Red blood cells (RBCs), also known as erythrocytes, are the most abundant cell type in the human body, playing a crucial role in oxygen transport. These cells are primarily responsible for carrying oxygen from the lungs to the tissues and returning carbon dioxide from the tissues to the lungs for exhalation. RBCs are characterized by their biconcave shape, which increases their surface area for gas exchange and allows them to navigate through narrow blood vessels. They lack a nucleus and most organelles, which provides more space for hemoglobin, the protein that binds oxygen. The average lifespan of an RBC is about 120 days, after which they are typically removed from circulation by the spleen. The production of RBCs, known as erythropoiesis, occurs in the bone marrow and is regulated by the hormone erythropoietin, primarily in response to oxygen levels in the body. Their metabolism is relatively simple, reflecting systemic metabolic homeostasis, and any alterations can indicate physiological changes, such as aging or disease conditions like Down syndrome.
Structure of Red Blood Cells
Detailed description of RBCs’ structure
Red blood cells (RBCs) are highly specialized cells characterized by their biconcave disk shape, which optimizes their flow properties in blood vessels and capillaries. They are typically about 7-8 micrometers in diameter and 2 micrometers thick at their thickest point. The cell membrane of RBCs is a lipid bilayer embedded with various proteins, including transmembrane proteins that anchor the membrane to a cytoskeletal network composed of proteins like spectrin and actin. The cytoplasm of RBCs is rich in hemoglobin, a protein responsible for oxygen transport. Hemoglobin constitutes about 95% of the dry weight of the cell and is crucial for the cell’s primary function of oxygen delivery.
How the Structure Relates to Their Function
The unique biconcave shape of RBCs increases their surface area-to-volume ratio, facilitating efficient gas exchange. This shape, combined with the flexibility provided by the cytoskeletal network, allows RBCs to deform as they pass through narrow capillaries without rupturing. The absence of organelles, including the nucleus, maximizes space for hemoglobin, enhancing the cell’s oxygen-carrying capacity. The lipid bilayer and associated proteins contribute to the cell’s stability and deformability, essential for enduring the mechanical stress encountered during circulation. These structural features collectively enable RBCs to efficiently transport oxygen from the lungs to tissues and return carbon dioxide from tissues to the lungs.
Comparison with Other Blood Components
