Plasma proteins are a diverse group of proteins found in blood plasma, the liquid component of blood. These proteins play crucial roles in various physiological processes, including maintaining blood volume, transporting hormones and nutrients, regulating pH balance, and supporting immune function. The most abundant plasma protein is albumin, which helps maintain osmotic pressure and serves as a carrier for many substances in the bloodstream. Other important plasma proteins include globulins (involved in immune responses), fibrinogen (essential for blood clotting), and various enzymes and regulatory proteins. Plasma proteins are synthesized primarily in the liver, although some are produced by other tissues or cells, such as antibodies produced by plasma cells. The composition and concentration of plasma proteins can change in response to various physiological and pathological conditions, making them valuable biomarkers for disease diagnosis and monitoring.
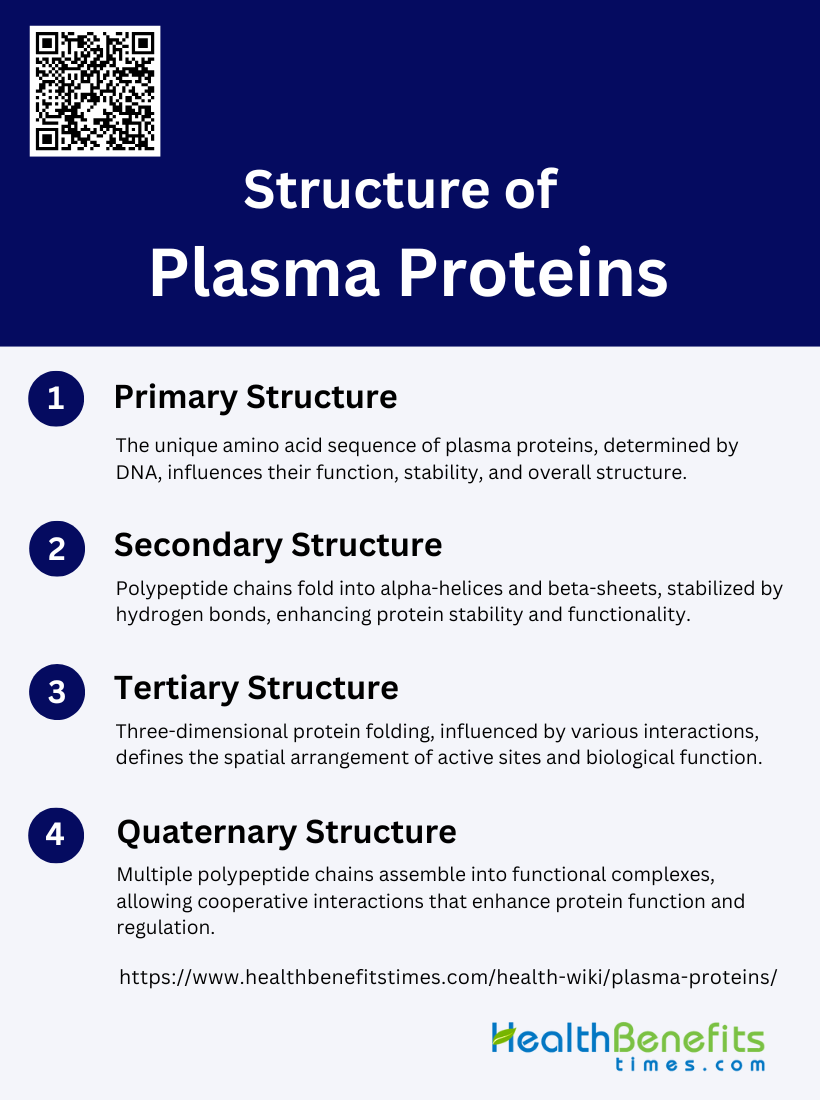
Structure of Plasma Proteins
The structure of plasma proteins is essential for their function and stability, organized into four hierarchical levels. These levels include the primary, secondary, tertiary, and quaternary structures, each contributing uniquely to the protein’s overall architecture. Below is a detailed explanation of each structural level:
1. Primary Structure
The primary structure of plasma proteins refers to the unique sequence of amino acids that are linked together by peptide bonds to form a polypeptide chain. This sequence is determined by the DNA sequence of the corresponding gene and is crucial for the proteins final structure and function. Each amino acid in the sequence has a specific side chain that can influence the protein’s properties and interactions. The primary structure is essentially a linear chain of amino acids, and any alteration in this sequence can lead to significant changes in the protein’s function and stability.
