The liver is a vital organ located in the right upper quadrant of the abdomen, beneath the diaphragm. It is the largest gland in the human body and plays a crucial role in various metabolic processes. The liver is responsible for detoxifying metabolites, synthesizing proteins, and producing biochemicals essential for digestion and growth. It regulates glycogen storage, decomposes red blood cells, and produces hormones. The liver generates bile, an alkaline fluid that aids in the digestion and absorption of fats. This bile is stored in the gallbladder and released into the small intestine to facilitate digestion. The liver’s specialized tissue, primarily composed of hepatocytes, manages a wide range of biochemical reactions necessary for maintaining essential bodily functions.
Description of the liver’s size and location in the body
The liver is the largest gland and internal organ in the human body, weighing between 1.2 and 1.8 kg in adults. It is located in the right upper quadrant of the abdomen, beneath the diaphragm, and extends across the midline to the left upper quadrant. The liver is protected by the rib cage and is surrounded by a thin connective tissue capsule known as Glisson’s capsule. It has a wedge-shaped structure with a convex superior surface and a flat or slightly concave inferior surface, and it is divided into two main lobes: a larger right lobe and a smaller left lobe, separated by the falciform ligament. The liver’s position can vary with body posture and respiratory movements, descending during deep inspiration and rising during expiration.
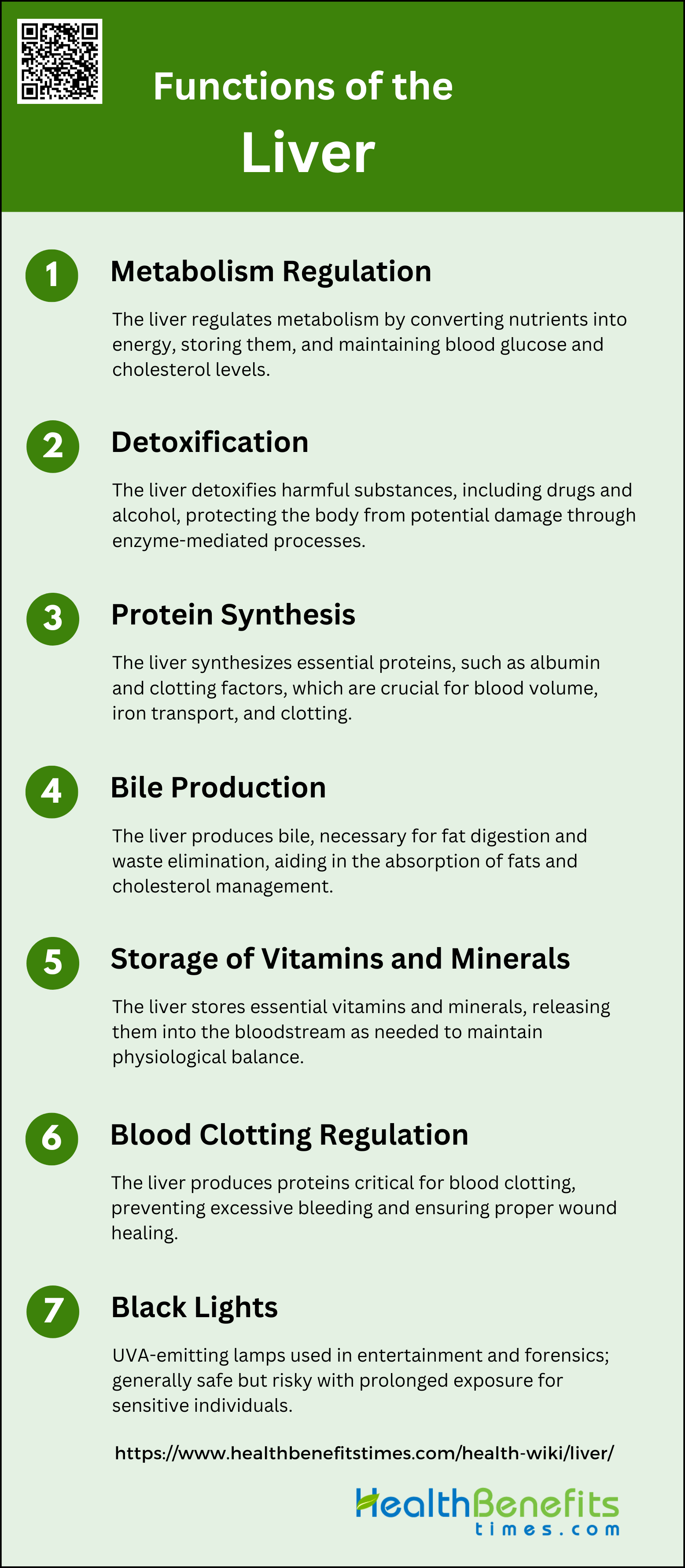
Functions of the Liver
The liver is a vital organ that performs a wide range of essential functions necessary for maintaining overall health. From regulating metabolism to detoxifying harmful substances, the liver’s roles are diverse and crucial. Below are some of the key functions of the liver:
1. Metabolism Regulation
The liver is central to the regulation of metabolism, converting nutrients from the diet into usable forms of energy and storing them for future use. It plays a crucial role in maintaining blood glucose levels through processes such as glycolysis, glycogenesis, glycogenolysis, and gluconeogenesis. Additionally, the liver metabolizes lipids, converting fatty acids into energy or storing them as triglycerides, and regulates cholesterol levels.
