Skin is the largest organ of the human body, serving as a complex and dynamic interface between the body and the external environment. It is composed of multiple layers, including the epidermis, dermis, and hypodermis, each with distinct functions and structures. The skin acts as a protective barrier against physical, chemical, and biological hazards, while also playing a crucial role in thermoregulation, sensation, and fluid balance. Skin also hosts a diverse microbiome that plays a crucial role in protecting against pathogens and maintaining overall health. Its ability to adapt to various climates through changes in pigmentation and other physiological mechanisms underscores its importance in human survival and adaptation. The skin’s ability to synthesize and metabolize various molecules, including vitamins and structural proteins, further underscores its importance in overall health and homeostasis. Understanding the multifaceted roles of skin is essential for advancing dermatological treatments and developing artificial skin technologies.
Structure of the Skin
The skin is the body’s largest organ, serving as a protective barrier and playing a crucial role in overall health. It is composed of three primary layers, each with distinct functions and characteristics. Below is an overview of these layers and their specific roles.
1. Epidermis
The epidermis is the outermost layer of the skin, primarily composed of keratinocytes, which are cells that produce keratin, a protective protein. This layer is stratified and squamous, meaning it is made up of multiple layers of flat cells. The epidermis is divided into several sub-layers, including the stratum basale, stratum spinosum, stratum granulosum, and the outermost stratum corneum, which acts as a major barrier against environmental stressors and pathogens. Additionally, the epidermis contains melanocytes, which produce pigment, and Langerhans cells, which are involved in immune responses. The epidermis plays a crucial role in protecting the body from external physical, chemical, and biological threats while also preventing water loss.
2. Dermis
The dermis lies beneath the epidermis and is primarily composed of dense connective tissue, including collagen and elastin fibers, which provide structural support and elasticity to the skin. This layer is subdivided into the papillary dermis, which is rich in blood vessels and nerve endings, and the reticular dermis, which contains thicker collagen fibers and provides tensile strength. The dermis houses various skin appendages such as hair follicles, sweat glands, and sebaceous glands, as well as immune cells like macrophages and mast cells. It also contains a network of blood vessels and nerves that facilitate thermoregulation, sensation, and nutrient delivery to the skin.
3. Hypodermis (Subcutaneous Layer)
