Metabolic disorders are a group of conditions that occur due to disruptions in the normal metabolic processes within the body. These disorders can affect the body’s ability to convert food into energy and are often characterized by abnormalities in the metabolism of carbohydrates, fats, and proteins. Common examples include diabetes mellitus, obesity, metabolic syndrome, and hyperlipidemia. These conditions can lead to serious health complications such as cardiovascular diseases, liver disease, and increased risk of stroke. Metabolic disorders can be influenced by genetic factors, lifestyle choices, and environmental factors, and their management typically involves a combination of dietary changes, physical activity, and medications to control symptoms and prevent complications.
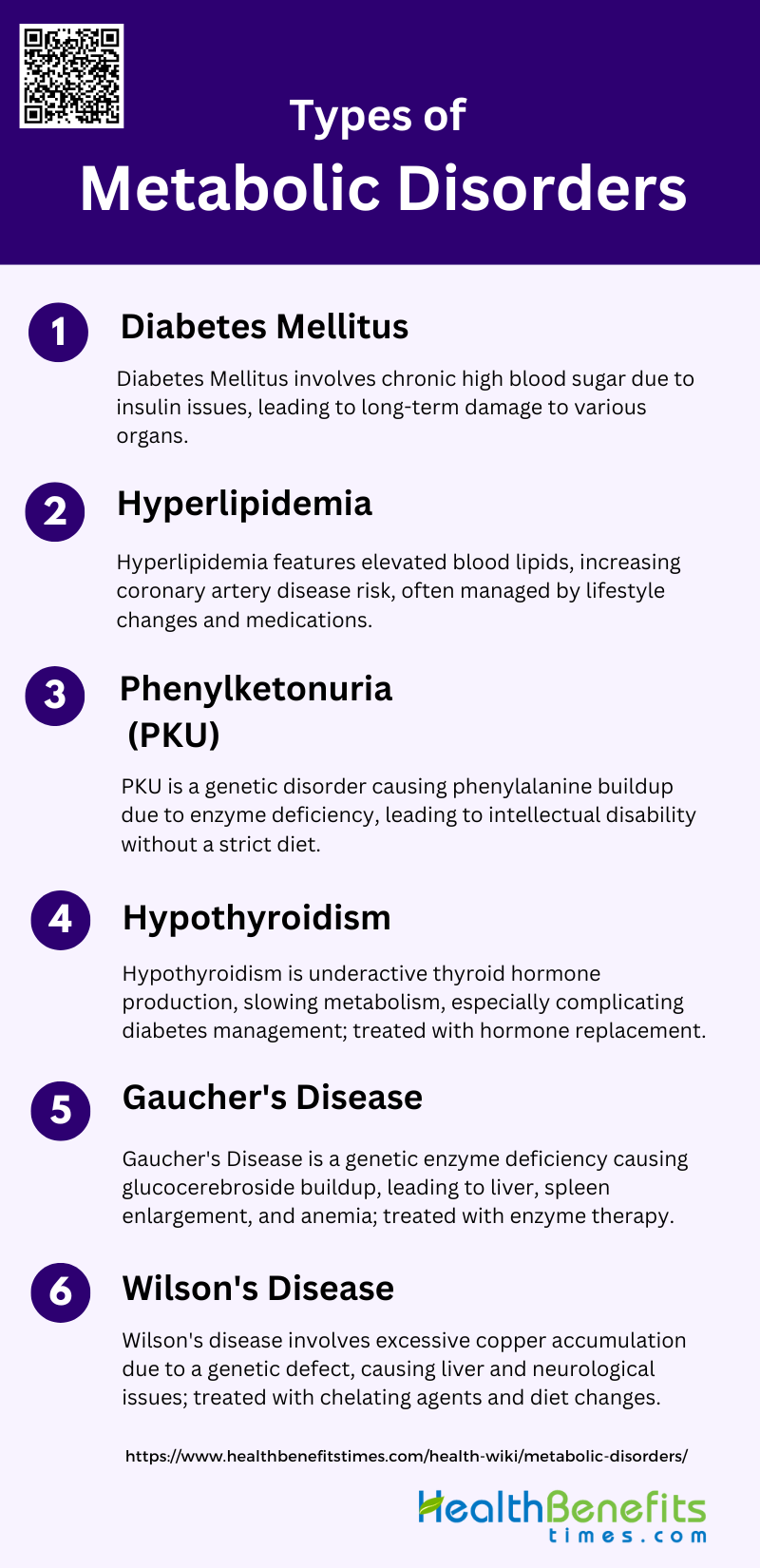
Types of Metabolic Disorders
These disorders can be genetic or acquired and affect the body’s ability to perform essential biochemical reactions. Below are some common types of metabolic disorders:
1. Diabetes Mellitus
Diabetes Mellitus is a group of metabolic diseases characterized by chronic hyperglycemia due to defects in insulin secretion, insulin action, or both. This condition leads to long-term damage and dysfunction of various organs, including the eyes, kidneys, nerves, heart, and blood vessels. The two main types are Type 1, caused by an absolute deficiency of insulin secretion, and Type 2, which involves a combination of insulin resistance and inadequate insulin secretion. Symptoms include polyuria, polydipsia, weight loss, and blurred vision. Long-term complications can include retinopathy, nephropathy, neuropathy, and increased risk of cardiovascular diseases.
2. Hyperlipidemia
Hyperlipidemia refers to elevated levels of lipids in the blood, which can include cholesterol and triglycerides. It is often associated with metabolic syndrome, type 2 diabetes, and familial combined hyperlipidemia (FCHL). These conditions share common features such as central obesity, insulin resistance, and hypertension. Hyperlipidemia increases the risk of premature coronary artery disease. Treatment typically involves lifestyle changes and medications like statins and niacin to manage lipid levels and reduce cardiovascular risk.
