability to colonize and infect host tissues.
5. Virulence Factors
The primary virulence factor of S. epidermidis is its ability to form biofilms, which protect the bacteria from the host immune response and antibiotics. Other virulence factors include surface proteins that facilitate adhesion to host tissues and medical devices, and enzymes like proteases that degrade host proteins. The presence of mobile genetic elements, such as insertion sequences and plasmids, also contributes to its virulence by enabling the acquisition of antibiotic resistance genes.
6. Clinical Significance
- epidermidis is a leading cause of nosocomial infections, particularly in immunocompromised patients and those with indwelling medical devices like catheters and prosthetic joints. It is associated with conditions such as bacteremia, endocarditis, and surgical site infections. The bacterium’s ability to form biofilms on medical devices makes infections difficult to treat, often requiring the removal of the infected device.
7. Genetic Features
Genetically, S. epidermidis is highly diverse, with significant variability in its genome due to frequent recombination and the acquisition of mobile genetic elements. It possesses a core set of genes shared with other staphylococci, but also unique genes that contribute to its adaptability and pathogenicity. The presence of the SCCmec gene cassette confers methicillin resistance, and other resistance genes are often located on plasmids and transposons. The genetic diversity within S. epidermidis populations is a key factor in its ability to adapt to different environments and develop resistance to antibiotics.
Role of Staphylococcus Epidermidis in Skin Health
Staphylococcus epidermidis is a key player in maintaining skin health through various mechanisms. It acts as a protective barrier, modulates the immune response, and produces antimicrobial substances. Below is the Role of Staphylococcus Epidermidis in Skin Health:
1. Protective Barrier
Staphylococcus epidermidis acts as a protective barrier against pathogenic bacteria by producing antimicrobial peptides (AMPs) that selectively inhibit harmful microbes. These peptides, such as phenol-soluble modulins (PSMs), target and reduce the survival of pathogens like Staphylococcus aureus and Group A Streptococcus while preserving the normal skin microbiome. Additionally, S. epidermidis enhances the production of AMPs by keratinocytes, further bolstering the skin’s defense against infections.
2. Immune Modulation
epidermidis plays a crucial role in modulating the skin’s immune response by interacting with immune cells and promoting the expression of antimicrobial proteins. It activates gamma delta (GD) T cells and upregulates perforin-2 (P-2), which aids in the clearance of intracellular pathogens like methicillin-resistant Staphylococcus aureus (MRSA). Moreover, S. epidermidis can stimulate Toll-like receptor 2 (TLR2) signaling, leading to increased production of human beta-defensins, which are essential for antimicrobial defense.
3. Production of Antimicrobial Substances
epidermidis produces various antimicrobial substances that help control harmful bacteria on the skin. Phenol-soluble modulins (PSMs) produced by S. epidermidis exhibit strong antimicrobial activity against skin pathogens, working synergistically with human AMPs like LL-37 to enhance their effectiveness. Additionally, S. epidermidis can stimulate the production of antimicrobial peptides such as human beta-defensins in keratinocytes, further contributing to the skin’s antimicrobial defense.
Benefits of Staphylococcus Epidermidis
Staphylococcus epidermidis offers numerous benefits for skin health through its various functions. It aids in skin protection, colonization resistance, immune modulation, and more. Below are the key benefits it provides:
1. Skin Protection and Homeostasis
Staphylococcus epidermidis plays a crucial role in maintaining skin protection and homeostasis. It is a key constituent of the normal microbiota on human skin, balancing the inflammatory response after skin injury and producing antimicrobial molecules that selectively inhibit skin pathogens. Additionally, S. epidermidis helps in maintaining the skin’s moisture retention and lipid content, which are essential for a healthy skin barrier. The bacterium also contributes to the overall balance of the skin microbiome, ensuring that pathogenic microorganisms do not overgrow and disrupt the skin’s natural state. This balance is vital for preventing skin diseases and maintaining overall skin health.
2. Colonization Resistance
Staphylococcus epidermidis is instrumental in providing colonization resistance, which is the ability of the skin microbiota to prevent the colonization and overgrowth of pathogenic microorganisms. S. epidermidis produces antimicrobial peptides, such as phenol-soluble modulins (PSMs), which selectively inhibit the growth of harmful bacteria like Staphylococcus aureus while sparing beneficial skin microbes. This selective antimicrobial action helps maintain a healthy skin microbiome and prevents infections. Furthermore, S. epidermidis can ferment glycerol to produce short-chain fatty acids like succinic acid, which inhibit the growth of Propionibacterium acnes, a bacterium associated with acne vulgaris. These mechanisms collectively contribute to the skin’s defense against pathogenic colonization.
