 Primary Aldosteronism (PA) is a condition characterized by the excessive production of aldosterone, a hormone produced by the adrenal glands that regulates sodium and potassium levels in the blood. This overproduction leads to secondary hypertension, which is often resistant to conventional treatments. PA is commonly caused by either unilateral adrenal adenoma or bilateral adrenal hyperplasia. The condition can result in significant complications, including hypokalemia (low potassium levels), cardiovascular issues, and renal damage. Diagnosis typically involves screening tests such as the aldosterone-to-renin ratio, confirmatory tests, and imaging studies, with adrenal vein sampling being crucial for distinguishing between unilateral and bilateral disease. Treatment options include surgical removal of the affected adrenal gland or medical management with mineralocorticoid receptor antagonists.
Primary Aldosteronism (PA) is a condition characterized by the excessive production of aldosterone, a hormone produced by the adrenal glands that regulates sodium and potassium levels in the blood. This overproduction leads to secondary hypertension, which is often resistant to conventional treatments. PA is commonly caused by either unilateral adrenal adenoma or bilateral adrenal hyperplasia. The condition can result in significant complications, including hypokalemia (low potassium levels), cardiovascular issues, and renal damage. Diagnosis typically involves screening tests such as the aldosterone-to-renin ratio, confirmatory tests, and imaging studies, with adrenal vein sampling being crucial for distinguishing between unilateral and bilateral disease. Treatment options include surgical removal of the affected adrenal gland or medical management with mineralocorticoid receptor antagonists.
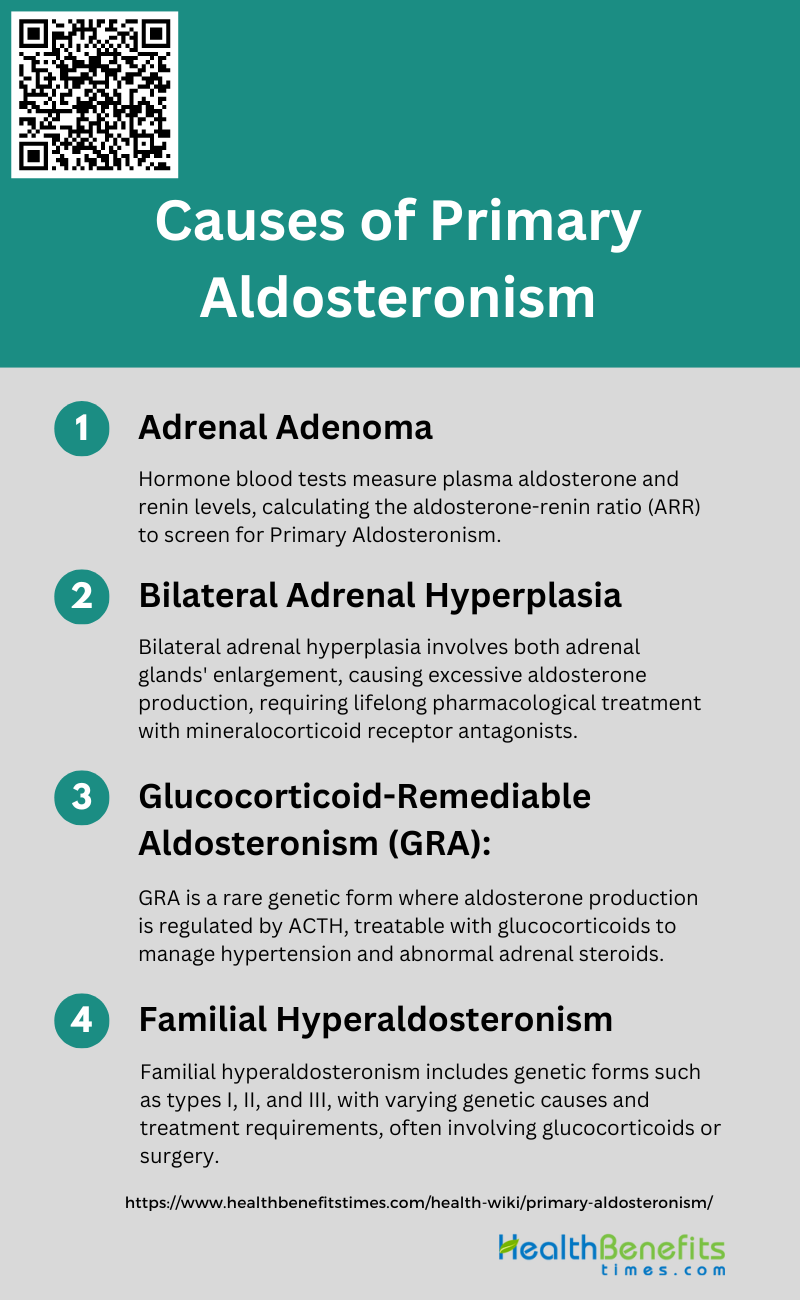
Causes of Primary Aldosteronism
Primary aldosteronism, also known as Conn’s syndrome, is a condition characterized by excessive production of the hormone aldosterone from the adrenal glands. This overproduction can stem from various underlying factors that disrupt the normal regulation of aldosterone. Below is a list of the most common causes of primary aldosteronism.
