Night blindness, or nyctalopia, is a condition characterized by difficulty seeing in low light or darkness. This visual impairment is often a symptom of underlying retinal disorders, such as retinitis pigmentosa or congenital stationary night blindness, where the rod cells in the retina fail to function properly. Night blindness can also result from vitamin A deficiency, which is crucial for the production of rhodopsin, a pigment in the eye that helps with vision in dim light. Individuals with night blindness may struggle with activities like driving at night or moving around in poorly lit environments. While it can be a congenital condition, it may also develop due to other health issues like diabetes or cataracts.
Symptoms of Night Blindness
Night blindness is a condition characterized by difficulty seeing in low light or darkness. This can significantly impact daily activities, especially those requiring vision in dim environments. Below are some common symptoms associated with night blindness:
1.Difficulty Seeing in Low Light: Patients with Congenital Stationary Night Blindness (CSNB) often report difficulty seeing in low light conditions, particularly those with CSNB1, who experience more severe night vision problems compared to CSNB2 patients.
2. Blurry or Cloudy Vision: Blurry or cloudy vision can be a symptom of night blindness, especially in conditions like retinitis pigmentosa, where there is atrophy of the pigment epithelium, leading to impaired vision in low light.
3. Sensitivity to Light: Enhanced sensitivity to light, particularly to short wavelengths, is a characteristic symptom in patients with the enhanced S cone syndrome, a form of night blindness.
4. Difficulty Adapting to Darkness: Patients with certain forms of stationary night blindness, such as those with mutations in genes like RHO or GNAT1, exhibit prolonged dark adaptation times, requiring much longer than normal to adjust to darkness.
5. Trouble Seeing Distant Objects: Night blindness can also manifest as trouble seeing distant objects, as seen in conditions like myopia, where the image of distant objects falls in front of the retina, exacerbating vision problems in low light.
6. Inability to See Stars: Inability to see stars is a common complaint among patients with CSNB1, who are blind at low light intensities equivalent to starlight but regain vision at higher light intensities.
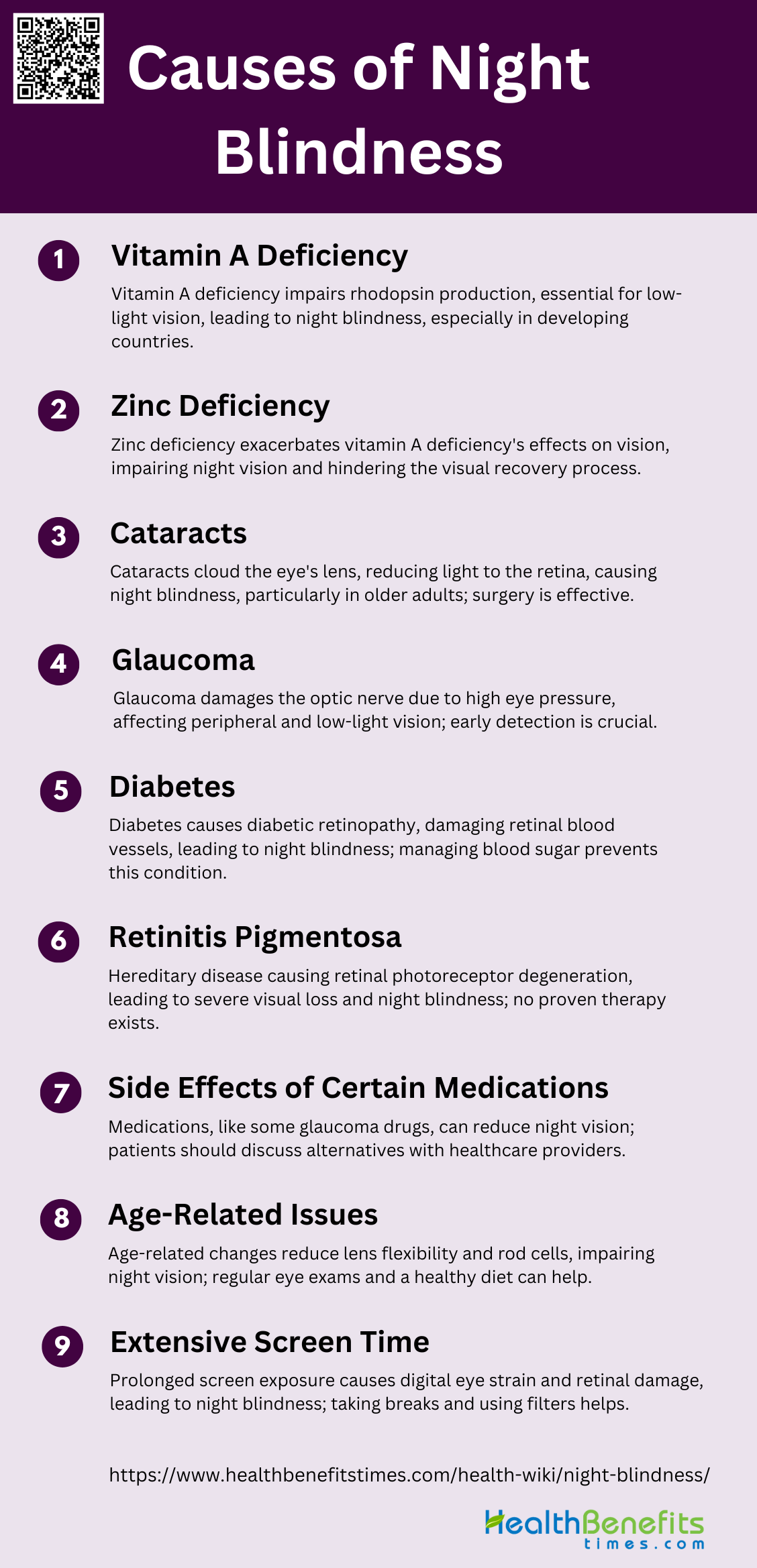
Causes of Night Blindness
Night blindness, or nyctalopia, can be caused by various underlying conditions affecting the eyes. These causes can range from nutritional deficiencies to genetic disorders. Below are some common causes of night blindness:
1. Vitamin A Deficiency