3. Immune System Modulation
Staphylococcus epidermidis significantly influences the immune system’s modulation. It has been shown to upregulate the expression of antimicrobial proteins such as perforin-2 in human skin gamma delta T cells, enhancing the skin’s ability to clear intracellular pathogens. This bacterium also helps in balancing the immune response, reducing excessive inflammation that can lead to skin damage. Moreover, S. epidermidis can produce metabolites that activate the aryl hydrocarbon receptor (AhR) pathway, which is involved in skin differentiation and immune response regulation. These interactions highlight the bacterium’s role in modulating the immune system to maintain skin health and prevent disease.
4. Production of Beneficial Compounds
Staphylococcus epidermidis produces several beneficial compounds that contribute to skin health. Among these are antimicrobial peptides like phenol-soluble modulins (PSMs), which have strong lipid membrane interactions and selectively inhibit skin pathogens. Additionally, S. epidermidis can ferment glycerol to produce short-chain fatty acids such as succinic acid, which inhibit the growth of acne-causing bacteria. These compounds not only protect the skin from harmful microorganisms but also help maintain the balance of the skin microbiome. The production of these beneficial compounds underscores the importance of S. epidermidis in promoting a healthy skin environment.
5. Skin Microbiome Balance
Staphylococcus epidermidis plays a pivotal role in maintaining the balance of the skin microbiome. It acts as a key member of the healthy skin microbiota, involved in the defense against pathogens and modulating the immune system. By producing antimicrobial peptides and other inhibitory compounds, S. epidermidis prevents the overgrowth of harmful bacteria, thereby maintaining microbial diversity and balance. This balance is crucial for preventing skin disorders and ensuring the skin’s overall health. Furthermore, the bacterium’s ability to promote the growth of other beneficial microorganisms highlights its role in sustaining a stable and healthy skin microbiome.
Potential Risks and Challenges of Staphylococcus Epidermidis
While Staphylococcus epidermidis is generally harmless, it poses several risks and challenges, particularly in medical settings. It can act as an opportunistic pathogen and is associated with various complications. Below are the key risks and challenges it presents:
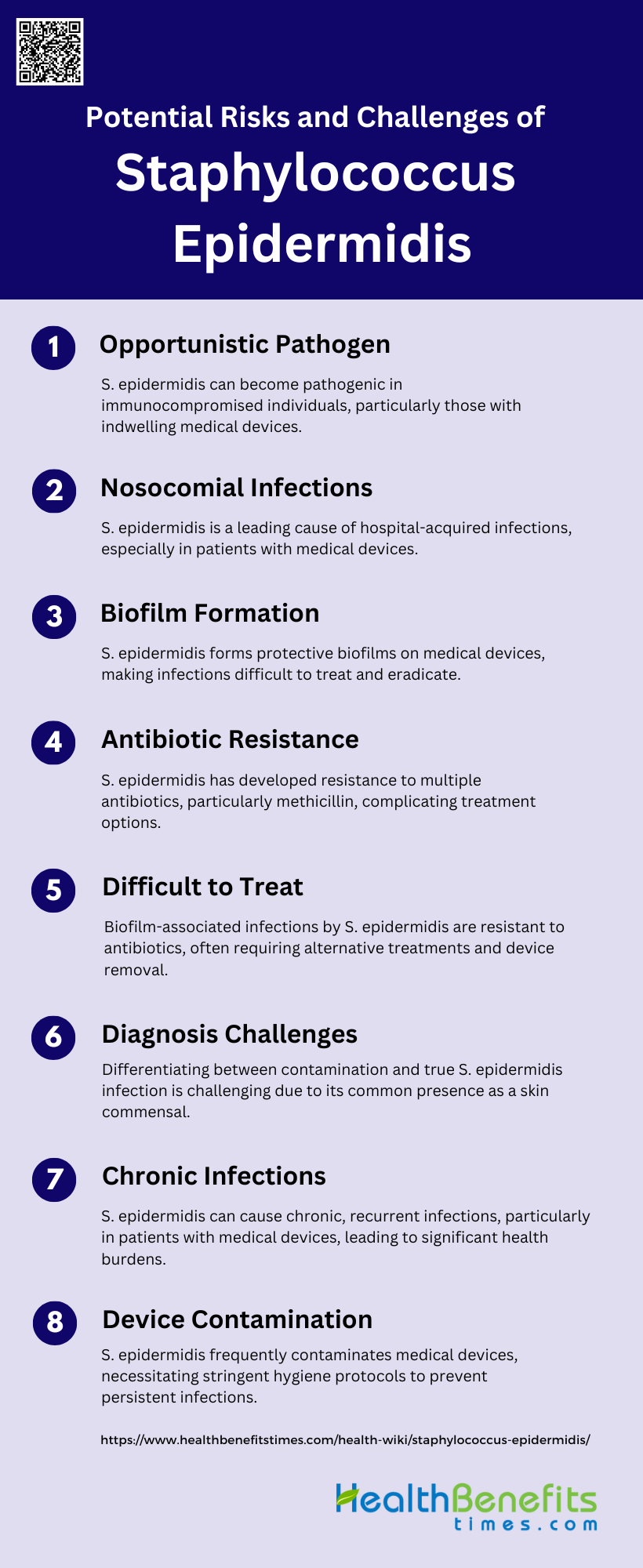
1. Opportunistic Pathogen
Staphylococcus epidermidis is a commensal bacterium that resides on human skin and mucous membranes. However, it can become an opportunistic pathogen, particularly in immunocompromised individuals or those with indwelling medical devices. The transition from a harmless commensal to a pathogen is facilitated by its ability to form biofilms and its resistance to antibiotics, which protect it from the host immune system and antimicrobial treatments. This opportunistic behavior makes S. epidermidis a significant cause of nosocomial infections, especially in hospital settings where invasive procedures are common.