1. Adrenal Adenoma
Adrenal adenoma, also known as aldosterone-producing adenoma (APA), is one of the primary causes of primary aldosteronism (PA). APAs are benign tumors of the adrenal gland that autonomously produce aldosterone, leading to hypertension and hypokalemia. Genetic studies have identified several somatic mutations in genes such as KCNJ5, ATP1A1, ATP2B3, and CACNA1D, which are implicated in the pathogenesis of APAs. These mutations result in increased aldosterone production and cell proliferation by altering ion channel function and calcium signaling pathways. Surgical removal of the adenoma often results in the resolution of hypertension and normalization of aldosterone levels.
2. Bilateral Adrenal Hyperplasia
Bilateral adrenal hyperplasia (BAH), also known as idiopathic hyperaldosteronism, is another major cause of PA. BAH is characterized by the diffuse enlargement of both adrenal glands, leading to excessive aldosterone production. Unlike APAs, the genetic basis of BAH is less well understood, although it is known to be a sporadic condition. Patients with BAH typically require lifelong pharmacological treatment with mineralocorticoid receptor antagonists to manage their condition. BAH is more prevalent than APA and accounts for a significant proportion of PA cases, especially in patients with resistant hypertension.
3. Familial Hyperaldosteronism
Familial hyperaldosteronism (FH) encompasses several genetic forms of PA, including FH types I, II, and III. FH type I, also known as glucocorticoid-remediable aldosteronism (GRA), is caused by a chimeric gene resulting from unequal crossing-over between CYP11B1 and CYP11B2. This condition is characterized by aldosterone production that is suppressible by glucocorticoids . FH type II is inherited in an autosomal dominant manner and is associated with both APAs and BAH, although the specific genetic mutations are not well defined. FH type III is caused by mutations in the KCNJ5 gene and often requires early bilateral adrenalectomy due to severe hyperaldosteronism .
4. Glucocorticoid-Remediable Aldosteronism (GRA)
Glucocorticoid-remediable aldosteronism (GRA) is a rare form of familial hyperaldosteronism caused by a chimeric gene that fuses the regulatory region of CYP11B1 with the coding region of CYP11B2. This genetic alteration leads to aldosterone production being regulated by adrenocorticotropic hormone (ACTH) instead of the renin-angiotensin system. As a result, aldosterone levels can be suppressed by glucocorticoid treatment, which reduces ACTH levels. GRA is characterized by hypertension, variable hyperaldosteronism, and elevated levels of abnormal adrenal steroids such as 18-oxocortisol and 18-hydroxycortisol. Early diagnosis and treatment with glucocorticoids can effectively manage the condition and prevent complications.
Sign and Symptoms of Primary Aldosteronism
The hormonal imbalance can lead to a distinctive set of signs and symptoms that, if recognized early, can be managed effectively. Below is a list of the common clinical manifestations associated with primary aldosteronism.