2. Secondary Structure
Secondary structure refers to the local folding of the polypeptide chain into specific patterns such as alpha-helices, beta-pleated sheets, and random coils. These structures are stabilized primarily by hydrogen bonds between the backbone atoms of the amino acids. The alpha-helix is a right-handed coil where each amino acid forms a hydrogen bond with the fourth amino acid ahead in the chain, while beta-sheets consist of beta-strands connected laterally by at least two or three backbone hydrogen bonds, forming a sheet-like structure. These secondary structures contribute to the overall stability and functionality of the protein.
3. Tertiary Structure
The tertiary structure of plasma proteins is the overall three-dimensional shape that the polypeptide chain assumes after folding. This structure is stabilized by various interactions, including hydrophobic interactions, hydrogen bonds, ionic bonds, and disulfide bridges between cysteine residues. The tertiary structure is crucial for the protein’s biological activity, as it determines the spatial arrangement of the active sites and other functional regions. Techniques such as X-ray crystallography and nuclear magnetic resonance (NMR) are often used to study and model the tertiary structure of proteins.
4. Quaternary Structure
Quaternary structure refers to the assembly of multiple polypeptide chains into a single functional protein complex. These polypeptide chains, also known as subunits, can be identical or different and are held together by non-covalent interactions such as hydrogen bonds, ionic bonds, and hydrophobic interactions. The quaternary structure is essential for the functionality of many proteins, including hemoglobin, which consists of four subunits. This level of structure allows for cooperative interactions between subunits, which can enhance the protein’s functionality and regulation.
Types of plasma proteins
Plasma proteins are vital components of the blood, each serving unique and essential functions. The primary types of plasma proteins include albumin, globulins, and fibrinogen, each contributing to various physiological processes. Below are Types of plasma proteins:
1. Albumin
Albumin is a crucial plasma protein, constituting about 55% of the total blood proteins. It is primarily synthesized in the liver and plays a significant role in maintaining the osmotic pressure necessary for the proper distribution of body fluids between body tissues and the bloodstream. Albumin is also involved in the transport of various substances, including hormones, vitamins, and drugs, throughout the body. Its widespread presence in cells, connective tissues, and interstitial spaces indicates its essential role in tissue nutrition and internal nitrogen metabolism. Additionally, albumin’s turnover rate is closely correlated with body size, highlighting its dynamic nature in physiological processes.
2. Globulins
Globulins are a diverse group of plasma proteins that make up about 38% of the total blood proteins. They are categorized into alpha, beta, and gamma globulins, each with distinct functions and origins. While many globulins are produced by the liver, others are synthesized by the immune system. Alpha and beta globulins are involved in various transport and enzymatic activities, including the binding and transport of lipids and metal ions. Gamma globulins, or immunoglobulins, are critical components of the immune response, providing defense against infections. The differential localization and function of globulins underscore their importance in both normal physiological processes and pathological conditions.
3. Fibrinogen
Fibrinogen is a key plasma protein involved in blood coagulation. It is primarily synthesized in the liver and is converted into fibrin during the clotting process, forming a mesh that helps to stop bleeding. Fibrinogen is found predominantly in the lymphatic and vascular channels, connective tissues, and interstitial spaces, reflecting its role in maintaining hemostasis. The synthesis of fibrinogen can be significantly influenced by hormonal and nutritional factors, with increased production observed in response to certain injuries and inflammatory conditions. Its presence in amyloid fibrils also indicates a role in pathological states such as amyloidosis.