Vitamin A deficiency is a well-known cause of night blindness, primarily due to its critical role in the visual cycle. Vitamin A is essential for the production of rhodopsin, a pigment in the retina that helps the eye sees in low-light conditions. Acute deprivation of vitamin A impairs photoreceptor function, leading to poor vision under dim light conditions, known as night blindness. Chronic deficiency can result in more severe retinal dystrophies and photoreceptor cell death, which can lead to permanent blindness. This condition is particularly prevalent in developing countries, where vitamin A deficiency is a leading cause of preventable childhood blindness.
2. Zinc Deficiency
Zinc plays a crucial role in maintaining healthy vision, and its deficiency can exacerbate the effects of vitamin A deficiency, leading to night blindness. Zinc is involved in the metabolism of vitamin A and the formation of rhodopsin. Studies have shown that zinc supplementation can potentiate the effect of vitamin A in restoring night vision, particularly in individuals with low initial serum zinc concentrations. Zinc deficiency alone, however, may not be sufficient to cause night blindness but can significantly impair the visual recovery process when combined with vitamin A deficiency.
3. Cataracts
Cataracts, characterized by the clouding of the eye’s lens, are a significant cause of night blindness, especially in older adults. The clouded lens scatters light, reducing the amount of light that reaches the retina, which is particularly problematic in low-light conditions. Cataracts are the leading cause of blindness globally and are highly prevalent in both developing and developed countries. Surgical removal of cataracts is a common and effective treatment, but access to surgery can be limited in low-resource settings, making cataracts a persistent cause of night blindness.
4. Glaucoma
Glaucoma, a group of eye conditions that damage the optic nerve, can also lead to night blindness. The damage is often caused by abnormally high pressure in the eye, which can impair peripheral vision and make it difficult to see in low-light conditions. Glaucoma is one of the leading causes of blindness worldwide, and its prevalence is expected to increase with the aging population. Early detection and treatment are crucial to prevent the progression of the disease and associated night blindness.
5. Diabetes
Diabetes can lead to night blindness through diabetic retinopathy, a condition where high blood sugar levels cause damage to the blood vessels in the retina. This damage can lead to poor night vision and, in severe cases, complete blindness. Diabetic retinopathy is a significant cause of vision impairment and blindness globally, and its prevalence is increasing with the rise in diabetes cases. Managing blood sugar levels and regular eye examinations are essential to prevent and treat diabetic retinopathy.
