Pollen allergy, also known as hay fever or allergic rhinitis, is a common allergic reaction to pollen grains released by plants. These tiny particles are one of the primary causes of allergic rhinitis and asthma, affecting millions worldwide. The prevalence of pollen allergies varies depending on factors such as climate, geographical location, and the types of flora present in an area. Symptoms typically include sneezing, runny or congested nose, itchy eyes, and sometimes asthma. Climate change has been shown to exacerbate pollen allergies by increasing the potency and duration of pollen seasons, as well as contributing to phenomena like thunderstorm asthma, which can trigger severe asthma attacks in sensitized individuals. Diagnosis often involves identifying specific allergens through immunoglobulin E (IgE) testing, and treatment options include avoiding exposure, using anti-allergic medications, and allergen immunotherapy, which is the only treatment that modifies the course of the allergy.
Causes of Pollen Allergy
Pollen allergy, also known as hay fever, is triggered by the immune system’s response to pollen grains from plants. Various factors contribute to the onset and severity of this condition. Below are the primary causes of pollen allergy:
1. Pollen Grains
Pollen grains are a primary cause of allergic reactions, particularly respiratory allergies such as hay fever and asthma. These grains contain proteins or glycoproteins that act as allergens, triggering immune responses in sensitized individuals. Pollen allergens are typically water-soluble and can withstand various environmental conditions, including changes in pH and temperature. The allergenic proteins in pollen grains can vary in their potency, and their presence in the air is influenced by factors such as plant species, climate, and environmental pollution. The interaction between pollen grains and air pollutants can further enhance their allergenicity, making them more likely to cause allergic reactions.
2. Immune Response
The immune response to pollen allergens involves a complex interaction between the body’s defense mechanisms and environmental factors. When pollen allergens enter the body, they can trigger the production of specific IgE antibodies, leading to hypersensitivity reactions. This immune response is characterized by the release of immunomodulatory and pro-inflammatory mediators, which can exacerbate symptoms in predisposed individuals. The allergic response is a result of the immune system’s disturbed reaction to otherwise harmless environmental agents, leading to symptoms such as rhinitis, conjunctivitis, and asthma. The severity of the immune response can be influenced by genetic predisposition and environmental factors, including air pollution and climate change.
3. Genetic Predisposition
Genetic predisposition plays a significant role in the development of pollen allergies. Individuals with a family history of allergies are more likely to develop allergic reactions to pollen. Genetic factors can influence the immune system’s sensitivity to allergens and the production of specific IgE antibodies. However, while genetic control is important, environmental influences are crucial in determining the specific allergens to which a person will develop hypersensitivity. The interaction between genetic predisposition and environmental factors, such as air pollution and climate change, can further increase the risk of developing pollen allergies.
4. Climate Change and Air Pollution
Climate change and air pollution are significant contributors to the increasing prevalence of pollen allergies. Rising levels of CO2 and atmospheric temperatures can lead to higher pollen concentrations and increased allergenicity of pollen grains. Air pollutants, such as sulphur dioxide, ozone, and nitrogen oxides, can enhance the allergenic potential of pollen by modifying their proteins and increasing airway reactivity. Additionally, extreme weather events, such as thunderstorms, can exacerbate respiratory allergies by dispersing pollen and other allergens more widely. The combined effects of climate change and air pollution create a more challenging environment for individuals with pollen allergies.
5. Geographical and Environmental Factors
Geographical and environmental factors significantly impact the prevalence and severity of pollen allergies. Urbanization and industrialization have been linked to higher rates of pollen-induced respiratory allergies, as urban areas tend to have higher levels of air pollution and allergenic pollen. Environmental conditions, such as temperature, humidity, and wind patterns, can influence pollen counts and the distribution of allergens. Studies have shown that people living in urban areas are more affected by pollen allergies compared to those in rural areas, likely due to the higher concentration of pollutants and allergenic plants in cities. Understanding these geographical and environmental factors is essential for managing and mitigating the impact of pollen allergies on public health.