Unlike RBCs, white blood cells (WBCs) and platelets have more complex structures with nuclei and various organelles. WBCs are involved in immune responses and have a variety of forms, including lymphocytes, monocytes, and granulocytes, each with specific functions in pathogen defense and inflammation. Platelets, or thrombocytes, are small, anucleate cell fragments derived from megakaryocytes and play a crucial role in blood clotting and hemostasis. While RBCs are primarily concerned with gas transport, WBCs and platelets are essential for immune defense and wound healing, respectively. The structural simplicity of RBCs, lacking nuclei and organelles, is a key adaptation for their specialized role in oxygen transport, contrasting with the more complex structures of WBCs and platelets that support their diverse functions.
Function of Red Blood Cells
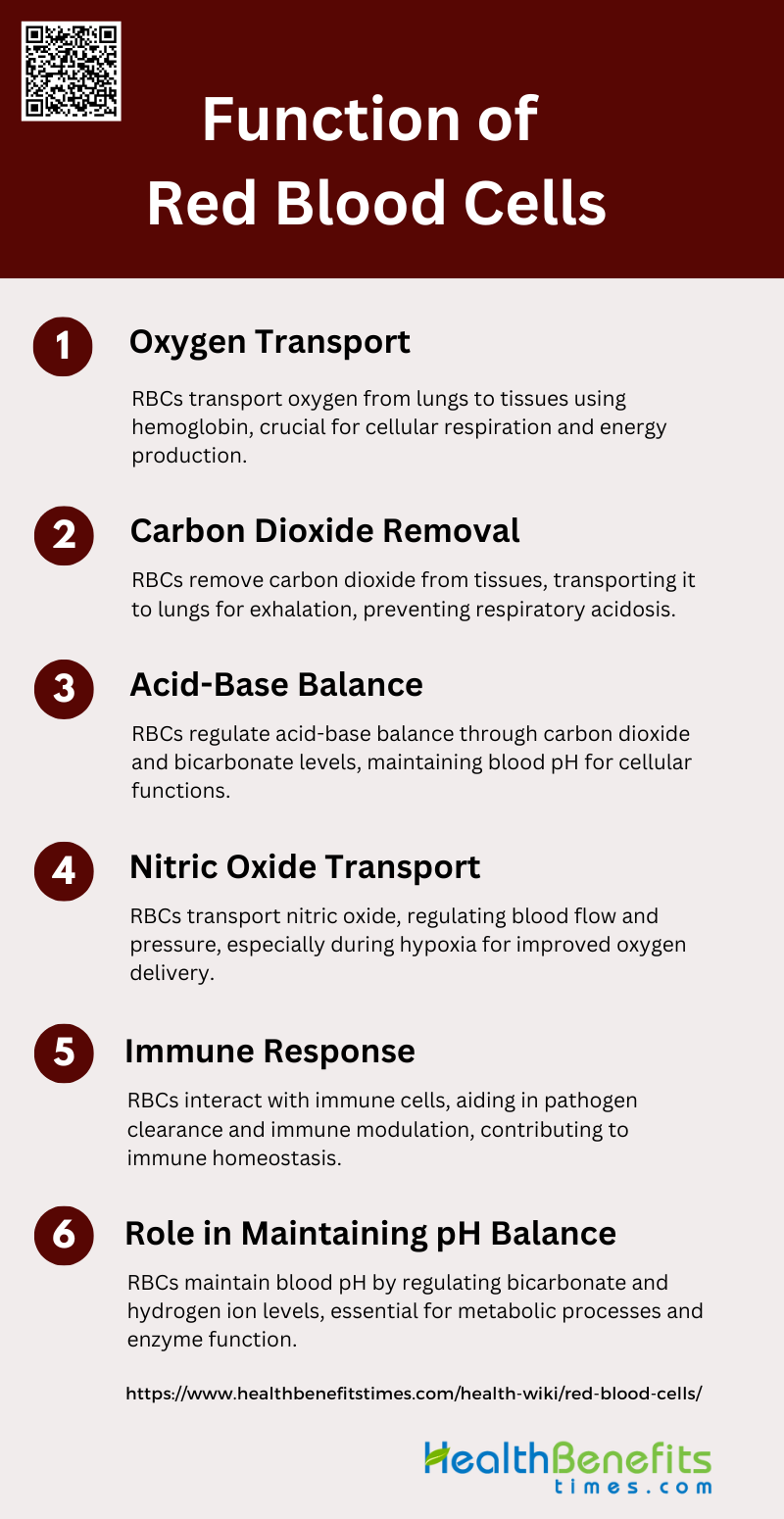
Red blood cells (RBCs) play a vital role in maintaining physiological homeostasis by transporting gases throughout the body. They are primarily responsible for delivering oxygen from the lungs to tissues and removing carbon dioxide from tissues to the lungs. Key functions of RBCs include:
1. Oxygen Transport
Red blood cells (RBCs) are primarily responsible for the transport of oxygen from the lungs to various tissues throughout the body. This function is facilitated by hemoglobin, a protein within RBCs that binds to oxygen molecules. The flexible structure of RBCs allows them to navigate through even the smallest capillaries, ensuring efficient oxygen delivery to all cells and tissues. This oxygen transport is crucial for cellular respiration, which is the process by which cells produce energy. The efficiency of this system is vital for maintaining the body’s overall metabolic functions and energy levels.
2. Carbon Dioxide Removal
In addition to oxygen transport, RBCs play a critical role in the removal of carbon dioxide, a waste product of cellular metabolism. Carbon dioxide is transported from the tissues back to the lungs, where it is exhaled. Hemoglobin in RBCs also binds to carbon dioxide, facilitating its transport. This dual role of RBCs in gas exchange is essential for maintaining the body’s respiratory balance and preventing the buildup of carbon dioxide, which can lead to respiratory acidosis if not properly managed.
3. Acid-Base Balance
RBCs contribute significantly to the body’s acid-base balance, a critical aspect of homeostasis. They achieve this by regulating the levels of carbon dioxide and bicarbonate in the blood. The enzyme carbonic anhydrase, present in RBCs, catalyzes the conversion of carbon dioxide and water to carbonic acid, which then dissociates into bicarbonate and hydrogen ions. This reaction helps buffer the blood, maintaining its pH within a narrow range, which is crucial for normal cellular functions.