3. Phenylketonuria (PKU)
Phenylketonuria (PKU) is a genetic metabolic disorder characterized by a deficiency in the enzyme phenylalanine hydroxylase, which is necessary for the metabolism of the amino acid phenylalanine. Without this enzyme, phenylalanine accumulates in the body, leading to intellectual disability, behavioral problems, and seizures if untreated. Early diagnosis through newborn screening and a strict diet low in phenylalanine can prevent the severe outcomes associated with this disorder.
4. Hypothyroidism
Hypothyroidism is a condition where the thyroid gland does not produce enough thyroid hormones, leading to a slowdown in metabolic processes. It is closely linked with diabetes mellitus, as both conditions can influence each other. Symptoms of hypothyroidism include fatigue, weight gain, cold intolerance, and depression. In diabetic patients, untreated hypothyroidism can impair metabolic control and exacerbate complications. Management involves thyroid hormone replacement therapy and regular monitoring of thyroid function, especially in diabetic patients.
5. Gaucher’s Disease
Gaucher’s Disease is a genetic disorder resulting from a deficiency in the enzyme glucocerebrosidase, leading to the accumulation of glucocerebroside in various body tissues. This accumulation causes symptoms such as enlarged liver and spleen, bone pain, and anemia. Gaucher’s Disease is one of the lysosomal storage disorders and can vary in severity. Treatment options include enzyme replacement therapy and substrate reduction therapy, which aim to reduce the buildup of glucocerebroside in the body.
6. Wilson’s Disease
Wilson’s disease is a rare genetic disorder characterized by excessive accumulation of copper in the liver, brain, and other vital organs due to a defect in copper transport. Symptoms can include liver disease, neurological symptoms, and psychiatric disturbances. Early diagnosis and treatment are crucial to prevent severe complications. Treatment typically involves chelating agents that bind copper and promote its excretion, as well as dietary modifications to reduce copper intake.