1. Hypertension: Elevated blood pressure that is often resistant to conventional treatment.
2. Hypokalemia: Low potassium levels in the blood, which may cause muscle weakness, cramping, and fatigue.
3. Hypernatremia: Elevated sodium levels in the blood.
4. Metabolic Alkalosis: Increased blood pH due to loss of hydrogen ions or an excess of bicarbonate.
5. Polyuria: Increased urine output.
6. Polydipsia: Increased thirst.
7. Headaches: Often due to high blood pressure.
8. Nocturia: Frequent urination at night.
9. Tingling or Numbness: Especially in the limbs, due to low potassium levels.
10. Cardiac Arrhythmias: Irregular heartbeats, which can be caused by low potassium levels.
11. Muscle Weakness: General muscle weakness or muscle cramps due to hypokalemia.
12. Fatigue: General feeling of tiredness or lack of energy.
13. Visual Disturbances: In severe cases, due to prolonged hypertension.
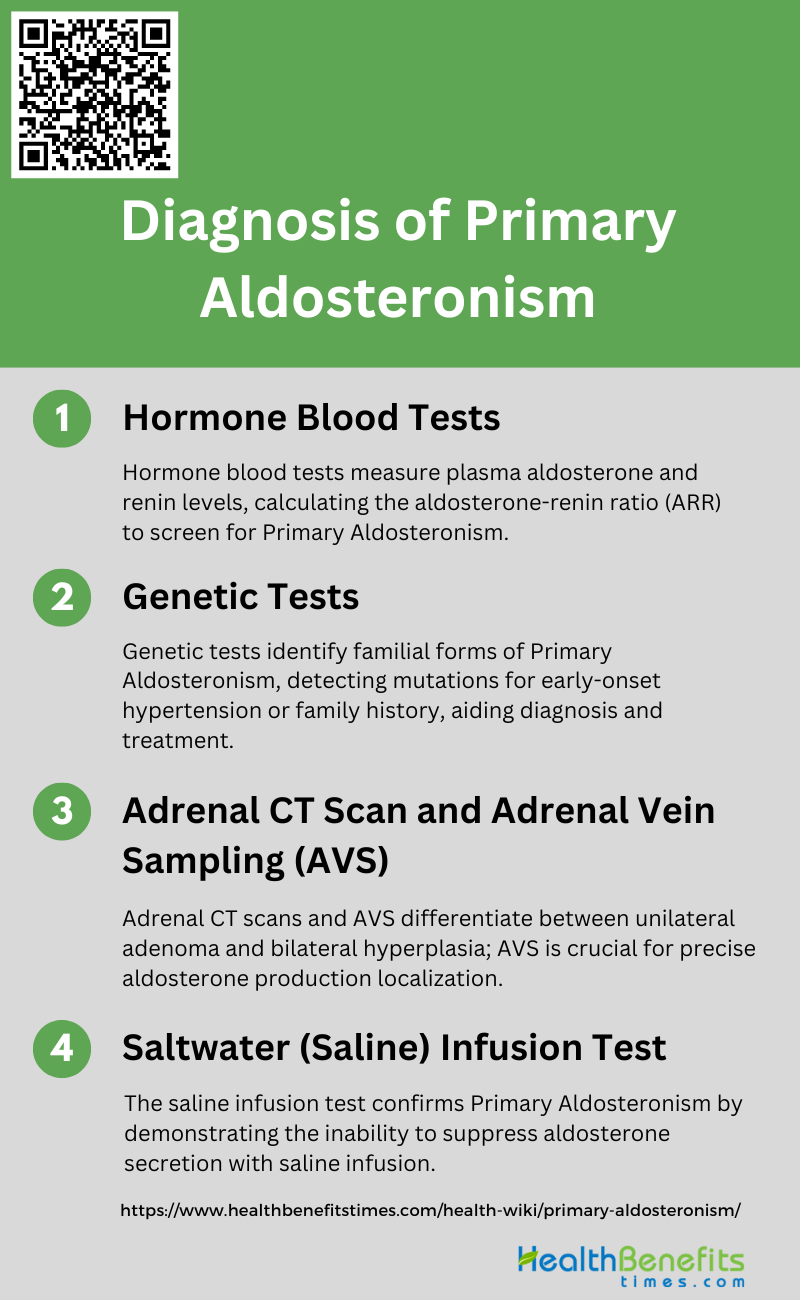
Diagnosis of Primary Aldosteronism
The diagnosis of Primary Aldosteronism is a critical step in managing patients with hypertension and involves a series of tests to confirm excess production of aldosterone. It is essential to accurately identify this condition as it can lead to targeted treatments that significantly improve outcomes. Following are the key steps in the diagnostic process:
1. Hormone Blood Tests
Hormone blood tests are essential in the initial diagnosis of primary aldosteronism (PA). These tests typically measure plasma aldosterone concentration (PAC) and plasma renin activity (PRA), and the aldosterone-renin ratio (ARR) is calculated. A high ARR is indicative of PA and warrants further confirmatory testing. The ARR is a widely recommended screening tool due to its high sensitivity and specificity in detecting PA. Additionally, confirmatory tests such as the saline infusion test or the captopril challenge test are often employed to validate the diagnosis by demonstrating autonomous aldosterone secretion.
