Oxygenated blood is blood that has been enriched with oxygen through the process of respiration in the lungs. When we breathe in, oxygen from the air enters the lungs and diffuses across the thin walls of the alveoli (tiny air sacs) into the bloodstream. There, it binds to hemoglobin molecules within red blood cells, turning the blood a bright red color. This oxygen-rich blood then leaves the lungs via the pulmonary veins and enters the left side of the heart, which pumps it out to the rest of the body through the aorta and other arteries. Oxygenated blood is crucial for supplying oxygen to all the tissues and organs of the body, enabling them to carry out their vital functions. The oxygen it carries is used by cells for aerobic respiration, the process by which they generate energy. Once the oxygen has been delivered to the tissues, the now deoxygenated blood returns to the heart and lungs to be re-oxygenated, completing the circulatory cycle.
Difference between Oxygenated and Deoxygenated Blood
Oxygenated blood is typically found in the arteries, while deoxygenated blood, which has lower oxygen content, is found in the veins. Oxygenated blood is pumped from the heart to the rest of the body through the arteries, delivering oxygen to tissues and organs. In contrast, deoxygenated blood returns to the heart through the veins after oxygen has been delivered and carbon dioxide has been collected from the tissues. The color difference between these two types of blood is notable: oxygenated blood appears bright red due to the high levels of oxygen bound to hemoglobin, whereas deoxygenated blood is darker red because of the reduced oxygen content. This color distinction is crucial in medical settings, such as during central venous catheterization, where identifying the type of blood can guide proper medical procedures.
How Blood Gets Oxygenated
The lungs play a crucial role in the oxygenation of blood, primarily through the function of the alveoli, which are tiny air sacs where gas exchange occurs. When air is inhaled, it reaches the alveoli, where oxygen diffuses across the alveolar membrane into the pulmonary capillaries, while carbon dioxide diffuses from the blood into the alveoli to be exhaled. This process is driven by the partial pressure gradients of oxygen and carbon dioxide, ensuring efficient gas exchange. Proper lung function is essential for maintaining these gradients and ensuring that blood is adequately oxygenated. Any impairment in lung function, such as in cases of lung injury or disease, can disrupt this delicate balance, leading to inadequate oxygenation of the blood and subsequent tissue hypoxia. Thus, the integrity of the alveolar-capillary interface and the overall health of the lungs are vital for effective blood oxygenation.
The Journey of Oxygen through the Body
How oxygen enters the bloodstream
Oxygen enters the bloodstream through a process that begins with inhalation. When we breathe in, air travels through the respiratory tract and reaches the alveoli, tiny air sacs in the lungs. The alveoli are surrounded by a network of capillaries, which are small blood vessels. Oxygen diffuses across the thin walls of the alveoli into the blood in the capillaries due to the concentration gradient between the alveolar air and the blood. This process is facilitated by the large surface area and thin barrier of the alveolar-capillary membrane, allowing efficient gas exchange.
Transporting oxygenated blood
Once oxygen has diffused into the blood, it binds to hemoglobin molecules within red blood cells. The heart plays a crucial role in transporting this oxygenated blood throughout the body. The left side of the heart pumps oxygen-rich blood into the systemic circulation via the aorta. Blood travels through arteries, arterioles, and capillaries, delivering oxygen to tissues and organs. The circulatory system ensures that oxygen is distributed to meet the metabolic demands of different tissues. After releasing oxygen, the now deoxygenated blood returns to the right side of the heart and is pumped to the lungs for reoxygenation.
Functions of Oxygenated Blood
Oxygenated blood is vital for sustaining life and maintaining the body’s homeostasis. It performs several critical functions that are essential for overall health and well-being. Below are the key functions of oxygenated blood:
1. Oxygen Delivery
Oxygen delivery is a primary function of oxygenated blood, facilitated by red blood cells (RBCs) which contain hemoglobin. Hemoglobin binds oxygen in the lungs and releases it in tissues where it is needed. This process is finely tuned by the allosteric properties of hemoglobin, which adjust its oxygen affinity based on the local environment, such as pH and carbon dioxide levels. Additionally, RBCs can sense hypoxic conditions and release vasodilatory compounds like nitric oxide (NO) to enhance blood flow to oxygen-deprived tissues, ensuring adequate oxygen delivery.
