Mucous membranes are specialized layers of epithelial tissue that line various body cavities and organs exposed to the external environment. These moist, protective surfaces are found in areas such as the respiratory tract, gastrointestinal tract, urogenital tract, and the inner surface of eyelids. Mucous membranes play a crucial role in the body’s defense system by acting as a physical barrier against pathogens and harmful substances. They secrete mucus, a thick, slippery fluid that traps particles and microorganisms, preventing them from entering deeper tissues. Additionally, mucous membranes contain immune cells and antibodies that help fight off infections. These membranes are also involved in various physiological processes, including absorption of nutrients in the intestines and facilitating gas exchange in the lungs. Their unique structure and functions make mucous membranes an essential component of the body’s innate immune system and overall health.
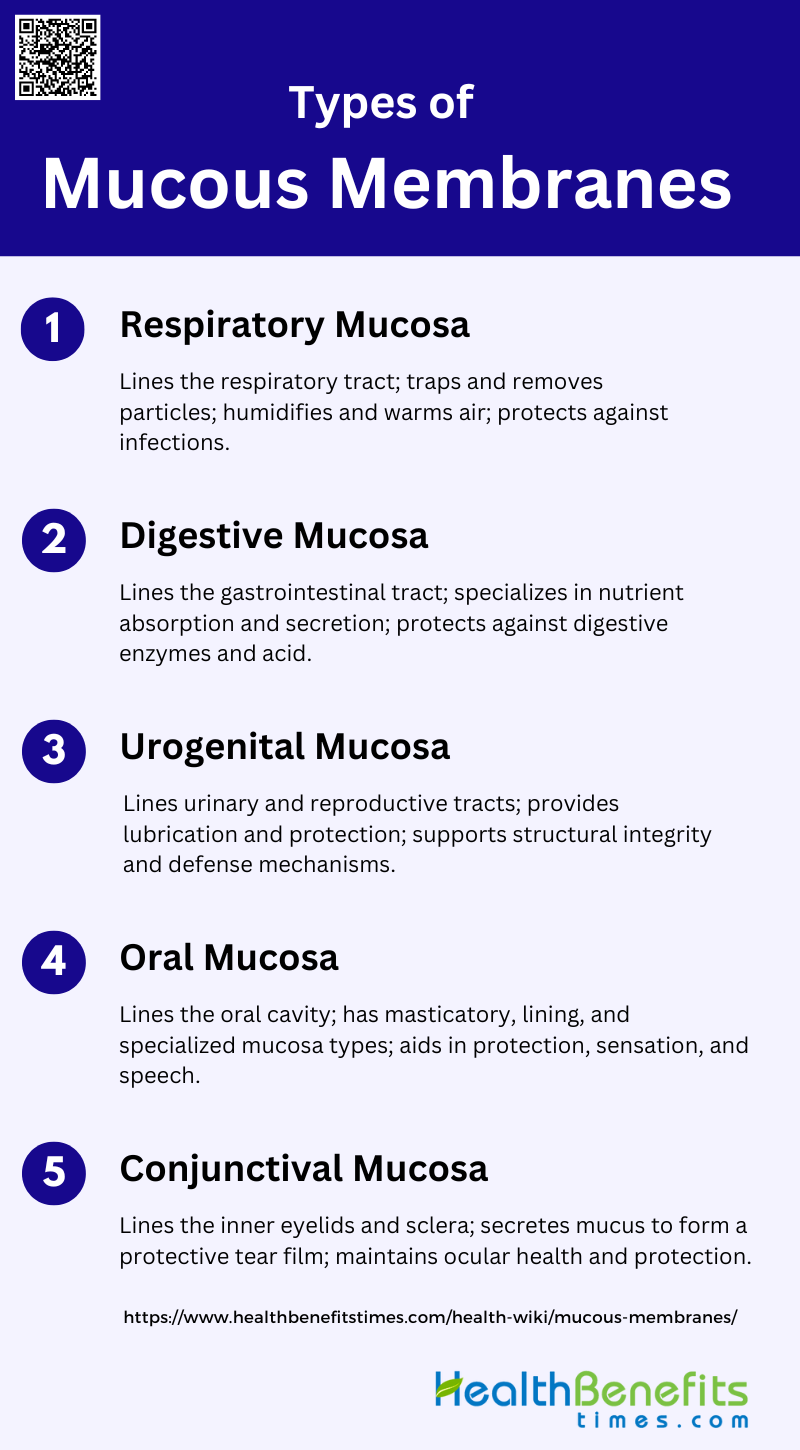
Types of Mucous Membranes
Mucous membranes, also known as mucosae, are linings of mostly endodermal origin, covered in epithelium, and are involved in absorption and secretion. They line various cavities in the body and surround internal organs. Here are the different types of mucous membranes:
1. Respiratory Mucosa
The respiratory mucosa lines the respiratory tract, including the nasal cavity, trachea, and bronchi. It consists of a pseudostratified ciliated columnar epithelium with goblet cells that secrete mucus. This mucus traps dust, pathogens, and other particles, which are then moved out of the respiratory tract by the cilia. The underlying lamina propria contains blood vessels, nerves, and immune cells, providing structural support and defense mechanisms. The respiratory mucosa plays a crucial role in humidifying and warming inhaled air, as well as in protecting the respiratory system from infections and environmental pollutants.