2. Adrenal CT Scan and Adrenal Vein Sampling (AVS)
Adrenal CT scans and adrenal vein sampling (AVS) are critical in differentiating between unilateral aldosterone-producing adenoma (APA) and bilateral adrenal hyperplasia (BAH) in PA patients. CT scans are non-invasive and can identify adrenal nodules, but they lack the sensitivity and specificity required for definitive diagnosis. AVS, on the other hand, is considered the gold standard for subtype diagnosis, as it directly measures aldosterone levels from both adrenal veins, providing precise lateralization of aldosterone production . Despite its invasiveness and technical challenges, AVS is crucial for determining the appropriate treatment strategy, such as adrenalectomy for APA or medical management for BAH.
3. Genetic Tests
Genetic tests play a supplementary role in the diagnosis of primary aldosteronism, particularly in identifying familial forms of the disease. Genetic testing is recommended for patients with early-onset hypertension or a family history of PA, as it can detect mutations associated with familial hyperaldosteronism types I, II, and III. For instance, glucocorticoid-remediable aldosteronism (GRA) can be identified through genetic testing, which involves screening for the chimeric gene responsible for this condition. Identifying genetic mutations not only aids in diagnosis but also informs treatment strategies and genetic counseling for affected families.
4. Saltwater (Saline) Infusion Test
The saline infusion test is a confirmatory test used to validate the diagnosis of primary aldosteronism by demonstrating the inability to suppress aldosterone secretion. During the test, saline is infused intravenously, and PAC is measured before and after the infusion. A post-infusion PAC above a certain threshold confirms PA. This test is particularly useful in distinguishing PA from other forms of hypertension, as patients with PA will not show the expected suppression of aldosterone levels. The saline infusion test is a reliable and widely used method for confirming autonomous aldosterone production in suspected PA cases.
Complications of primary aldosteronism
Primary aldosteronism, a condition characterized by excessive production of the hormone aldosterone, can lead to a range of serious health complications if left untreated. These complications stem from the hormone’s impact on blood pressure and electrolyte balance, often resulting in chronic conditions that affect various organ systems. Below is a list of the potential complications associated with primary aldosteronism:
