Lipid peroxidation is a biochemical process in which free radicals, particularly reactive oxygen species (ROS), attack lipids containing carbon-carbon double bonds, especially polyunsaturated fatty acids, in cell membranes. This oxidative degradation leads to the formation of lipid peroxides, which can further decompose into reactive aldehydes such as malondialdehyde (MDA) and 4-hydroxynonenal (4-HNE). These products can cause significant cellular damage, affecting membrane integrity, fluidity, and function, and can contribute to various pathological conditions, including inflammation, atherosclerosis, and neurodegenerative diseases. Lipid peroxidation is also a key feature in the process of ferroptosis, an iron-dependent form of cell death characterized by the accumulation of lipid peroxides.
Types of Lipids Involved in Lipid Peroxidation
Lipid peroxidation primarily affects polyunsaturated fatty acids (PUFAs) due to their multiple double bonds, which are highly susceptible to oxidative attack. These lipids are crucial components of cell membranes and play vital roles in maintaining cellular structure and function. Below are the main types of lipids involved in lipid peroxidation:
1. Polyunsaturated Fatty Acids (PUFAs)
Polyunsaturated fatty acids (PUFAs) are highly susceptible to lipid peroxidation due to their multiple double bonds, which are prone to attack by free radicals. This susceptibility makes PUFAs a significant focus in studies of oxidative stress and lipid peroxidation. Lipid peroxidation of PUFAs leads to the formation of lipid hydroperoxides, which can further degrade into reactive aldehydes such as 4-hydroxy-2-nonenal (4-HNE) and malondialdehyde (MDA). These products can diffuse within or escape from the cell, attacking various biomolecules and potentially leading to cellular damage and disease. Despite their vulnerability, PUFAs play crucial roles in cell signaling, membrane structure, and energy provision, highlighting the dual nature of their biological effects.
2. Phospholipids
Phospholipids, particularly those containing PUFAs, are integral components of cell membranes and are highly susceptible to lipid peroxidation. The oxidation of phospholipids can significantly alter membrane properties, leading to changes in membrane fluidity, permeability, and the function of membrane-bound proteins. Phospholipid oxidation products, such as hydroxy-alkenals, can form covalent adducts with proteins and other lipids, affecting cellular signaling and gene expression. The presence of antioxidants like alpha-tocopherol in phospholipid domains can mitigate these effects by protecting against oxidative damage. The distribution of phospholipids within the membrane can influence their susceptibility to peroxidation, with non-raft domains being more accessible to molecular oxygen and thus more prone to oxidation.
3. Cholesterol
Cholesterol is another lipid that undergoes peroxidation, although it is less susceptible than PUFAs. Cholesterol oxidation products, such as oxysterols, can be formed through both enzymatic and non-enzymatic mechanisms. These products can disrupt membrane structure and function, contributing to the pathogenesis of diseases like atherosclerosis and neurodegenerative disorders. Cholesterol’s role in lipid rafts, which are membrane microdomains enriched in cholesterol and sphingolipids, also affects its susceptibility to peroxidation. These rafts are less permeable to oxygen, potentially reducing the rate of cholesterol oxidation compared to other membrane regions. However, the extreme reactivity of certain cholesterol precursors, like 7-dehydrocholesterol, underscores the importance of understanding cholesterol peroxidation in health and disease.
4. Glycolipids
Glycolipids, which consist of a lipid moiety linked to a carbohydrate, are also susceptible to lipid peroxidation, although they are less studied compared to PUFAs and phospholipids. The oxidation of glycolipids can lead to the formation of reactive aldehydes and other oxidative products that can affect cellular functions and signaling pathways. Glycolipids are important components of cell membranes, particularly in the outer leaflet, and their oxidation can disrupt membrane integrity and cellular communication. The role of glycolipids in lipid rafts, similar to cholesterol, may influence their susceptibility to peroxidation and the subsequent biological effects. Understanding the peroxidation of glycolipids is crucial for elucidating their role in oxidative stress-related diseases and developing targeted antioxidant therapies.