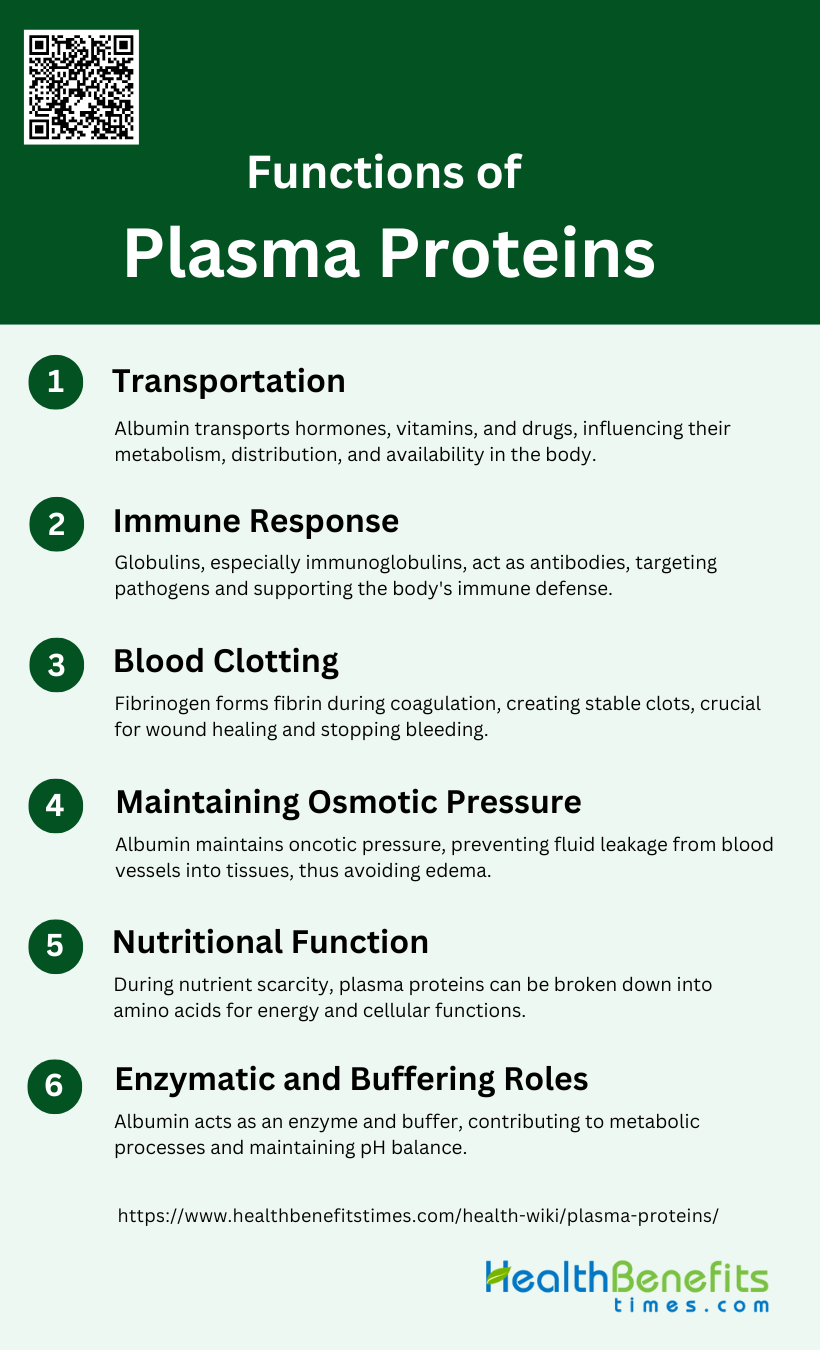
Functions of Plasma Proteins
Plasma proteins perform a variety of essential functions that are crucial for maintaining homeostasis and overall health. These functions include transportation of substances, immune response, blood clotting, maintaining osmotic pressure, nutritional support, and enzymatic and buffering roles. Below are Functions of Plasma Proteins:
1. Transportation
Albumin is a key plasma protein responsible for the transport of various substances in the blood. It binds to a wide range of molecules, including hormones, vitamins, and drugs, significantly influencing their pharmacokinetics and toxicokinetics. This binding capacity allows albumin to transport these substances efficiently throughout the body, ensuring their availability where needed and aiding in their metabolism and excretion.