The hypodermis, also known as the subcutaneous layer, is the deepest layer of the skin, composed mainly of loose connective tissue and adipose tissue. This layer acts as an insulator, conserving body heat, and serves as an energy reserve by storing fat. The hypodermis also provides cushioning and protection for underlying muscles and bones, and it supports the overlying dermis and epidermis. Additionally, it contains larger blood vessels and nerves that extend into the dermis, playing a role in the overall vascular and neural network of the skin. The hypodermis is essential for maintaining skin integrity and facilitating wound healing.
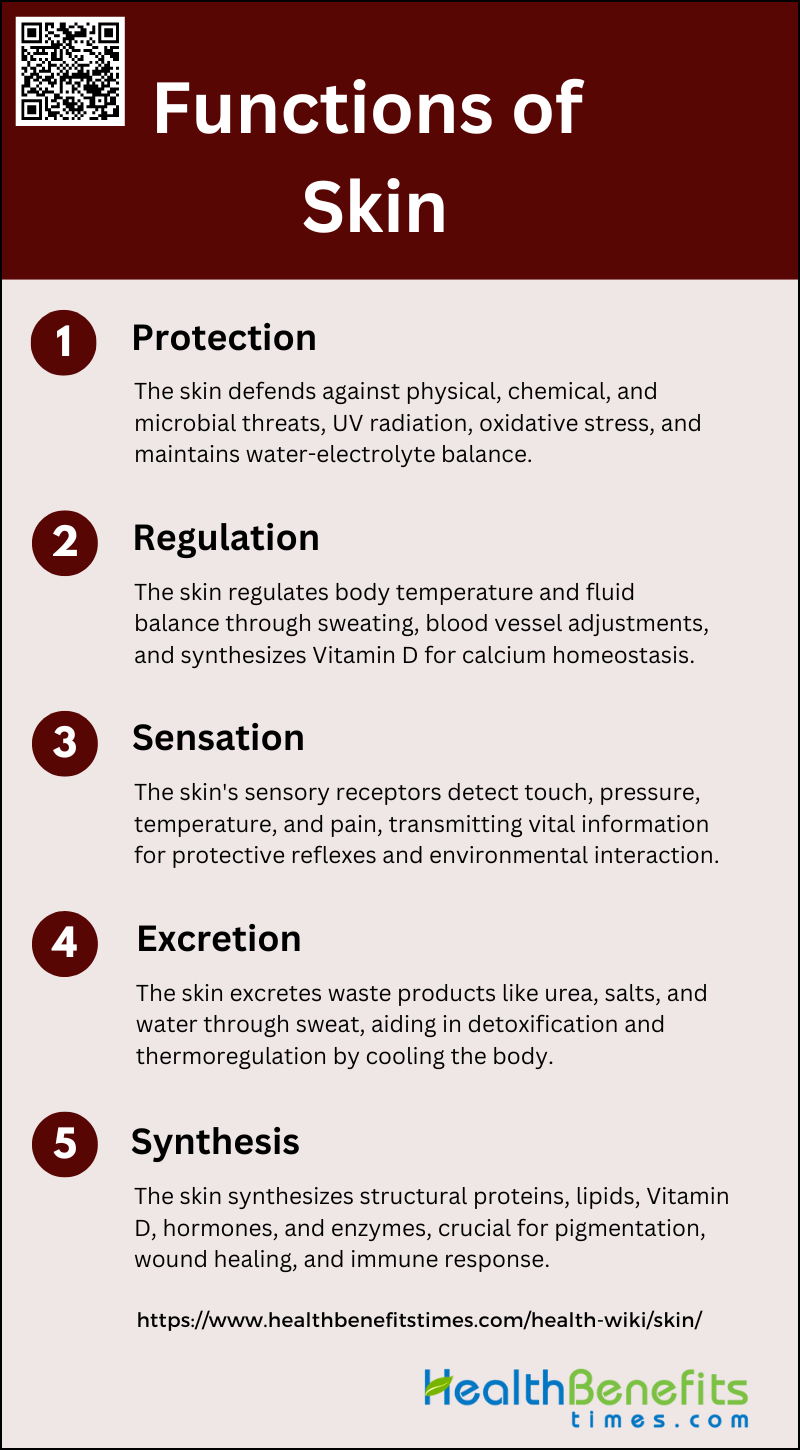
Functions of Skin
The skin is the body’s largest organ and serves multiple essential functions that are vital for overall health and well-being. It acts as a protective barrier, regulates body temperature, provides sensory information, excretes waste products, and synthesizes important compounds. Below are the key functions of the skin:
1. Protection
The skin serves as the body’s primary defense system against external threats, including physical, chemical, and microbiological hazards. It acts as a barrier to ultraviolet (UV) radiation, oxidative stress, and microbial invasion, thanks to its complex structure comprising the epidermis, dermis, and subcutaneous layers. The stratum corneum, the outermost layer of the epidermis, plays a crucial role in maintaining this barrier by controlling the transcutaneous movement of water and electrolytes. Additionally, the skin’s oiliness and the presence of antimicrobial peptides further enhance its protective functions, preventing undue water loss and resisting harmful substances.
2. Regulation
The skin is integral to the regulation of body temperature and fluid balance, contributing to homeostasis. It achieves thermoregulation through mechanisms such as sweating and vasodilation or vasoconstriction of blood vessels. The sweat glands secrete sweat, which evaporates to cool the body, while the vasomotor nerves control blood flow to the skin’s surface, aiding in heat dissipation or retention. Furthermore, the skin’s ability to synthesize Vitamin D upon exposure to sunlight is vital for calcium homeostasis and bone health. These regulatory functions are essential for maintaining the body’s internal environment within optimal limits.
3. Sensation
These receptors, including Meissner’s and Pacinian corpuscles, transmit sensory information to the brain, allowing for the perception of touch, pressure, temperature, and pain. This sensory input is crucial for protective reflexes and for interacting with the environment. The development of artificial skin, or e-skin, aims to emulate these sensory functions, enhancing applications in robotics and prosthetics by providing advanced sensory data processing capabilities.