The Process of Lipid Peroxidation
Lipid peroxidation is a crucial biochemical process involving the oxidative degradation of lipids. This process can lead to cell damage and is implicated in various diseases. Understanding the steps involved is essential for comprehending its impact on health.
1. Initiation
Lipid peroxidation begins when free radicals or reactive oxygen species (ROS) attack lipids containing carbon-carbon double bonds, particularly polyunsaturated fatty acids (PUFAs). Common initiators include superoxide radicals, perhydroxyl radicals, and hydroxyl radicals, which can be generated through various enzymatic and non-enzymatic reactions. For instance, the iron-catalyzed Fenton reaction produces hydroxyl radicals that initiate lipid peroxidation by abstracting hydrogen atoms from PUFAs, forming lipid radicals. Additionally, hydrogen peroxide, produced by superoxide dismutation or enzymatic reactions, plays a crucial role in generating these initiating radicals.
2. Propagation
Once initiated, lipid peroxidation propagates through a chain reaction where lipid radicals react with molecular oxygen to form lipid peroxyl radicals. These peroxyl radicals can further react with other lipids, perpetuating the cycle and spreading the peroxidation process. The presence of lipid hydroperoxides (LOOH) significantly enhances propagation, as they break down to form more reactive intermediates. Factors such as the composition of fatty acyl chains and the structural properties of lipid membranes influence the rate of propagation. NADPH-dependent lipid peroxidation exemplifies this, where iron-catalyzed breakdown of LOOH leads to rapid formation of reactive products.
3. Termination
The lipid peroxidation process is terminated when antioxidants neutralize the free radicals, preventing further propagation. Antioxidants like Vitamin E, superoxide dismutase (SOD), and catalase play a critical role in quenching lipid peroxyl radicals and other reactive species, thereby stopping the chain reaction. Sphingomyelins in biological membranes also act as “biophysical antioxidants,” forming hydrogen-bond networks that inhibit peroxidation propagation. The balance between free radical generation and antioxidant defense is crucial for controlling lipid peroxidation and preventing cellular damage.
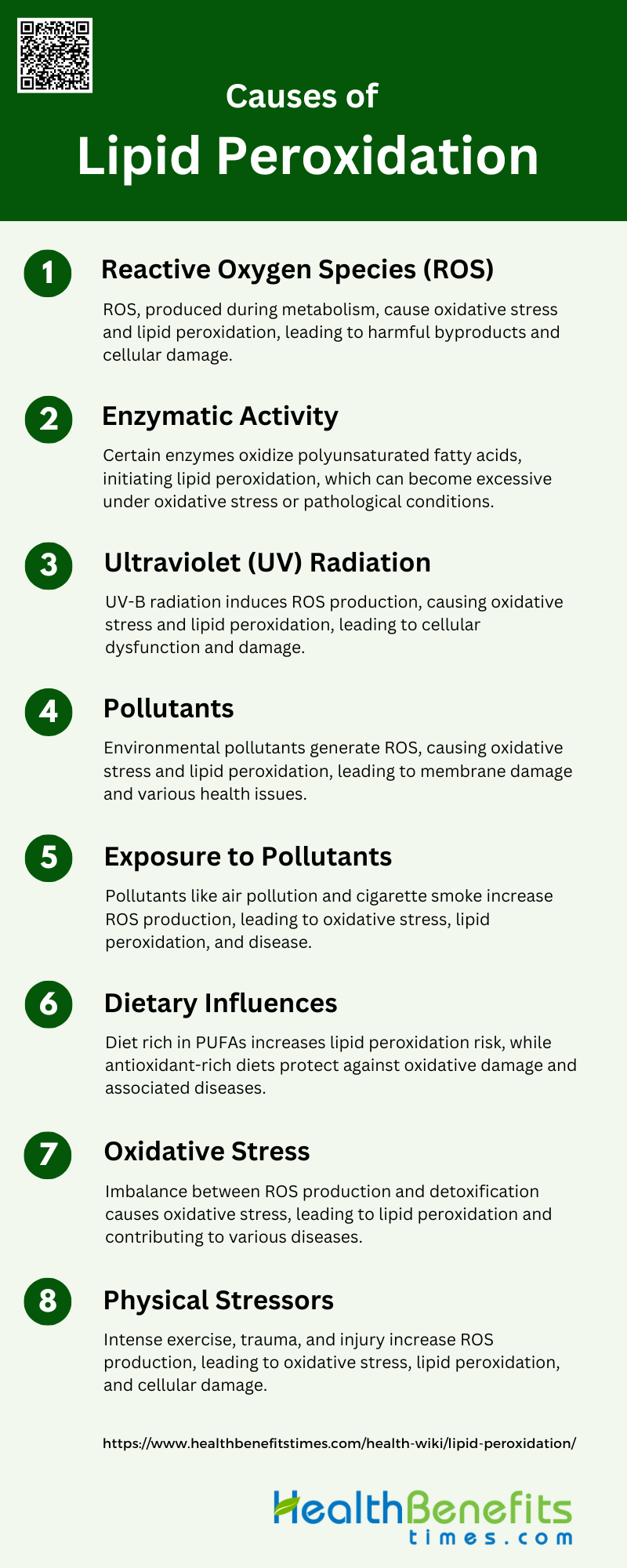
Causes of Lipid Peroxidation
Lipid peroxidation is primarily driven by oxidative stress, which results from an imbalance between free radicals and antioxidants in the body. Various factors contribute to this process, leading to cellular damage and disease progression. Here are the key causes:
