Macular degeneration, specifically age-related macular degeneration (AMD), is a prevalent eye condition that primarily affects the central part of the retina known as the macula. This area is crucial for sharp, detailed vision necessary for activities like reading, driving, and recognizing faces. AMD is a leading cause of vision loss among individuals aged 60 and older in developed countries. The condition can be classified into two types: dry AMD, characterized by the gradual breakdown of light-sensitive cells and the accumulation of drusen (proteinaceous deposits), and wet AMD, marked by the abnormal growth of blood vessels under the retina, leading to rapid vision loss. While peripheral vision typically remains intact, central vision deteriorates, significantly impacting quality of life.
Types of Macular Degeneration
Macular degeneration is a medical condition that affects the central part of the retina, leading to vision loss. It primarily occurs in older adults and is a leading cause of blindness in people over 50. There are two main types of macular degeneration:
1. Dry AMD
Dry age-related macular degeneration (AMD) is a progressive eye condition that primarily affects the central area of the retina known as the macula, leading to a gradual loss of central vision. It is characterized by the presence of drusen, which are yellow deposits under the retina, and atrophic changes in the retinal pigment epithelium. Dry AMD is the most prevalent form of AMD, accounting for approximately 85-90% of all cases. The progression of dry AMD can lead to advanced geographic atrophy, where large areas of the retina become damaged, resulting in significant vision loss. Despite its high prevalence, there are currently no approved treatments to halt or reverse the progression of dry AMD. Management strategies primarily focus on lifestyle modifications, such as increasing antioxidant intake and quitting smoking, to reduce risk factors. Research is ongoing to develop effective therapies, with several potential treatments targeting the complement cascade and other molecular pathways under investigation.
2. Wet AMD
Wet age-related macular degeneration (wet AMD) is a severe form of AMD characterized by the abnormal growth of blood vessels beneath the retina, leading to leakage and scarring that can cause rapid and significant vision loss. This neovascularization process is primarily driven by vascular endothelial growth factor (VEGF), making anti-VEGF therapy the current gold standard for treatment. Wet AMD is less common than dry AMD but is responsible for approximately 90% of acute blindness cases due to AMD. The prevalence of wet AMD increases with age, and it is influenced by genetic factors, such as polymorphisms in the HTRA1 gene, as well as lifestyle factors like smoking and diet. Despite advancements in treatment, wet AMD remains a progressive condition, and ongoing research is focused on developing more effective and lasting therapies.
