Lymphocytes are a type of white blood cell that play a crucial role in the immune system by defending the body against infections and diseases. They are primarily found in the blood and lymphatic system and are categorized into three main types: T cells, B cells, and natural killer (NK) cells. Lymphocytes are characterized by their ability to recognize specific antigens through receptors on their surface, enabling them to mount targeted immune responses. They are essential for both the adaptive immune response, which provides long-term immunity, and the innate immune response, which offers immediate defense against pathogens.
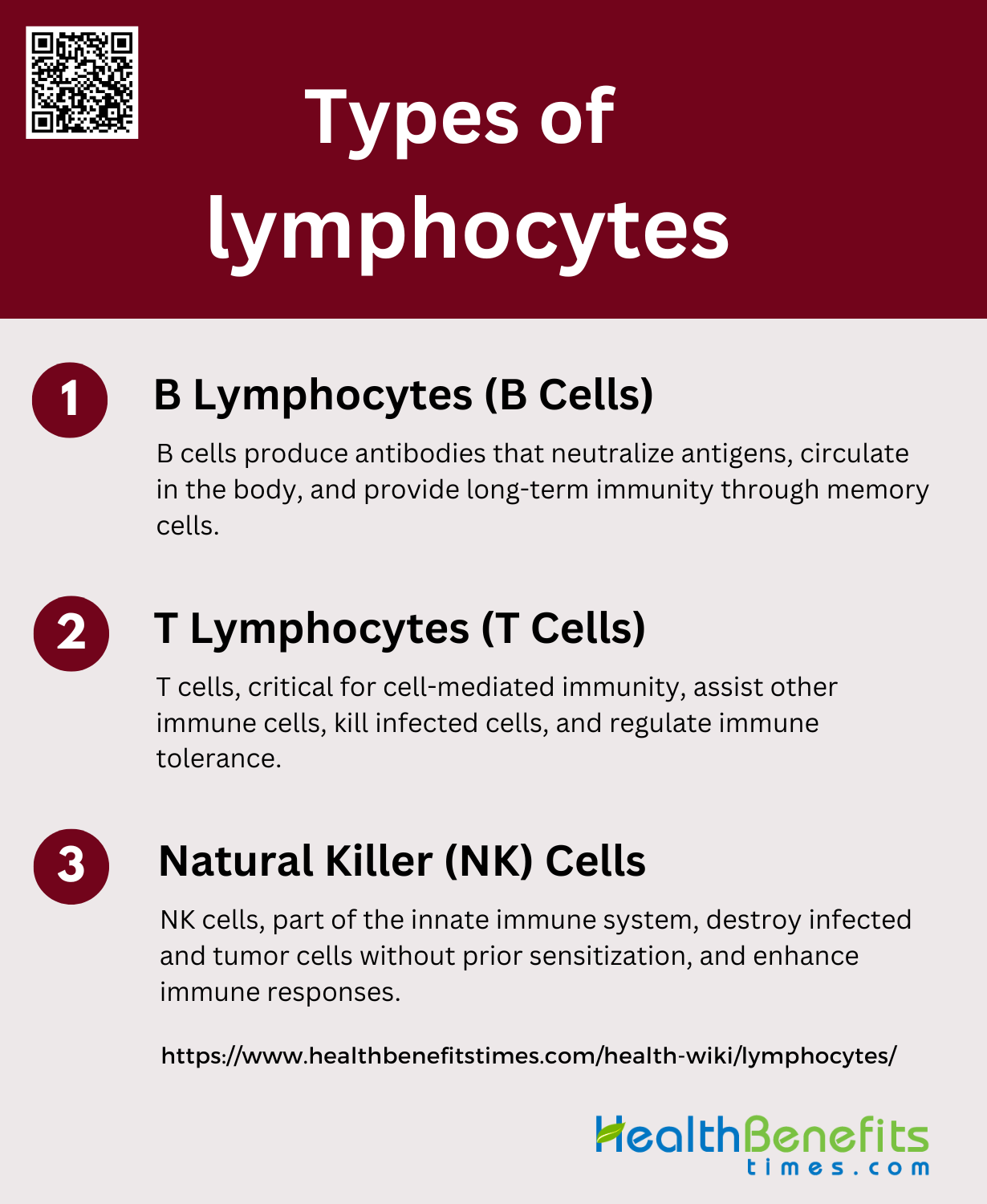
Types of lymphocytes
Lymphocytes are a vital component of the immune system, playing a crucial role in defending the body against infections and diseases. They are primarily divided into three main types, each with distinct functions and characteristics. Below is an overview of the different types of lymphocytes and their roles in the immune response.