1. Reactive Oxygen Species (ROS)
Reactive oxygen species (ROS) are highly reactive molecules produced in cells through various metabolic processes, such as oxidative phosphorylation in the mitochondrial respiratory chain and the activity of NAD(P)H oxidases. When ROS production exceeds the cell’s antioxidant defenses, oxidative stress occurs, leading to cellular damage. ROS can react with lipids, causing lipid peroxidation, which results in the formation of harmful products like 4-hydroxynonenal and malondialdehyde. These products can disrupt cellular membranes and contribute to cell death and various diseases, including neurodegenerative disorders and cardiovascular diseases.
2. Enzymatic Activity
Lipid peroxidation can also be initiated by enzymatic activity. Enzymes such as lipoxygenases, cyclooxygenases, and cytochrome P450 enzymes can catalyze the oxidation of polyunsaturated fatty acids, leading to the formation of lipid peroxides. These enzymatic reactions are tightly regulated under normal physiological conditions to maintain cellular homeostasis. However, during oxidative stress or pathological conditions, the activity of these enzymes can become dysregulated, resulting in excessive lipid peroxidation and subsequent cellular damage. This enzymatic lipid peroxidation plays a role in various diseases, including inflammation and cancer.
3. Ultraviolet (UV) Radiation
Ultraviolet (UV) radiation, particularly UV-B, can induce the production of ROS in cells, leading to oxidative stress and lipid peroxidation. UV-B radiation causes the formation of ROS such as superoxide and hydrogen peroxide, which can damage cellular components, including lipids. This oxidative damage results in the formation of lipid peroxides and other harmful byproducts, contributing to cellular dysfunction and death. Protective agents like ascorbic acid can mitigate the effects of UV-induced lipid peroxidation by scavenging ROS and enhancing cellular antioxidant defenses.
4. Pollutants
Environmental pollutants, including heavy metals, pesticides, and industrial chemicals, can induce lipid peroxidation by generating ROS. These pollutants can disrupt cellular redox balance, leading to oxidative stress and the formation of lipid peroxides. The oxidative damage caused by pollutants can alter membrane integrity, protein function, and DNA structure, contributing to various health issues such as respiratory diseases, cardiovascular disorders, and cancer. Understanding the mechanisms by which pollutants induce lipid peroxidation is crucial for developing strategies to mitigate their harmful effects6.