2. Digestive Mucosa
The digestive mucosa lines the gastrointestinal tract, from the mouth to the anus, and is specialized for nutrient absorption and secretion. It consists of an epithelial layer, a lamina propria, and a muscularis mucosae. The epithelial layer varies in structure along the tract, from stratified squamous epithelium in the esophagus to simple columnar epithelium in the stomach and intestines. Goblet cells within the epithelium secrete mucus to protect the lining from digestive enzymes and acidic conditions. The lamina propria contains blood vessels, lymphatics, and immune cells, facilitating nutrient absorption and immune responses.
3. Urogenital Mucosa
The urogenital mucosa lines the urinary and reproductive tracts, including the urethra, bladder, vagina, and cervix. It consists of a stratified squamous epithelium in the vagina and cervix, and a transitional epithelium in the bladder and urethra. Goblet cells and other mucus-secreting cells are present, providing lubrication and protection against pathogens. The underlying connective tissue contains blood vessels, nerves, and immune cells, supporting the mucosa’s structural integrity and defense mechanisms. The urogenital mucosa plays a vital role in protecting against infections and facilitating reproductive functions.
4. Oral Mucosa
The oral mucosa lines the oral cavity and consists of three types: masticatory, lining, and specialized mucosa. The masticatory mucosa, found in the gingivae and hard palate, is tough and keratinized, providing resistance to mechanical stress. The lining mucosa, present in the lips, cheeks, and soft palate, is flexible and non-keratinized, allowing for movement and flexibility. The specialized mucosa on the dorsum of the tongue contains taste buds and a mix of masticatory and lining features. The oral mucosa’s structure reflects its functions in protection, sensation, and facilitating speech and mastication.
5. Conjunctival Mucosa
The conjunctival mucosa lines the inner surface of the eyelids and covers the sclera. It consists of a stratified columnar epithelium with goblet cells that secrete mucus, forming a protective tear film over the eye. This mucus layer helps to trap and remove debris, pathogens, and other particles, while also keeping the eye moist. The underlying connective tissue contains blood vessels, nerves, and immune cells, providing structural support and defense mechanisms. The conjunctival mucosa plays a crucial role in maintaining ocular health and protecting the eye from infections and environmental irritants.
Structure of Mucous Membranes
Mucous membranes consist of an epithelial layer, a lamina propria, and sometimes a muscularis mucosae. These layers work together to protect the body from pathogens and facilitate the absorption and secretion of substances. The structure of mucous membranes can be categorized as follows:
1. Epithelial Layer
The epithelial layer of the mucous membrane is a single layer of columnar cells that serves as the first line of defense against external agents. This layer includes various cell types such as enterocytes, goblet cells, endocrine cells, Paneth cells, and intraepithelial lymphocytes, each contributing to the overall function of the epithelium. The epithelial cells are tightly bound by junctional complexes, including tight junctions, intermediate junctions, and desmosomes, which regulate the paracellular space and maintain the integrity of the barrier. This layer is crucial for nutrient absorption, secretion of mucus and hormones, and protection against pathogens.