4. Excretion
Sweat glands eliminate metabolic waste such as urea, salts, and water, which helps in detoxifying the body. This excretory function is not only vital for waste removal but also contributes to thermoregulation by cooling the body through the evaporation of sweat. The skin’s ability to excrete waste products underscores its importance in maintaining overall physiological balance and health.
5. Synthesis
Beyond its barrier and sensory roles, the skin functions as an active biofactory, synthesizing a range of structural proteins, lipids, and signaling molecules. It is involved in the production of Vitamin D, hormones, and various enzymes that play roles in processes such as pigmentation, wound healing, and immune response. The skin’s endocrine function includes the synthesis and metabolism of hormones like corticosteroids and sex hormones, which influence numerous physiological processes. This synthetic capability highlights the skin’s multifaceted role in maintaining bodily functions and overall health.
Types of Skin
Human skin varies in texture, color, and sensitivity, and can be categorized into several types based on these characteristics. Understanding your skin type is crucial for proper skincare and treatment. Below are the main types of skin:
1. Normal Skin
Normal skin is characterized by a balanced sebum production and good blood circulation, resulting in a smooth, even texture without significant blemishes or imperfections. It is neither too oily nor too dry, and it typically has a healthy glow. People with normal skin experience minimal sensitivity and have small, barely visible pores. To maintain normal skin, it is essential to follow a basic skincare routine that includes gentle cleansing, regular moisturizing, and sun protection. Using products that are not too harsh or overly hydrating helps in preserving the skin’s natural balance and preventing potential issues.
2. Dry Skin
Dry skin is marked by a lack of moisture and natural oils, leading to a rough, flaky, and sometimes itchy texture. It often feels tight, especially after cleansing, and may show visible lines and cracks. This skin type is more prone to irritation and can be exacerbated by environmental factors such as cold weather and low humidity. To care for dry skin, it is crucial to use gentle, hydrating cleansers and rich moisturizers that contain humectants and emollients. Regular application of a thick, nourishing moisturizer helps to lock in moisture and protect the skin barrier.
3. Oily Skin
Oily skin is characterized by an overproduction of sebum, which can lead to a shiny appearance and enlarged pores. This skin type is more prone to acne and blackheads due to the excess oil that can clog pores. People with oily skin often experience a greasy feeling, particularly in the T-zone (forehead, nose, and chin). To manage oily skin, it is important to use non-comedogenic products that do not clog pores, and to cleanse the skin regularly with a gentle, foaming cleanser. Using oil-free moisturizers and products containing salicylic acid can help control oil production and prevent breakouts.
4. Combination Skin
Combination skin features both oily and dry areas, typically with an oily T-zone and dry or normal cheeks. This skin type can be challenging to manage because it requires balancing the needs of both dry and oily areas. The T-zone may be prone to acne and shine, while the cheeks may feel tight and dry. To care for combination skin, it is essential to use a gentle cleanser and lightweight, non-comedogenic moisturizers. Targeted treatments, such as using a mattifying product on the T-zone and a hydrating serum on the cheeks, can help address the specific needs of each area.
5. Sensitive Skin
Sensitive skin is easily irritated and can react to various environmental factors, skincare products, and even stress. It often appears red, inflamed, and may feel itchy or burning. This skin type is more prone to conditions like rosacea and eczema. To care for sensitive skin, it is important to use hypoallergenic and fragrance-free products that are formulated for sensitive skin. Gentle cleansing and moisturizing with products containing soothing ingredients like aloe vera and chamomile can help calm and protect the skin. Avoiding harsh exfoliants and potential irritants is also crucial in managing sensitive skin.