2. Nosocomial Infections
Staphylococcus epidermidis is a leading cause of nosocomial infections, particularly in patients with medical devices such as catheters and prosthetic joints. These infections are challenging to treat due to the bacterium’s ability to form biofilms on inert surfaces, which protect it from both the immune system and antibiotic treatments. The high prevalence of antibiotic-resistant strains in hospital environments further complicates treatment, making S. epidermidis a significant burden in healthcare settings. Epidemiological studies have shown that hospital-acquired strains differ significantly from community-acquired ones in terms of biofilm formation and antibiotic resistance.
3. Biofilm Formation
One of the most critical virulence factors of Staphylococcus epidermidis is its ability to form biofilms. These biofilms are complex, three-dimensional structures composed of polysaccharides, proteins, and extracellular DNA, which provide a protective environment for the bacteria. Biofilm formation is particularly problematic on medical devices, where it can lead to persistent infections that are resistant to both the immune system and antibiotic treatments. Subinhibitory concentrations of certain antibiotics can even induce biofilm formation, exacerbating the problem. This makes biofilm-associated infections particularly difficult to eradicate.
4. Antibiotic Resistance
Staphylococcus epidermidis has developed resistance to multiple antibiotics, making infections difficult to treat. Methicillin-resistant Staphylococcus epidermidis (MRSE) is particularly concerning, with resistance rates as high as 92% in some studies. The bacterium has also shown resistance to other antibiotics like quinolones and glycopeptides, including vancomycin. This resistance is often facilitated by biofilm formation, which protects the bacteria from antibiotic penetration. The emergence of multidrug-resistant strains necessitates the development of alternative therapeutic agents and strategies.
5. Difficult to Treat
Infections caused by Staphylococcus epidermidis are notoriously difficult to treat due to several factors. The bacterium’s ability to form biofilms on medical devices provides a protective niche that is resistant to both the immune system and antibiotics. Additionally, the high prevalence of multidrug-resistant strains further complicates treatment options. Traditional antibiotics often fail to eradicate these infections, necessitating the use of alternative agents like minocycline, rifampin, and newer drugs such as quinupristin/dalfopristin and oxazolidinones. The removal of infected medical devices is often required to fully resolve the infection.
6. Diagnosis Challenges
Diagnosing infections caused by Staphylococcus epidermidis is challenging due to its ubiquitous presence as a skin commensal. Distinguishing between contamination and true infection in blood cultures is particularly difficult. Clinicians must consider multiple factors, including the number of positive samples, patient symptoms, and the presence of medical devices, to make an accurate diagnosis. Molecular biology tools and genomic analyses are increasingly being used to identify specific resistance genes and pathogenicity traits, but these methods are not yet universally available.
7. Chronic Infections
Staphylococcus epidermidis is often associated with chronic infections, particularly those involving indwelling medical devices. These chronic infections are primarily due to the bacterium’s ability to form biofilms, which provide a persistent source of infection that is resistant to both the immune system and antibiotic treatments. Biofilm-associated infections can lead to recurrent episodes of bacteremia and sepsis, particularly in vulnerable populations like neonates and immunocompromised patients. The chronic nature of these infections poses significant medical and economic burdens.
8. Device Contamination
Staphylococcus epidermidis is a major cause of device-associated infections, including those involving catheters, prosthetic joints, and heart valves. The bacterium’s ability to form biofilms on these devices makes it particularly adept at causing persistent infections. Subinhibitory concentrations of certain antibiotics can even induce biofilm formation, worsening the problem. The contamination of medical devices often necessitates their removal to fully eradicate the infection, adding to the complexity and cost of treatment. Improved hygiene and sterilization protocols are essential to reduce the risk of device contamination.