Causes of Metabolic Disorders
These disorders can be influenced by genetic predispositions, lifestyle choices, and environmental exposures. Below are some of the primary causes of metabolic disorders:
1. Genetic Factors
Genetic predisposition plays a significant role in the development of metabolic disorders. Mutations in both nuclear and mitochondrial genomes have been identified as contributors to metabolic syndrome (MetS) and its components, such as obesity, insulin resistance, and cardiovascular diseases. These genetic mutations can affect mitochondrial function, which is central to energy metabolism, thereby influencing the regulation of metabolic processes. Studies have shown that defects in mitochondrial DNA can lead to metabolic abnormalities, highlighting the importance of genetic factors in the pathogenesis of MetS.
2. Environmental Influences
Environmental factors, including exposure to pollutants and chemicals, significantly contribute to metabolic disorders. Persistent organic pollutants (POPs) and other endocrine-disrupting chemicals (EDCs) have been linked to mitochondrial dysfunction, which is a key factor in the development of insulin resistance and metabolic syndrome. Chronic exposure to these pollutants can lead to the accumulation of toxins in the body, exacerbating metabolic abnormalities. This environmental impact necessitates further research to understand the precise mechanisms and develop strategies for mitigation.
3. Lifestyle Factors
Lifestyle choices, such as diet and physical activity, are crucial determinants of metabolic health. Sedentary behavior and high-calorie diets rich in fats and sugars can lead to obesity, insulin resistance, and other components of metabolic syndrome. Nutritional stress from unhealthy diets promotes oxidative stress and inflammation, which are underlying factors in the development of metabolic disorders. Conversely, regular physical activity has been shown to improve mitochondrial function and insulin sensitivity, highlighting the importance of lifestyle modifications in preventing and managing metabolic syndrome.
4. Organ Dysfunction
Organ dysfunction, particularly in the liver, pancreas, and cardiovascular system, is closely associated with metabolic disorders. Impaired mitochondrial function in these organs can lead to decreased energy production, lipid accumulation, and insulin resistance. For instance, mitochondrial dysfunction in the heart can result in diminished cardiac energetic efficiency and diastolic dysfunction, contributing to cardiovascular diseases. Similarly, liver and pancreatic dysfunctions impede glucose metabolism, further exacerbating metabolic abnormalities.
5. Mitochondrial Disorders
Mitochondrial dysfunction is a central feature of many metabolic disorders. It involves impaired oxidative phosphorylation, reduced mitochondrial biogenesis, and increased oxidative stress, which collectively disrupt cellular energy metabolism. Mitochondrial dysfunction can be caused by genetic mutations, environmental toxins, and aging. This dysfunction leads to the accumulation of reactive oxygen species (ROS), causing cellular damage and contributing to the pathogenesis of metabolic syndrome, diabetes, and cardiovascular diseases.
6. Hormonal Imbalances
Hormonal imbalances, such as those involving insulin, cortisol, and thyroid hormones, play a significant role in metabolic disorders. Insulin resistance, a hallmark of metabolic syndrome, is often accompanied by dysregulation of other hormones that control metabolism. For example, elevated cortisol levels due to chronic stress can lead to increased blood glucose and lipid levels, promoting obesity and insulin resistance. Hormonal imbalances can also affect mitochondrial function, further complicating the metabolic landscape and increasing the risk of associated diseases.