2. Immune Response
Globulins, particularly immunoglobulins, play a crucial role in the immune system. They function as antibodies, identifying and neutralizing pathogens such as bacteria and viruses. This action is vital for the body’s defense mechanisms, helping to prevent infections and diseases by targeting and eliminating foreign invaders.
3. Blood Clotting
Fibrinogen is an essential plasma protein involved in the blood coagulation process. Upon activation by thrombin, fibrinogen is converted into fibrin, which forms a mesh that traps blood cells and platelets, creating a stable blood clot. This process is critical for stopping bleeding and initiating wound healing.
4. Maintaining Osmotic Pressure
Albumin is pivotal in maintaining colloidal osmotic pressure, also known as oncotic pressure, in the blood. This pressure is essential for preventing the leakage of fluid from blood vessels into surrounding tissues, thereby preventing edema. By maintaining the balance of fluid distribution, albumin ensures proper vascular function and tissue hydration.
5. Nutritional Function
Under extreme conditions, such as prolonged fasting or severe illness, plasma proteins can serve as a nutrient source. The body can break down these proteins into amino acids, which are then used for energy production and vital cellular functions, ensuring survival during periods of nutrient scarcity.
6. Enzymatic and Buffering Roles
Albumin also exhibits enzymatic activities, such as esterase or pseudoesterase activity, which contribute to various metabolic processes. Additionally, albumin helps maintain pH balance in the blood by acting as a buffer, neutralizing excess acids and bases to stabilize the body’s internal environment.
Plasma Protein Synthesis
Plasma protein synthesis is a crucial process in the human body, primarily occurring in the liver. These proteins are essential for various functions, including blood clotting, immune responses, and maintaining osmotic balance. Below are the key aspects of plasma protein synthesis:
1. Sites of Synthesis in the Body
Plasma proteins are primarily synthesized in the liver, which is responsible for producing most of the major plasma proteins, including albumin, fibrinogen, and a significant portion of the globulins. The liver’s role in plasma protein synthesis has been confirmed through various methods, such as the use of isotopic tracers and perfused liver studies, which demonstrate that the liver can synthesize these proteins both qualitatively and quantitatively similar to an intact organism. Additionally, electron microscopic studies have shown that protein synthesis in hepatocytes occurs mainly on ribosomes in the rough endoplasmic reticulum. While the liver is the dominant site, other tissues like the placenta and fetal tissues may also contribute to plasma protein synthesis during specific developmental stages.
2. Factors Influencing Synthesis
Several factors influence the synthesis of plasma proteins, including hormonal regulation, nutrient availability, and the presence of specific stimulating factors. Insulin, for example, has been shown to differentially affect the synthesis of specific plasma proteins. Nutrient availability, particularly amino acids and iron, also plays a crucial role in protein synthesis, as demonstrated in studies with rabbit reticulocytes. Additionally, factors released by human keratinocytes and monocytes can regulate the synthesis of acute phase plasma proteins in hepatic cells, indicating that immune responses and cellular interactions significantly impact plasma protein production. The synthesis process is also influenced by the rate of protein degradation, which is regulated to compensate for protein turnover.