4. Nitric Oxide Transport
RBCs are also involved in the transport and regulation of nitric oxide (NO), a molecule that plays a vital role in vascular tone and blood flow. NO is produced by endothelial cells and can bind to hemoglobin in RBCs. This binding regulates the bioavailability of NO, which is essential for vasodilation and maintaining blood pressure. During hypoxic conditions, RBCs release NO, which helps to improve blood flow and oxygen delivery to tissues. This function highlights the dynamic role of RBCs beyond mere gas transport.
5. Immune Response
RBCs have been found to play a role in the immune response, interacting with various immune cells such as macrophages and platelets. They can influence the immune system by modulating the activity of these cells and participating in the clearance of pathogens. RBCs can also bind to immune complexes and facilitate their removal from the circulation, thus preventing excessive immune reactions and maintaining immune homeostasis. This interaction underscores the multifaceted roles of RBCs in both respiratory and immune functions.
6. Role in Maintaining pH Balance
The role of RBCs in maintaining pH balance is closely linked to their function in acid-base balance. By regulating the levels of carbon dioxide and bicarbonate, RBCs help to buffer the blood and maintain its pH within the optimal range. This is crucial for enzyme function and overall metabolic processes. The ability of RBCs to rapidly respond to changes in pH and adjust the levels of bicarbonate and hydrogen ions ensures that the body’s internal environment remains stable, which is essential for health and disease prevention.
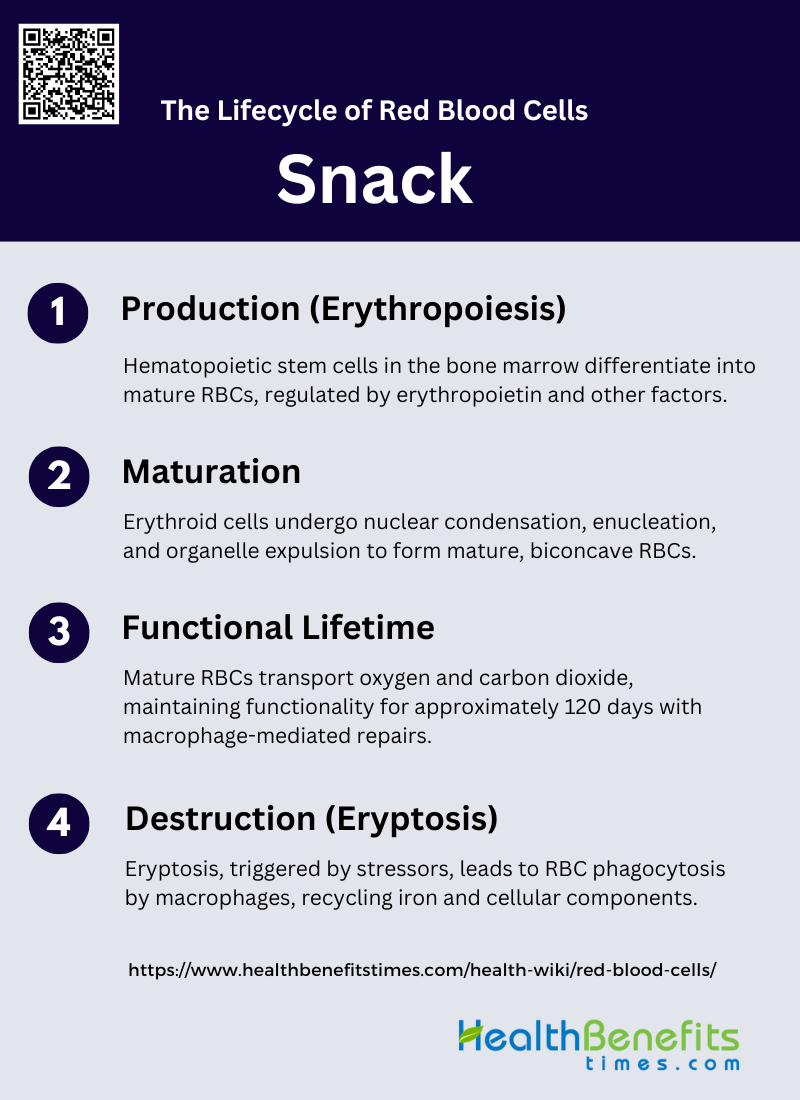
The lifecycle of Red Blood Cells
Red blood cells (RBCs) undergo a well-defined lifecycle that ensures efficient oxygen transport and waste removal. From their production in the bone marrow to their eventual breakdown in the spleen, RBCs maintain critical bodily functions. The stages of the RBC lifecycle include:
1. Production (Erythropoiesis)
Erythropoiesis is the process by which hematopoietic stem cells differentiate into mature red blood cells (RBCs). This complex, multi-step process occurs primarily in the bone marrow and is tightly regulated by various signaling pathways, transcription factors, and microRNAs. The differentiation begins with hematopoietic stem cells transforming into early erythroid progenitors, such as burst-forming units-erythroid (BFU-E), and then into late erythroid progenitors, known as colony-forming units-erythroid (CFU-E). These progenitors further differentiate into morphologically recognizable erythroid precursors. A critical regulator of erythropoiesis is erythropoietin (EPO), which promotes the survival and proliferation of erythroid cells by inhibiting apoptosis through pathways like PI3K/AKT and upregulating anti-apoptotic proteins such as Bcl-XL.