6. Retinitis Pigmentosa
Retinitis pigmentosa (RP) is a group of hereditary eye diseases characterized by the progressive degeneration of retinal photoreceptors, leading to severe visual loss and night blindness. Symptoms often include poor night vision and constriction of peripheral vision, which progresses to affect central vision later in the disease course. Currently, there is no proven therapy for RP, although some studies have explored the potential benefits of vitamin A and fish oils in slowing the progression of the disease.
7. Side Effects of Certain Medications
Certain medications can cause night blindness as a side effect. For example, some drugs used to treat glaucoma, such as beta-blockers, can reduce the production of aqueous humor, leading to decreased night vision. Other medications, including some antipsychotics and antihistamines, can also impair night vision by affecting the eye’s ability to adapt to low-light conditions. It is essential for patients to discuss potential side effects with their healthcare providers and consider alternative treatments if night blindness becomes a significant issue.
8. Age-Related Issues
Age-related changes in the eye can lead to night blindness. As people age, the lens of the eye can become less flexible and more opaque, reducing the amount of light that reaches the retina. Additionally, the number of rod cells, which are responsible for vision in low-light conditions, decreases with age. Age-related macular degeneration (AMD) is another condition that can impair night vision, although it primarily affects central vision. Regular eye examinations and a healthy diet rich in vitamins and antioxidants can help mitigate some of these age-related changes.
9. Extensive Screen Time
Extensive screen time can contribute to night blindness by causing digital eye strain and disrupting the normal functioning of the retina. Prolonged exposure to blue light from screens can lead to phototoxicity, which damages the retinal cells and impairs night vision. Additionally, staring at screens for extended periods can reduce the blink rate, leading to dry eyes and further exacerbating vision problems. Taking regular breaks, using blue light filters, and maintaining proper screen ergonomics can help reduce the risk of night blindness associated with extensive screen time.
Diagnosis of Night Blindness
Diagnosing night blindness involves a comprehensive eye examination and medical history review. Various tests may be conducted to determine the underlying cause and extent of the condition. Below are some common methods used in the diagnosis of night blindness:
1. Initial Consultation with an Ophthalmologist
During the initial consultation for night blindness, an ophthalmologist will gather a comprehensive medical history and inquire about the patient’s symptoms, including the onset and severity of night vision difficulties. The ophthalmologist will also ask about any relevant family history of eye disorders, previous surgeries, and overall health conditions that might contribute to night blindness, such as vitamin A deficiency or genetic disorders. This initial step is crucial for identifying potential underlying causes and determining the appropriate diagnostic tests to confirm the diagnosis and guide treatment.
2. Comprehensive Eye Exam
A comprehensive eye exam is essential for diagnosing night blindness. This exam typically includes visual acuity tests, slit-lamp examination, and fundoscopy to assess the overall health of the retina and other structures of the eye. Special attention is given to the rod cells in the retina, which are responsible for vision in low-light conditions. The ophthalmologist may also perform dark adaptation tests to evaluate how well the eyes adjust from bright to dim lighting. These tests help in identifying any abnormalities in the retina that could be causing night blindness, such as retinitis pigmentosa or congenital stationary night blindness.
3. Possible Additional Tests
Additional tests may be necessary to pinpoint the exact cause of night blindness. Electroretinography (ERG) is a key diagnostic tool that measures the electrical responses of the rod and cone cells in the retina to light stimuli, helping to identify functional impairments. Blood tests to measure serum vitamin A levels are also important, as vitamin A deficiency is a common cause of night blindness. Imaging tests, such as optical coherence tomography (OCT), can provide detailed images of the retina’s structure, aiding in the diagnosis of retinal diseases. These tests collectively help in forming a comprehensive understanding of the patient’s condition and guiding effective treatment strategies.
Treatment Options for Night Blindness
Treating night blindness depends on its underlying cause and may involve various approaches. These treatments can range from dietary changes to medical interventions. Below are some common treatment options for night blindness:
1. Vitamin A Supplementation
Vitamin A supplementation has been shown to significantly reduce the incidence of night blindness, particularly in populations with high rates of vitamin A deficiency. A study conducted in Nepal demonstrated that weekly supplementation with vitamin A reduced the incidence of night blindness during pregnancy from 10.7% to 6.7% among the participants. Additionally, the study found that women who adhered strictly to the supplementation regimen experienced a 67% reduction in verified night blindness. However, while vitamin A supplementation markedly reduced the incidence, it did not completely eliminate night blindness, suggesting that higher doses or additional nutrients might be necessary for complete prevention.