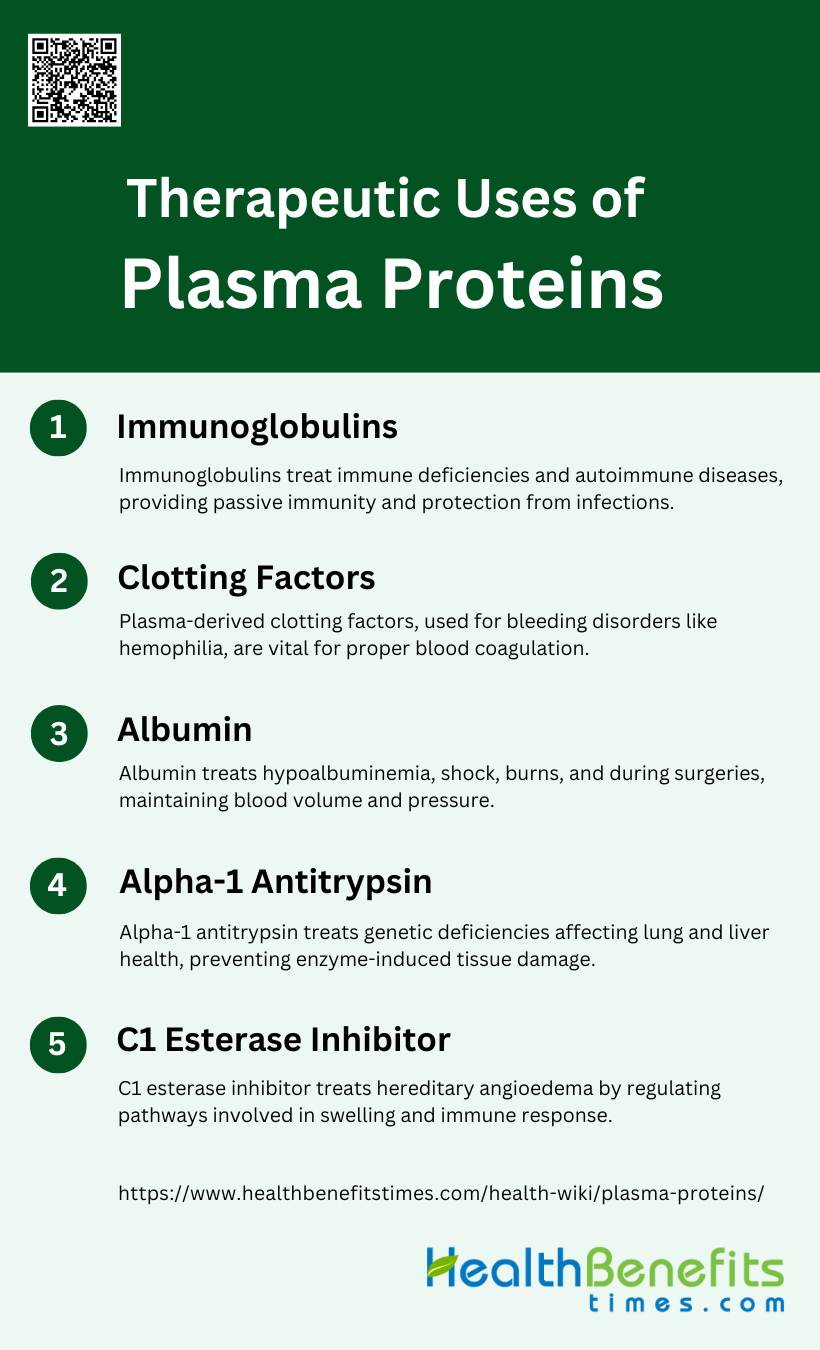
Therapeutic Uses of Plasma Proteins
Plasma proteins have a wide range of therapeutic applications, playing crucial roles in treating various medical conditions. These proteins are used to enhance immune function, aid in blood clotting, and manage protein deficiencies, among other uses. Below are some key therapeutic uses of plasma proteins:
1. Immunoglobulins
Immunoglobulins (IgGs) are essential plasma-derived proteins used in the treatment of various immune deficiencies and autoimmune diseases. They are available in polyvalent forms, which provide broad-spectrum immunity, and hyperimmune forms, which target specific pathogens such as hepatitis B, rabies, and tetanus. Immunoglobulins are derived from human plasma and are crucial for patients with compromised immune systems, offering passive immunity and reducing the risk of infections. Recent advances have also seen the use of convalescent plasma containing therapeutic antibodies for treating infectious diseases.