Symptoms of Pollen Allergy
Pollen allergy manifests through a variety of symptoms that can significantly impact daily life. These symptoms are triggered when the immune system overreacts to pollen grains in the air. Common symptoms include sneezing, runny or stuffy nose, itchy eyes, and throat irritation.
1. Respiratory Symptoms
Pollen allergies often manifest through various respiratory symptoms, including sneezing, runny nose, and nasal congestion. These symptoms are primarily due to the body’s immune response to inhaled pollen, which is recognized as a foreign substance. The immune system releases histamines and other chemicals, leading to inflammation and irritation of the nasal passages. This results in the classic symptoms of allergic rhinitis, such as sneezing and a runny or blocked nose. The severity of these symptoms can vary depending on the pollen concentration in the air and individual sensitivity. In some cases, these symptoms can be severe enough to interfere with daily activities and sleep, significantly impacting the quality of life.
2. Eye Symptoms
Eye symptoms are another common manifestation of pollen allergies, often referred to as allergic conjunctivitis. These symptoms include watery, itchy, and red eyes, which occur when pollen comes into contact with the conjunctiva, the membrane covering the white part of the eyes and the inner eyelids. The immune response to pollen in this area leads to the release of histamines, causing inflammation and irritation. These symptoms can be particularly bothersome, leading to discomfort and difficulty in performing daily tasks. In severe cases, the symptoms can also affect vision temporarily due to excessive tearing and swelling. Effective management often requires a combination of antihistamines and avoiding exposure to pollen.
3. Skin Symptoms
Although less common than respiratory and eye symptoms, pollen allergies can also cause skin reactions such as rashes and hives. These symptoms occur when pollen particles come into direct contact with the skin or through systemic allergic reactions. The skin’s immune response to pollen involves the release of histamines and other inflammatory mediators, leading to redness, itching, and the formation of hives or rashes. These skin symptoms can vary in severity from mild irritation to more extensive and painful rashes. Managing these symptoms typically involves the use of topical antihistamines or corticosteroids and minimizing skin exposure to pollen.
4. Severity and Variations
The severity and variations of pollen allergy symptoms can be influenced by several factors, including the type of pollen, geographic location, and individual sensitivity. Seasonal variations play a significant role, with symptoms often peaking during specific pollen seasons such as spring for tree pollen, summer for grass pollen, and fall for weed pollen. Climate change is also contributing to longer and more intense pollen seasons, potentially increasing the severity and duration of symptoms. Additionally, the presence of other allergens and pollutants can exacerbate symptoms, leading to more severe allergic reactions and complications such as asthma. Understanding these variations is crucial for effective management and treatment of pollen allergies.
Diagnosing of Pollen Allergy
Diagnosing pollen allergy involves a series of steps to accurately identify the allergens causing symptoms. This process typically includes a detailed medical history, physical examination, and various tests to confirm the diagnosis. Below are the key methods used in diagnosing pollen allergies:
1. Medical History and Physical Examination
Diagnosing pollen allergies begins with a thorough medical history and physical examination. This initial step involves gathering detailed information about the patient’s symptoms, their onset, duration, and any potential triggers. Physicians also inquire about family history of allergies, as genetic predisposition can play a significant role. Physical examination focuses on identifying signs of allergic reactions, such as nasal congestion, conjunctivitis, and skin rashes. This comprehensive approach helps in forming a preliminary diagnosis and guides further testing to confirm the presence of pollen allergies.
2. Skin Prick Tests
Skin prick tests (SPTs) are a cornerstone in the diagnosis of pollen allergies. This method involves introducing small amounts of allergen extracts into the skin, typically on the forearm or back, and observing the reaction. A positive test is indicated by the formation of a wheal and flare at the test site. SPTs are highly valued for their rapid results and ability to identify specific allergens causing the symptoms. Recent advancements, such as the Skin Prick Automated Test (SPAT), have improved the reliability and patient comfort during testing, reducing inconsistent results compared to manual methods.