2. Maturation
The maturation of erythroid cells involves several morphological and biochemical changes, culminating in the formation of mature erythrocytes. During this process, erythroblasts undergo nuclear condensation and enucleation, resulting in the formation of reticulocytes. These reticulocytes then expel their organelles, including mitochondria, through a process known as mitophagy, and remodel their plasma membrane to become fully mature, biconcave red blood cells. The interaction between erythroblasts and macrophages in erythroblastic islands is crucial for the enucleation process. Additionally, various proteins and signaling pathways, such as those involving actin cytoskeleton rearrangement and clathrin-dependent vacuole formation, play essential roles in these final maturation steps.
3. Functional Lifetime
Once mature, red blood cells enter the bloodstream, where they have a functional lifespan of approximately 120 days. During this time, they are responsible for transporting oxygen from the lungs to tissues and returning carbon dioxide to the lungs for exhalation. Despite lacking organelles and the ability to synthesize new proteins, RBCs maintain their functionality through robust antioxidant defense mechanisms and continuous repair processes mediated by macrophages in the spleen. These macrophages help repair minor damages and maintain the integrity of the RBCs, ensuring their efficient function throughout their lifespan.
4. Destruction (Eryptosis)
Eryptosis is the programmed cell death of red blood cells, analogous to apoptosis in nucleated cells. This process is triggered by various stressors, including oxidative stress, increased intracellular calcium levels, and changes in cell membrane potential. Eryptosis involves the exposure of phosphatidylserine on the outer leaflet of the RBC membrane, signaling macrophages to phagocytose and remove the senescent or damaged cells from circulation. This mechanism is essential for recycling iron and other cellular components. However, in pathological conditions such as chronic kidney disease, the rate of eryptosis can be significantly increased, leading to a shortened RBC lifespan and contributing to anemia.
Normal Ranges of Red Blood Cells
Explanation of RBC Count and Its Significance
Red blood cell (RBC) count is a critical parameter in the evaluation of an individual’s overall health. RBCs are responsible for transporting oxygen from the lungs to the rest of the body and returning carbon dioxide to the lungs for exhalation. The hemoglobin within RBCs binds to oxygen, facilitating this essential process. Accurate RBC counts are vital for diagnosing and managing various medical conditions, particularly anemias, which are characterized by a deficiency in the number or quality of RBCs. The significance of RBC count extends to both clinical and academic fields, as it helps in understanding the physiological variations and pathological states of the human body.
Normal RBC Count Ranges
Maintaining normal red blood cell (RBC) counts is crucial for effective physiological function and overall health. These ranges can vary based on factors such as age, sex, and altitude. Typical RBC counts are measured in millions per microliter (µL) of blood and include:
- Men: The normal RBC count for men typically ranges from 4.7 to 6.1 million cells per microliter of blood. This range is based on extensive studies and is crucial for diagnosing conditions like polycythemia and anemia.
- Women: For women, the normal RBC count is slightly lower, ranging from 4.2 to 5.4 million cells per microliter. This difference is attributed to physiological variations, including hormonal influences and menstrual blood loss.
- Children: The RBC count in children varies significantly with age. For instance, newborns have higher RBC counts, which gradually decrease as they grow. The normal range for children from birth to 13 years has been established through comprehensive studies, providing a basis for pediatric health assessments.
