Prostaglandins are lipid compounds derived from fatty acids, primarily arachidonic acid, through the cyclooxygenase (COX) enzyme pathway. They play a crucial role in various physiological and pathological processes in the human body, including inflammation, pain, fever, and the regulation of blood flow. There are several types of prostaglandins, such as PGE2, PGD2, PGF2α, and PGI2, each with distinct functions and effects on different tissues and organs. These molecules act as local hormones, binding to specific receptors on target cells to trigger a range of cellular responses. For instance, during inflammation, prostaglandins contribute to vasodilation and increased permeability of blood vessels, facilitating the immune response. However, they can also be involved in pathological conditions when their production is dysregulated, leading to chronic inflammation and pain.
Chemical structure and classification
Chemical structure and classification are fundamental aspects of chemistry that facilitate the organization, comparison, and understanding of chemical compounds. The development of automated systems for chemical classification, such as ClassyFire, has significantly advanced the field by providing a comprehensive, structure-based taxonomy known as ChemOnt. This system categorizes compounds into over 4800 different classes based on their structural features, enabling large-scale, rapid classification of millions of compounds. Similarly, ChEBI offers a dual classification system based on both structural features and biological roles, enhancing the retrieval and organization of chemical data. Automated classification methods, such as those using SMARTS expressions and logical operators, further refine the precision and granularity of chemical class definitions, allowing for high-quality, error-free classification in chemical databases. These advancements not only streamline the annotation and analysis of chemical compounds but also support various cheminformatics tasks, including the prediction of biological activities and the study of metabolic pathways. Overall, the integration of computational tools and ontologies in chemical classification has revolutionized the way chemists and researchers manage and interpret vast chemical datasets.
Types of Prostaglandins
Prostaglandins are a diverse group of lipid compounds that have varying effects on different tissues and organs. Each type of prostaglandin plays a unique role in physiological processes such as inflammation, blood flow regulation, and pain modulation. Below are some of the key types of prostaglandins:
1. Prostaglandin E2 (PGE2)
Prostaglandin E2 (PGE2) is a potent lipid mediator synthesized from arachidonic acid through the action of cyclooxygenases (COX-1 and COX-2). It is the most abundantly detected prostaglandin in various tissues and exerts a wide range of physiological and pathological actions via four receptor subtypes (EP1-4). PGE2 plays a significant role in exacerbating inflammatory responses and immune diseases. It induces acute inflammation through mast cell activation via the EP3 receptor and chronic inflammation through T helper cell differentiation and proliferation via the EP2 and EP4 receptors. Additionally, PGE2 is involved in various cellular signaling pathways, including those that regulate cyclic AMP and calcium ion concentrations.
2. Prostaglandin I2 (PGI2 or Prostacyclin)
Prostaglandin I2 (PGI2), also known as prostacyclin, is another important prostaglandin synthesized from arachidonic acid. It is primarily produced by endothelial cells and plays a crucial role in vascular homeostasis. PGI2 acts through its specific receptor, the IP receptor, to induce vasodilation and inhibit platelet aggregation, thus preventing thrombosis. It also has anti-inflammatory properties and can modulate immune responses. The balance between PGI2 and thromboxane A2 (TXA2) is essential for maintaining cardiovascular health, as an imbalance can lead to conditions such as hypertension and atherosclerosis. Although not explicitly covered in the provided papers, PGI2’s role in vascular biology is well-documented in the literature.
3. Prostaglandin D2 (PGD2)
Prostaglandin D2 (PGD2) is another member of the prostaglandin family, synthesized from arachidonic acid. It is primarily produced by mast cells and plays a significant role in allergic reactions and inflammation. PGD2 acts through its receptors, DP1 and DP2, to mediate various physiological responses, including bronchoconstriction, vasodilation, and inhibition of platelet aggregation. It is also involved in the regulation of adipogenesis and obesity, as it influences the differentiation of preadipocytes to mature adipocytes. PGD2’s role in adipogenesis highlights its importance in metabolic processes and its potential impact on lifestyle-related diseases such as cardiovascular disease and type 2 diabetes mellitus.