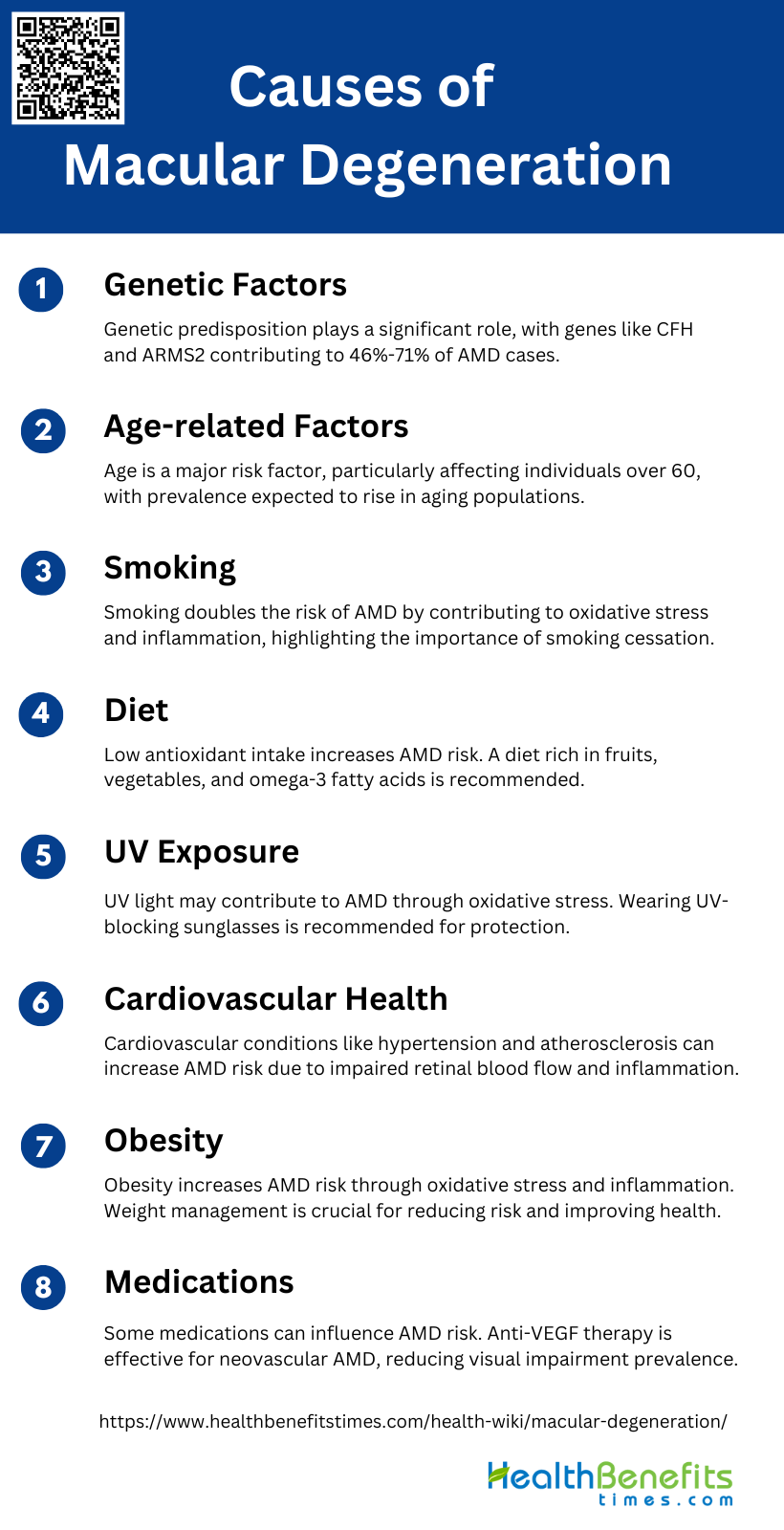
Causes of Macular Degeneration
Macular degeneration can result from various factors. While the exact mechanisms are not fully understood, research has identified several key contributors to the development and progression of this eye condition. The following list outlines some of the primary causes of macular degeneration:
1. Genetic Factors
Age-related macular degeneration (AMD) is significantly influenced by genetic factors. Research has identified over 50 genetic susceptibility loci, with the CFH and ARMS2 genes being the most notable. Genetic dysregulation in pathways such as complement, lipid, angiogenic, and inflammatory pathways are implicated in AMD’s pathogenesis. Genome-wide association studies have revealed numerous common variants associated with AMD, and sequencing has increased our understanding of how rare genetic variants impact the disease. Genetic factors are estimated to contribute to 46%-71% of AMD cases, highlighting the importance of genetic predisposition in the development and progression of this condition.
2. Age-related Factors
Age is one of the most consistent and significant risk factors for AMD. The prevalence of AMD increases with age, particularly affecting individuals over 60 years old. As populations age, the incidence of AMD is expected to rise, making it a major public health concern. Advanced age-related macular degeneration, including neovascular (wet) and geographic atrophy (late dry), is associated with substantial, progressive visual impairment. The aging process contributes to the dysregulation of various biological pathways, including oxidative stress and inflammation, which are crucial in the pathogenesis of AMD.
3. Smoking
Smoking is a well-established risk factor for AMD, consistently associated with an increased risk of developing the disease. Chronic cigarette smoking contributes to oxidative stress and inflammation, which are key mechanisms in AMD pathogenesis. Studies have shown that smoking can double the risk of AMD, and quitting smoking is one of the most effective preventive strategies. The harmful effects of smoking on the retina and its role in accelerating the progression of AMD underscore the importance of smoking cessation in managing and preventing this condition.