1. Hypertension: Persistent high blood pressure due to excessive aldosterone.
2. Hypokalemia: Low potassium levels, leading to muscle weakness, cramps, and fatigue.
3. Metabolic Alkalosis: Elevated blood pH due to increased bicarbonate reabsorption.
4. Cardiovascular Issues: Increased risk of heart disease, heart attacks, and strokes.
5. Renal Damage: Potential for chronic kidney disease and reduced kidney function.
6. Glucose Intolerance: Higher likelihood of developing diabetes or impaired glucose tolerance.
7. Bone Health: Risk of osteoporosis due to calcium imbalance.
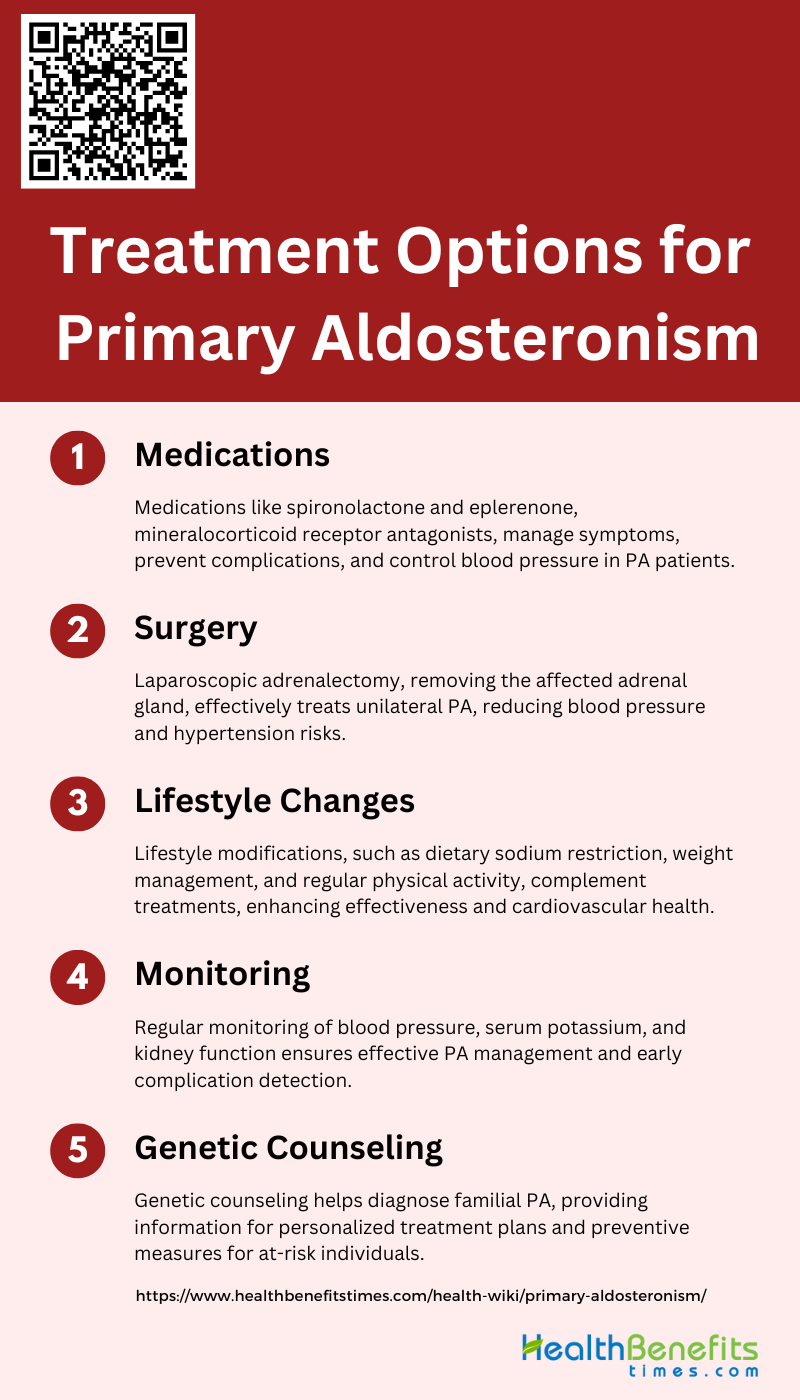
Treatment Options for Primary Aldosteronism
Primary Aldosteronism, a condition characterized by excess production of the hormone aldosterone, can lead to serious health complications if left untreated. Fortunately, there are several effective treatment options available to manage this condition. Below is a list of the most commonly recommended treatments for Primary Aldosteronism, each tailored to individual patient needs and circumstances.
1. Medications
Medications for primary aldosteronism (PA) primarily involve the use of mineralocorticoid receptor antagonists (MRAs) such as spironolactone and eplerenone. Spironolactone is more potent but can have adverse effects, particularly in men, due to its hormonal side effects. Eplerenone is often used as an alternative with fewer side effects. In cases where MRAs are insufficient, additional medications like epithelial sodium channel blockers (e.g., amiloride), thiazide diuretics, and calcium channel blockers may be employed to control blood pressure. These medications help manage the symptoms and prevent complications associated with PA, such as hypertension and hypokalemia.
2. Surgery
Surgical treatment for PA typically involves laparoscopic adrenalectomy, which is the removal of the adrenal gland producing excess aldosterone. This procedure is particularly effective for patients with unilateral PA, where one adrenal gland is affected. Surgery can significantly reduce blood pressure and, in many cases, cure hypertension. It also mitigates the risk of chronic kidney disease and other cardiovascular complications associated with PA. Studies have shown that surgical outcomes are comparable to medical treatments in terms of blood pressure control and reduction of left ventricular mass, although the benefits of surgery are often observed sooner.