3. Blood Tests
Blood tests, particularly those measuring specific immunoglobulin E (IgE) levels, are crucial for diagnosing pollen allergies. These tests, such as the ImmunoCAP ISAC and Allergy Explorer (ALEX2), detect the presence of IgE antibodies against specific pollen allergens in the patient’s blood. Molecular diagnostics, or component-resolved diagnostics (CRD), have enhanced the precision of these tests by identifying individual allergenic components, thus improving the management of pollen allergies. Blood tests are especially useful when skin tests are not feasible due to skin conditions or medication interference.
4. Home Testing Kits
Home testing kits for pollen allergies offer a convenient alternative for preliminary screening. These kits typically involve collecting a small blood sample via a finger prick and sending it to a laboratory for analysis. While they provide a level of accessibility and ease, the accuracy and comprehensiveness of home testing kits can vary. They are generally considered less reliable than clinical tests conducted under medical supervision. However, they can be a useful tool for initial assessment and may prompt individuals to seek further professional evaluation if results indicate potential allergies.
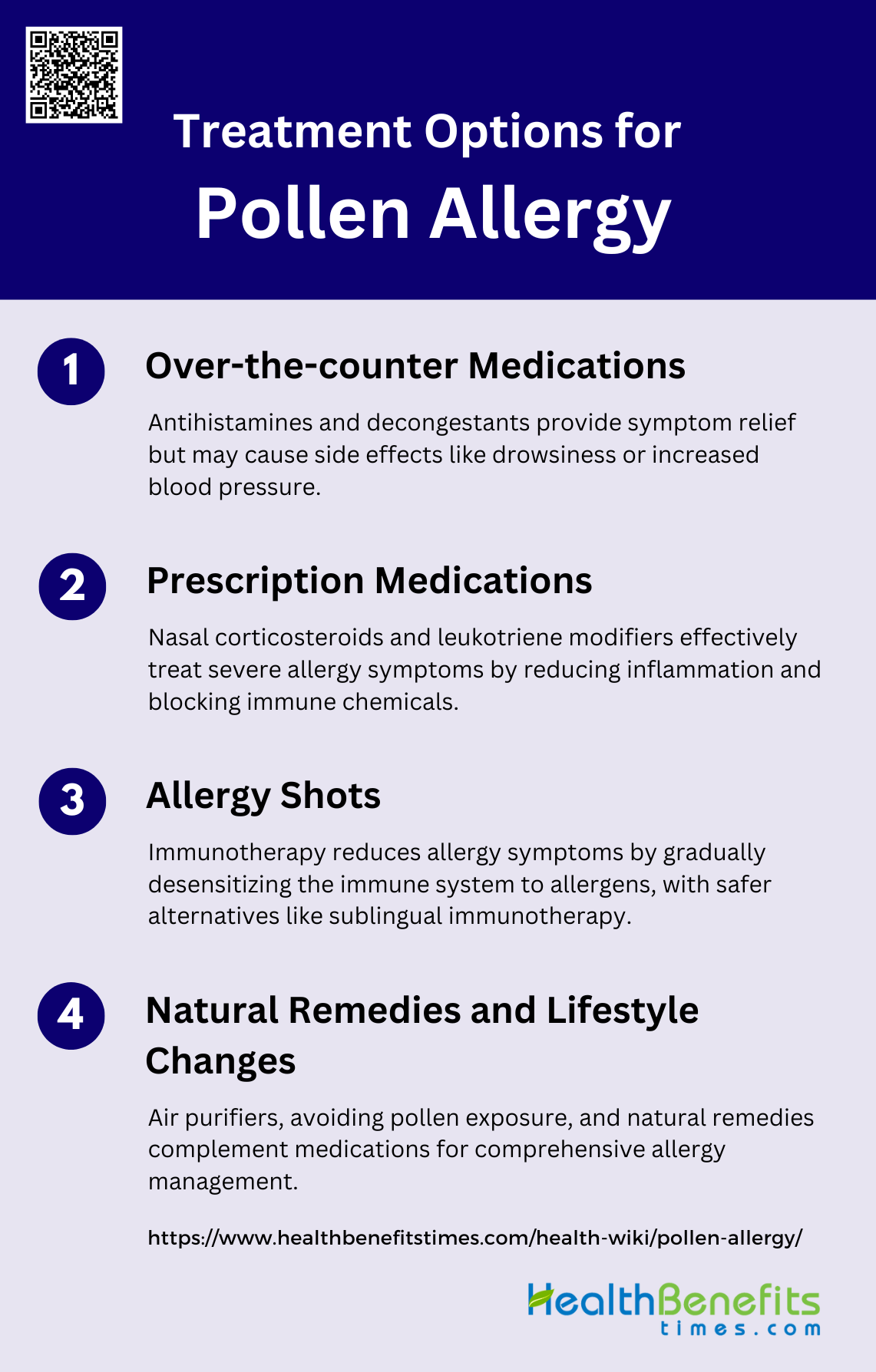
Treatment Options for Pollen Allergy
Treating pollen allergy involves a combination of strategies to manage symptoms and improve quality of life. These options range from medications to lifestyle changes and immunotherapy. Below are the key treatment options for pollen allergies:
1. Over-the-counter medications
Over-the-counter medications such as antihistamines and decongestants are commonly used to manage symptoms of pollen allergies. Antihistamines work by blocking histamine, a substance in the body that causes allergic symptoms. Decongestants help reduce nasal congestion by narrowing the blood vessels in the nasal passages. These medications are generally effective for mild to moderate symptoms and are easily accessible without a prescription. However, they may cause side effects such as drowsiness or increased blood pressure, and their effectiveness can vary from person to person.