4. Diet
Dietary factors play a crucial role in the development and progression of AMD. Low dietary intake of antioxidants, such as zinc and carotenoids, has been linked to an increased risk of AMD. Nutritional supplements containing high doses of antioxidants and zinc can slow the progression of the disease. Additionally, maintaining a healthy diet rich in fruits, vegetables, and omega-3 fatty acids is recommended to reduce the risk of AMD. Dietary modifications, along with other lifestyle changes, can significantly impact the onset and progression of AMD.
5. UV Exposure
Exposure to ultraviolet (UV) light has been suggested as a potential risk factor for AMD, although the evidence is less consistent compared to other factors. UV light can induce oxidative stress and damage retinal cells, contributing to the pathogenesis of AMD. Protective measures, such as wearing sunglasses that block UV rays, are recommended to minimize UV exposure and potentially reduce the risk of AMD. Further research is needed to fully understand the relationship between UV exposure and AMD development.
6. Cardiovascular Health
Cardiovascular health is closely linked to AMD, with several cardiovascular risk factors being associated with the disease. Hypertension, atherosclerosis, and other cardiovascular conditions can contribute to the development and progression of AMD. The underlying mechanisms include impaired blood flow to the retina and increased oxidative stress and inflammation. Managing cardiovascular health through lifestyle changes and medical interventions can help reduce the risk of AMD and improve overall ocular health.
7. Obesity
Obesity is another significant risk factor for AMD. Excess body weight is associated with increased oxidative stress and inflammation, which are key contributors to AMD pathogenesis. Studies have shown that obesity can increase the risk of developing AMD and accelerate its progression. Weight management through a healthy diet and regular physical activity is recommended to reduce the risk of AMD and improve overall health. Addressing obesity as part of a comprehensive approach to AMD prevention is crucial.
8. Medications
Certain medications have been implicated in the development and progression of AMD. For example, long-term use of medications that affect lipid metabolism or blood pressure may influence AMD risk. Additionally, intravitreal anti-vascular endothelial growth factor (VEGF) therapy, such as ranibizumab and bevacizumab, is highly effective in treating neovascular AMD and has significantly decreased the prevalence of visual impairment. Ongoing research is exploring new therapeutic agents and their potential impact on AMD management. Understanding the role of medications in AMD is essential for optimizing treatment strategies.
Symptoms of Macular Degeneration
1. Dry AMD