4. Prostaglandin F2α (PGF2α)
Prostaglandin F2α (PGF2α) is a prostaglandin that plays a crucial role in reproductive physiology, particularly in the regulation of the menstrual cycle and labor. It is synthesized from arachidonic acid and acts through its receptor, the FP receptor. PGF2α is involved in the contraction of smooth muscle cells, including those in the uterus, making it essential for processes such as menstruation and childbirth. Additionally, PGF2α has been shown to regulate adipogenesis and obesity by influencing the differentiation of preadipocytes to mature adipocytes. Its role in these processes underscores its importance in both reproductive and metabolic health.
Functions of Prostaglandins
Prostaglandins are versatile lipid compounds that perform a wide range of functions within the human body. They are involved in critical processes such as inflammation, pain sensation, and the regulation of blood flow. The following is a list of key functions of prostaglandins:
1. Role in Inflammation and Healing
Prostaglandins play a crucial role in the inflammatory response and healing processes. They are lipid autacoids derived from arachidonic acid and are generated by the action of cyclooxygenase (COX) enzymes. Prostaglandins mediate various aspects of inflammation, including vasodilation, increased vascular permeability, and leukocyte recruitment to the site of injury. They are involved in both the promotion and resolution of inflammation, highlighting their dual role in these processes. Nonsteroidal anti-inflammatory drugs (NSAIDs) inhibit COX enzymes, thereby reducing prostaglandin synthesis and alleviating inflammation and pain.
2. Regulation of Blood Flow
Prostaglandins are key regulators of blood flow, particularly through their vasodilatory effects. They are known to dilate peripheral blood vessels, thereby lowering arterial pressure. This vasodilatory effect can be mediated by changes in circulating blood levels of prostaglandins or their concentration in blood vessel walls. Prostaglandins also play a role in regulating renal blood flow and sodium reabsorption, which further influences blood pressure. Their ability to modulate blood flow is critical during conditions of increased metabolic demand, such as exercise and reactive hyperemia.
3. Effects on Reproductive Health
Prostaglandins significantly impact reproductive health by influencing various stages of the reproductive process, including ovulation, fertilization, implantation, and labor. For instance, prostaglandin E2 (PGE2) is crucial for the fertilization of the ovum in vivo. Mice deficient in the EP2 receptor for PGE2 exhibit infertility due to the failure of the ovum to become fertilized. Prostaglandins are also present in high concentrations in menstrual and amniotic fluids, suggesting their role in labor and postpartum uterine contraction. These findings underscore the importance of prostaglandins in reproductive physiology .
4. Involvement in Gastric Acid Secretion
Prostaglandins play a protective role in the gastrointestinal tract by regulating gastric acid secretion and maintaining mucosal integrity. They inhibit gastric acid secretion and promote the production of mucus and bicarbonate, which protect the gastric lining from acidic damage. Prostaglandins such as PGE2 and prostacyclin (PGI2) are particularly effective in this regard. Their cytoprotective properties help prevent ulcer formation and accelerate ulcer healing, making them crucial for gastrointestinal health.
5. Influence on Kidney Function
Prostaglandins are vital modulators of renal function, particularly in regulating renal blood flow and glomerular filtration rate. They are synthesized in the kidneys and influence various aspects of renal hemodynamics. In states of decreased renal perfusion, prostaglandins help maintain renal blood flow and glomerular filtration by counteracting vasoconstrictive forces. NSAIDs, which inhibit prostaglandin synthesis, can lead to significant alterations in renal function, especially in conditions of reduced renal perfusion. This highlights the importance of prostaglandins in maintaining renal homeostasis.
