Pain is a complex and subjective experience that involves both sensory and emotional components. According to the revised 2020 definition by the International Association for the Study of Pain (IASP), pain is “an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage”. This definition acknowledges that pain can occur not only in response to actual tissue damage but also in situations where the threat of damage is perceived or when the experience resembles that of tissue damage. Pain is inherently personal and can vary widely in intensity, duration, and nature, making it challenging to assess and manage, especially in populations with limited ability to self-report, such as young children or individuals with cognitive impairments. The experience of pain encompasses physiological, behavioral, social, and cognitive aspects, highlighting its multidimensional nature and the importance of considering these factors in both clinical assessment and treatment approaches.
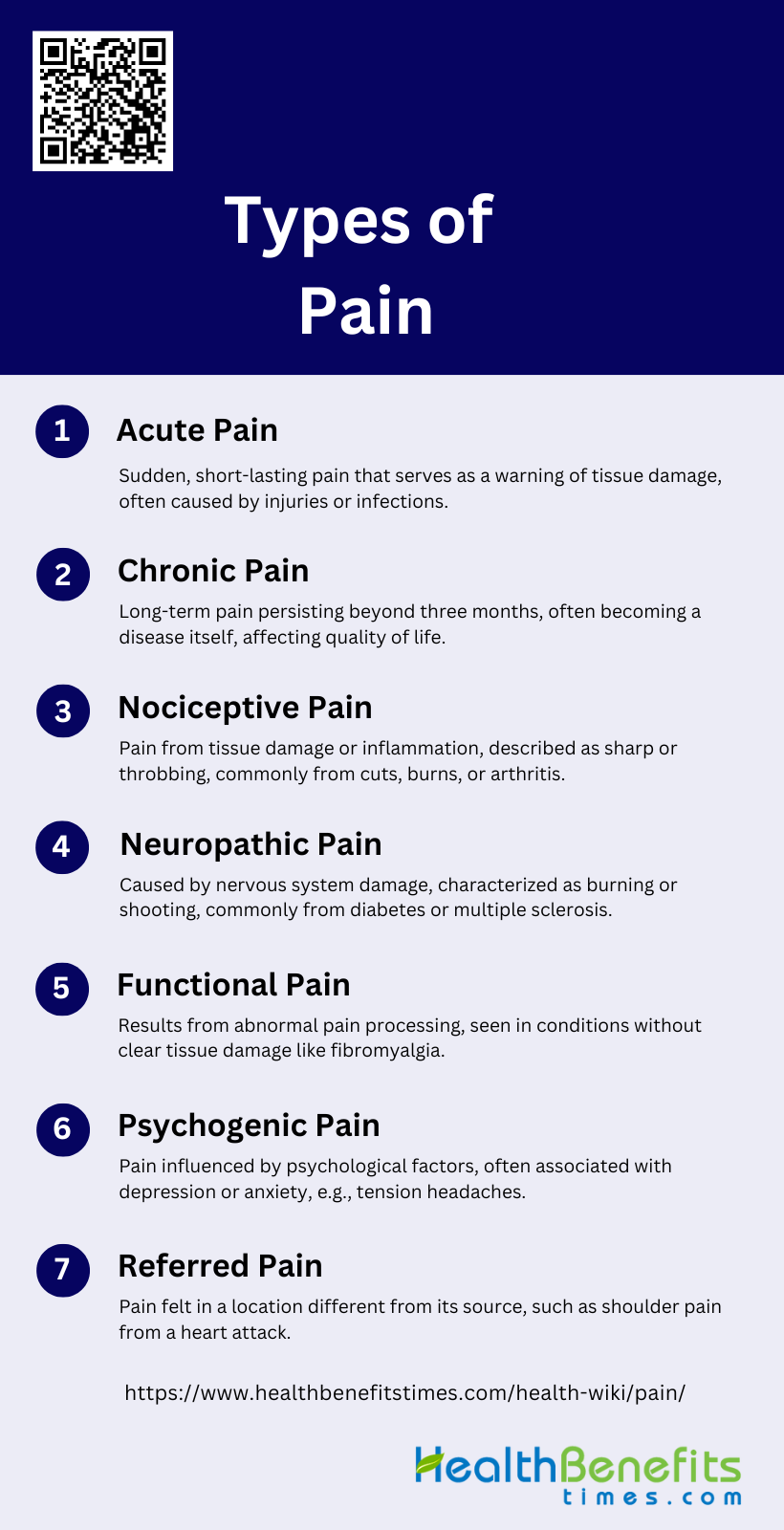
Types of Pain
Pain can be classified into various types based on its origin, duration, and intensity. Understanding these categories helps in diagnosing and treating different pain conditions effectively. Below is a list of the primary types of pain:
1. Acute Pain
Acute pain is a sudden onset of pain that typically lasts for a short duration, usually less than three months. It serves as a warning signal of actual or potential tissue damage and is often sharp and intense. Common causes include injuries, surgeries, and acute illnesses such as infections or inflammations.