2. Prescription medications
Prescription medications for pollen allergies include nasal corticosteroids and leukotriene modifiers. Nasal corticosteroids are highly effective in reducing inflammation and treating nasal symptoms such as congestion, sneezing, and runny nose. Leukotriene modifiers, such as montelukast, work by blocking leukotrienes, which are chemicals in the immune system that contribute to allergy symptoms. These medications are often recommended for more severe cases or when over-the-counter options are insufficient. Studies have shown that nasal corticosteroids have a significant impact on symptom relief, often comparable to other treatments like sublingual immunotherapy.
3. Allergy shots
Allergy shots, or immunotherapy, involve regular injections of small amounts of allergens to gradually desensitize the immune system. This treatment has been shown to significantly reduce symptoms and medication requirements in individuals with allergic rhinitis. However, the use of injection immunotherapy is limited by the potential for severe systemic reactions. Sublingual immunotherapy (SLIT) has emerged as a safer alternative, providing significant symptom relief and reducing medication needs without the risk of severe reactions. SLIT is particularly effective for pollen-induced seasonal allergic rhinitis and has a comparable impact to nasal corticosteroids.
4. Natural remedies and lifestyle changes
Natural remedies and lifestyle changes can also play a crucial role in managing pollen allergies. Using home air purifiers can help reduce indoor pollen levels, while strategies such as keeping windows closed during high pollen seasons, showering after outdoor activities, and using pollen masks can minimize exposure. These approaches are often used in conjunction with medications to provide comprehensive relief. While natural remedies may not be as immediately effective as pharmacological treatments, they are essential for long-term management and prevention of allergy symptoms.