Symptoms of Metabolic Disorders
Metabolic disorders can manifest through a variety of symptoms that often affect multiple systems within the body. These symptoms may range from mild to severe and can significantly impact an individual’s quality of life. Common signs include unexplained weight changes, fatigue, and digestive issues. Below are some of the key symptoms associated with metabolic disorders:
- Tiredness and Lack of Energy
- Unintended Weight Changes
- Changes in Skin
- Developmental Delays
- Increased Blood Pressure
- High Blood Sugar
- Excess Body Fat Around the Waist
- Abnormal Cholesterol or Triglyceride Levels
- Stomach Pain and Vomiting
- Muscle Weakness and Exercise Intolerance
- Jaundice
- Seizures
Diagnosis of Metabolic Disorders
Diagnosing metabolic disorders involves a comprehensive evaluation of medical history, physical examination, and various diagnostic tests. These tests may include blood tests, genetic testing, and imaging studies to identify abnormalities in metabolic processes. Below are some of the key diagnostic methods used to detect metabolic disorders:
1. Blood tests and their significance
Blood tests play a crucial role in the diagnosis of metabolic disorders by measuring the levels of enzymes, hormones, and metabolites. These tests are essential for newborn screening (NBS) and family screening, as well as for monitoring treatment and prognosis. For instance, dried blood spot (DBS) specimens have been widely used since the 1960s for monitoring patients with inherited metabolic disorders (IMDs) due to their convenience and the ability to perform high-throughput analysis using advanced techniques like ultra-performance liquid chromatography (UPLC-MS/MS). Additionally, targeted metabolomic analysis of plasma samples can effectively diagnose various IMDs by distinguishing patient samples from controls through principal component analysis and hierarchical clustering. The precision and reliability of these tests are critical, as they help in the early detection and management of metabolic disorders.
2. Genetic testing for inherited disorders
Genetic testing has become increasingly important for diagnosing inherited metabolic disorders (IMDs), especially with the advent of Next Generation Sequencing (NGS) and whole exome/genome sequencing (ES/GS). These techniques have significantly improved the diagnostic yield for IMDs, particularly in adult patients presenting with unexplained neurological symptoms or phenotypes involving multiple organ systems. In a cohort study, molecular genetic diagnosis was achieved in 64% of patients, highlighting the effectiveness of genetic testing in identifying specific mutations and aiding in patient management. Furthermore, genetic testing not only helps in diagnosing the affected individual but also in identifying at-risk family members, thereby facilitating early intervention and treatment.
3. Imaging studies and biopsy procedures
Imaging studies and biopsy procedures are vital for diagnosing certain metabolic disorders, particularly those involving structural abnormalities or specific tissue involvement. For example, muscle biopsies are often required for the definitive diagnosis of mitochondrial oxidative phosphorylation (OXPHOS) disorders, as they allow for mtDNA and enzymatic testing. These invasive procedures, although challenging, provide critical information that supports the diagnosis and guides treatment decisions. Additionally, in vitro techniques using white blood cells, somatic cell cultures, and amniotic fluid cells have simplified the detection of hereditary metabolic diseases, reducing the need for surgical biopsies under general anesthesia. These methods are essential for confirming diagnoses and tailoring appropriate therapeutic strategies for patients with metabolic disorders.
Treatment of Metabolic Disorders
The treatment of metabolic disorders involves a multifaceted approach tailored to the specific condition and individual needs. Common strategies include lifestyle modifications, medication, and sometimes surgical interventions. Below are some of the primary treatment methods for managing metabolic disorders:
1. Dietary Changes
Dietary modifications are a cornerstone in the management of metabolic disorders. The Mediterranean and DASH (Dietary Approaches to Stop Hypertension) diets have shown significant benefits in managing metabolic syndrome, characterized by abdominal obesity, dyslipidemia, hypertension, and insulin resistance. These diets emphasize the consumption of high-quality foods; including fruits, vegetables, whole grains, and lean proteins, while reducing the intake of saturated fats, Tran’s fats, and cholesterol. Such dietary patterns not only improve individual metabolic parameters but also offer a sustainable approach to long-term health without the need for highly restrictive diets.
2. Medications
Pharmacological interventions are essential when lifestyle modifications alone are insufficient to manage metabolic disorders. Medications targeting specific components of metabolic syndrome, such as statins for dyslipidemia, antihypertensives for high blood pressure, and insulin sensitizers for insulin resistance, are commonly used. Emerging therapies, including peroxisome proliferator-activated receptor agonists, show promise in broadening the treatment landscape. Additionally, medications like thiazolidinediones and renin-angiotensin system blockers have shown benefits in managing hypertension and improving insulin sensitivity, respectively.