5. Exposure to Pollutants
Exposure to environmental pollutants, such as air pollution and cigarette smoke, can significantly increase the production of ROS, leading to oxidative stress and lipid peroxidation. These pollutants contain reactive chemicals that can directly or indirectly generate ROS, causing damage to cellular lipids. The resulting lipid peroxidation products can disrupt cellular membranes and contribute to the pathogenesis of diseases like chronic obstructive pulmonary disease (COPD), asthma, and cardiovascular diseases. Antioxidant defenses play a critical role in protecting cells from pollutant-induced oxidative damage.
6. Dietary Influences
Dietary factors can influence lipid peroxidation through the intake of antioxidants and pro-oxidants. Diets rich in polyunsaturated fatty acids (PUFAs) are more susceptible to lipid peroxidation due to the high reactivity of PUFAs with ROS. Conversely, diets high in antioxidants, such as vitamins C and E, can protect against lipid peroxidation by scavenging ROS and enhancing the body’s antioxidant defenses. The balance between pro-oxidant and antioxidant intake is crucial in modulating lipid peroxidation and its associated health effects, including inflammation and chronic diseases.
7. Oxidative Stress
Oxidative stress occurs when there is an imbalance between the production of ROS and the body’s ability to detoxify them through antioxidant defenses. This imbalance leads to the accumulation of ROS, which can initiate lipid peroxidation. The resulting lipid peroxides and their byproducts can cause significant cellular damage, contributing to the development of various diseases, including neurodegenerative disorders, cardiovascular diseases, and cancer. Enhancing antioxidant defenses through diet, lifestyle changes, and pharmacological interventions can help mitigate oxidative stress and its harmful effects.
8. Physical Stressors
Physical stressors, such as intense exercise, trauma, and ischemia-reperfusion injury, can lead to increased ROS production and subsequent lipid peroxidation. During intense physical activity or injury, the elevated oxygen consumption and metabolic rate can overwhelm the body’s antioxidant defenses, resulting in oxidative stress. The lipid peroxidation products generated can damage cellular membranes, proteins, and DNA, impairing cellular function and contributing to inflammation and tissue damage. Strategies to enhance antioxidant defenses and reduce oxidative stress are important in managing the effects of physical stressors.
Biological Implications of Lipid Peroxidation
Lipid peroxidation has significant biological consequences, affecting cellular integrity and function. It plays a critical role in the pathogenesis of various diseases and aging processes. Here are two types of primary biological implications:
1. Cell Membrane Damage
Lipid peroxidation (LPO) significantly impacts cellular membranes by altering their structural integrity and function. The oxidation of membrane lipids, particularly polyunsaturated fatty acids, leads to the formation of lipid peroxides and reactive aldehydes such as 4-hydroxy-2-nonenal (HNE) and malondialdehyde. These products disrupt membrane fluidity, increase permeability, and affect lipid-lipid and lipid-protein interactions, ultimately compromising membrane stability and function. The resulting changes in membrane properties can impair ion and nutrient transport, disrupt signaling pathways, and lead to cell death. Additionally, lipid peroxidation can cause phase separation in membranes, further disturbing the organization and function of membrane domains.
2. Impact on Cellular Components
Lipid peroxidation products, such as reactive aldehydes, can covalently modify proteins, DNA, and other cellular components, leading to significant cellular damage. These modifications can result in protein dysfunction, DNA mutations, and impaired cellular signaling. The accumulation of such damage contributes to cellular aging and the pathogenesis of various diseases, including neurodegenerative disorders like Alzheimer’s disease. Moreover, lipid peroxidation can induce oxidative stress, which further exacerbates cellular damage and promotes inflammatory and apoptotic pathways. The genotoxic effects of lipid peroxidation products highlight their role in disease progression and the importance of maintaining redox homeostasis to prevent cellular dysfunction.
Impact of Lipid Peroxidation on Health
Lipid peroxidation significantly affects overall health by contributing to the development and progression of various diseases. This oxidative process can lead to cellular dysfunction and chronic health conditions. Here are the key health impacts:
1. Cellular Damage and Dysfunction
Lipid peroxidation (LPO) can significantly disrupt cellular function by altering membrane organization and damaging vital proteins and DNA. This process is initiated by various oxidants, including reactive oxygen species (ROS) and environmental pollutants, leading to cellular dysfunction and widespread tissue damage if unchecked. The products of LPO, such as 4-hydroxy-2-nonenal (HNE) and malondialdehyde (MDA), are highly reactive and can modify cellular components, resulting in cytotoxicity and loss of cellular integrity. However, at sublethal concentrations, LPO products can induce adaptive responses, enhancing cellular tolerance against oxidative stress.