2. Lamina Propria
The lamina propria is a highly dynamic and complex layer situated between the epithelial layer and the muscularis mucosae. It is rich in immune cells, including plasma cells, lymphocytes, macrophages, eosinophils, and dendritic cells, which play a significant role in the mucosal immune response. This layer also contains blood and lymph vessels, nerve varicosities, and fibroblasts, contributing to its structural and functional diversity. The lamina propria acts as a communication hub, facilitating interactions between immune cells and epithelial cells, and is involved in processes such as cellular trafficking, immune response regulation, and tissue repair.
3. Muscularis Mucosae
The muscularis mucosae is the innermost layer of the mucosa, composed of smooth muscle fibers. This layer is responsible for the local movement of the mucous membrane, which aids in the expulsion of glandular secretions and enhances contact between the mucosa and luminal contents. The muscularis mucosae also plays a role in maintaining the structural integrity of the mucosa and facilitating the absorption and secretion processes. Changes in the muscularis mucosae, such as thinning and myocyte dissociation, have been observed with aging, indicating its importance in maintaining mucosal function and integrity.
Function of Mucous Membranes
Mucous membranes are essential components of the body’s defense and maintenance systems. They line various cavities and canals, providing protection, hydration, lubrication, and sensory functions. Below are the key functions of mucous membranes:
1. Protection
Mucous membranes serve as a critical barrier against pathogens by forming a physical and biochemical shield. The mucus layer, composed of glycoproteins called mucins, is secreted by goblet cells and covers mucosal surfaces such as the gastrointestinal (GI) tract, lungs, and urogenital tract. This layer traps and neutralizes pathogens, toxins, and environmental irritants, preventing them from penetrating the epithelial cells and causing infections. Additionally, the mucus barrier is selectively permeable, allowing essential nutrients and gases to pass through while blocking harmful substances. Disruptions in mucin production or mucus layer integrity can lead to increased susceptibility to infections and inflammatory diseases.
2. Moisturization
Mucous membranes play a vital role in keeping tissues hydrated by maintaining a moist environment. The mucus layer, rich in water and glycoproteins, ensures that the epithelial surfaces remain lubricated and hydrated, which is essential for their proper function. This hydration is crucial for the mucosal surfaces in the eyes, lungs, and GI tract, where dryness can lead to irritation and impaired function. The continuous secretion of mucus by goblet cells helps to replenish and maintain this moist environment, ensuring that the tissues do not dry out and remain healthy.
3. Lubrication
The lubrication provided by mucous membranes is essential for the smooth passage of food and waste through the gastrointestinal tract. Mucins, the primary components of mucus, form a gel-like layer that reduces friction and facilitates the movement of the food bolus and stool. This lubrication is not only crucial for digestion but also for protecting the epithelial cells from mechanical damage caused by the passage of solid particles. Inadequate mucus production or altered mucin composition can lead to conditions such as constipation or intestinal blockages, highlighting the importance of mucus in maintaining gastrointestinal health.
4. Sensory Functions
Mucous membranes also play a significant role in detecting environmental changes and initiating appropriate responses. The mucus layer contains various receptors and signaling molecules that can sense changes in the external environment, such as the presence of pathogens or toxins. These sensory functions are crucial for triggering immune responses and maintaining homeostasis. For example, in the gut, the mucus layer interacts with the microbiota and immune cells to regulate immune tolerance and inflammation. This sensory capability ensures that the body can quickly respond to potential threats and maintain a balanced internal environment.
Locations of Mucous Membranes in the Body
Mucous membranes are found throughout the body, lining various cavities and canals that are exposed to the external environment. These membranes play crucial roles in protection, hydration, and sensory functions. Below are the primary locations of mucous membranes in the body:
1. Respiratory System
Mucous membranes in the respiratory system play a crucial role in protecting the body from inhaled pathogens and particles. These membranes line the nasal passages, trachea, and bronchi, providing a barrier that traps and expels foreign substances. Histological studies have shown that the trachea’s mucous membrane contains clusters of lymphocytes and plasma cells within the stroma of the tracheal glands, as well as lymphocytic sheaths around excretory ducts. Additionally, a continuous subepithelial layer of lymphoid cells is present in the trachea, contributing to the immune defense mechanisms of the respiratory tract.