2. Chronic Pain
Chronic pain persists for longer than three months and can continue even after the initial injury or illness has healed. It is often considered a disease in itself due to its complex nature and significant impact on quality of life. Common conditions associated with chronic pain include arthritis, fibromyalgia, and chronic back pain.
3. Nociceptive Pain
Nociceptive pain arises from the activation of nociceptors due to tissue damage or inflammation. It is typically described as sharp, aching, or throbbing and is often localized to the area of injury. Examples include pain from cuts, burns, and inflammatory conditions like arthritis.
4. Neuropathic Pain
Neuropathic pain is caused by a lesion or disease affecting the somatosensory nervous system. It is often described as burning, shooting, or electric shock-like and can be either spontaneous or provoked by stimuli. Common causes include diabetic neuropathy, postherpetic neuralgia, and multiple sclerosis.
5. Functional Pain
Functional pain results from abnormal central processing of normal sensory input, leading to hypersensitivity. It is often seen in conditions where no clear structural or tissue damage is evident, such as fibromyalgia and irritable bowel syndrome. The exact mechanisms are not fully understood but involve altered pain modulation in the central nervous system.
6. Psychogenic Pain
Psychogenic pain is pain that is primarily caused or exacerbated by psychological factors. It can manifest in any part of the body and is often associated with conditions like depression and anxiety. Common examples include tension headaches and some forms of chronic back pain.
7. Referred Pain
Referred pain is pain perceived at a location other than the site of the painful stimulus. It occurs due to the convergence of nerve fibers in the spinal cord, leading to the brain misinterpreting the source of the pain. Common examples include shoulder pain from a heart attack and arm pain from a cervical spine issue.
Causes of Pain
Pain can arise from a multitude of sources, each contributing to the discomfort experienced. Identifying the root causes is crucial for effective treatment and management. Below is a list of common causes of pain:
1. Tissue Damage
Tissue damage is a primary cause of pain, often resulting from injury, surgery, or inflammation. When tissues are damaged, they release inflammatory mediators such as prostaglandins and cytokines, which activate nociceptors (pain receptors) in the affected area. This activation leads to the sensation of pain, which serves as a protective mechanism to prevent further injury. For instance, post-surgical pain is a common example where tissue damage from the surgical procedure leads to acute pain, which can sometimes transition into chronic pain if not managed properly. Effective pain management strategies, including the use of anti-inflammatory drugs and local anesthetics, are crucial in mitigating pain resulting from tissue damage.
2. Nerve Damage or Dysfunction
Nerve damage or dysfunction, often referred to as neuropathic pain, occurs when there is direct injury to the nerves. This type of pain is characterized by sensations such as burning, tingling, or shooting pain. Surgical procedures, such as breast cancer surgery involving intercostobrachial nerve resection, can lead to chronic postsurgical neuropathic pain (CPSNP) in some patients. Factors such as preoperative pain, psychological burden, and insomnia are associated with the development of CPSNP. Additionally, conditions like complex regional pain syndrome (CRPS) also involve nerve dysfunction and are marked by severe pain and inflammation.