6. Influence on Blood Clotting
Prostaglandins have a complex role in blood clotting, primarily through their effects on platelet aggregation. Prostaglandins such as thromboxane A2 (TXA2) promote platelet aggregation and vasoconstriction, which are essential for clot formation. Conversely, prostacyclin (PGI2) inhibits platelet aggregation and promotes vasodilation, thereby preventing excessive clotting. This balance between pro-aggregatory and anti-aggregatory prostaglandins is crucial for maintaining hemostasis and preventing thrombotic disorders. The differential effects of various prostaglandins on blood clotting underscore their regulatory importance in vascular health.
Health Benefits of Prostaglandins
Prostaglandins, though often associated with pain and inflammation, also confer several health benefits essential for maintaining bodily functions. These lipid compounds play pivotal roles in various physiological processes, from protecting the stomach lining to regulating blood flow. Below are some of the key health benefits of prostaglandins:
1. Gastrointestinal Health
Prostaglandins play a crucial role in maintaining gastrointestinal health by regulating various physiological processes. They help protect the gastric mucosa by stimulating the secretion of mucus and bicarbonate, which form a protective barrier against stomach acid. Additionally, prostaglandins promote blood flow to the stomach lining, aiding in tissue repair and regeneration. However, the use of nonsteroidal anti-inflammatory drugs (NSAIDs) can inhibit prostaglandin synthesis, leading to gastrointestinal complications such as ulcers and bleeding. Understanding the balance of prostaglandin activity is essential for developing therapeutic strategies to protect the gastrointestinal tract while managing pain and inflammation.
2. Cardiovascular Health
Prostaglandins are vital in cardiovascular health, influencing vascular tone, platelet aggregation, and myocardial function. They help regulate blood pressure by causing vasodilation or vasoconstriction, depending on the specific type of prostaglandin involved. For instance, prostacyclin (PGI2) is a potent vasodilator and inhibitor of platelet aggregation, playing a protective role against thrombosis and atherosclerosis. Conversely, thromboxane A2 (TXA2) promotes vasoconstriction and platelet aggregation, which can contribute to cardiovascular diseases. The dual roles of prostaglandins in promoting and resolving inflammation highlight their complex involvement in cardiovascular health.
3. Reproductive Health
Prostaglandins are essential in reproductive health, influencing various aspects of the reproductive system in both males and females. In females, they are involved in the regulation of the menstrual cycle, ovulation, and labor. Prostaglandins such as PGE2 and PGF2α play critical roles in uterine contractions and cervical ripening during childbirth. In males, prostaglandins are found in seminal fluid and are believed to aid in sperm motility and function. The therapeutic use of prostaglandins in gynecology includes the induction of labor and the treatment of certain types of infertility.
4. Inflammation and Pain Management
Prostaglandins are key mediators in the inflammatory response and pain perception. They are produced at sites of tissue damage or infection, where they contribute to the classic signs of inflammation: redness, heat, swelling, and pain. Prostaglandins such as PGE2 and PGI2 sensitize nerve endings, enhancing the perception of pain. NSAIDs alleviate pain and inflammation by inhibiting the cyclooxygenase enzymes (COX-1 and COX-2) responsible for prostaglandin synthesis. However, prostaglandins also play roles in resolving inflammation, indicating their dual function in both promoting and resolving inflammatory processes.
5. Eye Health
Prostaglandins have significant applications in ophthalmology, particularly in the treatment of glaucoma. Prostaglandin analogues are effective in reducing intraocular pressure (IOP) by increasing the outflow of aqueous humor from the eye. These agents can lower IOP by 20-40%, making them a first-line therapy for glaucoma. However, caution is advised in patients with a history of inflammatory eye diseases, as prostaglandins can exacerbate conditions like uveitis and keratitis. The safety profile of prostaglandin analogues generally supports their widespread use in managing ocular hypertension and glaucoma.
6. Renal Function
Prostaglandins are crucial in maintaining renal function by regulating blood flow within the kidneys and modulating the balance of salt and water. They help maintain glomerular filtration rate (GFR) and promote the excretion of sodium, which is vital for blood pressure regulation. NSAIDs can impair renal function by inhibiting prostaglandin synthesis, leading to reduced renal blood flow and potential kidney damage. Understanding the role of prostaglandins in renal physiology is essential for developing treatments that protect kidney function while managing pain and inflammation.