2. Digestive System
In the digestive system, mucous membranes are essential for both protection and absorption. These membranes line the mouth, esophagus, stomach, and intestines, secreting mucus to facilitate the passage of food and protect the underlying tissues from digestive enzymes and acidic conditions. The upper part of the esophagus features a continuous subepithelial layer of lymphoid cells, while the intestinal crypts contain lymphocytes, which play a role in immune surveillance. The presence of interepithelial lymphocytes and lymphoid nodules further enhances the protective function of the digestive mucous membranes.
3. Urogenital System
The mucous membranes of the urogenital system are vital for maintaining a barrier against infections and facilitating the passage of urine and reproductive fluids. These membranes line the urinary tract, including the urethra and bladder, as well as the reproductive organs. Histological analysis has revealed that the urinary system’s mucous membranes share similar protective structures with those of the respiratory and digestive systems, including interepithelial lymphocytes and lymphoid nodules. These features help to prevent the invasion of pathogens and maintain the health of the urogenital tract.
4. Sensory Organs
Mucous membranes in sensory organs, such as the eyes, nose, and mouth, are crucial for protecting these delicate structures from environmental hazards. In the nasal passages, the mucous membrane traps dust and microbes, preventing them from reaching the lungs. The eyes are protected by the conjunctival mucous membrane, which secretes mucus to keep the surface moist and free from debris. Similarly, the oral mucous membrane helps to protect the mouth from mechanical damage and infection. These membranes are equipped with immune cells, such as lymphocytes, to provide an additional layer of defense.
Common conditions affecting mucous membranes
Mucous membranes can be affected by various conditions, impacting their ability to protect and maintain the body’s health. These conditions can range from infections to chronic diseases, each presenting unique challenges. Below are some common conditions affecting mucous membranes:
1. Candidiasis (Yeast Infection)
Candidiasis, commonly known as a yeast infection, is caused by the overgrowth of Candida species, particularly Candida albicans. This condition often affects the mucous membranes of the mouth, leading to oral thrush, characterized by white patches on the tongue and inner cheeks. It can cause discomfort, pain, and difficulty swallowing. Risk factors include immunosuppression, diabetes, and the use of broad-spectrum antibiotics. Effective management involves antifungal medications and addressing underlying conditions to prevent recurrence.
2. Canker Sores
Canker sores, or aphthous stomatitis, are small, painful ulcers that appear on the mucous membranes inside the mouth. They are typically round or oval with a white or yellow center and a red border. The exact cause is unknown, but factors such as stress, minor mouth injuries, acidic foods, and certain medical conditions can trigger their development. While canker sores usually heal on their own within one to two weeks, treatments like topical corticosteroids and antimicrobial mouthwashes can help alleviate pain and speed up healing.
3. Herpes Simplex Virus Infections
Herpes simplex virus (HSV) infections are common viral infections that affect the mucous membranes, particularly in the oral and genital regions. HSV-1 typically causes oral herpes, presenting as cold sores or fever blisters around the mouth. These lesions are painful and can recur periodically. The virus remains dormant in nerve cells and can be reactivated by factors such as stress, illness, or sun exposure. Antiviral medications like acyclovir can reduce the severity and frequency of outbreaks.
4. Oral Lichen Planus
Oral lichen planus is a chronic inflammatory condition that affects the mucous membranes inside the mouth. It presents as white, lacy patches or red, swollen tissues, and can cause pain or discomfort, especially when eating or drinking. The exact cause is unknown, but it is believed to be an autoimmune disorder. Management includes topical corticosteroids to reduce inflammation and pain, and regular monitoring to check for potential malignant transformation.
5. Mucositis
Mucositis is the painful inflammation and ulceration of the mucous membranes lining the digestive tract, commonly occurring as a side effect of chemotherapy and radiation therapy in cancer patients. It can lead to severe pain, difficulty eating and swallowing, and an increased risk of infection. Management strategies include good oral hygiene, pain relief medications, and protective coatings for the mucous membranes. Preventive measures such as cryotherapy and the use of growth factors can also be beneficial.
6. Mucous Membrane Pemphigoid (MMP)
Mucous membrane pemphigoid (MMP) is a group of chronic autoimmune blistering diseases that predominantly affect the mucous membranes, including the oral, ocular, nasal, and genital areas. It is characterized by the formation of blisters and erosions due to autoantibodies targeting components of the basement membrane zone. MMP can lead to significant morbidity due to scarring and functional impairment. Treatment involves immunosuppressive therapies to control the autoimmune response and prevent disease progression.