2. Detoxification
The liver is essential for detoxifying harmful substances, including drugs, alcohol, and other xenobiotics. It uses enzymes like P450 monooxygenases to metabolize these compounds, making them easier to excrete. This detoxification process protects the liver and the body from potential damage caused by toxic substances.
3. Protein Synthesis
The liver synthesizes a variety of essential proteins, including albumin, transferrin, and clotting factors. These proteins are crucial for various bodily functions, such as maintaining blood volume, transporting iron, and facilitating blood clotting. The liver’s ability to produce these proteins is vital for overall health and homeostasis.
4. Bile Production
The liver produces bile, which is essential for the digestion and absorption of fats. Bile acids, synthesized from cholesterol, help emulsify dietary fats, making them easier to digest. Additionally, bile aids in the elimination of waste products, including bilirubin and excess cholesterol, from the body.
5. Storage of Vitamins and Minerals
The liver stores several key vitamins and minerals, including vitamins A, D, E, K, and B12, as well as iron and copper. This storage function ensures a steady supply of these essential nutrients, which are released into the bloodstream as needed to maintain physiological balance and support various bodily functions.
6. Blood Clotting Regulation
The liver produces several proteins that are critical for blood clotting, including fibrinogen and prothrombin. These clotting factors are essential for preventing excessive bleeding and ensuring proper wound healing. The liver’s role in synthesizing these proteins is crucial for maintaining hemostasis.
7. Immune Function
The liver supports the immune system by producing immune factors and housing resident macrophages known as Kupffer cells. These cells help remove bacteria and other pathogens from the bloodstream, playing a vital role in the body’s defense mechanisms. The liver’s immune functions are essential for protecting the body from infections and maintaining overall health.