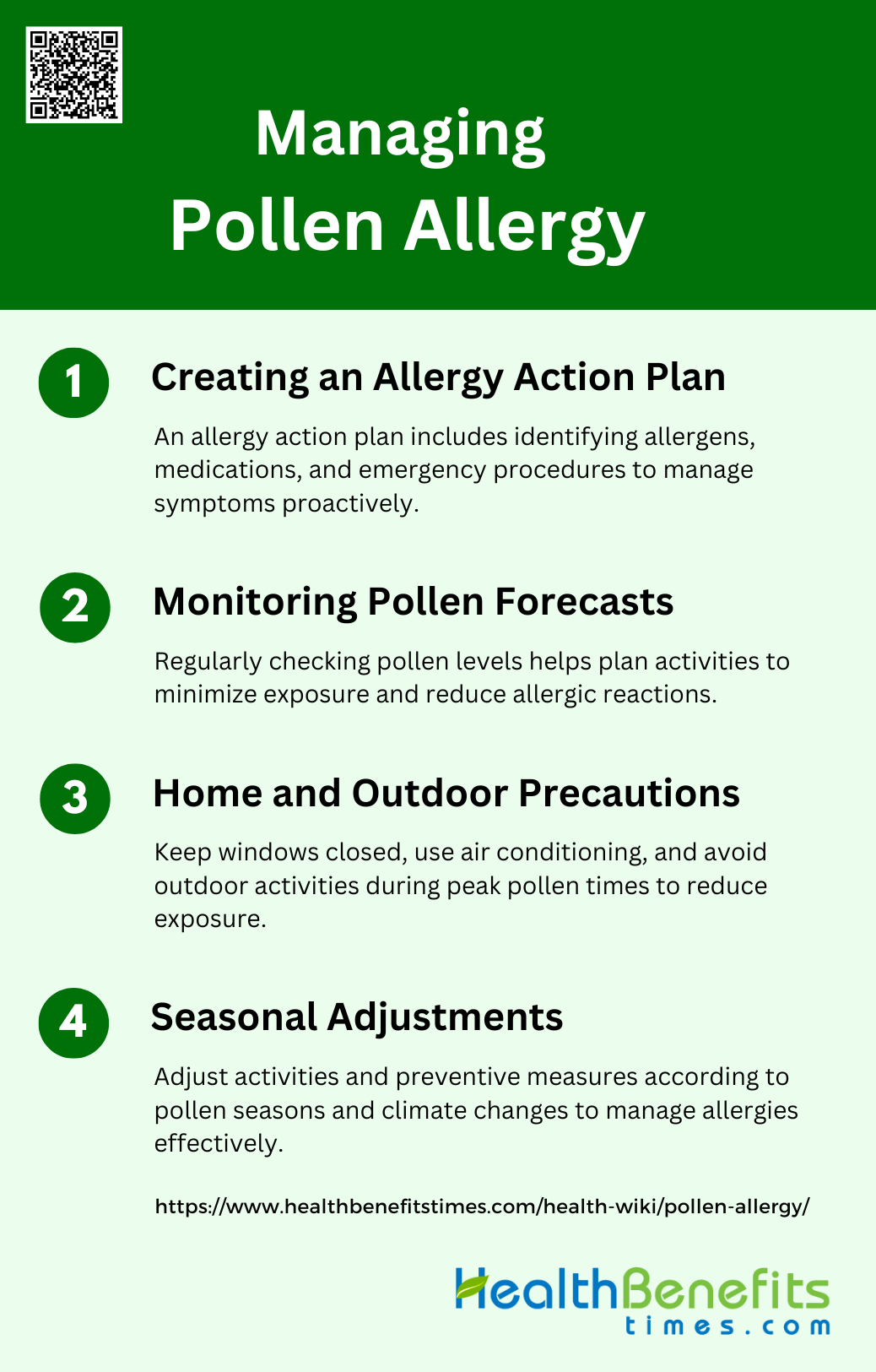
Managing Pollen Allergy
Managing pollen allergy requires a multifaceted approach to minimize exposure and alleviate symptoms. This includes both preventive measures and treatments to control allergic reactions. Below are the key strategies for managing pollen allergies:
1. Creating an Allergy Action Plan
Creating an allergy action plan is essential for managing pollen allergies effectively. This plan should include steps to identify and avoid allergens, medications to control symptoms, and emergency procedures for severe reactions. Regular consultations with healthcare providers can help tailor the plan to individual needs. For instance, medications should be taken at least 30 minutes before outdoor activities to prevent symptoms. Additionally, wearing a mask and taking a shower upon returning home can significantly reduce pollen exposure and alleviate symptoms. An action plan ensures that individuals are prepared and can manage their allergies proactively.