- Visual Distortions
- Reduced Central Vision
- Increased Need for Bright Light
- Difficulty Adapting to Low Light
- Blurriness of Printed Words
- Difficulty Recognizing Faces
- Dark or Blurry Spots
- Color Perception Changes
- Delayed Dark Adaptation
2. Wet AMD
- Sudden Visual Distortions
- Rapid Loss of Central Vision
- Increased Blurriness
- Difficulty Recognizing Faces
- Color Perception Changes
- Visual Hallucinations
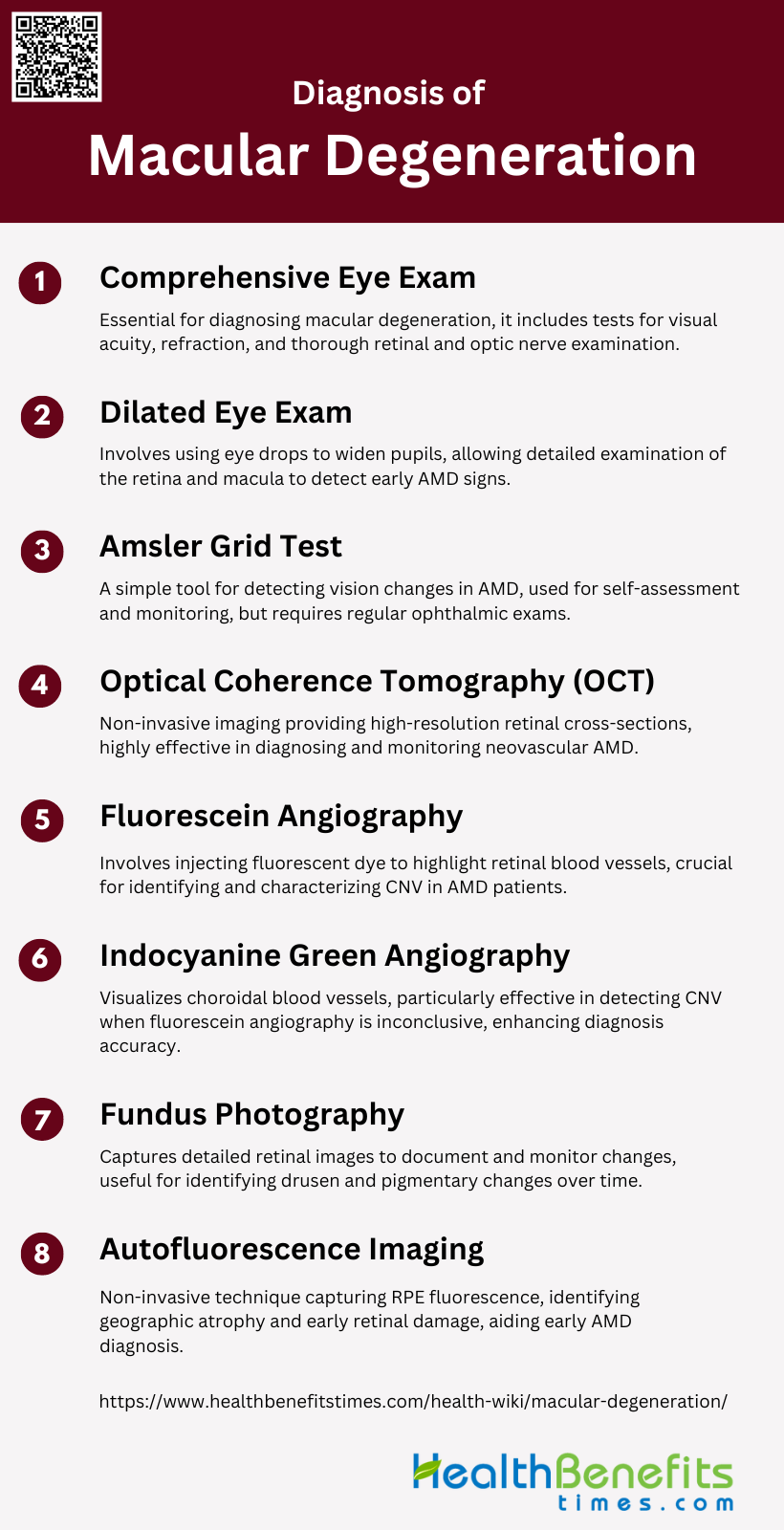
Diagnosis of Macular Degeneration
Macular degeneration is a common eye condition that primarily affects older adults, leading to loss of central vision. Early diagnosis is crucial for managing the progression of the disease and maintaining quality of life. The following steps outline the typical diagnostic process for macular degeneration:
1. Comprehensive Eye Exam
A comprehensive eye exam is essential for diagnosing macular degeneration and involves a series of tests to evaluate the overall health of the eyes. This exam typically includes visual acuity tests, refraction tests, and a thorough examination of the retina and optic nerve using specialized equipment. The comprehensive eye exam helps in identifying early signs of age-related macular degeneration (AMD) and other ocular conditions, allowing for timely intervention and management.
2. Dilated Eye Exam
A dilated eye exam is a critical component in diagnosing macular degeneration. During this procedure, eye drops are used to widen the pupils, allowing the ophthalmologist to get a better view of the retina and macula. This detailed examination can reveal the presence of drusen, pigmentary changes, and other abnormalities associated with AMD. The dilated eye exam is particularly useful in detecting early and intermediate stages of the disease, which might not be visible with undilated pupils.
3. Amsler Grid Test
The Amsler grid test is a simple, yet effective tool for detecting metamorphopsia, a common symptom of macular degeneration. Patients with nonneovascular AMD are encouraged to use the Amsler grid for self-assessment to monitor any changes in their vision. Although the test is easy and inexpensive, its sensitivity and specificity for detecting neovascular AMD are moderate, suggesting that it should be used in conjunction with regular ophthalmic examinations for accurate diagnosis.
4. Optical Coherence Tomography (OCT)
Optical Coherence Tomography (OCT) is a non-invasive imaging technique that provides high-resolution cross-sectional images of the retina. OCT is highly effective in diagnosing and monitoring neovascular AMD by detecting the presence of choroidal neovascularization (CNV) and fluid accumulation. Studies have shown that OCT has high sensitivity and moderate specificity for diagnosing AMD, making it a valuable tool in both initial diagnosis and ongoing management of the disease.