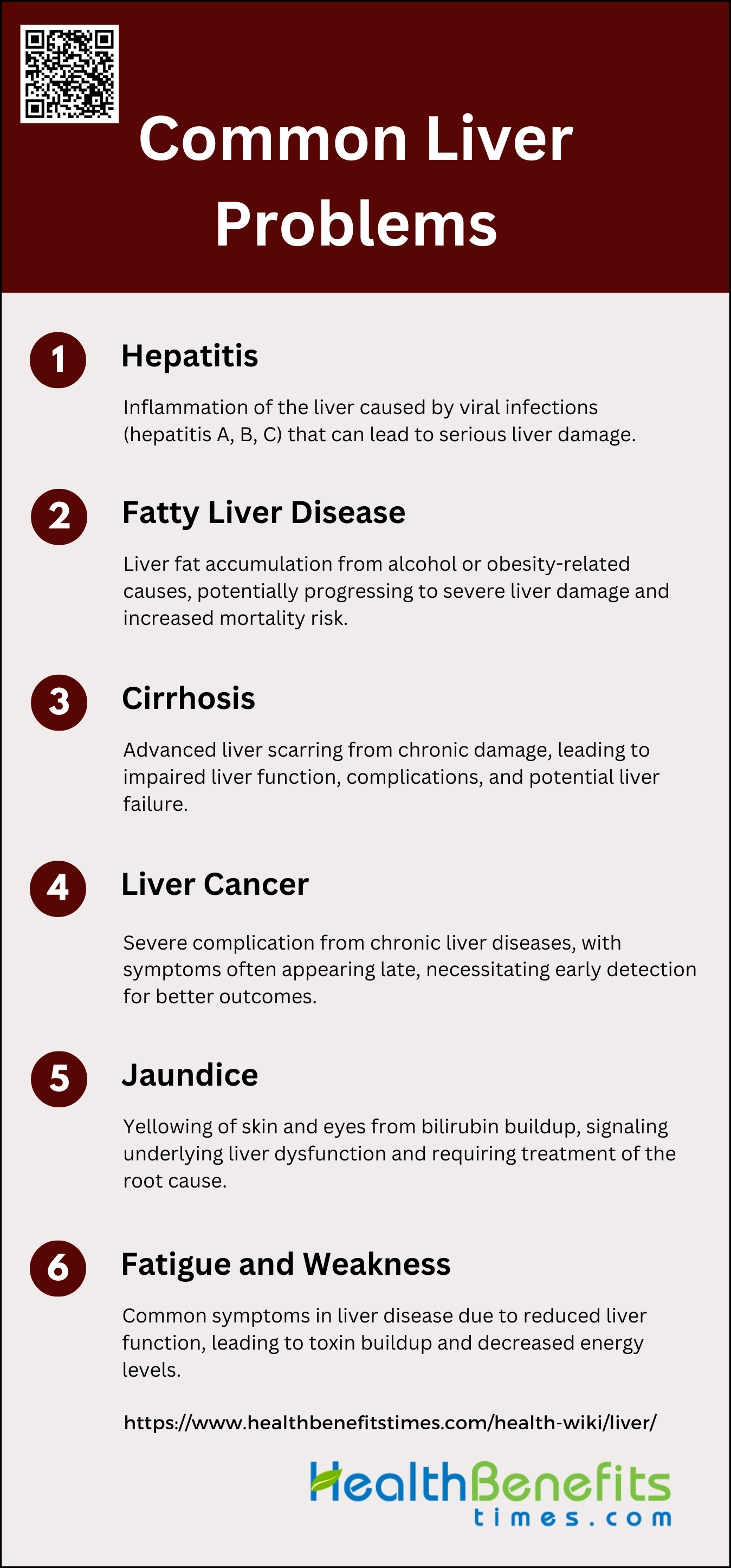
Common Liver Problems
The liver is susceptible to a variety of conditions that can impair its function and overall health. These issues can range from mild to severe and may require medical intervention. Below are some common liver problems:
1. Hepatitis
Hepatitis is an inflammation of the liver, commonly caused by viral infections, including hepatitis A, B, and C. Hepatitis A is typically spread through contaminated food and water, while hepatitis B and C are primarily transmitted through blood and bodily fluids. Symptoms of hepatitis can range from mild to severe and include jaundice (yellowing of the skin and eyes), fatigue, abdominal pain, loss of appetite, and nausea. Chronic hepatitis B and C can lead to long-term liver damage, cirrhosis, and liver cancer if left untreated.
2. Fatty Liver Disease
Non-alcoholic fatty liver disease (NAFLD) and alcoholic liver disease (ALD) are two major types of fatty liver disease. NAFLD is the most common chronic liver disease globally, often associated with obesity and type 2 diabetes, and can progress to non-alcoholic steatohepatitis (NASH), cirrhosis, and hepatocellular carcinoma. ALD results from excessive alcohol consumption, leading to liver inflammation and damage. Both conditions share overlapping pathophysiological mechanisms and can coexist, complicating diagnosis and treatment. The progression of these diseases can result in significant liver damage and increased risk of liver-related mortality.