3. Lifestyle Changes
Lifestyle modifications are an essential component of managing PA. Dietary sodium restriction is crucial because the harmful effects of hyperaldosteronism are exacerbated by high salt intake. Reducing sodium intake can help control blood pressure and reduce the need for medications. Additionally, maintaining a healthy weight, engaging in regular physical activity, and avoiding excessive alcohol consumption can further aid in managing hypertension and improving overall cardiovascular health. These lifestyle changes complement medical and surgical treatments, enhancing their effectiveness and helping to prevent long-term complications.
4. Monitoring
Regular monitoring is vital for patients with PA to ensure effective management and to detect any complications early. This includes frequent blood pressure measurements, serum potassium level checks, and kidney function tests. Monitoring helps in adjusting medication dosages and assessing the effectiveness of treatment. For patients who undergo surgery, follow-up imaging and hormonal assessments are necessary to confirm the success of the procedure and to check for any recurrence of the disease. Continuous monitoring is essential to prevent the progression of cardiovascular and renal complications associated with PA.
5. Genetic Counseling
Genetic counseling is recommended for patients with familial forms of PA or those with identified genetic mutations. Understanding the genetic basis of PA can help in early diagnosis and targeted treatment, potentially improving outcomes. Genetic counseling provides patients and their families with information about the hereditary nature of the condition, the risks of transmission to offspring, and the implications for other family members. This approach can guide personalized treatment plans and inform decisions about screening and preventive measures for at-risk individuals.
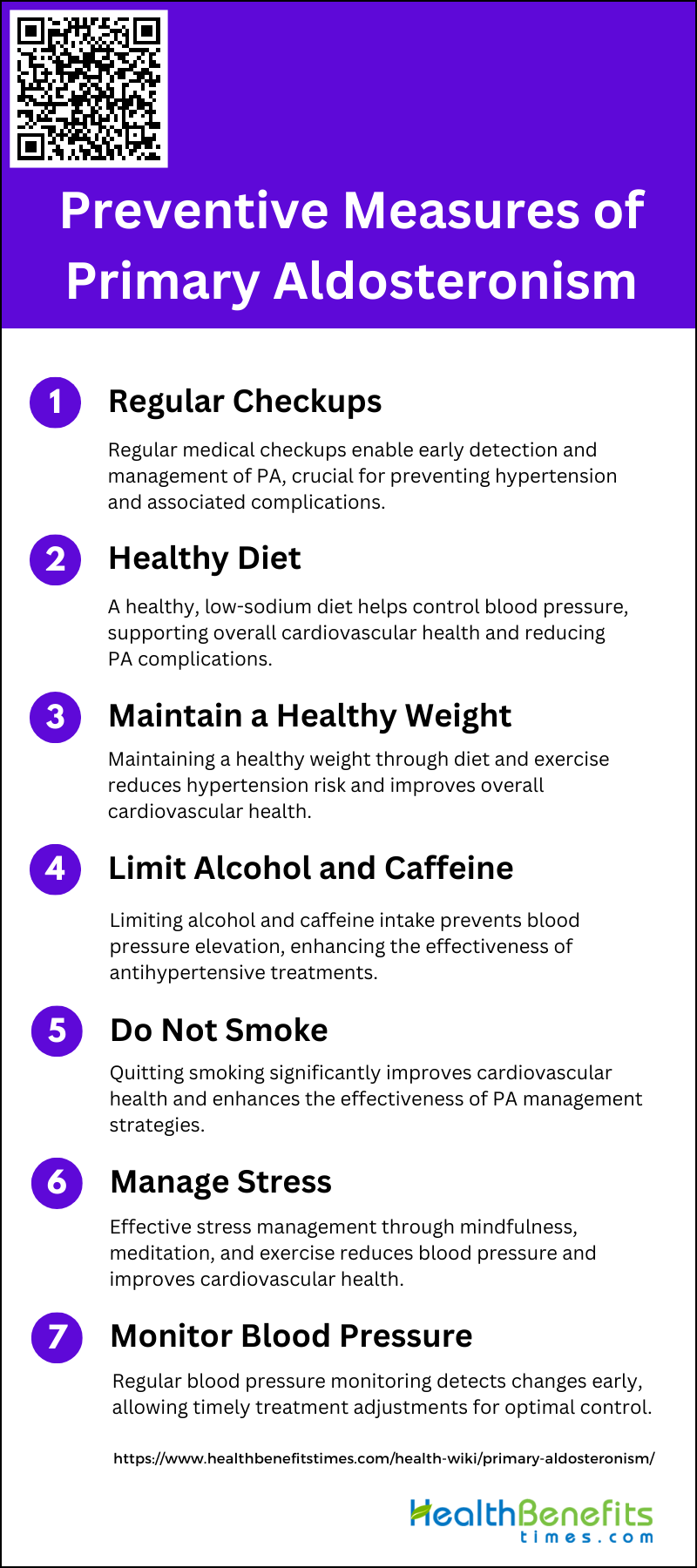
Preventive measures of Primary Aldosteronism
To mitigate the risks associated with this disorder, it is crucial to adopt a proactive approach to prevention. Below is a list of measures that can be taken to prevent the onset or progression of Primary Aldosteronism.