5. Fluorescein Angiography
Fluorescein angiography (FA) is a diagnostic procedure that involves injecting a fluorescent dye into the bloodstream to highlight the blood vessels in the retina. This test is particularly useful for identifying and characterizing CNV in AMD patients. FA provides detailed information about the size, location, and type of CNV, which is crucial for planning treatment strategies. Despite the advent of newer imaging techniques, FA remains a gold standard for diagnosing and monitoring neovascular AMD.
6. Indocyanine Green Angiography
Indocyanine Green Angiography (ICGA) is another imaging technique used to visualize the choroidal blood vessels. ICGA is particularly effective in detecting CNV, especially in cases where fluorescein angiography might be inconclusive. Studies have shown that ICGA can provide complementary information to OCT, enhancing the accuracy of AMD diagnosis. ICGA is also useful in assessing the composition and size of CNV, aiding in the management and treatment of the disease.
7. Fundus Photography
Fundus photography involves capturing detailed images of the retina, which can be used to document and monitor changes over time. This technique is useful for identifying drusen, pigmentary changes, and other retinal abnormalities associated with AMD. Fundus photography provides a permanent record that can be compared over successive visits to track the progression of the disease. It is often used in conjunction with other diagnostic tests to provide a comprehensive assessment of retinal health.
8. Autofluorescence Imaging
Autofluorescence imaging is a non-invasive technique that captures the natural fluorescence emitted by the retinal pigment epithelium (RPE). This imaging method is particularly useful for identifying areas of geographic atrophy and other changes in the RPE associated with AMD. Autofluorescence imaging can reveal early signs of retinal damage that might not be visible with other imaging techniques, making it a valuable tool in the early diagnosis and monitoring of AMD.
Treatment Options for AMD
1. Dry AMD
Dry age-related macular degeneration (AMD) is a progressive condition that leads to vision loss, primarily affecting older adults. While there is no definitive cure, several treatment options can help manage the disease and slow its progression. Nutritional supplements, such as those containing antioxidant vitamins C and E, lutein, zeaxanthin, and zinc, have been shown to reduce the risk of progression to advanced AMD. Lifestyle changes, including quitting smoking and adopting a diet rich in antioxidants, are also recommended to mitigate risk factors. Emerging drug treatments, such as complement inhibitors and visual cycle modulators, are currently under investigation and show promise in clinical trials. Additionally, low vision rehabilitation can provide patients with strategies and tools to maximize their remaining vision and maintain their quality of life. These combined approaches offer a multifaceted strategy to manage dry AMD effectively.
2. Wet AMD
Wet age-related macular degeneration (AMD) is a severe form of AMD characterized by the growth of abnormal blood vessels under the retina, leading to rapid vision loss. Several treatment options are available to manage this condition, each targeting different aspects of the disease.
- Anti-VEGF Injections: Anti-vascular endothelial growth factor (VEGF) therapy is the cornerstone of wet AMD treatment. Agents such as ranibizumab, bevacizumab, and aflibercept are commonly used to inhibit VEGF, thereby reducing neovascularization and improving visual acuity. Studies have shown that these injections can significantly improve visual outcomes and reduce retinal thickness.
- Photodynamic Therapy (PDT): PDT involves the use of a photosensitizing agent, verteporfin, which is activated by laser light to destroy abnormal blood vessels. This therapy is often used in combination with anti-VEGF injections to enhance efficacy and reduce the frequency of injections needed.
- Laser Therapy: Laser photocoagulation is another treatment option, particularly effective in the early stages of retinal angiomatous proliferation (RAP), a subtype of wet AMD. This method uses focused laser light to seal off leaking blood vessels, although it is less commonly used due to the risk of damaging surrounding retinal tissue.
- Gene Therapy: Emerging treatments such as gene therapy aim to provide long-term solutions by targeting the underlying genetic causes of wet AMD. These therapies are still in the experimental stages but hold promise for future treatment paradigms.