3. Cirrhosis
Cirrhosis is the advanced scarring of the liver caused by long-term liver damage from conditions such as chronic hepatitis, NAFLD, and ALD. It develops as the liver attempts to repair itself, leading to the formation of scar tissue that impairs liver function. Complications of cirrhosis include portal hypertension, liver failure, and an increased risk of liver cancer. Symptoms may include jaundice, fatigue, easy bruising, and fluid accumulation in the abdomen (ascites). Early detection and management of underlying causes are crucial to prevent the progression of cirrhosis and its associated complications.
4. Liver Cancer
Liver cancer, particularly hepatocellular carcinoma (HCC), is a severe complication of chronic liver diseases such as hepatitis B and C, NAFLD, and ALD. Risk factors for liver cancer include chronic viral hepatitis, cirrhosis, obesity, type 2 diabetes, and excessive alcohol consumption. Symptoms of liver cancer often appear in advanced stages and may include weight loss, loss of appetite, upper abdominal pain, and jaundice. Early detection through regular monitoring of at-risk individuals is essential for improving treatment outcomes and survival rates.
5. Jaundice
Jaundice is a condition characterized by the yellowing of the skin and eyes due to the accumulation of bilirubin, a byproduct of red blood cell breakdown. It is often a symptom of underlying liver problems, such as hepatitis, cirrhosis, or bile duct obstruction. Jaundice can indicate liver dysfunction, as the liver is responsible for processing and excreting bilirubin. In addition to yellowing of the skin and eyes, symptoms may include dark urine, pale stools, and itching. Addressing the underlying cause of jaundice is crucial for effective treatment and management.
6. Fatigue and Weakness
Fatigue and weakness are common symptoms associated with various liver diseases, including hepatitis, NAFLD, ALD, and cirrhosis. These symptoms result from the liver’s reduced ability to perform its essential functions, such as detoxification, metabolism, and energy production. Chronic liver disease can lead to a buildup of toxins in the body, contributing to feelings of tiredness and muscle weakness. Managing the underlying liver condition and maintaining a healthy lifestyle can help alleviate these symptoms and improve overall quality of life.
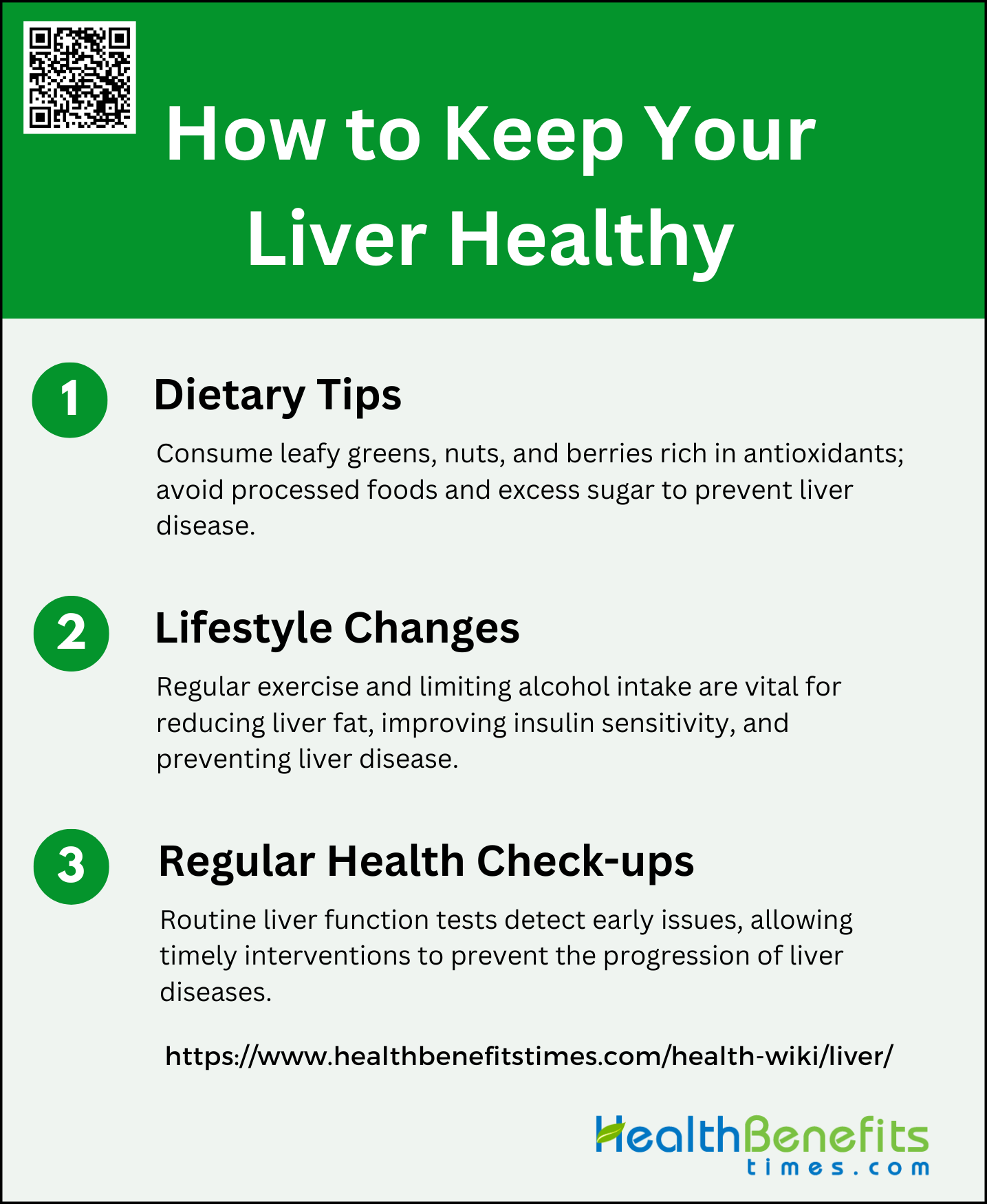