Factors Affecting RBC Count
Several factors can influence RBC count, including age, sex, altitude, and health conditions. Age is a significant factor, with newborns having higher RBC counts that stabilize as they age. Sex differences are evident, with men generally having higher RBC counts than women due to hormonal differences and other physiological factors. Altitude also plays a crucial role; individuals living at higher altitudes tend to have higher RBC counts to compensate for lower oxygen levels in the environment. Health conditions such as anemia, dehydration, and chronic diseases can significantly alter RBC counts, necessitating careful monitoring and management.
Methods of Measuring RBC Count
The most common method for measuring RBC count is the Complete Blood Count (CBC) test. This test provides a comprehensive overview of the different components of blood, including RBC count, hemoglobin concentration, and hematocrit levels. Advanced techniques such as flow cytometry and laser light scattering have been developed to improve the accuracy of these measurements. These methods allow for precise determination of cell volume and hemoglobin concentration, which are essential for diagnosing and managing various hematological conditions. The CBC test remains a cornerstone in clinical diagnostics due to its reliability and comprehensive nature.
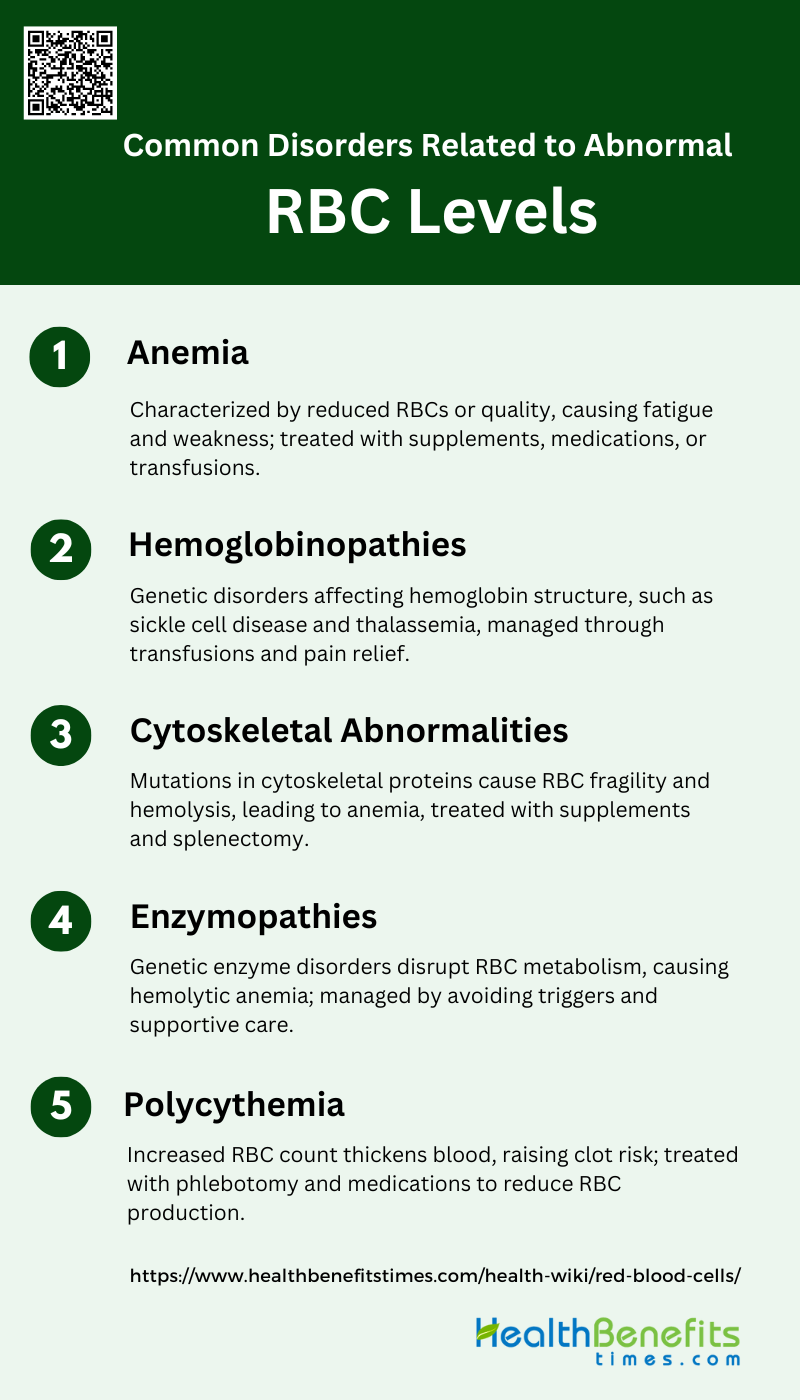
Common Disorders Related to abnormal RBC levels
Abnormal red blood cell (RBC) levels can indicate various health issues, ranging from nutritional deficiencies to chronic diseases. Both elevated and reduced RBC counts can lead to significant clinical symptoms and require medical attention. Common disorders associated with abnormal RBC levels include:
1. Anemia
Anemia is a condition characterized by a deficiency in the number or quality of red blood cells (RBCs), which impairs the blood’s ability to carry oxygen. Causes of anemia include genetic mutations, nutritional deficiencies, chronic diseases, and increased RBC destruction. Symptoms often include fatigue, weakness, shortness of breath, and pallor. Treatments vary depending on the type and cause of anemia but may include dietary supplements (iron, vitamin B12, folic acid), medications to stimulate RBC production, and in severe cases, blood transfusions or bone marrow transplants. Research indicates that increased intracellular calcium in RBCs is a common factor in various types of anemia, suggesting potential therapeutic targets.