2. Reducing Screen Time
Reducing screen time can help alleviate symptoms of night blindness, particularly in individuals who experience eye strain or digital eye fatigue. Prolonged exposure to screens can lead to digital eye strain, which exacerbates difficulties in low-light conditions. Although specific studies on reducing screen time and its direct impact on night blindness are limited, it is generally recommended to follow the 20-20-20 rule: every 20 minutes, take a 20-second break and look at something 20 feet away. This practice can help reduce eye strain and improve overall eye health, potentially mitigating some symptoms associated with night blindness.
3. Prescription Eyeglasses or Contact Lenses
Prescription eyeglasses or contact lenses can correct refractive errors that may contribute to night blindness. Conditions such as myopia (nearsightedness) can worsen night vision, making it difficult to see in low-light conditions. By correcting these refractive errors, prescription lenses can improve overall visual acuity and contrast sensitivity, thereby enhancing night vision. While eyeglasses or contact lenses do not cure night blindness, they can significantly improve the quality of vision in low-light environments, making daily activities such as driving at night safer and more manageable.
4. Medications for Underlying Conditions
Medications that address underlying conditions, such as diabetes, can play a crucial role in managing night blindness. For instance, controlling blood sugar levels in diabetic patients can prevent or slow the progression of diabetic retinopathy, a condition that can impair night vision. Similarly, managing other health issues like hypertension or vitamin deficiencies through appropriate medications can help improve overall eye health and reduce symptoms of night blindness. Effective management of these underlying conditions is essential for maintaining good night vision and preventing further deterioration.
5. Cataract Surgery
Cataract surgery is a highly effective treatment for night blindness caused by cataracts. Cataracts, characterized by the clouding of the eye’s lens, can significantly impair vision, especially in low-light conditions. Surgery involves the removal of the cloudy lens and its replacement with an artificial intraocular lens, which restores transparency and improves vision. While cataract surgery is generally safe and effective, it carries risks of complications such as infection or irreversible vision loss. Nonetheless, it remains the most effective method for treating cataract-induced night blindness, offering significant improvements in visual function and quality of life.
6. Avoid Using Brighter Lighting at Home
Using dimmer lighting at home can help individuals with night blindness adapt better to low-light conditions. Bright lights can cause glare and reduce contrast sensitivity, making it more challenging for those with night blindness to see clearly. By using softer, dimmer lighting, individuals can reduce glare and improve their ability to see in low-light environments. Additionally, using task lighting that focuses light where it is needed can help minimize the overall brightness in a room, making it easier for individuals with night blindness to navigate their surroundings comfortably.
7. Avoiding Driving at Night
Avoiding driving at night is a practical measure for individuals with night blindness to ensure their safety and the safety of others. Night blindness can significantly impair the ability to see road signs, pedestrians, and other vehicles in low-light conditions, increasing the risk of accidents. By limiting driving to daylight hours, individuals with night blindness can avoid the challenges posed by reduced visibility and glare from oncoming headlights. This precautionary measure helps prevent accidents and ensures that individuals with night blindness can travel safely and confidently.
8. Herbal Supplements
Herbal supplements containing antioxidants and anti-inflammatory compounds may offer potential benefits for managing night blindness. Certain medicinal plants and natural products have been traditionally used to improve eye health and treat conditions like cataracts, which can contribute to night blindness. For example, plant-based antioxidants can help reduce oxidative stress, a key factor in the development of age-related eye conditions. While more research is needed to confirm the efficacy of specific herbal supplements, incorporating antioxidant-rich herbs into the diet may support overall eye health and alleviate some symptoms of night blindness.