How to Keep Your Liver Healthy
Maintaining liver health is crucial for overall well-being, as the liver performs many vital functions. Adopting healthy lifestyle habits can significantly reduce the risk of liver diseases. Below are some tips on how to keep your liver healthy:
1. Dietary Tips
To maintain a healthy liver, incorporating specific foods into your diet is essential. Leafy greens, nuts, and berries are particularly beneficial due to their high content of antioxidants and essential nutrients. Leafy greens like spinach and kale are rich in vitamins and minerals that support liver function. Nuts, especially those high in unsaturated fats, can help reduce liver fat and improve overall liver health. Berries, rich in polyphenols, have anti-inflammatory properties that can protect the liver from damage. Conversely, it is crucial to avoid processed foods and excessive sugar, as these can lead to the development of non-alcoholic fatty liver disease (NAFLD) and other metabolic disorders.
2. Lifestyle Changes
Regular exercise is vital for maintaining liver health. Physical activity helps reduce liver fat and improves insulin sensitivity, which is crucial for preventing and managing liver diseases such as NAFLD. Engaging in regular exercise, whether through aerobic activities or resistance training, can significantly lower liver enzyme levels and reduce inflammation. Additionally, limiting alcohol intake is essential, as excessive alcohol consumption can lead to liver cirrhosis and other severe liver conditions. By adopting a balanced lifestyle that includes regular exercise and moderate alcohol consumption, you can significantly enhance your liver’s health and functionality.
3. Regular Health Check-ups
Regular health check-ups, including liver function tests, are crucial for early detection and management of liver issues. Liver function tests measure enzymes and proteins in the blood that indicate how well the liver is working. Early detection of abnormalities can lead to timely interventions, preventing the progression of liver diseases. Monitoring for early signs of liver issues, such as jaundice, fatigue, and abdominal pain, can also prompt early medical consultation and treatment. Regular check-ups and monitoring are essential components of a proactive approach to maintaining liver health and preventing severe liver conditions.