2. Hemoglobinopathies
Hemoglobinopathies are genetic disorders affecting the structure or production of hemoglobin, the protein in RBCs that carries oxygen. Common hemoglobinopathies include sickle cell disease and thalassemia. These conditions are caused by mutations in the genes encoding hemoglobin. Symptoms can range from mild anemia to severe pain, organ damage, and increased risk of infections. Treatments often involve managing symptoms and complications through blood transfusions, pain management, and in some cases, bone marrow transplants. Advances in genetic testing have improved the diagnosis and understanding of these disorders, aiding in better management and treatment strategies.
3. Cytoskeletal Abnormalities
Cytoskeletal abnormalities in RBCs are often due to mutations in the genes encoding cytoskeletal proteins, leading to conditions such as hereditary spherocytosis, elliptocytosis, and stomatocytosis. These disorders result in RBCs that are more prone to hemolysis, causing hemolytic anemia. Symptoms include jaundice, splenomegaly, and fatigue. Diagnosis typically involves blood smear analysis and specialized tests like ektacytometry. Treatments may include folic acid supplementation, splenectomy, and in severe cases, blood transfusions. Recent studies highlight the role of next-generation sequencing in diagnosing these conditions, providing insights into their genetic basis and aiding in the development of targeted therapies.
4. Enzymopathies
Enzymopathies are genetic disorders affecting enzymes involved in RBC metabolism, leading to hemolytic anemia. Common enzymopathies include glucose-6-phosphate dehydrogenase (G6PD) deficiency and pyruvate kinase (PK) deficiency. These conditions disrupt the normal metabolic processes in RBCs, making them more susceptible to oxidative damage and hemolysis. Symptoms include jaundice, fatigue, and dark urine. Diagnosis is based on enzyme activity assays and genetic testing. Treatment focuses on avoiding triggers that cause hemolysis, such as certain foods and medications, and managing symptoms through supportive care and, in severe cases, blood transfusions.
5. Polycythemia
Polycythemia is a condition characterized by an increased number of RBCs, which can lead to thickened blood and an increased risk of clotting. Causes include genetic mutations, chronic hypoxia, and tumors producing erythropoietin. Symptoms may include headaches, dizziness, itching, and an increased risk of thrombotic events. Treatment aims to reduce the RBC count and improve blood flow, often through phlebotomy, medications to suppress bone marrow activity, and managing underlying conditions. Understanding the molecular mechanisms and genetic factors involved in polycythemia is crucial for developing effective treatments and improving patient outcomes.
Symptoms of RBC Disorders
Red blood cell (RBC) disorders can manifest through a variety of symptoms, affecting different parts of the body. Common symptoms include:
1. Fatigue and Weakness: Due to reduced oxygen delivery to tissues, individuals often feel tired and weak.
2. Pallor: A noticeable paleness of the skin and mucous membranes, particularly the conjunctiva and face.
3. Shortness of Breath: Difficulty in breathing, especially during physical activity, as a result of decreased oxygen levels in the blood.
4. Jaundice: Yellowing of the skin and eyes due to the breakdown of abnormal RBCs, commonly seen in hemolytic anemias.
5. Frequent Infections: Increased susceptibility to infections, as seen in disorders like sickle cell disease, due to compromised immune function.