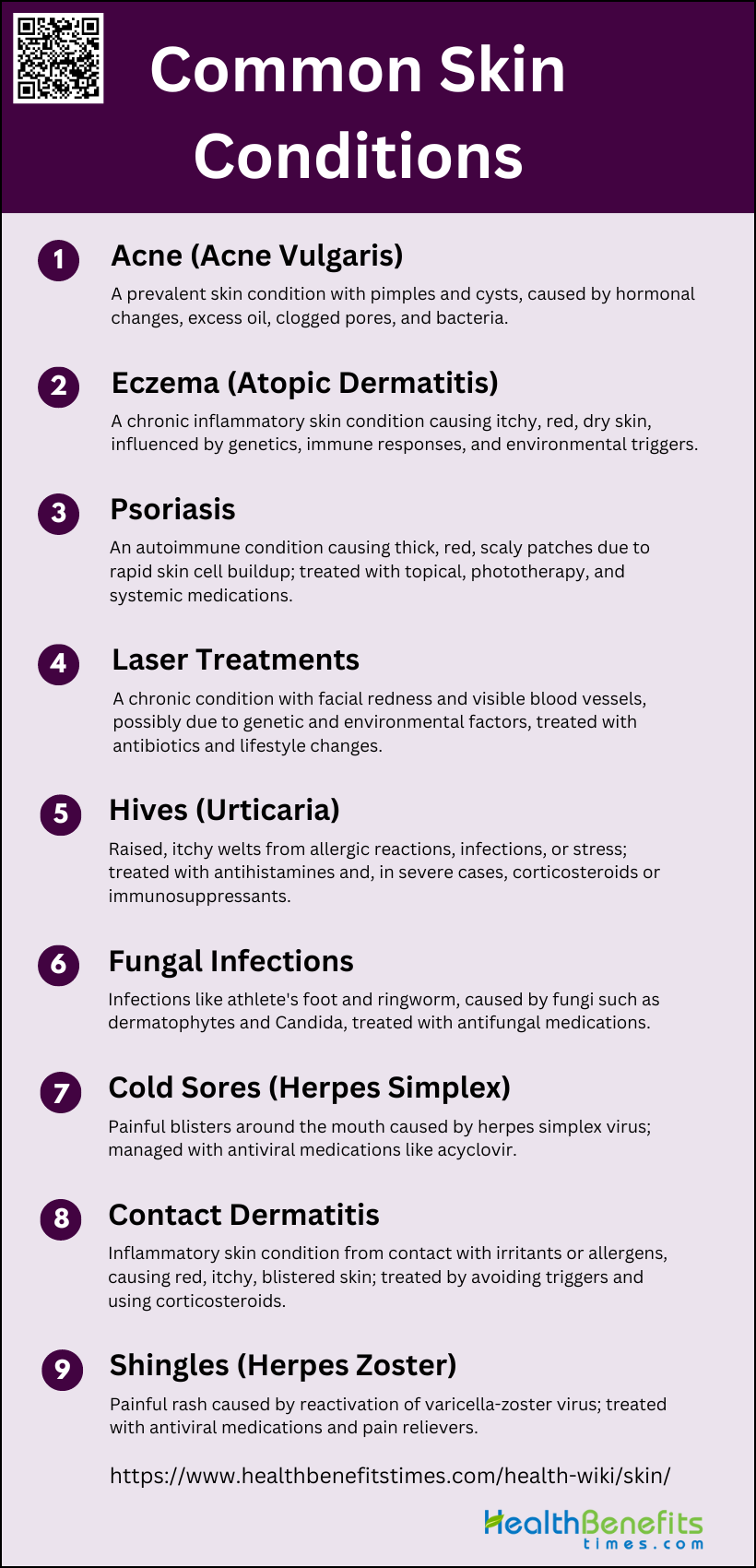
Common Skin Conditions
Proper diagnosis and treatment are essential for managing these conditions effectively. Below are some of the most common skin conditions:
1. Acne (Acne Vulgaris)
Acne vulgaris is a prevalent skin condition characterized by the presence of pimples, blackheads, and cysts, primarily affecting adolescents but also adults. It is caused by a combination of factors including hormonal changes, excess oil production, clogged pores, and bacterial infection (Propionibacterium acnes). Treatment options include topical retinoids, benzoyl peroxide, antibiotics, and in severe cases, oral isotretinoin. Maintaining a balanced skin microbiota is also crucial for managing acne.