7. Behcet’s Disease
Behcet’s disease is a rare, chronic inflammatory disorder that affects multiple systems, including the mucous membranes. It is characterized by recurrent oral and genital ulcers, uveitis, and skin lesions. The exact cause is unknown, but it is believed to involve an abnormal immune response. Management includes immunosuppressive and anti-inflammatory medications to control symptoms and prevent complications. Regular monitoring and a multidisciplinary approach are essential for managing this complex condition.
8. Burning Mouth Syndrome
Burning mouth syndrome is a chronic condition characterized by a burning sensation in the mouth, often affecting the tongue, lips, and palate. The cause is often idiopathic, but it can be associated with nutritional deficiencies, hormonal changes, and psychological factors. Patients may also experience dry mouth and altered taste. Management focuses on symptom relief through medications such as antidepressants, anticonvulsants, and topical treatments, as well as addressing any underlying conditions.
How to Maintain Healthy Mucous Membranes
Maintaining healthy mucous membranes is essential for overall well-being as they play a crucial role in protecting the body from pathogens and keeping tissues moist. Proper care involves a combination of hydration, nutrition, and lifestyle habits. Here are some effective strategies to ensure your mucous membranes remain in optimal condition:
1. Stay Hydrated
Maintaining adequate hydration is crucial for the health of mucous membranes. Proper hydration ensures that the mucus remains at an optimal consistency, which is essential for trapping and expelling pathogens and debris. Dehydration can lead to thicker mucus, which is less effective at performing these protective functions. Additionally, hydration supports the overall function of epithelial cells that produce mucus, thereby maintaining the integrity of the mucosal barrier.
2. Optimize Your Diet
A balanced diet rich in essential nutrients supports the health of mucous membranes. Nutrients such as vitamins A, C, and E, along with omega-3 fatty acids, play a significant role in maintaining the integrity and function of mucosal barriers. These nutrients help in the production and maintenance of mucus and support the immune system in defending against pathogens. A diet that includes a variety of fruits, vegetables, and healthy fats can contribute to the resilience of mucous membranes .
3. Supplement Wisely
Certain supplements can enhance the health of mucous membranes. Probiotics, for instance, help maintain a balanced microbiota, which is crucial for preventing infections and inflammation. Supplements like zinc and vitamin D also support mucosal health by enhancing immune function and promoting the repair of epithelial tissues. However, it is important to consult with a healthcare provider before starting any new supplement regimen to ensure it is appropriate for your individual health needs.
4. Maintain a Healthy Environment
The environment plays a significant role in the health of mucous membranes. Exposure to pollutants, allergens, and irritants can compromise the mucosal barrier and lead to inflammation and infection. Maintaining a clean living space, using air purifiers, and avoiding exposure to tobacco smoke and other harmful substances can help protect mucous membranes. Additionally, ensuring adequate humidity levels can prevent the drying out of mucosal surfaces, which is essential for their protective functions.
5. Practice Good Hygiene
Good hygiene practices are essential for maintaining healthy mucous membranes. Regular hand-washing, avoiding touching the face, and using tissues or elbows to cover coughs and sneezes can prevent the introduction of pathogens to mucosal surfaces. Additionally, maintaining oral hygiene through regular brushing and flossing can protect the mucous membranes in the mouth and throat from infections and inflammation.
6. Consider Dietary Fiber
Dietary fiber plays a crucial role in maintaining the health of mucous membranes, particularly in the gastrointestinal tract. Fiber supports the growth of beneficial gut bacteria, which in turn helps maintain the integrity of the mucosal barrier. A diet high in fiber can prevent conditions such as inflammatory bowel disease by promoting a healthy balance of gut microbiota and reducing inflammation. Foods rich in fiber include fruits, vegetables, whole grains, and legumes.
7. Avoid Harmful Substances
Avoiding harmful substances such as tobacco, excessive alcohol, and recreational drugs is essential for the health of mucous membranes. These substances can damage the epithelial cells that produce mucus, leading to a compromised mucosal barrier and increased susceptibility to infections and inflammation. Additionally, certain medications and environmental toxins can have similar detrimental effects, so it is important to be mindful of exposure to these substances and seek alternatives when possible.