7. Respiratory Health
Prostaglandins play a role in respiratory health by modulating airway tone and inflammatory responses in the lungs. They can cause bronchoconstriction or bronchodilation, influencing conditions such as asthma and chronic obstructive pulmonary disease (COPD). Prostaglandins like PGE2 have anti-inflammatory properties that can help reduce airway inflammation and improve respiratory function. However, the balance of different prostaglandins is critical, as some can exacerbate respiratory conditions. Therapeutic strategies targeting prostaglandin pathways hold potential for managing respiratory diseases effectively.
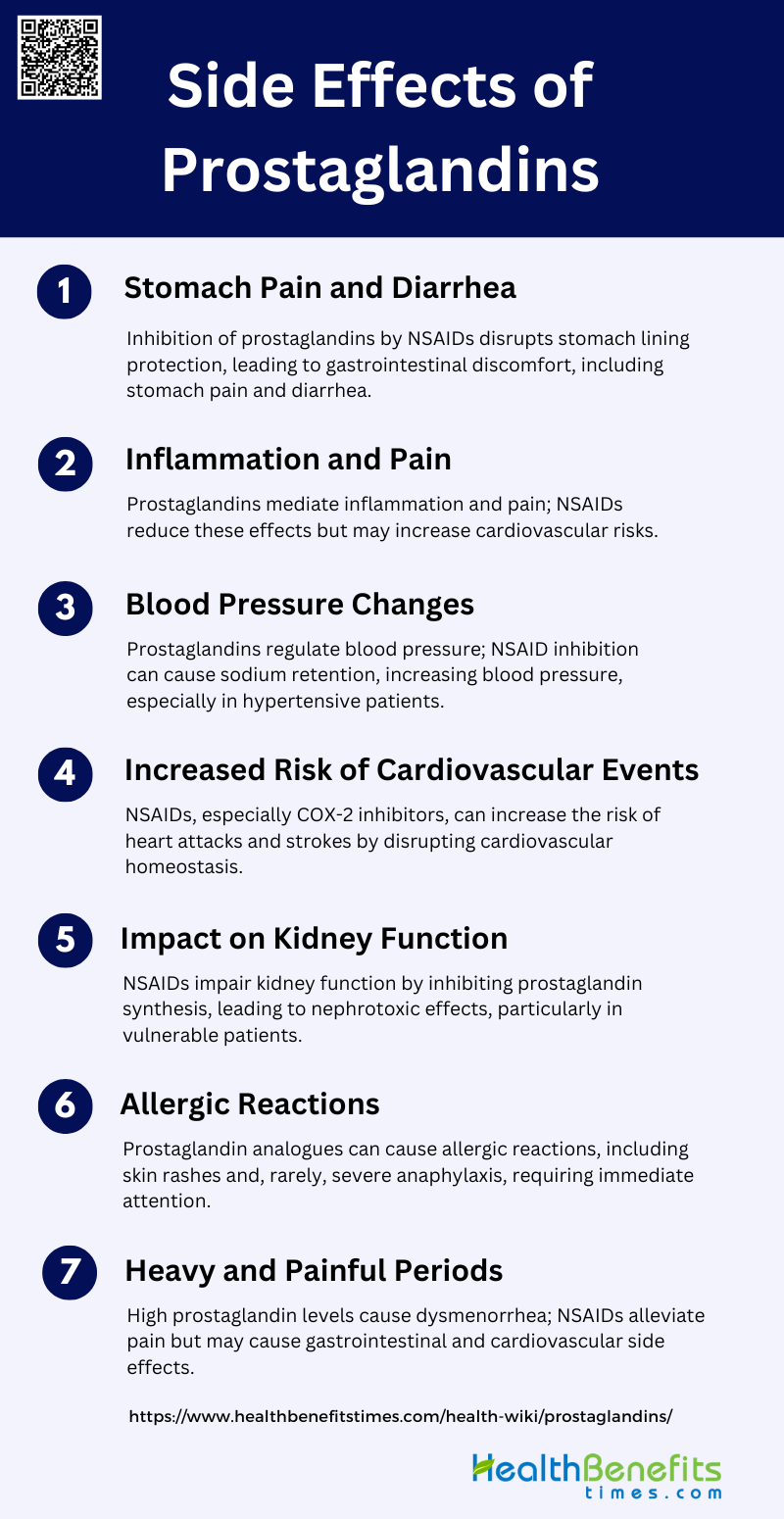
Side Effects of Prostaglandins
While prostaglandins are crucial for various bodily functions, their overproduction or dysregulation can lead to several adverse effects. These side effects can impact different systems in the body, causing discomfort and contributing to various medical conditions. Below are some of the common side effects of prostaglandins:
1. Stomach Pain and Diarrhea
Prostaglandins play a significant role in gastrointestinal physiology, and their inhibition can lead to adverse effects such as stomach pain and diarrhea. Nonsteroidal anti-inflammatory drugs (NSAIDs), which inhibit prostaglandin synthesis, are commonly associated with gastrointestinal side effects. This is because prostaglandins help protect the stomach lining by promoting mucus and bicarbonate secretion and maintaining blood flow. Inhibition of prostaglandin synthesis by NSAIDs can disrupt these protective mechanisms, leading to gastrointestinal discomfort, including stomach pain and diarrhea. The risk of these side effects is present with both non-selective NSAIDs and COX-2-specific inhibitors, although the latter may have a slightly reduced risk of gastrointestinal complications.
2. Inflammation and Pain
Prostaglandins are key mediators of inflammation and pain. They are produced at sites of tissue damage or infection, where they cause inflammation, pain, and fever as part of the healing process. NSAIDs alleviate pain and inflammation by inhibiting the cyclooxygenase (COX) enzymes, which are responsible for prostaglandin synthesis. However, this inhibition can also lead to side effects. For instance, while COX-2 inhibitors are designed to reduce inflammation and pain with fewer gastrointestinal side effects, they have been associated with increased cardiovascular risks. The role of prostaglandins in pain pathways is complex, involving various receptors and signaling mechanisms that contribute to the sensation of pain.