1. B Lymphocytes (B Cells)
B lymphocytes, or B cells, are a crucial component of the adaptive immune system. They are primarily responsible for the production of antibodies, which are proteins that specifically recognize and bind to foreign antigens, neutralizing them or marking them for destruction by other immune cells. B cells develop in the bone marrow and undergo a maturation process that allows them to produce a diverse array of antibodies through a mechanism known as V(D)J recombination. Once mature, B cells circulate in the blood and lymphatic system, and upon encountering their specific antigen, they can differentiate into plasma cells that secrete large quantities of antibodies or memory B cells that provide long-term immunity.
2. T Lymphocytes (T Cells)
T lymphocytes, or T cells, are another essential component of the adaptive immune system, playing a pivotal role in cell-mediated immunity. They develop in the thymus and are characterized by the presence of T cell receptors (TCRs) on their surface, which recognize antigens presented by major histocompatibility complex (MHC) molecules on the surface of other cells. T cells can be broadly categorized into several subsets, including helper T cells (CD4+), which assist other immune cells, cytotoxic T cells (CD8+), which directly kill infected or cancerous cells, and regulatory T cells, which help maintain immune tolerance and prevent autoimmune diseases. Advances in immunology have also identified other specialized T cell subsets, such as IL-17-producing T cells and natural killer T cells, which have unique roles in immune regulation and response.
3. Natural Killer (NK) Cells
Natural Killer (NK) cells are a type of lymphocyte that plays a critical role in the innate immune system. Unlike B and T cells, NK cells do not require prior sensitization to recognize and kill virally infected cells and tumor cells. They are equipped with a variety of activating and inhibitory receptors that allow them to detect stressed cells in the absence of antibodies and MHC, making them a first line of defense against infections and malignancies. NK cells can induce apoptosis in target cells through the release of cytotoxic granules containing perforin and granzymes. Additionally, NK cells produce cytokines such as IFN-γ, which enhance the immune response. Recent research has also highlighted the potential of NK cells in cancer immunotherapy and their role in transplantation outcomes.
Functions of Lymphocytes
They perform various functions to protect the body from infections and diseases. Below are the primary functions of different types of lymphocytes:
1. Humoral Immunity
Humoral immunity is primarily mediated by B lymphocytes, which are responsible for the production of antibodies. These antibodies are crucial for neutralizing pathogens and facilitating their removal from the body. Upon encountering an antigen, B cells differentiate into plasma cells that secrete large quantities of antibodies specific to that antigen. This process is essential for the protection against a variety of pathogens and is a key component of the adaptive immune response. Additionally, B cells can present antigens to T cells, further enhancing the immune response. The production of different antibody isotypes by B cells also plays a role in opsonization and complement fixation, which are important for pathogen clearance.
2. Memory Formation
Memory formation in the immune system involves both B and T lymphocytes. After an initial encounter with an antigen, some B and T cells differentiate into memory cells. These memory cells persist in the body for long periods and can rapidly respond upon re-exposure to the same antigen. This rapid and robust response is the basis for long-lasting immunity and is a critical feature of adaptive immunity. Memory B cells, in particular, can quickly differentiate into plasma cells and produce antibodies upon re-exposure to their specific antigen, providing a faster and more effective immune response. Similarly, memory T cells can quickly proliferate and mount a strong response, contributing to the overall immune memory.
3. Cell-Mediated Immunity
Cell-mediated immunity is primarily mediated by T lymphocytes, which play a crucial role in defending against intracellular pathogens such as viruses and some bacteria. T cells can be divided into various subsets, including cytotoxic T cells (CD8+), which directly kill infected cells, and helper T cells (CD4+), which assist other immune cells by producing cytokines. Helper T cells can be further classified into Th1, Th2, Th17, and Tfh cells, each with distinct roles in immune regulation and pathogen defense. For instance, Th1 cells produce IFN-γ to activate macrophages, while Th2 cells are involved in activating eosinophils and mast cells. Regulatory T cells (Tregs) also play a role in maintaining immune tolerance and preventing autoimmunity.