2. Eczema (Atopic Dermatitis)
Eczema, or atopic dermatitis, is a chronic inflammatory skin condition marked by itchy, red, and dry skin. It is influenced by genetic factors, skin barrier defects, immune responses, and environmental triggers. Common treatments include topical corticosteroids, moisturizers, and immunomodulators. Addressing skin infections, particularly fungal infections like Malassezia and Candida, is also important for effective management.
3. Psoriasis
Psoriasis is an autoimmune condition that results in the rapid buildup of skin cells, leading to thick, red, scaly patches. It is caused by an overactive immune system and genetic predisposition. Treatments include topical treatments (corticosteroids, vitamin D analogs), phototherapy, and systemic medications (methotrexate, biologics) to reduce inflammation and slow down skin cell production.
4. Rosacea
Rosacea is a chronic skin condition characterized by facial redness, visible blood vessels, and sometimes acne-like bumps. The exact cause is unknown, but it is believed to involve a combination of genetic and environmental factors, as well as an imbalance in the skin microbiota. Treatment options include topical and oral antibiotics, laser therapy, and lifestyle changes to avoid triggers.
5. Hives (Urticaria)
Hives, or urticaria, are raised, itchy welts on the skin that can result from allergic reactions, infections, or stress. The exact cause is often unknown, but it involves the release of histamine and other chemicals from the skin. Treatment typically includes antihistamines to reduce itching and swelling, and in severe cases, corticosteroids or immunosuppressants.
6. Fungal Infections
Fungal infections of the skin, such as athlete’s foot, ringworm, and yeast infections, are caused by various fungi including dermatophytes, Candida, and Malassezia. These infections can cause itching, redness, and scaling. Treatment involves antifungal medications, either topical or oral, depending on the severity and location of the infection.
7. Cold Sores (Herpes Simplex)
Cold sores are caused by the herpes simplex virus (HSV), which leads to painful blisters around the mouth. The virus remains dormant in the body and can be reactivated by factors such as stress, illness, or sun exposure. Treatment includes antiviral medications like acyclovir to reduce the severity and duration of outbreaks.
8. Contact Dermatitis
Contact dermatitis is an inflammatory skin condition caused by direct contact with irritants or allergens, leading to red, itchy, and sometimes blistered skin. Treatment involves identifying and avoiding the triggering substance, using topical corticosteroids to reduce inflammation, and applying moisturizers to repair the skin barrier.
9. Shingles (Herpes Zoster)
Shingles is caused by the reactivation of the varicella-zoster virus, which also causes chickenpox. It results in a painful rash, often with blisters, typically on one side of the body. Treatment includes antiviral medications to reduce the severity and duration of the outbreak, pain relievers, and sometimes corticosteroids to manage severe pain.
Skin Care Tips
Taking care of your skin is essential for maintaining a healthy and youthful appearance. Incorporating effective skin care tips into your daily routine can make a significant difference. Here are some valuable tips to help you achieve radiant skin:
1. Protect Yourself from the Sun
Sun exposure is a major cause of accelerated skin aging and skin cancer. Effective sun protection includes limiting time in the midday sun, checking the Ultraviolet (UV) index, using shade wisely, wearing protective clothing such as broad hats and eyewear, and using sunscreen properly. Avoiding sunlamps and tanning beds is also crucial. Continuous sun protection from early childhood onward is essential to avoid extrinsic skin damage and skin cancer. Public health approaches are needed to implement preventive and basic skin care worldwide to reach high numbers of dermatological patients and care receivers.
2. Don’t Smoke
Smoking has detrimental effects on skin health, contributing to wrinkles, sagging skin, irregular pigmentation, and skin cancers. Environmental exposures to tobacco smoke progressively damage the skin’s cellular and extracellular structures. Avoiding smoking and tobacco is one of the most effective measures for maintaining healthy skin and a healthful life3. Lifestyle factors such as smoking negatively affect skin health, leading to conditions like dry skin, itching, ulcers, dyspigmentation, and wrinkles. Therefore, quitting smoking is crucial for both skin health and overall well-being.