2. Clotting Factors
Clotting factors, including factors VIII, IX, and von Willebrand factor, are critical for managing bleeding disorders such as hemophilia and von Willebrand disease. These proteins are derived from human plasma and are essential for proper blood coagulation. The development of recombinant alternatives has reduced the reliance on plasma-derived clotting factors, but plasma-derived products remain vital for certain patients. Advances in plasma fractionation and viral inactivation techniques have significantly improved the safety and efficacy of these therapeutic proteins.
3. Albumin
Albumin is the most abundant protein in human plasma and has been used therapeutically for over 40 years. It is primarily used to treat hypoalbuminemia, shock, burns, and during surgeries to maintain blood volume and pressure. Albumin’s ability to bind and transport various substances makes it a versatile therapeutic agent. Despite the advent of recombinant technologies, plasma-derived albumin remains a cornerstone in clinical practice due to its proven efficacy and safety profile.
4. Alpha-1 Antitrypsin
Alpha-1 antitrypsin (A1AT) is a protease inhibitor used to treat A1AT deficiency, a genetic disorder that can lead to severe lung and liver disease. Plasma-derived A1AT is the standard treatment, providing the necessary protein to inhibit destructive enzymes in the lungs. Advances in recombinant technology have led to the development of glyco-engineered CHO cell lines producing A1AT with humanized N-glycosylation profiles, potentially reducing the dependence on plasma-derived sources. This innovation aims to ensure a safer and more sustainable supply of A1AT for therapeutic use.
5. C1 Esterase Inhibitor
C1 esterase inhibitor (C1-INH) is used to treat hereditary angioedema (HAE), a condition characterized by recurrent episodes of severe swelling. Plasma-derived C1-INH is effective in preventing and treating acute HAE attacks by regulating the complement and contact system pathways. Recombinant C1-INH with humanized glycosylation profiles has been developed to provide a safer alternative to plasma-derived products, minimizing the risk of infectious disease transmission. The increasing availability of C1-INH has significantly improved the quality of life for patients with HAE.
Importance of Plasma Protein Balance
Maintaining a proper balance of plasma proteins is essential for various physiological functions and overall health. These proteins are involved in maintaining oncotic pressure, transporting substances, immune function, blood clotting, and more. Below are the key aspects of plasma protein balance:
1. Maintaining Oncotic Pressure
Plasma proteins, particularly albumin, play a crucial role in maintaining oncotic pressure, which is essential for the regulation of fluid distribution between blood vessels and tissues. Albumin, being the most abundant plasma protein, exerts a significant osmotic force that helps retain water within the circulatory system, thereby preventing edema and ensuring proper vascular fluid balance. This function is vital for maintaining blood volume and pressure, which are critical for normal cardiovascular function and overall homeostasis.
2. Transport of Substances
Plasma proteins, especially serum albumin, are key transporters of various substances within the bloodstream. They bind and carry hormones, vitamins, fatty acids, metals, and drugs, facilitating their distribution to different tissues and organs. This transport function is essential for the proper delivery of nutrients and medications, as well as the removal of waste products and toxins from the body. The ability of albumin to bind a wide range of ligands also influences the pharmacokinetics and efficacy of many therapeutic agents.
3. Immune Function
Plasma proteins, including immunoglobulins and complement proteins, are integral to the immune system. Immunoglobulins (antibodies) identify and neutralize pathogens, while complement proteins enhance the ability of antibodies and phagocytic cells to clear microbes and damaged cells. These proteins work together to protect the body against infections and play a role in inflammation and immune regulation. The balance and proper functioning of these proteins are crucial for an effective immune response and for preventing autoimmune disorders.
4. Blood Clotting
Plasma proteins are essential for the blood clotting process, which prevents excessive bleeding following injury. Key proteins involved in coagulation include fibrinogen, prothrombin, and various clotting factors that interact in a complex cascade to form a stable blood clot. Thrombin, a central enzyme in this process, converts fibrinogen to fibrin, which forms the structural basis of a clot. Proper regulation of these proteins ensures balanced hemostasis, preventing both excessive bleeding and inappropriate clot formation.