2. Nutrient Transport
Oxygenated blood is also responsible for transporting essential nutrients to various tissues and organs. Blood plasma carries glucose, amino acids, fatty acids, and vitamins absorbed from the digestive tract to cells throughout the body. This nutrient transport is crucial for cellular metabolism and energy production. The blood-brain barrier, for instance, tightly regulates the delivery of nutrients to the central nervous system, ensuring proper neuronal function and protecting against toxins. Thus, the efficient transport of nutrients by oxygenated blood is vital for maintaining overall physiological health.
3. Hormone Distribution
Hormones are chemical messengers that regulate various physiological processes, and their distribution is another critical function of oxygenated blood. Blood transports hormones from endocrine glands to target organs and tissues, where they exert their effects. For example, insulin from the pancreas regulates glucose uptake in cells, while adrenaline from the adrenal glands prepares the body for ‘fight or flight’ responses. This hormone distribution ensures that the body’s metabolic activities are coordinated and responsive to internal and external stimuli.
4. Temperature Regulation
Oxygenated blood plays a significant role in maintaining body temperature. Blood vessels can dilate or constrict to regulate heat loss or retention. In response to cold, blood flow to the skin is reduced to conserve heat, while in a hot environment, blood flow increases to dissipate heat through the skin. This thermoregulatory function is crucial for maintaining homeostasis and ensuring that enzymatic and metabolic processes occur at optimal temperatures. Additionally, the high specific heat capacity of blood allows it to absorb and distribute heat effectively throughout the body.
5. Waste Removal
The removal of metabolic waste products is another essential function of oxygenated blood. Blood transports waste products like carbon dioxide, urea, and lactic acid from tissues to excretory organs such as the lungs, kidneys, and liver. Efficient waste removal prevents the accumulation of toxic substances that can alter the cellular microenvironment and impair metabolic activities. For instance, carbon dioxide is transported from tissues to the lungs, where it is exhaled, while urea is filtered out by the kidneys and excreted in urine.
6. pH Balance
Maintaining pH balance is critical for proper cellular function, and oxygenated blood plays a key role in this process. Blood contains buffers like bicarbonate, hemoglobin, and plasma proteins that help neutralize excess acids or bases. The respiratory system also contributes by regulating carbon dioxide levels, which influence blood pH. For example, increased carbon dioxide levels lower blood pH, triggering a respiratory response to expel more CO2 and restore balance. This intricate regulation ensures that the body’s pH remains within the narrow range necessary for enzymatic and metabolic activities.
7. Immune Function
Oxygenated blood supports the immune system by transporting white blood cells (leukocytes) and other immune components to sites of infection or injury. Leukocytes play a crucial role in identifying and neutralizing pathogens, while platelets help in wound healing and clot formation. Blood components like plasma also contain antibodies and other proteins that aid in immune responses. This immune function is vital for protecting the body against infections and facilitating recovery from injuries. Additionally, blood-derived vesicles influence immune responses and vascular integrity, further enhancing immune competence.
8. Clotting
Blood clotting, or coagulation, is a critical function of oxygenated blood that prevents excessive bleeding when injuries occur. Platelets and clotting factors in the blood work together to form clots that seal wounds and stop hemorrhage. This process involves a cascade of reactions that result in the formation of a fibrin mesh, which stabilizes the clot. Effective clotting is essential for wound healing and maintaining vascular integrity. Blood components like plasma and cryoprecipitate are often transfused to support clotting in patients with bleeding disorders or during surgeries.