3. Treat Your Skin Gently
Treating your skin gently involves using appropriate over-the-counter cleansers, moisturizers, sunscreens, and rejuvenators to create individualized, daily skin care regimens. Avoiding harsh soaps and limiting bath time can help maintain the skin’s natural oils. Patting the skin dry with a towel instead of rubbing it can also prevent irritation. Additionally, using a moisturizer that suits your skin type can help keep the skin hydrated and healthy. Gentle skin care practices are essential to prevent damage and maintain the skin’s integrity.
4. Eat a Healthy Diet
A well-balanced diet and adequate hydration are crucial for maintaining healthy skin. Consuming a variety of fruits, vegetables, lean proteins, and whole grains can provide the necessary nutrients for skin health. Health care providers recommend a diet rich in antioxidants, vitamins, and minerals to support skin function and appearance. Proper nutrition can help combat the effects of environmental stressors and aging on the skin. Therefore, eating a healthy diet is a fundamental aspect of skin care and overall health.
5. Manage Stress
Managing stress is vital for maintaining healthy skin. Chronic stress can trigger skin problems such as acne, eczema, and psoriasis. Stress management techniques such as exercise, meditation, and adequate sleep can help improve skin health. Health care providers emphasize the importance of a balanced lifestyle to reduce stress and its impact on the skin. By managing stress effectively, individuals can promote better skin health and overall well-being.
6. Simplify Your Skin Care Routine
Simplifying your skin care routine can make it more manageable and effective. Using a few well-chosen products that suit your skin type can provide the necessary care without overwhelming the skin. Over-the-counter cosmeceuticals such as cleansers, moisturizers, and sunscreens can be used to create a basic yet effective skin care regimen. Health care providers can guide individuals in selecting the right products and avoiding unnecessary ones. A simplified routine can help maintain healthy skin without causing irritation or damage.
7. Avoid Tanning Beds
Avoiding tanning beds is crucial for preventing skin cancer and other skin damage. The use of ultraviolet-emitting indoor tanning beds poses significant health risks, including potentially deadly melanoma and eye problems. Young adults, in particular, should be educated on the dangers of tanning beds and encouraged to avoid them. Primary care counseling and public health campaigns can help reduce the incidence of skin cancer by promoting safer alternatives to tanning beds. By avoiding tanning beds, individuals can significantly lower their risk of developing skin cancer.
Diet and Skin
Maintaining healthy, glowing skin isn’t just about the products you apply; it’s also about what you eat. Your diet plays a crucial role in skin health, providing essential nutrients that can help combat aging, acne, and other skin issues.
1. Impact of Nutrition on Skin Health
Nutrition plays a crucial role in maintaining skin health and can influence various skin conditions. Essential nutrients such as vitamins, carotenoids, and polyunsaturated fatty acids have been shown to improve skin integrity and function. For instance, vitamins and carotenoids provide photoprotection against ultraviolet light, although their sun-protection factor is relatively small compared to topical sunscreens. Nutritional patterns can affect the clinical course of skin diseases like acne, atopic dermatitis, and aging. Dietary interventions have demonstrated beneficial effects on skin appearance and health by restoring impaired skin structural and functional integrity. Additionally, supplementation with specific nutrients can boost cell-mediated immunity, which is particularly beneficial for elderly individuals. Therefore, a balanced diet rich in essential nutrients is vital for maintaining healthy skin and mitigating the effects of various skin disorders.
2. Foods Beneficial for Healthy Skin
Certain foods and dietary supplements have been identified as beneficial for skin health. For example, foods rich in antioxidants, such as fruits and vegetables, can help reduce oxidative stress and inflammation, which are key factors in skin aging and other skin conditions. Specific foods like curcumin, green tea, and coffee have shown effectiveness in treating psoriasis, while ginger has been beneficial for alopecia areata. Probiotics and Korean red ginseng are effective for atopic dermatitis, and essential oils from bergamot and sweet oranges can help manage acne by inhibiting sebaceous gland secretion. Additionally, supplements containing vitamins A, C, E, zinc, and selenium have shown promising results in improving skin conditions and providing UV protection. Incorporating these foods and supplements into the diet can enhance skin health and provide therapeutic benefits for various skin disorders.