4. Innate Immunity
Innate immunity is the body’s first line of defense against pathogens and involves various cell types, including innate lymphoid cells (ILCs) and innate-like B cells. These cells can respond rapidly to infections without the need for prior exposure to the pathogen. ILCs, for example, are tissue-resident cells that produce cytokines and help coordinate the early immune response. Innate-like B cells can also participate in early immune responses by producing natural antibodies and cytokines, and by presenting antigens to T cells. These innate immune responses are crucial for controlling infections until the adaptive immune system can mount a more specific and robust response.
5. Cytokine Production
Cytokine production is a critical function of both B and T lymphocytes, influencing various aspects of the immune response. T cells are well-known for their ability to produce a wide range of cytokines upon activation, which helps regulate the activity of other immune cells. B cells, although traditionally recognized for their role in antibody production, can also produce cytokines under specific conditions. These cytokines can influence the development, survival, and function of other immune cells, including T cells and innate immune cells. For example, B cell-derived cytokines such as IL-6 and TNF-α play roles in inflammation and the development of effector and memory T cell responses. The ability of B cells to produce cytokines adds another layer of complexity to their role in the immune system.
Lymphocyte Levels and Ranges
Normal Lymphocyte Count
The normal lymphocyte count in peripheral blood varies based on several factors, including age, gender, and ethnicity. For instance, a study on a healthy Korean population established that the mean lymphocyte count is approximately 1,928 cells/µL, which constitutes about 35.08% of the total white blood cells. These values can differ significantly across different populations and age groups. For example, children and adolescents have different lymphocyte subset distributions compared to adults. Therefore, it is crucial to consider these demographic factors when evaluating lymphocyte counts to determine what is considered “normal” for a specific individual or population.
Factors that Influence Lymphocyte Levels
Several factors can influence lymphocyte levels in the blood. These include demographic variables such as age, gender, and ethnicity, as well as environmental factors and medical treatments. For example, radiotherapy and chemotherapy in cancer patients can significantly reduce lymphocyte counts, with higher radiation doses and shorter treatment durations being associated with higher lymphocyte counts post-treatment. Additionally, infections like COVID-19 can cause significant fluctuations in lymphocyte levels, with severe cases showing marked lymphopenia and altered cytokine profiles. Other factors such as organ removal (e.g., thymus, spleen) and lifestyle choices also play a role in determining lymphocyte levels.
How to Measure Lymphocyte Levels
Lymphocyte levels are typically measured using blood tests, which can be performed through various techniques. Flow cytometry is a common method used to analyze lymphocyte subsets, providing detailed information on different types of lymphocytes such as T cells, B cells, and natural killer (NK) cells. Automated hematology analyzers are also used to count white blood cells and lymphocytes, offering a quick and efficient way to obtain these measurements. In clinical settings, peripheral blood samples are collected and analyzed to monitor immune status, diagnose diseases, and assess treatment effects. These tests are essential tools in both routine medical evaluations and specialized research studies.
Factors Affecting Lymphocyte Levels
Factors That Can Increase Lymphocyte Levels
Infections and certain cancers are known to increase lymphocyte levels. For instance, the presence of tumor-infiltrating lymphocytes (TILs) in breast cancer is a favorable prognostic factor, indicating an immune response against the tumor. Studies have shown that triple-negative and HER2-positive breast cancers exhibit higher levels of TILs compared to hormone receptor-positive subtypes, suggesting that these cancers may be more amenable to immunomodulation. Additionally, infections can stimulate the immune system, leading to an increase in lymphocyte counts. For example, Vgamma9Vdelta2 T lymphocytes, which are reactive against various intracellular pathogens, can proliferate in response to HIV-infected cells, thereby increasing lymphocyte levels.
Factors That Can Decrease Lymphocyte Levels
Several factors can lead to a decrease in lymphocyte levels, including autoimmune disorders, HIV/AIDS, and chemotherapy. HIV infection, particularly in its progression to AIDS, is associated with a significant reduction in CD4+ T lymphocytes, which compromises the immune system. Chemotherapy for cancer also results in lymphocyte depletion. For example, intensive chemotherapy for breast cancer significantly reduces B cells, CD4+ T cells, and CD8+ T cells, with some cell types remaining depleted even nine months post-treatment. Additionally, severe COVID-19 has been associated with lymphopenia, particularly affecting CD4+ and CD8+ T lymphocytes, which can exacerbate the severity of the disease.