3. Exercise, Stress Management, and Weight Control
Regular physical activity, stress management, and weight control are critical components in the treatment of metabolic disorders. Exercise, including both aerobic and strength training helps reduce visceral fat, improve insulin sensitivity, and lower blood pressure. Stress management techniques, such as mindfulness and cognitive-behavioral therapy, can mitigate the adverse effects of chronic stress on metabolic health. Achieving and maintaining a healthy weight through a combination of diet and exercise is essential for reducing the risk of developing metabolic syndrome and its associated complications.
4. Enzyme Replacement Therapy
Enzyme replacement therapy (ERT) is a targeted treatment approach for specific metabolic disorders caused by enzyme deficiencies. While not commonly used for broader metabolic syndrome, ERT is crucial for conditions like lysosomal storage diseases, where it helps replace the deficient enzyme, thereby reducing the accumulation of toxic substrates. This therapy can significantly improve the quality of life and clinical outcomes for patients with these rare metabolic disorders, although its application in more common metabolic conditions remains limited.
5. Bariatric Surgery
Bariatric surgery is a highly effective treatment for morbid obesity and its associated metabolic disorders, including type 2 diabetes, hypertension, and dyslipidemia. Procedures such as gastric bypass and sleeve gastrectomy result in significant and sustained weight loss, improved insulin sensitivity, and remission of type 2 diabetes in many patients. The metabolic benefits of bariatric surgery are mediated through both weight-dependent and weight-independent mechanisms, including changes in gut hormones and bile acids. This surgical intervention is increasingly recognized as a standard treatment for severe metabolic syndrome and obesity.
6. Liver Transplants
Liver transplantation is a treatment option for end-stage liver disease resulting from metabolic disorders such as nonalcoholic steatohepatitis (NASH). While not a first-line treatment, it becomes necessary when liver function is severely compromised. Post-transplant, patients often experience significant improvements in metabolic parameters, although the underlying metabolic disorder may still require ongoing management. Liver transplantation offers a life-saving option for patients with advanced liver disease, but it is accompanied by the need for lifelong immunosuppression and careful monitoring.
Living with Metabolic Disorders
Living with metabolic disorders requires ongoing management and lifestyle adjustments to maintain health and well-being. Individuals often need to adhere to specific dietary guidelines, regular physical activity, and medication regimens. Below are some key strategies for living with metabolic disorders:
1. Tips for managing daily life
Managing daily life with metabolic disorders involves adopting and maintaining healthy lifestyle choices. Regular physical activity and a balanced diet are crucial. Incorporating a Mediterranean-type diet, which emphasizes fruits, vegetables, whole grains, and healthy fats, can be particularly beneficial. Consistent exercise helps manage weight and improve insulin sensitivity, which is vital for controlling metabolic syndrome components. Small, sustainable changes are more effective than drastic, short-term measures. Additionally, individualized lifestyle education and regular follow-ups can significantly enhance adherence to healthy behaviors. Support from healthcare professionals, such as nurse-led interventions, can also improve self-efficacy and health-promoting behaviors.
2. Importance of regular medical check-ups
Regular medical check-ups are essential for individuals with metabolic disorders to monitor and manage the various risk factors associated with the condition. These check-ups help in early detection and management of complications such as cardiovascular diseases and type 2 diabetes. Continuous monitoring allows for timely adjustments in treatment plans, including pharmacological interventions when necessary. Regular assessments of blood pressure, glucose levels, and lipid profiles are crucial to prevent the progression of the disorder. Moreover, these check-ups provide opportunities for healthcare providers to reinforce the importance of lifestyle modifications and ensure that patients remain motivated and informed about their health status.
3. Support groups and resources
Support groups and resources play a vital role in managing metabolic disorders by providing emotional support, practical advice, and a sense of community. These groups can help individuals share experiences, challenges, and strategies for coping with the condition. Access to resources such as educational materials, lifestyle intervention programs, and professional guidance can significantly improve self-efficacy and adherence to healthy behaviors. Online forums and local community groups can offer additional support and information, making it easier for individuals to stay motivated and committed to their health goals. Engaging with support networks can also reduce feelings of isolation and empower individuals to take proactive steps in managing their condition.