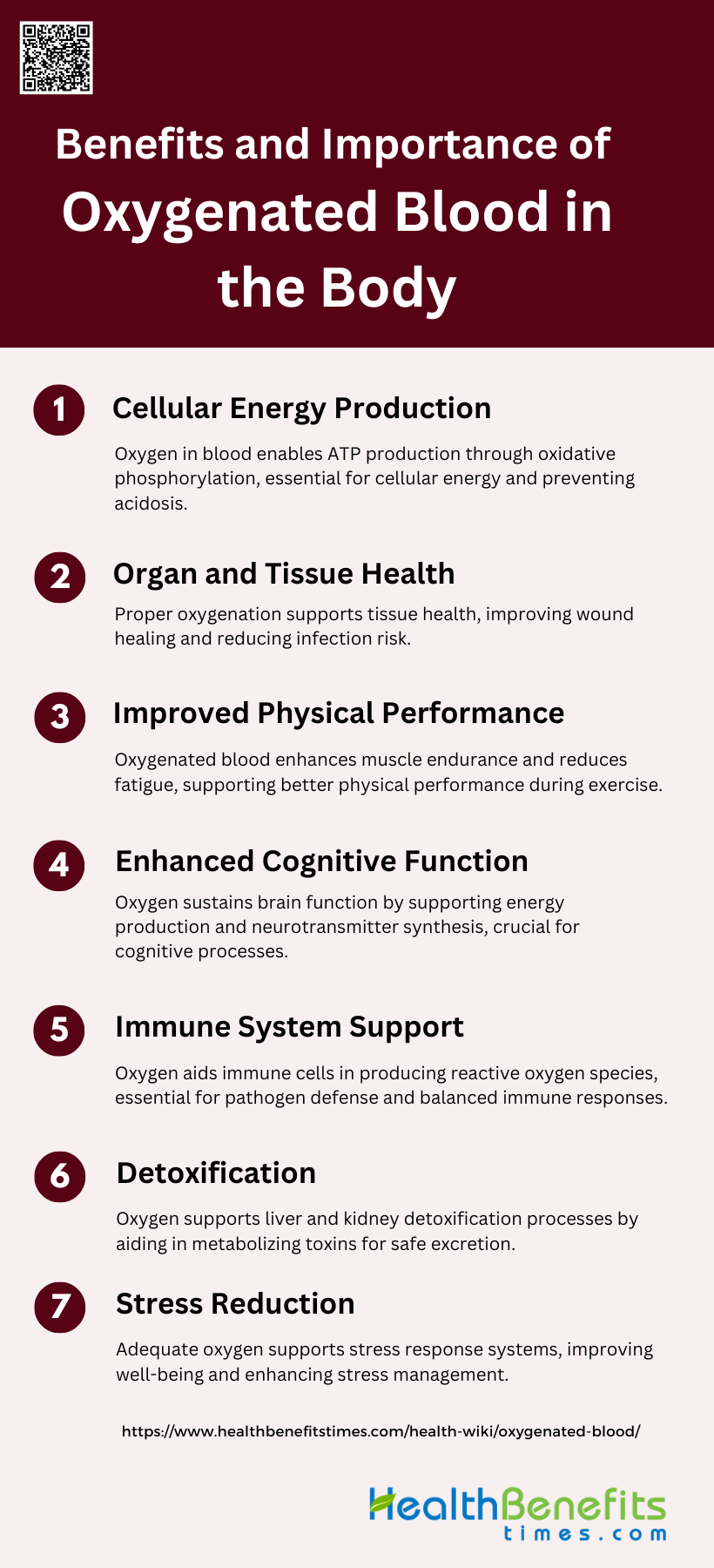
Benefits and importance of Oxygenated Blood in the Body
Oxygenated blood is crucial for various bodily functions and overall health. It supports cellular energy production, organ and tissue health, and enhances physical and cognitive performance. Below are the key benefits and importance of oxygenated blood in the body:
1. Cellular Energy Production
Oxygenated blood is crucial for cellular energy production, primarily through the process of oxidative phosphorylation in the mitochondria. Oxygen acts as the final electron acceptor in the electron transport chain, enabling the production of ATP, the energy currency of the cell. Without sufficient oxygen, cells resort to anaerobic metabolism, which is far less efficient and produces lactic acid as a byproduct, leading to acidosis and cellular damage. Therefore, maintaining adequate oxygen levels is essential for optimal cellular function and energy production.