2. Monitoring Pollen Forecasts
Monitoring pollen forecasts is a crucial step in managing pollen allergies. Pollen levels can vary significantly based on weather conditions, and staying informed can help individuals take preventive measures. Websites like the National Allergy Bureau provide up-to-date pollen information for specific areas. Studies have shown that weather conditions, such as increased CO2 levels and higher temperatures, can raise pollen concentrations, making it essential to monitor these forecasts regularly. By staying informed, individuals can plan their activities to minimize exposure during high pollen periods, thereby reducing the risk of allergic reactions.
3. Home and Outdoor Precautions
Taking precautions both at home and outdoors can significantly reduce pollen exposure and alleviate allergy symptoms. Indoors, it is advisable to keep windows closed, especially on days with high pollen counts, and to use air conditioning with clean filters. Regular cleaning of windows, bookshelves, and air conditioning vents can also help reduce indoor pollen levels. Outdoors, minimizing activities during peak pollen times, usually between 10 am and 4 pm, and wearing a filter mask while gardening or mowing the lawn can be effective. These measures collectively help in managing pollen allergies more effectively.
4. Seasonal Adjustments
Seasonal adjustments are necessary to manage pollen allergies effectively, as pollen levels can vary with the seasons. During peak pollen seasons, individuals should limit outdoor activities and take preventive measures such as wearing masks and washing clothes and hair after being outside. The impact of climate change on pollen seasons, with longer growing seasons and higher pollen production, necessitates more vigilant monitoring and adjustments. Physicians have noted an increase in allergy symptoms attributed to these changes, making it crucial to adapt lifestyle and medical strategies accordingly. These adjustments help in reducing exposure and managing symptoms throughout the year.
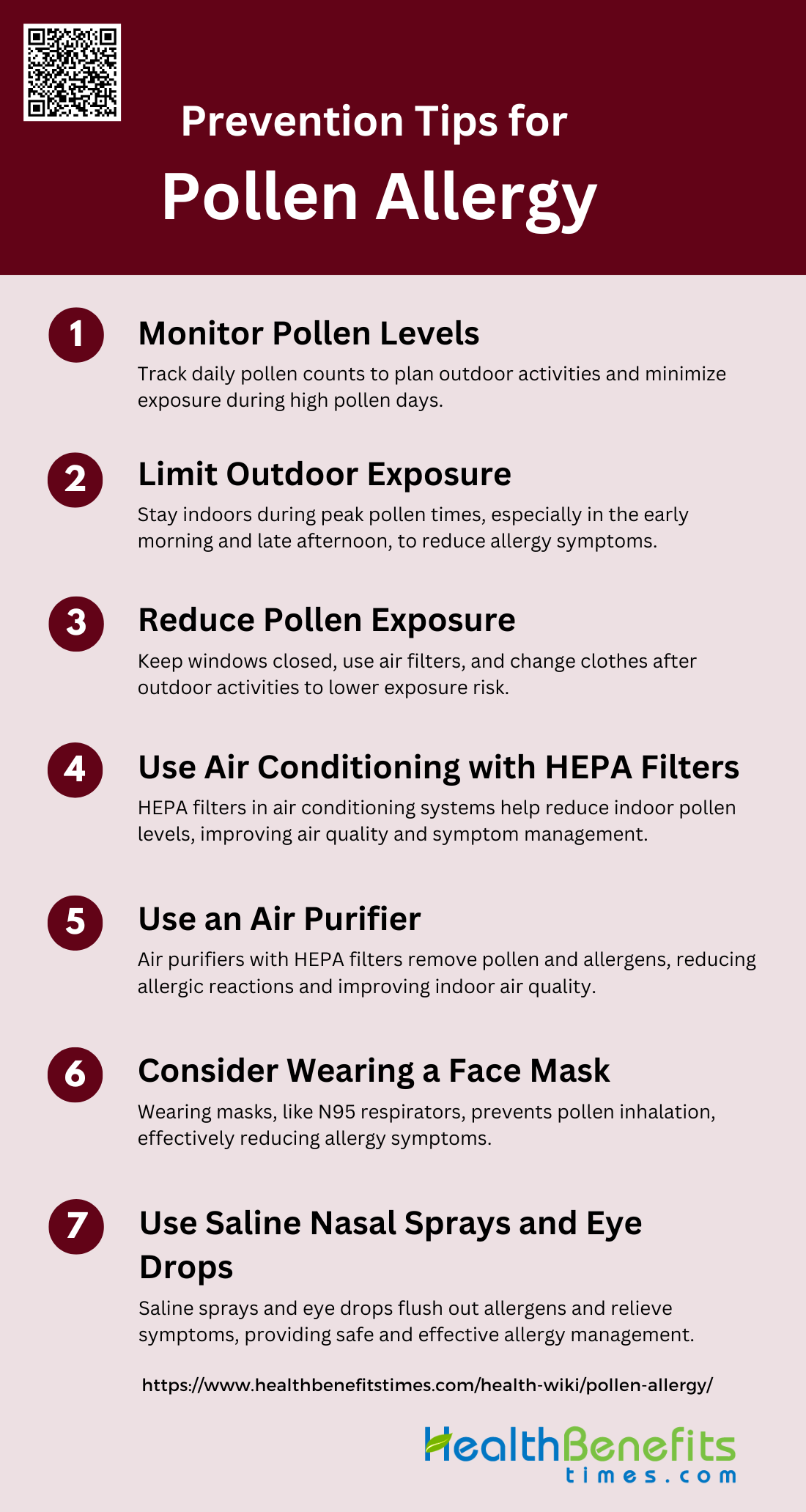
Prevention Tips for Pollen Allergy
Preventing pollen allergy involves proactive measures to reduce exposure and minimize symptoms. By incorporating these tips into your daily routine, you can better manage your allergy and improve your overall well-being. Below are the key prevention tips for pollen allergies:
1. Monitor Pollen Levels