3. Blood Pressure Changes
Prostaglandins have a significant impact on blood pressure regulation. They can cause vasodilation, which lowers blood pressure, and influence the renin-angiotensin-aldosterone system, which regulates blood volume and systemic vascular resistance. Inhibition of prostaglandin synthesis by NSAIDs can lead to alterations in blood pressure. For example, NSAIDs can cause sodium and water retention, leading to increased blood pressure. This effect is particularly concerning in patients with pre-existing hypertension or cardiovascular conditions. Both traditional NSAIDs and COX-2 inhibitors have been shown to affect blood pressure, although the degree of impact may vary.
4. Increased Risk of Cardiovascular Events
The use of NSAIDs, particularly COX-2 inhibitors, has been linked to an increased risk of cardiovascular events such as heart attack and stroke. Prostaglandins play a role in maintaining cardiovascular homeostasis, including the regulation of platelet aggregation and vascular tone. Inhibition of COX-2 can disrupt this balance, leading to pro-thrombotic states and increased cardiovascular risk. Studies have shown that both traditional NSAIDs and COX-2 inhibitors carry some level of cardiovascular risk, although the mechanisms may differ. The cardiovascular safety of these drugs remains a critical consideration in their clinical use.
5. Impact on Kidney Function
Prostaglandins are crucial for maintaining renal blood flow and glomerular filtration rate, especially in conditions of reduced renal perfusion. NSAIDs can impair kidney function by inhibiting prostaglandin synthesis, leading to various nephrotoxic effects such as acute renal failure, fluid and electrolyte imbalances, and nephrotic syndrome. This risk is particularly high in patients with pre-existing renal conditions, heart failure, or those who are dehydrated. COX-2 inhibitors were initially thought to spare renal function, but emerging data suggest they also pose significant renal risks.