2. Organ and Tissue Health
Optimal tissue oxygenation is vital for maintaining healthy organs and tissues. Adequate oxygen levels ensure that cells receive the necessary nutrients and energy to perform their functions effectively. Poor oxygenation can lead to tissue damage, impaired wound healing, and increased risk of infections. Factors such as age, lifestyle choices, and underlying medical conditions can affect tissue oxygenation, highlighting the importance of maintaining healthy habits to support microcirculation and tissue health.
3. Improved Physical Performance
Oxygenated blood enhances physical performance by improving the delivery of oxygen to muscles during exercise. This increased oxygen availability supports aerobic metabolism, which is more efficient than anaerobic pathways, thereby enhancing endurance and reducing fatigue. Athletes often use supplemental oxygen to boost performance, although the benefits and potential risks of hyperoxia are still under investigation. Ensuring adequate oxygenation during physical activity is crucial for optimal muscle function and performance.
4. Enhanced Cognitive Function
Oxygen is essential for brain function, as it supports the high metabolic demands of neural tissue. Adequate oxygenation ensures efficient energy production and neurotransmitter synthesis, which are critical for cognitive processes such as memory, attention, and problem-solving. Hypoxia, or reduced oxygen levels, can impair cognitive function and lead to symptoms such as confusion, dizziness, and even loss of consciousness in severe cases. Therefore, maintaining proper oxygen levels is crucial for cognitive health and function.
5. Immune System Support
Oxygenated blood plays a significant role in supporting the immune system. Oxygen is required for the production of reactive oxygen species (ROS) by immune cells, which are used to kill pathogens. However, excessive oxygen can lead to oxidative stress, which can damage immune cells and other tissues. Balancing oxygen levels is essential for optimal immune function, as both hypoxia and hyperoxia can have detrimental effects on the body’s ability to fight infections.
6. Detoxification
Oxygenated blood aids in the detoxification processes of the body by supporting the liver and kidneys, which are responsible for filtering and eliminating toxins. Oxygen is necessary for the metabolic processes that convert toxins into less harmful substances that can be excreted. Adequate oxygenation ensures that these organs function efficiently, thereby maintaining the body’s overall health and preventing the accumulation of harmful substances.
7. Stress Reduction
Proper oxygenation can help reduce stress by supporting the body’s physiological responses to stress. Oxygen is essential for the production of ATP, which is required for the functioning of stress-response systems, including the adrenal glands and the nervous system. Adequate oxygen levels can improve overall well-being, reduce the physical effects of stress, and enhance the body’s ability to cope with stressors. Engaging in activities that promote good oxygenation, such as regular exercise and deep breathing, can be beneficial for stress management.
Oxygenated Blood and Health
Factors that Affect Blood Oxygen Levels
Blood oxygen levels can be influenced by various factors, including altitude and respiratory diseases. At higher altitudes, the reduced atmospheric pressure leads to lower oxygen availability, which can result in hypoxemia, a condition characterized by low blood oxygen levels. Respiratory diseases such as chronic obstructive pulmonary disease (COPD) and asthma can also impair the lungs’ ability to oxygenate blood effectively. These conditions can cause inflammation and obstruction in the airways, reducing the efficiency of gas exchange. Maintaining optimal oxygen levels is crucial, as both hyperoxia (excess oxygen) and hypoxia (insufficient oxygen) can lead to severe health complications, including cell damage and cardiac arrest.