Abnormal Lymphocyte Levels
Causes of Low Lymphocyte Count
Lymphocytopenia, or low lymphocyte count, can be caused by various factors, including infections and autoimmune disorders. Infections such as HIV and systemic lupus erythematosus (SLE) are known to lead to lymphocytopenia due to their impact on the immune system. Additionally, idiopathic CD4+ T-lymphocytopenia, a condition characterized by unexplained low CD4+ T-cell counts, can result in severe opportunistic infections. Other causes include systemic inflammatory responses, as seen in severe COVID-19 cases, where inflammation and direct viral effects on lymphoid organs lead to lymphocyte depletion. Furthermore, lifestyle factors such as lack of sleep due to heavy workloads have also been implicated in exacerbating lymphocytopenia.
Causes of High Lymphocyte Count
Lymphocytosis, or high lymphocyte count, is often associated with infections and chronic inflammatory conditions. Viral infections, such as those caused by cytomegalovirus and Epstein-Barr virus, can lead to elevated lymphocyte levels as the body mounts an immune response. Chronic lymphocytic leukemia (CLL) and monoclonal B-cell lymphocytosis (MBL) are hematologic conditions characterized by high lymphocyte counts, with MBL potentially progressing to CLL. Chronic inflammatory conditions, including autoimmune diseases, can also result in lymphocytosis due to persistent immune activation. These elevated lymphocyte levels reflect the body’s ongoing efforts to combat infection or inflammation.
Potential Health Implications
Abnormal lymphocyte levels, whether low or high, have significant health implications. Lymphocytopenia can lead to increased susceptibility to infections and poorer outcomes in conditions like cardiovascular diseases and heart failure. It is also associated with higher risks of opportunistic infections and malignancies, particularly in conditions like idiopathic CD4+ T-lymphocytopenia. On the other hand, lymphocytosis can indicate underlying chronic infections or hematologic malignancies such as CLL, which carry risks of disease progression and secondary infections. Both conditions necessitate careful monitoring and management to mitigate associated health risks and improve patient outcomes.
Maintaining Healthy Lymphocyte Levels
Maintaining healthy lymphocyte levels is crucial for a robust immune system and overall well-being. Proper nutrition, regular exercise, and adequate sleep are essential for supporting lymphocyte function. Below are key strategies for maintaining healthy lymphocyte levels:
1. Manage Stress
Managing stress is crucial for maintaining healthy lymphocyte levels. Chronic stress has been shown to negatively impact the immune system, leading to decreased numbers of natural killer (NK) cells and other lymphocytes. Studies indicate that mental stress does not significantly affect the numbers of NK, T cells, or other lymphocyte subtypes, but overall lifestyle quality, which includes stress management, is essential for optimal immune function. Therefore, incorporating stress-reducing activities such as mindfulness, meditation, and regular physical exercise can help maintain healthy lymphocyte levels and improve overall immune health.
2. Adequate Sleep
Adequate sleep is essential for maintaining healthy lymphocyte levels. Insufficient sleep has been associated with increased micronuclei frequency in lymphocytes, indicating higher levels of DNA damage and reduced immune function. A study involving Japanese hard-metal workers found that those who slept less than six hours per day had significantly higher micronuclei frequency in their lymphocytes compared to those who had adequate sleep. Ensuring sufficient sleep, typically 7-9 hours per night for adults, can help maintain the integrity and function of lymphocytes, thereby supporting a robust immune system.
3. Avoid Smoking and Excessive Alcohol
Avoiding smoking and excessive alcohol consumption is vital for maintaining healthy lymphocyte levels. Smoking has been shown to significantly decrease the numbers of NK cells and other lymphocytes, while also increasing the frequency of micronuclei in lymphocytes, indicating higher DNA damage. Similarly, excessive alcohol consumption negatively affects the number of granzyme A-expressing cells, which are crucial for immune defense. By avoiding these harmful habits, individuals can support their immune system and maintain healthier lymphocyte levels, reducing the risk of infections and other health issues.
4. Consume Lean Proteins
Consuming lean proteins is important for maintaining healthy lymphocyte levels. Proteins provide the necessary building blocks for the production and function of lymphocytes and other immune cells. A balanced diet that includes lean proteins such as poultry, fish, beans, and legumes can support the immune system by ensuring adequate nutrient intake. Studies have shown that balanced nutrition significantly affects the numbers of NK cells and other lymphocytes, highlighting the importance of a protein-rich diet for immune health. Therefore, incorporating lean proteins into daily meals can help maintain optimal lymphocyte levels and overall immune function.