6. Allergic Reactions
Allergic reactions to prostaglandin analogues, although rare, can occur. These reactions may include skin rashes, itching, and in severe cases, anaphylaxis. The exact mechanism of these allergic responses is not well understood but is thought to involve immune system sensitization to the drug or its metabolites. Prostaglandin analogues used in ophthalmology, for instance, have been associated with local allergic reactions such as conjunctival hyperemia and periocular pigmentation. Systemic allergic reactions are less common but can be serious and require immediate medical attention.
7. Heavy and Painful Periods
Prostaglandins are involved in the regulation of menstrual cycles and uterine contractions. High levels of prostaglandins are associated with dysmenorrhea, which is characterized by heavy and painful menstrual periods. NSAIDs are commonly used to treat dysmenorrhea by reducing prostaglandin levels, thereby alleviating pain and reducing menstrual flow. However, the use of NSAIDs can also lead to side effects such as gastrointestinal discomfort and increased cardiovascular risk. The balance between therapeutic benefits and potential side effects must be carefully managed in the treatment of dysmenorrhea.
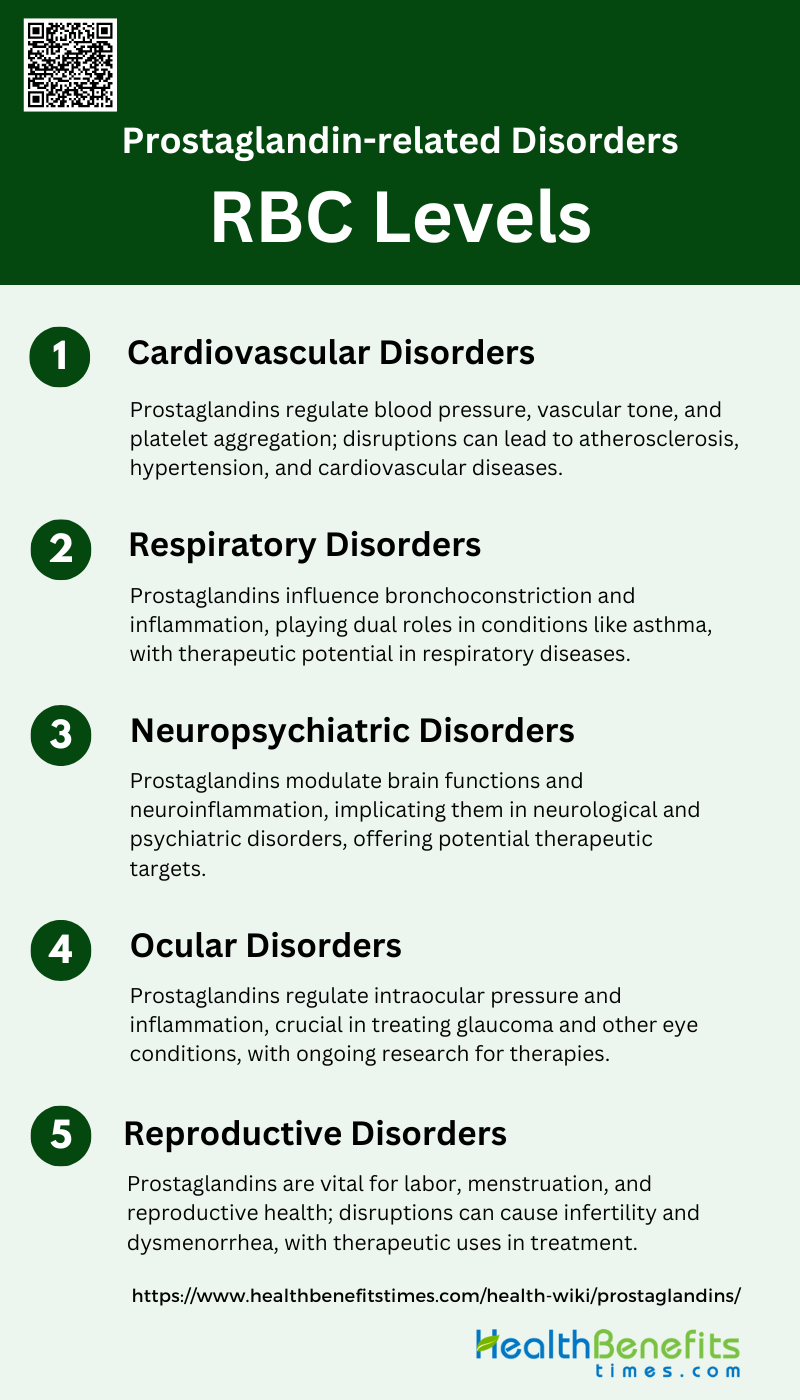
Prostaglandin-related Disorders
Prostaglandins, while essential for normal bodily functions, can be implicated in various disorders when their production or regulation is disrupted. These disorders can affect multiple systems, leading to a range of symptoms and health issues. Below are some common prostaglandin-related disorders:
1. Cardiovascular Disorders
Prostaglandins play a significant role in cardiovascular health and disease. They are involved in the regulation of blood pressure, vascular tone, and platelet aggregation. Prostaglandin F2α (FP) receptor, for instance, has been implicated in blood pressure regulation and atherosclerosis, highlighting its potential as a therapeutic target for cardiovascular diseases. Additionally, unstable metabolites of arachidonic acid, such as prostacyclin, are crucial in maintaining vascular homeostasis and preventing hypertension by modulating vascular smooth muscle tension. The complex interplay of prostaglandins in cardiovascular systems underscores their importance in both normal physiology and pathological conditions.
2. Respiratory Disorders