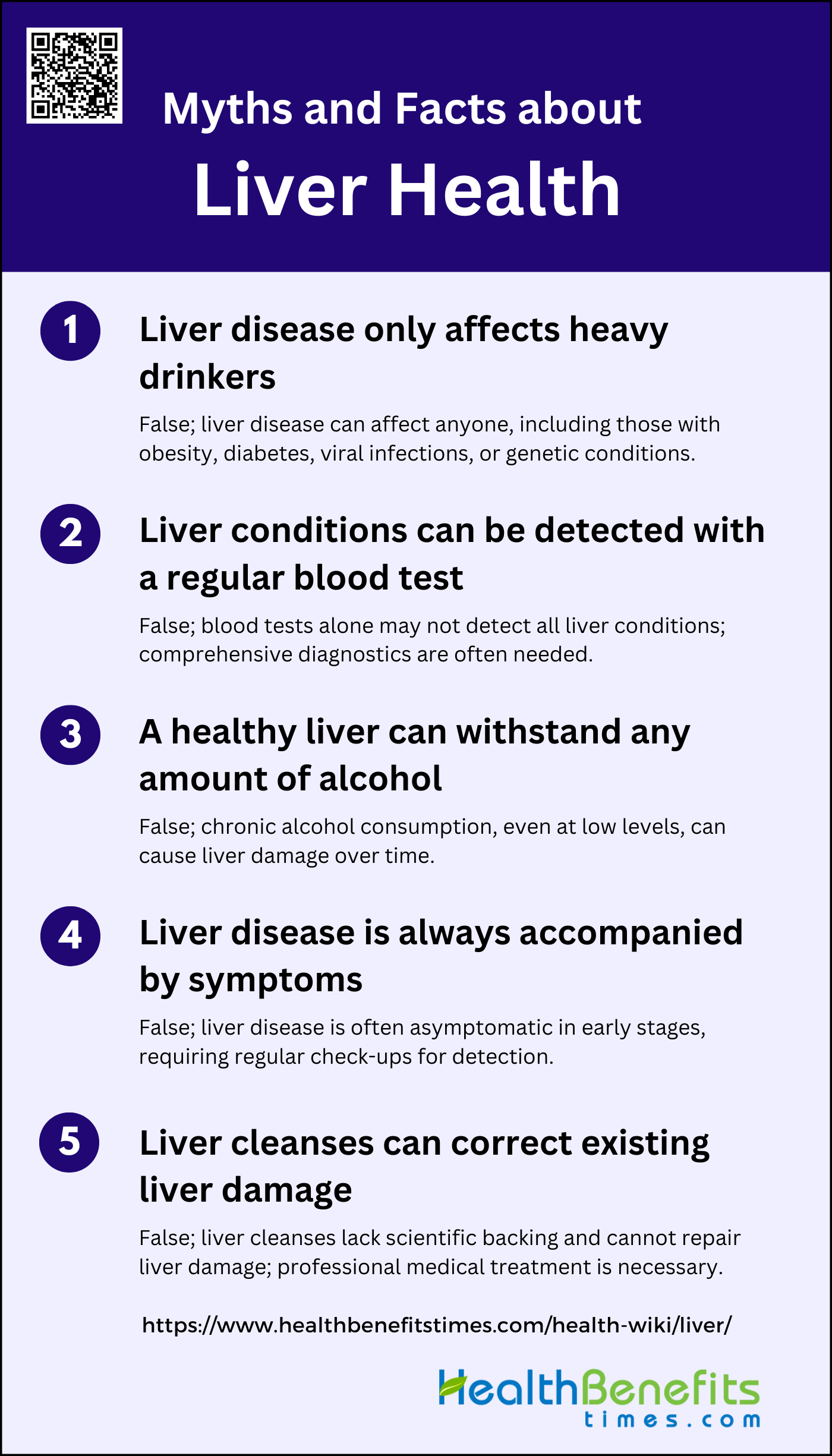
Myths and Facts about Liver Health
There are many misconceptions surrounding liver health that can lead to confusion and misinformation. Understanding the facts is essential for maintaining a healthy liver. Below are some common myths and facts about liver health:
1. Liver disease only affects heavy drinkers
This is a common misconception. While excessive alcohol consumption is a significant risk factor for liver disease, it is not the only cause. Non-alcoholic fatty liver disease (NAFLD), now referred to as metabolic dysfunction-associated steatotic liver disease (MASLD), is prevalent and linked to obesity and type 2 diabetes, affecting a significant portion of the population. Additionally, liver diseases can arise from viral infections, genetic factors, and autoimmune conditions. Therefore, liver disease can affect individuals regardless of their alcohol consumption habits.