Monitoring pollen levels is crucial for individuals with pollen allergies to manage their symptoms effectively. By keeping track of daily pollen counts, which are often available through weather reports or specialized apps, individuals can anticipate high pollen days and take preventive measures. Studies have shown that pollen concentrations can vary significantly based on location and time of day, with urban areas often experiencing higher levels in the morning. By staying informed about pollen levels, individuals can plan their outdoor activities accordingly, reducing their exposure and minimizing allergic reactions.
2. Limit Outdoor Exposure
Limiting outdoor exposure during peak pollen times is a highly recommended strategy for managing pollen allergies. Pollen levels are typically highest in the early morning and late afternoon, so staying indoors during these times can help reduce symptoms. Research indicates that avoiding outdoor activities during high pollen periods can significantly decrease the incidence of allergic reactions. Additionally, spending time in low-exposure environments, such as higher altitudes where pollen levels are lower, can also be beneficial. This approach helps minimize contact with allergens, thereby reducing the severity of symptoms.
3. Reduce Pollen Exposure
Reducing pollen exposure involves several practical steps that can help mitigate allergic reactions. Keeping windows and doors closed during high pollen seasons, using pollen screens, and regularly cleaning air filters in homes and cars are effective measures. Studies have shown that these practices can significantly lower indoor pollen levels, thereby reducing the overall exposure. Additionally, changing clothes and showering after spending time outdoors can remove pollen from the skin and hair, further decreasing the risk of allergic reactions. These combined efforts can create a more pollen-free environment, alleviating symptoms for allergy sufferers.
4. Use Air Conditioning with HEPA Filters
Using air conditioning with HEPA (High-Efficiency Particulate Air) filters is an effective way to reduce indoor pollen levels. HEPA filters are designed to trap tiny particles, including pollen, thereby improving indoor air quality. Research supports the use of HEPA filters in air conditioning systems to significantly lower the concentration of airborne allergens. This can be particularly beneficial during high pollen seasons when keeping windows closed and relying on filtered air can help maintain a pollen-free indoor environment. This approach not only reduces exposure but also helps in managing symptoms more effectively.