3. Central Sensitization
Central sensitization refers to the increased sensitivity of the central nervous system (CNS) to pain stimuli, often resulting in chronic pain conditions. This phenomenon occurs when the CNS undergoes changes that amplify pain signals, making even non-painful stimuli feel painful. Central sensitization is a key mechanism in conditions like fibromyalgia and chronic postoperative pain. It involves augmented CNS pain processing and altered pain modulation, leading to widespread and intense pain that is disproportionate to the initial injury or inflammation. Addressing central sensitization requires a comprehensive approach, including pharmacological and non-pharmacological therapies.
4. Poor Posture
Poor posture can lead to musculoskeletal pain by placing undue stress on muscles, ligaments, and joints. Over time, this stress can cause muscle imbalances, joint misalignment, and strain on the spine, leading to chronic pain conditions such as back pain and neck pain. Maintaining proper posture is essential to prevent these issues. Ergonomic interventions, physical therapy, and exercises aimed at strengthening the core and improving posture can help alleviate pain caused by poor posture. Chronic poor posture can also contribute to the development of conditions like tension-type headaches, which are associated with muscle tension and strain.
5. Being Overweight
Being overweight or obese increases the risk of developing pain due to the additional stress placed on weight-bearing joints, such as the knees and hips. This excess weight can lead to conditions like osteoarthritis, where the cartilage in the joints wears down, causing pain and inflammation. Additionally, obesity is associated with systemic inflammation, which can exacerbate pain conditions. Weight management through diet, exercise, and lifestyle changes is crucial in reducing pain and improving overall health. Studies have shown that weight loss can significantly reduce pain levels and improve function in individuals with obesity-related pain conditions.
6. Stress and Anxiety
Stress and anxiety are significant contributors to pain, as they can amplify the perception of pain and lead to chronic pain conditions. Psychological factors such as depression, anxiety, and stress are known to exacerbate pain and are often associated with conditions like chronic postoperative pain and fibromyalgia. The interplay between psychological stress and pain involves complex mechanisms, including the activation of the hypothalamic-pituitary-adrenal (HPA) axis and the release of stress hormones, which can sensitize the nervous system to pain. Addressing stress and anxiety through cognitive-behavioral therapy, mindfulness, and relaxation techniques can help manage pain effectively.
7. Sleep Problems
Sleep problems, including insomnia and poor sleep quality, are closely linked to the experience of pain. Lack of sleep can lower pain thresholds and increase pain sensitivity, leading to a vicious cycle where pain disrupts sleep, and poor sleep exacerbates pain. Chronic pain conditions such as fibromyalgia and chronic postoperative pain are often associated with sleep disturbances. Improving sleep hygiene, using cognitive-behavioral therapy for insomnia (CBT-I), and addressing underlying sleep disorders are essential strategies in managing pain and improving overall quality of life.
8. Injury or Trauma
Injury or trauma is a common cause of acute pain, which can sometimes transition into chronic pain if not properly managed. Traumatic injuries, such as fractures, burns, and soft tissue injuries, can lead to significant pain and disability. In some cases, maladaptive sensitization of the nervous system following trauma can result in chronic pain syndromes, characterized by persistent pain, allodynia, and hyperalgesia. Early and effective pain management, including the use of analgesics, physical therapy, and psychological support, is crucial in preventing the transition from acute to chronic pain in trauma patients.
9. Medical Conditions
Various medical conditions can cause pain, either as a primary symptom or as a secondary complication. Conditions such as arthritis, cancer, diabetes, and fibromyalgia are known to cause chronic pain. For example, cancer pain can result from tumor growth, treatment-related side effects, or nerve damage. Similarly, diabetic neuropathy is a common complication of diabetes that leads to nerve pain. Managing pain in these conditions requires a multidisciplinary approach, including pharmacological treatments, physical therapy, and psychological support, to address the underlying disease and alleviate pain symptoms.
10. Inflammation
Inflammation is a key driver of pain in many conditions, including arthritis, infections, and injuries. Inflammatory mediators such as prostaglandins, cytokines, and chemokines are released at the site of inflammation, activating nociceptors and causing pain. Chronic inflammation can lead to persistent pain conditions, as seen in rheumatoid arthritis and inflammatory bowel disease. Anti-inflammatory medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids, are commonly used to reduce inflammation and alleviate pain. Additionally, lifestyle modifications, including diet and exercise, can help manage chronic inflammation and associated pain.