Methods to Measure Blood Oxygen Levels
Pulse oximetry is a non-invasive method commonly used to measure blood oxygen levels. This technique involves placing a sensor, typically on a fingertip or earlobe, which uses light absorption through the skin to estimate the oxygen saturation of hemoglobin in the blood. The device emits light wavelengths that are absorbed differently by oxygenated and deoxygenated blood, allowing it to calculate the percentage of oxygen saturation (SpO2). Pulse oximetry is widely used in clinical settings due to its simplicity and effectiveness in providing real-time monitoring of a patient’s oxygen status, which is essential for managing conditions that affect respiratory function.
Importance of Maintaining Healthy Blood Oxygen Levels
Maintaining healthy blood oxygen levels is vital for ensuring that tissues and organs receive adequate oxygen to function properly. Oxygen is crucial for cellular respiration, the process by which cells produce energy. Insufficient oxygen levels can lead to hypoxia, causing symptoms such as shortness of breath, confusion, and in severe cases, organ failure. Conversely, excessive oxygen levels can result in hyperoxia, which can cause oxidative stress and damage to cells. Therefore, precise regulation of blood oxygen levels is essential, particularly in critical care settings, to prevent complications and support overall health.
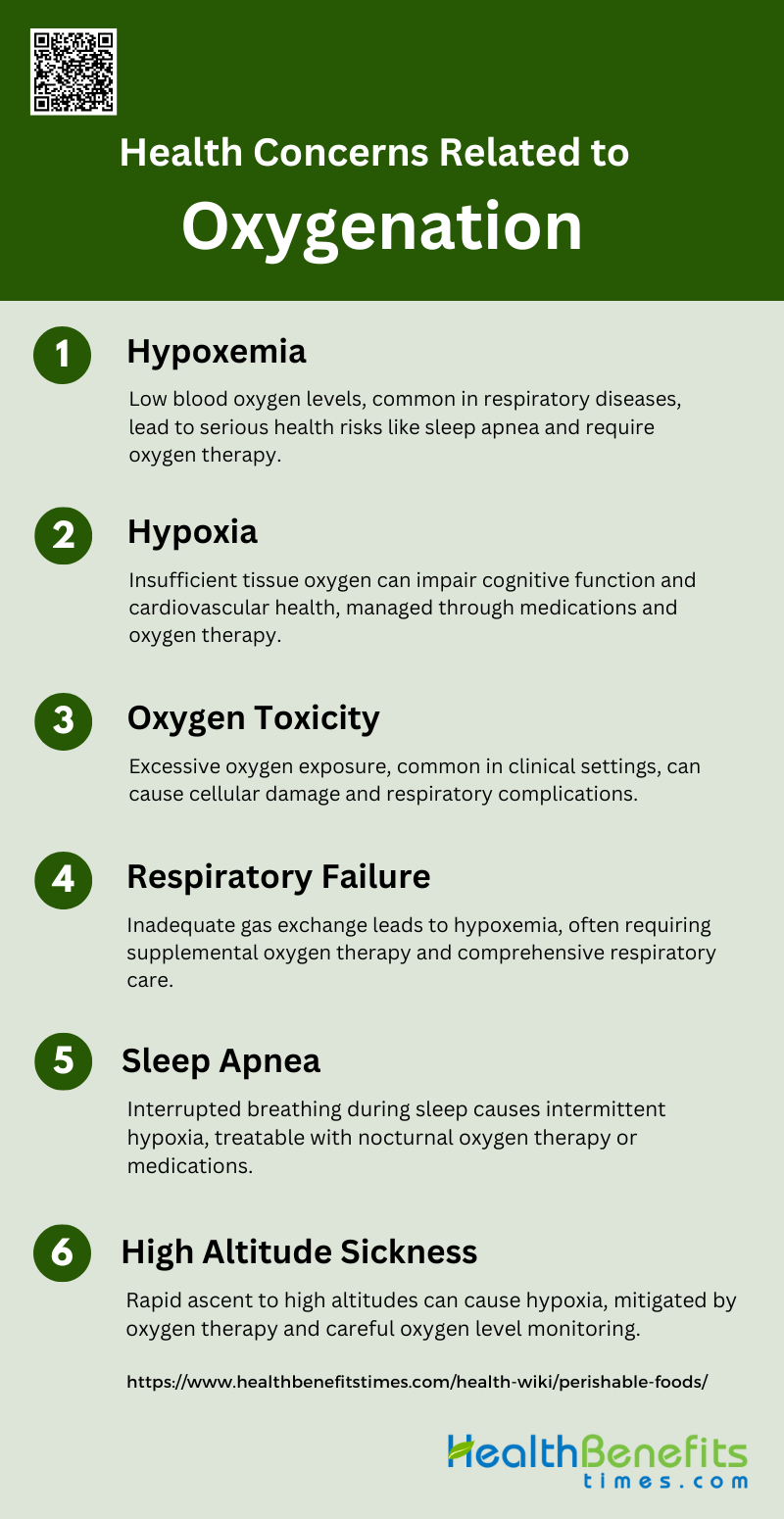
Health Concerns Related to Oxygenation
Oxygenation is a vital process for maintaining cellular function and overall health. Disruptions in oxygen levels can lead to a variety of serious health issues. Below is a list of health concerns related to oxygenation:
1. Hypoxemia
Hypoxemia refers to low levels of oxygen in the blood, which can lead to various health complications. It is particularly concerning for patients with chronic respiratory conditions such as chronic obstructive pulmonary disease (COPD) and pulmonary hypertension (PH). Studies have shown that patients with COPD experience significant nocturnal hypoxemia when exposed to high altitudes, which can exacerbate sleep apnea and other breathing disturbances. Similarly, PH patients also exhibit hypoxemia during altitude sojourns, which can be mitigated by nocturnal oxygen therapy. Chronic hypoxemia can trigger physiological responses such as increased erythropoietin levels and changes in red cell distribution width, which are markers of the body’s attempt to adapt to low oxygen levels.