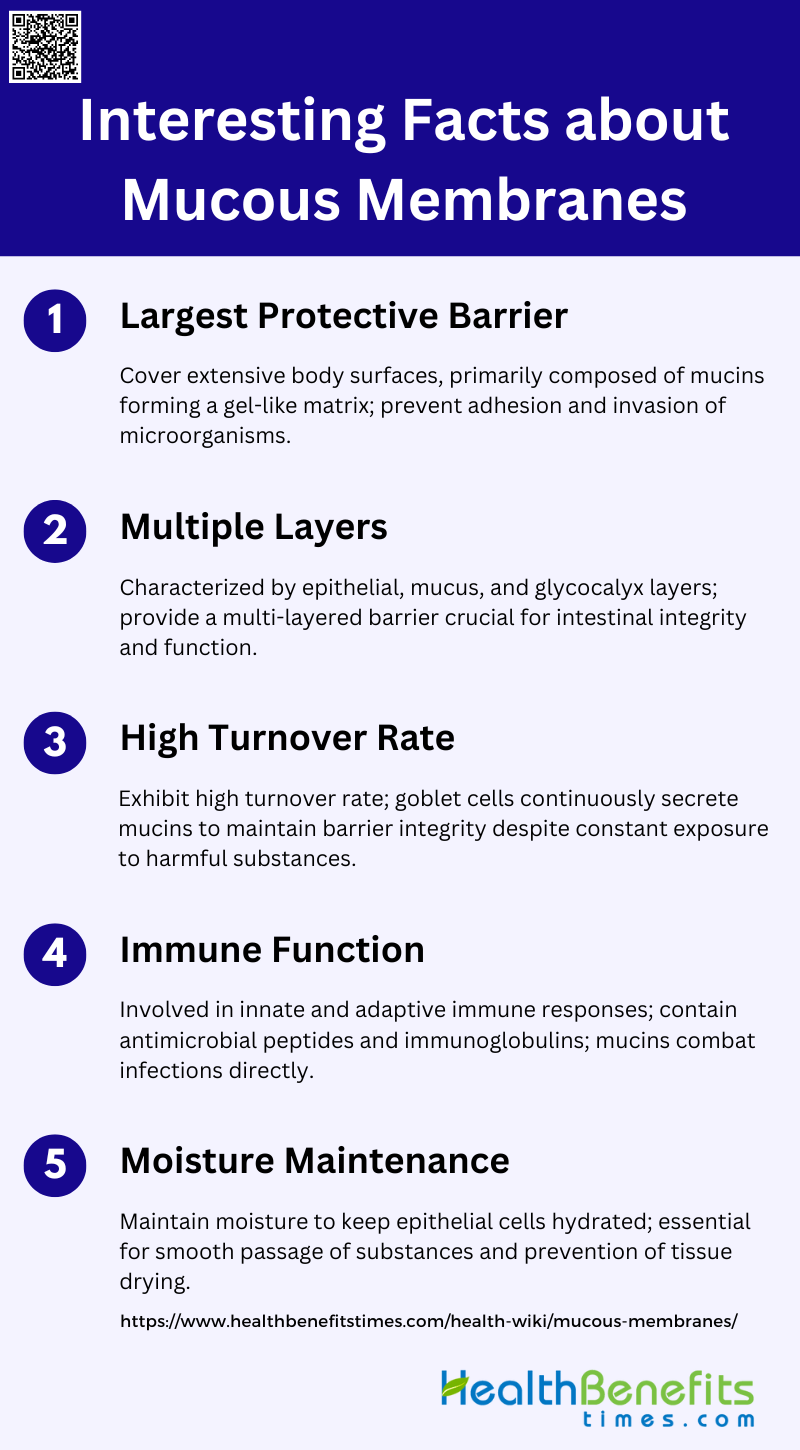
Interesting Facts about Mucous membranes
Mucous membranes are fascinating structures that line various cavities in the body and protect against infection. They are found in the respiratory, digestive, and urogenital tracts, playing a vital role in maintaining health. Here are some interesting facts about mucous membranes:
1. Largest Protective Barrier
Mucous membranes serve as the largest protective barrier in the body, covering extensive surfaces such as the gastrointestinal tract, respiratory tract, and reproductive organs. These membranes are primarily composed of mucins, which are high molecular weight glycoproteins that form a gel-like extracellular matrix. This matrix acts as a frontline defense against pathogens, physical damage, and chemical irritants. For instance, in the gastrointestinal tract, the mucus layer prevents the adhesion and invasion of harmful microorganisms, thereby maintaining intestinal health and preventing diseases like inflammatory bowel disease.