11. Post-surgery or Post-medical Treatment
Post-surgery or post-medical treatment pain is a common occurrence, with some patients developing chronic postsurgical pain (CPSP). Factors such as the type of surgery, preoperative pain, and psychological vulnerability can influence the development of CPSP. Surgical techniques that minimize nerve injury and the use of pharmacological agents to interrupt central sensitization mechanisms can help reduce the incidence of CPSP. Additionally, addressing psychosocial factors and providing comprehensive perioperative care are essential in preventing and managing post-surgical pain. Effective pain management strategies are crucial to improve patient outcomes and quality of life after surgery.
Pain Management Techniques
Managing pain effectively requires a comprehensive approach that addresses both the physical and psychological aspects. Various techniques can be employed to alleviate pain and improve quality of life. Below is a list of pain management techniques:
1. Professional Medical Treatment
Professional medical treatment forms the cornerstone of pain management, offering a range of evidence-based approaches to alleviate discomfort and improve quality of life.
- Medications: play a crucial role, with over-the-counter options like NSAIDs providing relief for mild to moderate pain, while prescription drugs such as opioids are reserved for severe cases.
- Surgical interventions: may be necessary for certain conditions, offering long-term solutions by addressing underlying causes of pain.
- Physical therapy: is an essential component, focusing on exercises and techniques to strengthen muscles, improve flexibility, and reduce pain through targeted movements and manual therapies. These professional treatments are often combined to create comprehensive pain management plans tailored to individual patient needs.
2. Alternative Therapies
Alternative therapies offer complementary approaches to pain management, often used alongside conventional treatments.
- Acupuncture: an ancient Chinese practice, involves inserting thin needles into specific points on the body to alleviate pain and promote healing.
- Chiropractic care: focuses on spinal manipulation and other manual adjustments to improve musculoskeletal alignment and reduce pain, particularly effective for back and neck issues.
- Massage therapy: provides relief through the manipulation of soft tissues, helping to reduce muscle tension, improve circulation, and promote relaxation. While the effectiveness of these therapies can vary among individuals, many patients report significant pain reduction and improved overall well-being when incorporating these alternative approaches into their pain management regimens.
3. Self-Management Techniques
Self-management techniques empower individuals to take an active role in their pain management, often complementing professional treatments.
- Home remedies and lifestyle changes: can significantly impact pain levels, including proper nutrition, regular exercise, and adequate sleep hygiene. Simple interventions like applying heat or cold packs, practicing good posture, and using ergonomic tools can also provide relief.
- Mindfulness and meditation: practices have gained recognition for their ability to reduce pain perception and improve coping skills. These techniques, such as deep breathing exercises, progressive muscle relaxation, and guided imagery, help individuals manage stress and anxiety associated with chronic pain, leading to improved pain tolerance and overall quality of life.
4. Technology in Pain Management
Technology has revolutionized pain management, offering innovative tools to track, analyze, and alleviate discomfort.
- Apps and wearable devices: have become increasingly popular, providing users with the ability to monitor pain levels, medication schedules, and activity patterns. These digital solutions often incorporate features like pain diaries, reminder systems, and educational resources to enhance self-management.
- Technology aids in tracking and managing pain: by collecting and analyzing data, allowing healthcare providers to make more informed decisions about treatment plans. Advanced technologies such as virtual reality for pain distraction, AI-powered pain prediction models, and smart implantable devices are pushing the boundaries of pain management, offering new hope for those suffering from chronic pain conditions.