- Emerging Treatments: Research is ongoing to develop new treatments for wet AMD, including the use of stem cell therapy and novel pharmacological agents. These emerging therapies aim to offer more effective and less invasive options for patients.
Preventive Measures of Macular degeneration
Macular degeneration is a leading cause of vision loss, but certain preventive measures can help reduce the risk. Adopting a healthy lifestyle and regular eye check-ups are essential. Here are some key preventive measures to consider:
1. Stop Smoking
Smoking is a well-established risk factor for the development and progression of age-related macular degeneration (AMD). Numerous studies have shown that smoking significantly increases the risk of AMD, making it one of the most critical lifestyle changes for prevention. The Age-Related Eye Disease Study (AREDS) highlighted that individuals who smoked more than 10 pack-years had a higher incidence of advanced AMD compared to non-smokers. Additionally, smoking contributes to oxidative stress and inflammation, which are key mechanisms in the pathogenesis of AMD. Therefore, quitting smoking is strongly recommended to reduce the risk of AMD.
2. Eat a Healthy Diet
A healthy diet rich in specific nutrients can play a crucial role in preventing AMD. Nutrients such as lutein, zeaxanthin, beta-carotene, omega-3 fatty acids, and zinc have been shown to reduce the risk of early AMD. The Mediterranean diet, which emphasizes plant-based foods, has been associated with a lower risk of developing AMD and its progression to advanced stages. The AREDS and AREDS2 studies also demonstrated that supplements containing vitamins C and E, beta-carotene, and zinc could reduce the progression to advanced AMD by 25% over five years. Thus, maintaining a nutrient-rich diet is essential for AMD prevention.
3. Exercise Regularly and Maintain a Healthy Weight
Regular physical activity and maintaining a healthy weight are important preventive measures for AMD. Obesity and a high body mass index (BMI) have been associated with an increased risk of AMD progression. Exercise helps improve cardiovascular health, which is beneficial since cardiovascular diseases are linked to AMD. Engaging in regular physical activity can help manage weight and reduce the risk of hypertension and other cardiovascular conditions, thereby lowering the risk of AMD.
4. Control Blood Pressure and Cholesterol Levels
Controlling blood pressure and cholesterol levels is vital in preventing AMD. Hypertension and high cholesterol are known risk factors for AMD, as they can contribute to the development of drusen and other retinal changes. Managing these conditions through lifestyle changes and medication can help reduce the risk of AMD progression. Regular monitoring and treatment of these cardiovascular risk factors are recommended to maintain overall eye health and prevent AMD.
5. Protect Eyes from UV and Blue Light Exposure by Wearing Sunglasses
Protecting the eyes from ultraviolet (UV) and blue light exposure is another preventive measure for AMD. Although the data on light exposure and AMD are inconsistent, wearing sunglasses can provide comfort and potential protection from UV light, which may benefit ocular structures, including the lens. Blue-blocking intraocular lenses and sunglasses can help filter harmful light and reduce the risk of retinal damage, thereby potentially lowering the risk of AMD.
6. Get Regular Comprehensive Eye Exams
Regular comprehensive eye exams are crucial for the early detection and management of AMD. Early and intermediate stages of AMD can be identified through routine eye exams, allowing for timely intervention and monitoring. Early detection can help implement preventive measures and slow the progression of the disease. Regular eye exams are especially important for individuals with a family history of AMD or other risk factors.
7. Consider Taking AREDS2 Formula Supplements
The AREDS2 formula supplements, which include vitamins C and E, lutein, zeaxanthin, and zinc, have been shown to reduce the risk of progression to advanced AMD in some patients. The AREDS and AREDS2 studies demonstrated that these supplements could decrease the progression to advanced AMD by 25% over five years. While micronutrient supplementation is a promising preventive measure, it is essential to consult with a healthcare provider before starting any new supplement regimen.
8. Stay Hydrated
Staying hydrated is important for overall health, including eye health. Adequate hydration helps maintain the health of the retina and other ocular structures. While specific studies on hydration and AMD are limited, maintaining proper hydration supports general bodily functions and can contribute to overall eye health. Drinking sufficient water and maintaining a balanced diet with hydrating foods can help support eye health and potentially reduce the risk of AMD.