Maintaining a Healthy Balance of Staphylococcus Epidermidis
Tips for Supporting a Healthy Skin Microbiome
Maintaining a healthy skin microbiome involves several strategies. Regular cleansing with mild, non-antimicrobial soaps can help preserve the natural balance of skin bacteria, including beneficial species like Staphylococcus epidermidis. Avoiding excessive use of antibiotics and harsh skincare products is crucial, as these can disrupt the microbiome and promote the growth of pathogenic bacteria. Additionally, incorporating probiotics and prebiotics into skincare routines may support the growth of beneficial microbes. Personalized skincare products that augment the skin with beneficial strains of S. epidermidis have shown promise in improving skin moisture retention and maintaining a healthy skin barrier.
Lifestyle Factors Affecting Staphylococcus Epidermidis
Several lifestyle factors can influence the balance of Staphylococcus epidermidis on the skin. Diet, stress, and hygiene practices play significant roles. A diet rich in nutrients and low in processed foods can support a healthy skin microbiome. Stress management is also important, as stress can alter the skin’s immune response and microbiome composition. Hygiene practices, such as regular but not excessive washing, help maintain the balance of S. epidermidis and other commensal bacteria. Overuse of antimicrobial products can disrupt this balance, leading to an overgrowth of pathogenic strains. Therefore, a balanced lifestyle that includes proper nutrition, stress management, and moderate hygiene practices is essential for maintaining a healthy population of S. epidermidis.
Importance of Skincare Routine
A consistent skincare routine is vital for maintaining the health of the skin microbiome, including Staphylococcus epidermidis. Regular cleansing helps remove excess oils and dead skin cells, which can harbor harmful bacteria. Moisturizing is crucial as it maintains the skin barrier, preventing dryness and irritation that can disrupt the microbiome. Using products that support the skin’s natural pH and contain beneficial bacteria can enhance the skin’s defense mechanisms. Studies have shown that personalized skincare routines that include the application of beneficial strains of S. epidermidis can improve skin hydration and barrier function, highlighting the importance of tailored skincare practices.
FAQs
1. Can Staphylococcus epidermidis be beneficial for individuals with acne-prone skin?
Staphylococcus epidermidis can help balance the skin microbiome and inhibit the growth of Propionibacterium acnes, a bacterium associated with acne. It produces antimicrobial compounds that may reduce the severity of acne.
2. How does the use of antibiotics affect the population of Staphylococcus epidermidis on the skin?
The use of antibiotics can disrupt the balance of the skin microbiome by reducing the population of Staphylococcus epidermidis. This can lead to overgrowth of other potentially harmful bacteria, affecting skin health.
3. What role does Staphylococcus epidermidis play in wound healing?
Staphylococcus epidermidis contributes to wound healing by producing antimicrobial peptides that protect against infections and by modulating the immune response to promote tissue repair.
4. Can Staphylococcus epidermidis transfer antibiotic resistance genes to other bacteria on the skin?
Yes, Staphylococcus epidermidis can transfer antibiotic resistance genes to other bacteria through horizontal gene transfer, potentially spreading resistance to more harmful pathogens.
5. Are there any skincare products that specifically promote the growth of Staphylococcus epidermidis?
Some skincare products are formulated with prebiotics or live bacterial cultures that support the growth of beneficial skin bacteria, including Staphylococcus epidermidis. These products aim to maintain or restore a healthy skin microbiome.
6. Can lifestyle changes impact the growth of Staphylococcus epidermidis on the skin?
Yes, lifestyle factors such as diet, stress, hygiene practices, and the use of skincare products can significantly impact the growth and balance of Staphylococcus epidermidis on the skin.
7. What are the symptoms of a Staphylococcus epidermidis infection?
Symptoms can include redness, swelling, warmth, pain at the site of infection, and fever. In cases of device-related infections, symptoms may include persistent fever or signs of sepsis.
8. Can Staphylococcus epidermidis infections be prevented in hospital settings?
Yes, infections can be prevented through strict hygiene protocols, proper sterilization of medical devices, and the use of antimicrobial coatings on medical implants to prevent biofilm formation.
9. How does Staphylococcus epidermidis interact with other skin bacteria?
Staphylococcus epidermidis interacts with other skin bacteria by producing antimicrobial compounds that inhibit pathogenic bacteria while promoting the growth of beneficial microbes, maintaining a balanced skin microbiome.
10. Are there specific conditions under which Staphylococcus epidermidis becomes pathogenic?
Staphylococcus epidermidis becomes pathogenic primarily in immunocompromised individuals, during breaches of the skin barrier, or in the presence of indwelling medical devices, where it can form biofilms and resist the host immune response.