Pain Management Tips for Daily Life
Managing chronic pain on a daily basis can be challenging, but incorporating certain strategies can make a significant difference. These tips aim to provide relief and improve overall well-being. Below is a list of pain management tips for daily life:
1. Exercise Regularly
Regular exercise is a cornerstone of pain management, particularly for chronic conditions such as low back pain and osteoarthritis. Exercise can reduce pain severity, improve physical function, and enhance overall quality of life. Various forms of exercise, including aerobic, strength, flexibility, and balance training, have been shown to be beneficial. For instance, a review of Cochrane Reviews found that physical activity and exercise programs can lead to small-to-moderate improvements in pain severity and physical function, although the quality of evidence is low due to small sample sizes and short follow-up periods. Therefore, incorporating regular exercise into daily routines can be a highly effective strategy for managing chronic pain.
2. Practice Stress Management
Stress management is crucial for individuals dealing with chronic pain, as stress can exacerbate pain symptoms and negatively impact overall well-being. Techniques such as cognitive-behavioral therapy (CBT), mindfulness meditation, and relaxation exercises have been shown to be effective in reducing stress and improving pain outcomes. A biobehavioral pain hygiene model suggests that integrating stress reduction strategies, such as meditation and maintaining a calm environment, can significantly improve pain management. Additionally, multimodal care approaches that include stress self-management have been recommended for persistent neck pain. Therefore, practicing stress management techniques can help mitigate pain and improve quality of life.
3. Improve Sleep Habits
Improving sleep habits is essential for managing chronic pain, as poor sleep can worsen pain and reduce the ability to cope with it. Mindfulness-based exercises, such as Baduanjin, have been found to improve sleep quality and alleviate musculoskeletal pain in individuals with chronic conditions. Additionally, addressing co-occurring symptoms like sleep disturbances through lifestyle modifications and cognitive-behavioral strategies can enhance overall pain management. Therefore, establishing a regular sleep routine and incorporating relaxation techniques before bedtime can help improve sleep quality and reduce pain.
4. Eat a Healthy Diet
A healthy diet plays a significant role in managing chronic pain by reducing inflammation and promoting overall health. Diet and lifestyle modifications, such as maintaining a healthy body weight and consuming anti-inflammatory foods, are recommended as part of a comprehensive pain management strategy. For example, a clinical practice guideline for managing chronic musculoskeletal pain emphasizes the importance of lifestyle modifications, including diet, to improve patient outcomes. Therefore, adopting a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can support pain management efforts.
5. Track Your Pain
Tracking pain can provide valuable insights into pain patterns and triggers, helping individuals and healthcare providers develop more effective management strategies. Self-management programs often include pain tracking as a component to enhance self-efficacy and mastery of pain management techniques. For instance, a study on self-management of osteoarthritic knee pain found that participants who tracked their pain and used self-management techniques experienced significant improvements in pain intensity and daily activity. Therefore, keeping a pain diary or using pain tracking apps can be a useful tool for managing chronic pain.
6. Use Hot and Cold Therapy
Hot and cold therapy are simple yet effective methods for managing pain. Applying heat can relax muscles and improve blood flow, while cold therapy can reduce inflammation and numb painful areas. These techniques are often recommended as part of self-management strategies for conditions like osteoarthritis and low back pain. For example, a self-management program for osteoarthritic knee pain that included the use of hot and cold compresses showed significant improvements in pain and function. Therefore, incorporating hot and cold therapy into daily routines can provide relief from chronic pain.
7. Stay Socially Connected
Staying socially connected is important for emotional well-being and can help alleviate the psychological burden of chronic pain. Social support can provide emotional comfort, reduce feelings of isolation, and improve overall quality of life. A review of self-management strategies for older adults with chronic pain highlighted the benefits of community-based programs that promote social interaction and support. Additionally, maintaining a positive support system is a key component of the biobehavioral pain hygiene model for managing chronic pain. Therefore, engaging in social activities and maintaining strong relationships can be beneficial for pain management.
8. Practice Self-Care
Practicing self-care is essential for managing chronic pain and improving overall well-being. Self-care strategies can include a range of activities such as relaxation techniques, mindfulness practices, and engaging in hobbies that bring joy and relaxation. Self-management programs that emphasize self-care have been shown to improve pain outcomes and enhance the ability to perform daily activities. For example, a clinical practice guideline for managing chronic musculoskeletal pain recommends self-management advice and education as part of a multimodal approach to treatment. Therefore, prioritizing self-care activities can help individuals better manage their pain and improve their quality of life.