1. Regular Checkups
Regular medical checkups are crucial for the early detection and management of primary aldosteronism (PA). Screening for PA is particularly recommended for hypertensive patients and those with hypokalemia, as these groups are at higher risk. Early detection through regular checkups allows for timely intervention, which can prevent the progression of hypertension and associated complications such as cardiovascular and kidney diseases. Regular monitoring of blood pressure and serum potassium levels, along with the aldosterone-renin ratio, can help in the early identification and management of PA.
2. Healthy Diet
A healthy diet plays a significant role in managing primary aldosteronism. Dietary sodium restriction is particularly important, as the deleterious effects of hyperaldosteronism are dependent on salt loading. Reducing sodium intake can help control blood pressure and reduce the risk of cardiovascular complications. Additionally, a diet rich in fruits, vegetables, and whole grains can support overall cardiovascular health and help maintain a healthy weight, which is beneficial for managing PA.
3. Maintain a Healthy Weight
Maintaining a healthy weight is essential for preventing and managing primary aldosteronism. Obesity is a known risk factor for hypertension, which can exacerbate the effects of PA. Weight management through a balanced diet and regular physical activity can help reduce blood pressure and improve overall cardiovascular health. Studies have shown that weight loss can lead to significant improvements in blood pressure control and reduce the need for antihypertensive medications.
4. Limit Alcohol and Caffeine
Limiting the intake of alcohol and caffeine is recommended for individuals with primary aldosteronism. Both substances can elevate blood pressure and counteract the effects of antihypertensive treatments. Excessive alcohol consumption is associated with an increased risk of hypertension and cardiovascular diseases, while high caffeine intake can cause temporary spikes in blood pressure. Moderation in the consumption of these substances can help maintain stable blood pressure levels and improve the effectiveness of PA management strategies.
5. Do Not Smoke
Smoking cessation is a critical preventive measure for primary aldosteronism. Smoking is a major risk factor for cardiovascular diseases and can exacerbate hypertension, making the management of PA more challenging. Quitting smoking can lead to significant improvements in cardiovascular health and reduce the risk of complications associated with PA. Additionally, smoking cessation can enhance the effectiveness of antihypertensive treatments and improve overall health outcomes.
6. Manage Stress
Effective stress management is important for individuals with primary aldosteronism. Chronic stress can lead to elevated blood pressure and worsen the symptoms of PA. Techniques such as mindfulness, meditation, and regular physical activity can help reduce stress levels and improve cardiovascular health. Managing stress can also enhance the effectiveness of medical treatments and support overall well-being. Incorporating stress-reducing activities into daily routines can be a valuable component of a comprehensive PA management plan.
7. Monitor Blood Pressure
Regular monitoring of blood pressure is essential for individuals with primary aldosteronism. Consistent blood pressure checks can help detect any changes early and allow for timely adjustments in treatment plans. Home blood pressure monitoring can be particularly useful for tracking daily fluctuations and ensuring that blood pressure remains within a healthy range. Monitoring blood pressure regularly can also help assess the effectiveness of treatments and make necessary modifications to achieve optimal control.