Prostaglandins are also critical in the respiratory system, influencing bronchoconstriction and inflammation. They have been implicated in various respiratory disorders, including asthma and bronchoconstrictive diseases. Prostaglandins can act as both pro-inflammatory and anti-inflammatory agents, depending on the context, which adds to the complexity of their role in respiratory healt. Their modulation of immune responses and inflammation makes them potential targets for therapeutic interventions in respiratory conditions. Understanding the dual roles of prostaglandins in respiratory disorders is essential for developing effective treatments.
3. Neuropsychiatric Disorders
In the realm of neuropsychiatric disorders, prostaglandins have been shown to modulate various brain functions and pathologies. Type 2 prostaglandins, produced by COX-2, are particularly implicated in the progression of neurological and psychiatric conditions. These compounds can influence neuroinflammation, which is a common feature in many brain disorders. The suppression of prostaglandin production has been suggested as a potential therapeutic strategy to alleviate symptoms of neuropsychiatric diseases. Further research is needed to fully understand the mechanisms by which prostaglandins affect brain health and to develop targeted treatments.
4. Ocular Disorders
Prostaglandins are also involved in ocular health, particularly in the regulation of intraocular pressure and inflammation. They are used therapeutically in the treatment of glaucoma, where they help to reduce intraocular pressure by increasing the outflow of aqueous humor. The role of prostaglandins in ocular inflammation and their potential therapeutic applications in other eye diseases are areas of ongoing research. Understanding the specific actions of different prostaglandins in the eye can lead to more effective treatments for various ocular disorders.
5. Reproductive Disorders
In the reproductive system, prostaglandins are essential for processes such as luteolysis, parturition, and the menstrual cycle. Prostaglandin F2α (FP) receptor is crucial for female reproductive functions, including the regulation of labor and menstrual pain. Alterations in prostaglandin production or metabolism can lead to reproductive disorders such as infertility and dysmenorrhea. Therapeutically, prostaglandins have been used to induce labor and manage other reproductive health issues, demonstrating their significant role in reproductive physiology and pathology. Further research into prostaglandin pathways could provide new insights into treating reproductive disorders.