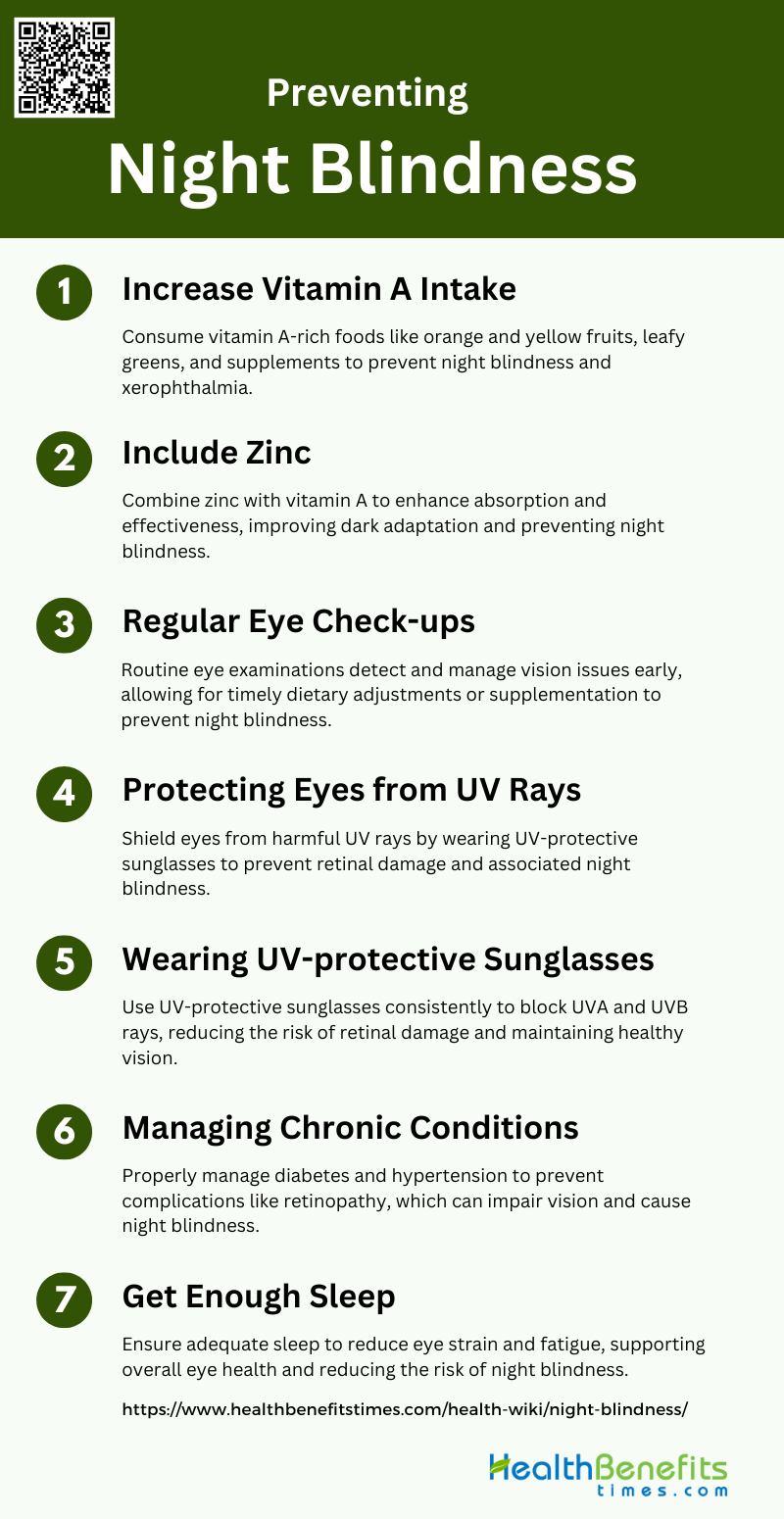
Preventing Night Blindness
Preventing night blindness involves adopting healthy lifestyle habits and addressing potential risk factors early. By taking proactive measures, individuals can reduce their chances of developing this condition. Key preventative strategies include:
1. Increase Vitamin A Intake
Increasing vitamin A intake is crucial for preventing night blindness, especially in populations with endemic vitamin A deficiency. Consuming orange and yellow fruits and vegetables, as well as leafy greens, can significantly boost vitamin A levels. Studies have shown that vitamin A supplementation reduces the incidence of night blindness in pregnant women and children. For instance, in Nepal, vitamin A supplementation during pregnancy reduced the incidence of night blindness from 10.7% to 6.7%. Additionally, vitamin A is essential for maintaining healthy vision and preventing xerophthalmia, a severe form of vitamin A deficiency that can lead to blindness.