When to Seek Medical Help for Pain
Indicators that Pain is Severe or Persistent Enough to Require Professional Intervention
Pain that is severe or persistent often necessitates professional intervention to prevent further complications and improve quality of life. Indicators include pain that lasts beyond the normal tissue healing time, typically 12 weeks, and significantly impacts daily activities, sleep, or mental health. Persistent pain following surgery, such as in cases of groin hernia repair or leg amputation, can also be a sign of severe pain requiring medical attention, especially if it is associated with nerve damage. Additionally, chronic pain that leads to disability, anxiety, depression, or decreased socialization should prompt a visit to a healthcare provider. Early identification and intervention are crucial to prevent the transition from acute to chronic pain.
Importance of Early Intervention for Chronic Pain to Avoid Long-term Consequences
Early intervention in chronic pain is essential to avoid long-term consequences such as disability, psychological distress, and reduced quality of life. Chronic pain affects more than 30% of people worldwide and can lead to significant personal and economic burdens if not managed promptly. Psychological interventions, particularly when applied early, have shown benefits in reducing pain intensity and improving self-efficacy in managing pain, especially in older adults. Identifying patients at risk for developing persistent pain through early screening can help tailor interventions that prevent chronic pain and its associated disabilities. Moreover, early and aggressive treatment of postoperative pain can reduce the risk of developing persistent pain states. Addressing chronic pain early can also mitigate neuroplastic changes and improve overall health outcomes.
FAQs
1. Can emotional stress cause physical pain?
Yes, emotional stress can contribute to or exacerbate physical pain. Chronic stress triggers the release of stress hormones, which can increase inflammation and sensitivity to pain. Conditions like tension headaches, neck pain, and lower back pain are often linked to psychological stress.
2. How can pain affect mental health?
Chronic pain can have a significant impact on mental health, leading to issues like anxiety, depression, and sleep disorders. Pain can limit daily activities, leading to isolation and decreased quality of life, which in turn worsens emotional well-being.
3. What role does diet play in managing chronic pain?
A diet rich in anti-inflammatory foods, such as fruits, vegetables, and omega-3 fatty acids, may help manage chronic pain by reducing inflammation. Additionally, maintaining a healthy weight can alleviate pain in weight-bearing joints like the knees and hips.
4. Can pain sensitivity change over time?
Yes, pain sensitivity can change due to factors such as central sensitization, where the central nervous system becomes more sensitive to pain stimuli. This often occurs in chronic pain conditions, making even mild stimuli feel painful over time.
5. Are there any genetic factors that influence pain perception?
Yes, genetic factors can influence how individuals perceive and tolerate pain. Certain genetic variations affect the way pain signals are processed in the brain and can determine a person’s susceptibility to chronic pain conditions.
6. What are the differences between pain tolerance and pain threshold?
Pain tolerance refers to the maximum level of pain a person can endure, while pain threshold is the point at which a stimulus begins to be perceived as painful. Both can vary greatly between individuals and can be influenced by psychological and physical factors.
7. Can the weather affect pain levels?
Yes, changes in weather, particularly cold temperatures and changes in barometric pressure, can influence pain levels in some individuals, especially those with conditions like arthritis. Cold weather can stiffen joints and increase discomfort.
8. How does age impact pain perception and management?
As people age, changes in the nervous system and decreased sensitivity to pain medications can alter how pain is perceived and managed. Older adults are more likely to suffer from chronic pain conditions such as arthritis, requiring tailored pain management strategies.
9. Can hormonal changes affect pain?
Yes, hormonal fluctuations, such as those experienced during menstruation, pregnancy, or menopause, can influence pain sensitivity and exacerbate conditions like migraines, joint pain, or fibromyalgia.
10. Can lack of physical activity worsen pain?
Yes, lack of physical activity can lead to muscle weakness, joint stiffness, and decreased mobility, all of which can worsen pain. Regular exercise, within an individual’s physical limits, can help reduce chronic pain by improving strength, flexibility, and circulation.