2. Hypoxia
Hypoxia is a condition where there is insufficient oxygen reaching the tissues, which can result from hypoxemia. It can occur acutely, such as during high-altitude exposure, or chronically in conditions like sleep apnea and COPD. Hypoxia can lead to significant health issues, including impaired cognitive function and increased risk of cardiovascular diseases. Research indicates that hypoxia during sleep, especially at high altitudes, can exacerbate sleep-disordered breathing and reduce cerebral oxygenation, which can be partially improved with medications like acetazolamide. Additionally, hypoxia triggers a cascade of cellular responses, including the stabilization of hypoxia-inducible factors that regulate genes involved in angiogenesis and metabolism.
3. Oxygen Toxicity
Oxygen toxicity occurs when tissues are exposed to excessively high levels of oxygen, leading to cellular damage. This condition is particularly relevant in clinical settings where supplemental oxygen is administered to patients with respiratory failure or other critical conditions. Studies suggest that maintaining oxygen saturation within a specific range (89-93%) can improve survival rates in critically ill patients, such as those with COVID-19, while avoiding the risks associated with hyperoxemia. Oxygen toxicity can manifest as lung damage, central nervous system effects, and other systemic issues, emphasizing the need for careful monitoring and regulation of oxygen therapy.
4. Respiratory Failure
Respiratory failure is a severe condition where the respiratory system fails to maintain adequate gas exchange, leading to hypoxemia and hypercapnia. It can result from various underlying conditions, including COPD, pulmonary fibrosis, and acute respiratory distress syndrome (ARDS). Patients with chronic respiratory diseases residing at high altitudes are at increased risk of respiratory failure due to the lower oxygen availability. Supplemental oxygen therapy is a critical intervention for these patients, helping to stabilize oxygen levels and improve survival outcomes. However, the management of respiratory failure requires a comprehensive approach, including addressing the underlying cause and optimizing ventilatory support.