2. Multiple Layers
Mucous membranes are characterized by their multiple layers, which include an epithelial layer, a mucus layer, and often a glycocalyx. The epithelial layer serves as a physical barrier, while the mucus layer, composed of secreted mucins, provides a protective gel that traps pathogens and particles. The glycocalyx, a dense layer of membrane-bound mucins, further enhances this barrier by presenting a complex array of glycan structures that interact with the external environment. This multi-layered structure is crucial for maintaining the integrity and function of mucosal surfaces, particularly in the intestines where it helps to segregate the microbiota from the epithelial cells.
3. High Turnover Rate
Mucous membranes exhibit a high turnover rate, which is essential for maintaining their protective functions. Goblet cells within these membranes continuously produce and secrete mucins to replenish the mucus layer. This dynamic process ensures that the barrier remains intact and functional, even in the face of constant exposure to harmful substances and microorganisms. Disruptions in this turnover process can compromise the integrity of the mucus barrier, leading to various pathological conditions such as chronic inflammatory diseases.
4. Immune Function
Mucous membranes play a significant role in the immune function of the body. They are involved in both innate and adaptive immune responses. The mucus layer contains antimicrobial peptides and immunoglobulins that neutralize pathogens. Additionally, mucins themselves have been found to have direct roles in combating infections, such as acting as anti-parasitic effector molecules. The immune cells within the mucosal layers, including those in the female reproductive tract, also adapt to unique challenges such as maintaining tolerance to fetal antigens during pregnancy while still providing robust antimicrobial defense.
5. Moisture Maintenance
One of the critical functions of mucous membranes is the maintenance of moisture. The mucus layer helps to keep the underlying epithelial cells hydrated, which is essential for their proper function and survival. This moisture barrier also facilitates the smooth passage of substances and prevents the drying out of tissues. In the oral cavity, for example, the mucus barrier, aided by saliva, ensures that the mucous membrane remains moist, thereby protecting it from mechanical damage and infection.
Common Myths about Mucous membranes
Mucous membranes are often misunderstood, leading to several myths about their function and importance. These misconceptions can affect how we care for our health and well-being. Here are some common myths about mucous membranes:
1. Green or Yellow Mucus Always Indicates a Bacterial Infection
Contrary to popular belief, green or yellow mucus does not always signify a bacterial infection. The color change is often due to the presence of white blood cells and the body’s immune response, which can occur during viral infections as well. Therefore, green or yellow mucus can be seen in both viral and bacterial infections, and color alone is not a definitive indicator of the type of infection.
2. Vaginal Discharge Always Indicates an Infection
Vaginal discharge is not always a sign of infection. It is a normal physiological process that helps keep the vagina clean and moist. The nature of the discharge can vary throughout the menstrual cycle due to hormonal changes. While certain types of discharge can indicate infections like bacterial vaginosis or yeast infections, not all discharge is pathological.
3. Mucus is Harmful and Should Be Eliminated
Mucus plays a crucial role in protecting mucous membranes by trapping pathogens and particles, preventing them from entering the body. It also keeps tissues moist, which is essential for their proper function. Therefore, mucus is not harmful and should not be eliminated; rather, it is a vital part of the body’s defense mechanism.
4. Pregnant Women Do Not Have Vaginal Discharge
It is a myth that pregnant women do not have vaginal discharge. In fact, vaginal discharge often increases during pregnancy due to heightened estrogen levels and increased blood flow to the vaginal area. This discharge, known as leukorrhea, is typically thin, white, and mild-smelling, and it serves to protect the birth canal from infection.
5. All Mucous Membranes Are the Same
Not all mucous membranes are the same; they vary significantly depending on their location and function within the body. For instance, the mucous membranes in the respiratory tract are designed to trap and expel particles, while those in the digestive tract aid in nutrient absorption and protect against pathogens. Each type of mucous membrane is specialized to perform specific functions crucial to maintaining overall health.