5. Use an Air Purifier
Air purifiers equipped with HEPA filters can be an excellent addition to the home environment for individuals with pollen allergies. These devices work by continuously filtering the air, removing pollen and other allergens. Studies have demonstrated that air purifiers can significantly reduce indoor allergen levels, leading to fewer allergic reactions. Placing air purifiers in commonly used rooms, such as bedrooms and living areas, can create a cleaner air environment, providing relief from symptoms. This non-pharmacological intervention is a practical step towards managing pollen allergies effectively.
6. Consider Wearing a Face Mask
Wearing a face mask can be an effective way to prevent pollen from entering the respiratory system, thereby reducing allergic reactions. Masks designed to filter out small particles, such as N95 respirators, can block a significant amount of pollen. Research has shown that nasal filters and face masks can substantially decrease the severity of allergic symptoms by preventing pollen inhalation. This preventive measure is particularly useful during outdoor activities or when pollen levels are high. By wearing a mask, individuals can protect themselves from direct exposure, leading to better management of their allergy symptoms.
7. Use Saline Nasal Sprays and Eye Drops
Saline nasal sprays and eye drops can provide immediate relief from pollen allergy symptoms by flushing out allergens and soothing irritated tissues. These non-pharmacological treatments are effective in reducing nasal congestion, itching, and eye discomfort. Studies have shown that saline solutions can help clear nasal passages and reduce the overall symptom burden. Additionally, using eye drops can alleviate symptoms like itchy and watery eyes, which are common during pollen seasons. These treatments are safe, easy to use, and can be an essential part of an allergy management plan.
FAQs
1. What types of plants produce the most allergenic pollen?
Different plants produce varying amounts and types of pollen that can trigger allergies. Common allergenic plants include trees like birch, oak, and cedar; grasses such as Timothy and Bermuda grass; and weeds like ragweed and sagebrush.
2. Can pollen allergies develop later in life?
Yes, it is possible for adults to develop pollen allergies even if they did not experience symptoms in childhood. Factors such as changes in environment, immune system, or prolonged exposure to allergens can contribute to the development of allergies later in life.
3. Are pollen allergies contagious?
No, pollen allergies are not contagious. They are an immune system response to pollen and are not transmitted from person to person.
4. Can diet or certain foods affect pollen allergies?
Some individuals with pollen allergies may experience cross-reactivity with certain foods, a condition known as oral allergy syndrome (OAS). For example, people allergic to birch pollen might react to apples, while those allergic to ragweed pollen might react to bananas or melons.
5. What is the difference between pollen allergy and other types of allergies (e.g., dust or pet allergies)?
Pollen allergy is specifically triggered by pollen grains from plants, whereas other types of allergies (such as dust mites, mold, or pet dander) are caused by different allergens. The symptoms may overlap, but the triggers are distinct, and treatments may vary based on the specific allergen.
6. Can pollen allergies cause complications if left untreated?
Yes, untreated pollen allergies can lead to complications such as sinus infections, worsening of asthma, and decreased quality of life due to chronic symptoms like nasal congestion, headaches, and sleep disturbances.
7. How do weather conditions impact pollen levels?
Weather conditions such as temperature, humidity, and wind can significantly affect pollen levels. Warm, dry, and windy days typically have higher pollen counts, while rain can temporarily reduce pollen in the air.
8. Can pets carry pollen indoors?
Yes, pets can carry pollen on their fur and bring it indoors, potentially triggering allergies in sensitive individuals. Regular grooming and cleaning of pets can help minimize this risk.
9. Are there any long-term health risks associated with frequent use of antihistamines or nasal sprays?
Long-term use of certain antihistamines can cause side effects such as drowsiness, dry mouth, or increased heart rate. Overuse of nasal decongestant sprays can lead to rebound congestion, where nasal passages become more congested once the spray’s effects wear off.
10. What is thunderstorm asthma, and how is it related to pollen allergies?
Thunderstorm asthma is a phenomenon where a combination of high pollen counts and storm conditions causes pollen grains to break into smaller particles, which can penetrate deeper into the airways. This can trigger severe asthma attacks in people with pollen allergies, particularly those with underlying asthma.