5. Sleep Apnea
Sleep apnea is a disorder characterized by repeated interruptions in breathing during sleep, leading to intermittent hypoxia and fragmented sleep. It is commonly observed in patients with COPD and those traveling to high altitudes. The condition can significantly impact quality of life and increase the risk of cardiovascular diseases. Nocturnal oxygen therapy has been shown to improve oxygen saturation and reduce the apnea-hypopnea index in patients with sleep apnea, particularly at high altitudes. Additionally, medications like acetazolamide can help improve cerebral oxygenation and reduce the severity of sleep apnea in these patients.
6. High Altitude Sickness
High altitude sickness, or acute mountain sickness (AMS), occurs when individuals ascend to high altitudes too quickly, leading to symptoms such as headache, nausea, and dizziness. It is primarily caused by hypoxia due to the reduced oxygen availability at high altitudes. Studies have shown that individuals with lower hypoxic chemosensitivity and irregular breathing patterns are more susceptible to AMS. Nocturnal oxygen therapy can help mitigate the effects of high altitude on oxygen saturation and reduce the incidence of AMS in susceptible individuals. Monitoring and managing oxygen levels are crucial for preventing and treating high altitude sickness.
How to boost Blood Oxygenation Naturally
Maintaining optimal blood oxygen levels is essential for overall health and well-being. Natural methods can effectively enhance oxygenation without the need for medical intervention. Below are several strategies to boost blood oxygenation naturally:
1. Practice Deep Breathing Exercises
Deep breathing exercises can significantly enhance blood oxygenation. A study involving patients who underwent cardiac surgery demonstrated that performing 30 deep breaths hourly, as opposed to 10, led to a notable increase in arterial oxygen tension and arterial oxygen saturation. Specifically, patients who practiced more frequent deep breathing had higher oxygen levels in their blood, which supports the implementation of such exercises to improve oxygenation, especially in the early postoperative period. This suggests that incorporating deep breathing exercises into daily routines can naturally boost blood oxygen levels.
2. Improve Your Posture
Maintaining good posture is essential for optimal lung function and blood oxygenation. Proper posture ensures that the lungs have enough space to expand fully, allowing for more efficient gas exchange. When the body is slouched, the diaphragm is compressed, which can restrict breathing and reduce oxygen intake. By sitting or standing up straight, the diaphragm can move more freely, enhancing lung capacity and improving oxygenation. This simple adjustment can make a significant difference in how well the body utilizes oxygen, contributing to overall better health and energy levels.
3. Exercise Regularly
Regular physical activity is a powerful way to enhance blood oxygenation. Exercise increases the body’s demand for oxygen, prompting the cardiovascular and respiratory systems to work more efficiently. A study on the effects of cocoa flavanol intake found that moderate-intensity exercise improved prefrontal cortex oxygenation, even under hypoxic conditions. This indicates that regular exercise, combined with a healthy diet, can significantly boost oxygen levels in the blood, supporting better brain function and overall health. Engaging in activities like walking, cycling, or swimming can help maintain high oxygen saturation levels.
4. Spend Time Outdoors
Spending time outdoors, especially in areas with fresh air, can significantly improve blood oxygenation. Natural environments typically have higher oxygen levels compared to indoor settings, which can be beneficial for respiratory health. Exposure to fresh air helps to clear the lungs and increases the amount of oxygen that enters the bloodstream. Additionally, outdoor activities often involve physical exercise, which further enhances oxygen intake and utilization. Therefore, incorporating outdoor time into daily routines can be a simple yet effective way to boost blood oxygen levels naturally.
5. Stay Hydrated
Staying well-hydrated is crucial for maintaining optimal blood oxygenation. Water is essential for the proper functioning of the body’s cells, including those involved in oxygen transport. Hydration helps to keep the blood thin, making it easier for the heart to pump oxygen-rich blood throughout the body. Dehydration, on the other hand, can lead to thicker blood, which can impede circulation and reduce oxygen delivery to tissues. Drinking adequate amounts of water daily ensures that the body’s systems operate efficiently, supporting better oxygenation and overall health.