5. Eat Foods Rich in Vitamins and Minerals
Eating foods rich in vitamins and minerals is essential for maintaining healthy lymphocyte levels. Nutritional imbalances have been linked to increased micronuclei frequency in lymphocytes, indicating higher DNA damage and compromised immune function. Vitamins such as A, C, D, and E, along with minerals like zinc and selenium, play crucial roles in supporting the immune system. A diet rich in fruits, vegetables, nuts, and seeds can provide these essential nutrients, helping to maintain the integrity and function of lymphocytes. Ensuring a well-balanced diet with adequate vitamins and minerals is key to supporting a healthy immune system.
6. Incorporate Antioxidant-Rich Foods
Incorporating antioxidant-rich foods into the diet can help maintain healthy lymphocyte levels. Antioxidants protect lymphocytes from oxidative stress and DNA damage. Long-term consumption of anthocyanin-rich fruit juice, for example, has been shown to significantly increase antioxidant markers in lymphocytes and reduce DNA strand-breaks. Foods such as berries, dark chocolate, nuts, and green leafy vegetables are rich in antioxidants and can support the immune system by protecting lymphocytes from oxidative damage. Including these foods in the diet can enhance lymphocyte health and overall immune function.
7. Include Probiotics
Including probiotics in the diet can positively impact lymphocyte levels and overall immune health. Probiotics, found in fermented foods like yogurt, kefir, and sauerkraut, help maintain a healthy gut microbiota, which in turn supports the immune system. Long-term consumption of anthocyanin-rich fruit juice has been shown to affect the gut microbiota and enhance the antioxidant response in lymphocytes. A healthy gut microbiota can improve the function and proliferation of lymphocytes, thereby strengthening the immune system. Incorporating probiotics into the diet can thus contribute to maintaining healthy lymphocyte levels and overall immune health.
FAQs
1. What are the potential symptoms of abnormal lymphocyte levels?
Abnormal lymphocyte levels, whether high or low, may present with symptoms such as frequent infections, fatigue, unexplained weight loss, night sweats, or swollen lymph nodes. However, many individuals with abnormal lymphocyte levels may be asymptomatic, especially in the early stages of a condition.
2. How do lymphocytes differ from other white blood cells, like neutrophils or monocytes?
Lymphocytes are primarily involved in adaptive immunity, recognizing specific antigens and mounting targeted immune responses, whereas neutrophils and monocytes are part of the innate immune system and are the first responders to infections, working in a more general, non-specific manner.
3. Can lifestyle changes alone normalize lymphocyte levels, or is medical intervention necessary?
While healthy lifestyle changes like proper nutrition, regular exercise, stress management, and adequate sleep can support immune health and help maintain normal lymphocyte levels, significant abnormalities often require medical intervention, especially if caused by underlying conditions like infections, autoimmune diseases, or cancer.
4. What is the role of lymphocytes in autoimmune diseases?
In autoimmune diseases, lymphocytes may mistakenly target the body’s own cells as if they were foreign, leading to inflammation and tissue damage. This dysfunction can involve both T cells and B cells, depending on the specific autoimmune condition.
5. How do vaccinations affect lymphocyte function?
Vaccinations stimulate the immune system to produce memory B and T cells specific to the pathogen in the vaccine. This primes the immune system to respond more rapidly and effectively upon future exposure to the actual pathogen.
6. Can lymphocyte levels be used to monitor the effectiveness of cancer treatments?
Yes, lymphocyte levels can be monitored during cancer treatment to assess the immune system’s response. For instance, certain immunotherapies aim to boost lymphocyte activity, and changes in lymphocyte levels may indicate how well the treatment is working.
7. Are there any genetic conditions that affect lymphocyte production or function?
Yes, several genetic disorders can impact lymphocyte production or function, such as Severe Combined Immunodeficiency (SCID) and Wiskott-Aldrich Syndrome. These conditions typically result in a compromised immune system and increased susceptibility to infections.
8. Can chronic stress cause long-term changes in lymphocyte levels?
Chronic stress can lead to sustained changes in lymphocyte levels, often resulting in immune suppression and reduced lymphocyte counts. Over time, this can make individuals more vulnerable to infections and potentially contribute to the development of chronic diseases.
9. How do lymphocyte levels change with age?
Lymphocyte levels generally decrease with age, particularly the number of naïve T cells, which can affect the body’s ability to respond to new infections. This is a natural part of the aging process, known as immunosenescence.
10. Can certain medications affect lymphocyte levels?
Yes, various medications, including immunosuppressants, corticosteroids, and certain chemotherapy drugs, can significantly affect lymphocyte levels by either reducing their production or altering their function.