5. Acid-Base Balance
Plasma proteins contribute to the buffering capacity of blood, helping to maintain acid-base balance. Albumin, in particular, can bind to hydrogen ions, thus acting as a buffer and stabilizing the pH of the blood. This buffering action is crucial for maintaining the optimal pH range necessary for various enzymatic and metabolic processes. Disruptions in plasma protein levels can lead to imbalances in acid-base homeostasis, affecting overall metabolic function and health.
6. Enzyme Activity
Certain plasma proteins exhibit enzymatic activities that are vital for metabolic processes. Human serum albumin (HSA), for example, displays pseudo-enzymatic activities such as esterase, enolase, and peroxidase functions, which are important for the metabolism of endogenous and exogenous compounds. These enzymatic properties enable plasma proteins to participate in detoxification processes, antioxidant defense, and the activation of pro-drugs, thereby contributing to overall metabolic homeostasis and protection against oxidative stress.
7. Vascular Integrity
Plasma proteins, particularly albumin and orosomucoid, are crucial for maintaining vascular integrity and endothelial permeability. They help regulate the passage of fluids and macromolecules across the vascular endothelium, ensuring that the vascular barrier functions properly. This regulation is essential for preventing leakage of plasma components into the interstitial space, which can lead to edema and tissue damage. Proper vascular integrity is vital for maintaining effective circulation and tissue perfusion.
8. Hormone Regulation
Plasma proteins play a significant role in hormone regulation by binding and transporting various hormones throughout the body. This binding not only facilitates the distribution of hormones but also protects them from degradation and regulates their bioavailability. For instance, albumin and other binding proteins transport thyroid hormones, cortisol, and sex hormones, ensuring that they reach their target tissues in a controlled manner. This regulation is crucial for maintaining hormonal balance and proper endocrine function.
FAQs
1. How do plasma protein levels change with age?
Plasma protein levels can fluctuate with age. Albumin, for example, tends to decrease as people get older, which can affect overall health. Some other plasma proteins, like immunoglobulins, may increase as the immune system adapts over time.
2. What are the effects of malnutrition on plasma protein synthesis?
Malnutrition, particularly protein-energy malnutrition, can reduce the liver’s ability to produce plasma proteins like albumin. This can lead to edema, weakened immune responses, and impaired wound healing.
3. Can certain medications affect plasma protein levels?
Yes, some medications, such as corticosteroids or chemotherapy drugs, can affect the synthesis or degradation of plasma proteins, potentially leading to altered levels of albumin, globulins, or other important proteins.
4. How are plasma proteins involved in managing chronic conditions like liver disease?
In liver disease, plasma protein production, particularly albumin, is often reduced, which can result in complications like ascites or fluid retention. Monitoring plasma protein levels helps manage these conditions.
5. Are plasma proteins affected by hydration levels?
Yes, dehydration can increase the concentration of plasma proteins like albumin, while overhydration can dilute them, affecting their functions such as maintaining osmotic pressure.
6. How does pregnancy affect plasma protein levels?
During pregnancy, plasma protein levels, especially albumin, may decrease due to hemodilution, while levels of certain globulins involved in immune function might increase to support the body’s defenses.
7. Can plasma protein abnormalities be a sign of autoimmune diseases?
Yes, abnormal plasma protein levels, particularly immunoglobulins, can indicate autoimmune diseases. Elevated levels of specific types of globulins may suggest conditions such as lupus or rheumatoid arthritis.
8. How do plasma proteins affect drug efficacy?
Plasma proteins, particularly albumin, bind to various drugs, affecting their bioavailability. Changes in plasma protein levels can alter the concentration of free (active) drug in the bloodstream, influencing the drug’s efficacy and potential side effects.
9. What is the role of plasma proteins in detoxification?
Plasma proteins like albumin help transport waste products and toxins to the liver for detoxification. Additionally, some proteins act as antioxidants, neutralizing harmful free radicals in the blood.
10. Do plasma proteins have a role in heat regulation?
While plasma proteins are not directly involved in temperature regulation, their role in maintaining blood volume and circulation helps support the body’s ability to regulate temperature, especially during dehydration or fever.