6. Eat Oxygen-Rich Foods
Consuming foods rich in antioxidants and nutrients can enhance blood oxygenation. For instance, cocoa flavanols have been shown to improve endothelial function and increase prefrontal cortex oxygenation at rest and during moderate-intensity exercise. Foods like leafy greens, berries, and beets are high in antioxidants and nitrates, which can improve blood flow and oxygen delivery. Including these foods in your diet can help maintain high oxygen levels in the blood, supporting better cardiovascular health and overall well-being.
7. Avoid Smoking
Avoiding smoking is critical for maintaining healthy blood oxygen levels. Smoking has been shown to reduce oxygen saturation and impair lung function, leading to decreased oxygen delivery to tissues. Chronic smokers often experience lower oxygen levels and are at higher risk for respiratory diseases such as COPD. Quitting smoking can significantly improve lung capacity and oxygenation, leading to better overall health. For those struggling with smoking cessation, seeking support from healthcare professionals and engaging in activities like yoga can be beneficial.
FAQs
1. Can oxygenated blood be artificially enhanced or supplemented?
Yes, oxygenated blood can be supplemented in certain medical situations, such as during surgeries or in critically ill patients. Supplemental oxygen is often administered through nasal tubes, masks, or even hyperbaric oxygen therapy to increase blood oxygen levels. This is common in treating conditions like respiratory failure or carbon monoxide poisoning.
2. What are some common symptoms of low oxygen levels in the blood (hypoxemia)?
Symptoms of hypoxemia include shortness of breath, rapid breathing, headaches, confusion, restlessness, dizziness, and bluish tint to the skin (cyanosis). If severe, it can lead to unconsciousness or organ failure.
3.Can blood oxygen levels fluctuate during the day?
Yes, blood oxygen levels can fluctuate depending on activity levels, altitude, or underlying medical conditions. For example, oxygen levels may be lower when a person is sleeping or in high altitudes, especially if they have lung or heart conditions.
4. How does anemia affect blood oxygenation?
Anemia, a condition characterized by low levels of hemoglobin, reduces the blood’s ability to carry oxygen. Even if the lungs are functioning well, less oxygen may be transported to the body’s tissues due to the lower hemoglobin levels, leading to symptoms such as fatigue and weakness.
5. Can stress impact blood oxygen levels?
Yes, stress can impact breathing patterns, often leading to shallow breathing. This can reduce the amount of oxygen entering the lungs and, in turn, decrease blood oxygen levels. Relaxation techniques like deep breathing can help improve oxygenation during stress.
6. How can I monitor my blood oxygen levels at home?
You can monitor your blood oxygen levels at home using a pulse oximeter, a small device that clips onto your finger and provides a reading of your blood’s oxygen saturation (SpO2) within seconds. Normal readings typically range from 95-100%.
7. How does carbon monoxide affect blood oxygenation?
Carbon monoxide binds to hemoglobin more easily than oxygen, reducing the blood’s ability to carry oxygen. This can result in tissue hypoxia even if the lungs are taking in enough oxygen. Carbon monoxide poisoning is a medical emergency that requires immediate treatment.
8. Are there long-term effects of chronic low oxygen levels?
Chronic low oxygen levels can lead to long-term complications such as heart disease, high blood pressure in the lungs (pulmonary hypertension), cognitive decline, and damage to vital organs. Regular medical monitoring and oxygen therapy can help manage these risks.
9. What role does the spleen play in oxygenation?
The spleen helps filter old or damaged red blood cells and is part of the body’s oxygenation and immune system processes. It plays an indirect role by ensuring that red blood cells, which carry oxygen, remain healthy and functional.
10. Can poor air quality affect blood oxygenation?
Yes, poor air quality, particularly in areas with high pollution, can affect lung function and reduce the efficiency of oxygen exchange, leading to lower blood oxygen levels. Long-term exposure to pollutants can contribute to respiratory diseases and chronic low oxygenation.