2. Include Zinc
Zinc plays a complementary role in preventing night blindness, particularly when combined with vitamin A. Zinc deficiency can impair dark adaptation, a key factor in night blindness. Research in Nepal demonstrated that zinc supplementation, when combined with vitamin A, significantly improved night vision in pregnant women with low initial serum zinc levels. Zinc enhances the effectiveness of vitamin A by improving its absorption and utilization in the body, thereby helping to restore night vision more effectively than vitamin A alone.
3. Regular Eye Check-ups
Regular eye check-ups are essential for early detection and management of night blindness and other vision-related issues. Routine examinations can help identify vitamin A deficiency and other underlying conditions that may contribute to night blindness. Early intervention through dietary adjustments or supplementation can prevent the progression of vision problems. Regular check-ups also provide an opportunity for healthcare providers to educate patients on the importance of maintaining adequate vitamin A levels and other preventive measures.
4. Protecting Eyes from UV Rays
Protecting eyes from UV rays is another important strategy to prevent night blindness and other eye conditions. Prolonged exposure to UV rays can damage the retina and exacerbate vision problems. Wearing UV-protective sunglasses can shield the eyes from harmful rays and reduce the risk of retinal damage. This preventive measure is particularly important for individuals who spend a lot of time outdoors, as it helps maintain overall eye health and prevents conditions that could lead to night blindness.
5. Wearing UV-protective Sunglasses
Wearing UV-protective sunglasses is a simple yet effective way to protect the eyes from harmful ultraviolet rays. These sunglasses block out 99-100% of both UVA and UVB radiation, reducing the risk of retinal damage and other eye conditions that can contribute to night blindness. Consistent use of UV-protective sunglasses can help maintain healthy vision and prevent the deterioration of night vision, especially in individuals who are frequently exposed to sunlight.
6. Managing Chronic Conditions
Managing chronic conditions such as diabetes and hypertension is crucial for preventing night blindness. These conditions can lead to complications that affect vision, including diabetic retinopathy and hypertensive retinopathy. Proper management through medication, lifestyle changes, and regular monitoring can help prevent these complications and maintain healthy vision. Additionally, addressing underlying health issues can improve overall well-being and reduce the risk of developing night blindness.
7. Get Enough Sleep
Getting enough sleep is essential for overall eye health and can help prevent night blindness. Adequate sleep allows the eyes to rest and recover, reducing strain and fatigue that can impair vision. Chronic sleep deprivation can lead to various health issues, including problems with night vision. Ensuring sufficient rest each night supports the body’s natural repair processes and helps maintain optimal eye function, thereby reducing the risk of night blindness.
Living with Night Blindness
Living with night blindness requires adapting to various challenges and finding ways to maintain safety and independence in low-light conditions. By employing specific strategies and utilizing available resources, individuals can effectively manage their daily lives. Key aspects of living with night blindness include:
1. Coping Strategies for Daily Life
Living with night blindness requires a range of coping strategies to manage daily activities effectively. Individuals often rely on adaptive techniques such as using alternative senses, optimizing their living environment, and employing technology to navigate their surroundings safely. For instance, visually impaired individuals in Iran have been found to use strategies like trusting others, enhancing emotional intelligence, and leveraging their memory to perform daily tasks. Additionally, proactive coping, reflective coping, and strategic planning have been positively correlated with better quality of life among those with visual impairments. These strategies help maintain autonomy and improve overall well-being.
2. Support Groups and Resources
Support groups and resources play a crucial role in helping individuals with night blindness manage their condition. Engaging with support groups provides emotional and social support, which is essential for coping with the uncertainties and challenges associated with visual impairments. For example, ex-Service personnel in the UK have benefited from being members of organizations like Blind Veterans UK, which offer a sense of community and practical assistance. Moreover, interactions with healthcare professionals and other social support systems have been identified as significant factors in managing the emotional and practical issues related to retinitis pigmentosa. These resources help individuals feel less isolated and more empowered to handle their condition.
3. Adaptive Technologies and Tools
Adaptive technologies and tools are indispensable for individuals living with night blindness, enabling them to perform daily activities more independently. Technologies such as low vision aids, screen readers, and specialized lighting can significantly enhance the quality of life for those with visual impairments. In Iran, visually impaired individuals have reported using various technological aids to cope with their daily living activities. Additionally, integrating low vision aids into daily routines has been a common strategy among younger ex-Service personnel in the UK, helping them adjust to their vision loss. These tools not only facilitate better navigation and task performance but also contribute to greater independence and confidence.