2. Liver conditions can be detected with a regular blood test
While regular blood tests can provide some insights into liver health by measuring liver enzymes, they are not always sufficient to detect all liver conditions. Specific tests, such as liver function tests, can indicate liver inflammation or damage, but they may not reveal the underlying cause or severity. More comprehensive diagnostic methods, like imaging studies or liver biopsies, are often necessary for a definitive diagnosis. Non-invasive tests, like the OWLiver serum lipidomics test, are also being used to assess liver health more accurately.
3. A healthy liver can withstand any amount of alcohol
This is a myth. While the liver is resilient and capable of regenerating, it has its limits. Chronic alcohol consumption, even at low levels, can lead to liver damage over time. There is no universally safe threshold for alcohol consumption that guarantees liver health, as individual risk can vary based on factors like genetics, sex, and overall health. Continued alcohol use can lead to conditions such as alcoholic liver disease, which progresses from fatty liver to fibrosis and cirrhosis.
4. Liver disease is always accompanied by symptoms
Liver disease is often asymptomatic in its early stages, making it difficult to detect without medical testing. Many individuals may not experience noticeable symptoms until the disease has progressed significantly. Conditions like non-alcoholic fatty liver disease (NAFLD) and spontaneous bacterial peritonitis can be present without obvious symptoms. Therefore, regular medical check-ups and screenings are crucial for early detection and management of liver diseases, even in the absence of symptoms.
5. Liver cleanses can correct existing liver damage
Liver cleanses and detox diets are popular but lack scientific evidence to support their effectiveness in repairing liver damage. The liver is naturally capable of detoxifying and regenerating itself without the need for special diets or supplements. While maintaining a healthy lifestyle, including a balanced diet and regular exercise, can support liver health, it is not a substitute for medical treatment in cases of liver damage. Consulting healthcare professionals for appropriate diagnosis and treatment is essential for managing liver conditions effectively.
FAQs
1. What are the early signs of liver disease?
Early signs of liver disease can include fatigue, weakness, nausea, loss of appetite, and unexplained weight loss. More specific symptoms can include dark urine, pale stools, and itching.
2. How does obesity affect liver health?
Obesity can lead to non-alcoholic fatty liver disease (NAFLD), which increases the risk of liver inflammation, fibrosis, and eventually cirrhosis and liver cancer. It also contributes to insulin resistance, further complicating liver function.
3. Are there specific foods that can harm the liver?
Foods high in saturated fats, trans fats, added sugars, and refined carbohydrates can contribute to liver damage and fatty liver disease. Processed foods and excessive salt intake should also be minimized.
4. How does hydration impact liver function?
Staying well-hydrated supports liver function by aiding in detoxification processes and bile production. Dehydration can impair the liver’s ability to function optimally.
5. What role does sleep play in liver health?
Adequate sleep is essential for overall health, including liver function. Poor sleep quality or sleep disorders can disrupt metabolic processes and may contribute to conditions like fatty liver disease.
6. Can liver problems affect mental health?
Yes, liver disease can lead to complications such as hepatic encephalopathy, which affects brain function and can cause cognitive issues. Additionally, chronic illness can impact mental health by increasing the risk of depression and anxiety.
7. What is the link between diabetes and liver health?
Individuals with diabetes are at higher risk for developing liver conditions like NAFLD. Insulin resistance, a common factor in type 2 diabetes, can lead to fat accumulation in the liver.
8. How often should one get liver function tests?
The frequency of liver function tests varies based on individual risk factors. People with liver disease or those at high risk (e.g., due to obesity, diabetes, or heavy alcohol use) may require more frequent testing. Consulting a healthcare provider is essential for personalized recommendations.
9. Can herbal supplements support liver health?
Certain herbal supplements, like milk thistle and dandelion root, are believed to support liver health. However, it’s crucial to consult a healthcare provider before using any supplements, as they can interact with medications or exacerbate liver issues.
10. Is it safe to take pain relievers with liver disease?
Some pain relievers, particularly acetaminophen, can be harmful to individuals with liver disease, as they are metabolized by the liver. It’s essential to consult a healthcare professional for safe pain management options.