2. DNA and Protein Adducts
Lipid peroxidation generates reactive aldehydes like HNE, MDA, and acrolein, which can form adducts with DNA and proteins, leading to mutagenic and carcinogenic effects. These adducts can cause significant DNA damage, contributing to the pathogenesis of various malignancies and degenerative diseases. The formation of exocyclic DNA adducts by these reactive aldehydes is a critical factor in the mutagenic processes associated with oxidative stress-induced LPO. Additionally, these adducts can induce epigenetic changes, further modulating inflammatory processes and potentially leading to autoimmunity.
3. Neurodegenerative Diseases
The brain is particularly susceptible to oxidative damage due to its high lipid content and oxygen consumption. Lipid peroxidation in the central nervous system (CNS) is linked to various neurodegenerative diseases, including Alzheimer’s disease, Parkinson’s disease, and multiple sclerosis. The reactive products of LPO, such as HNE, can modify proteins and disrupt cellular processes, contributing to neurodegeneration. Research has shown that oxidative stress and LPO are common themes in the altered energy metabolism and mitochondrial dysfunction observed in these disorders.
4. Cardiovascular Diseases
Lipid peroxidation plays a significant role in the development of cardiovascular diseases, such as atherosclerosis and hypertension. The oxidation of low-density lipoprotein (LDL) leads to the formation of foam cells and plaque development in arteries, a hallmark of atherosclerosis. Reactive products of LPO, including isolevuglandins (isoLGs), contribute to oxidative stress, inflammation, and endothelial dysfunction, exacerbating cardiovascular conditions. The involvement of LPO in these processes underscores its importance in the pathogenesis of cardiovascular diseases.
5. Inflammatory and Immune Responses
Lipid peroxidation products are implicated in the regulation of oxidative, immune, and inflammatory responses. Reactive aldehydes produced by LPO can modify cellular biomolecules, leading to the activation of inflammatory pathways and immune responses. These modifications can result in the formation of biomarkers for oxidative stress and inflammation, such as chlorinated phospholipids, which are associated with diseases like atherosclerosis and arthritis. Understanding the role of LPO in these processes is crucial for developing therapeutic strategies to mitigate inflammation and immune-related diseases.
6. Metabolic Disorders
Lipid peroxidation is also linked to metabolic disorders, including obesity and diabetes. The reactive products of LPO, such as isoLGs, contribute to oxidative stress, mitochondrial dysfunction, and inflammation, which are key factors in the development of these conditions. The formation of LPO products can disrupt cellular homeostasis and metabolic processes, leading to insulin resistance and other metabolic abnormalities. Addressing the impact of LPO on metabolic health is essential for understanding and managing these disorders.
Measuring Lipid Peroxidation
Techniques Used to Measure Lipid Peroxidation Levels
Lipid peroxidation levels are commonly measured using various analytical techniques, each with its own advantages and limitations. High-performance liquid chromatography (HPLC) is frequently employed for the determination of malondialdehyde (MDA), a key biomarker of lipid peroxidation, due to its sensitivity and reproducibility. Gas chromatography-mass spectrometry (GC-MS) is another powerful technique used to quantify lipid peroxidation products such as 4-hydroxynonenal (4-HNE) and F2-isoprostanes, offering high specificity and sensitivity. Colorimetric assays, which involve the reaction of MDA and 4-HNE with specific reagents to produce a chromophore, are also used for their simplicity and cost-effectiveness, although they may lack the specificity of chromatographic methods9. Immunoassays, particularly for F2-isoprostanes, provide a simpler alternative but may suffer from lower specificity compared to chromatographic techniques. Inter-laboratory studies have shown that HPLC-based methods for MDA measurement are particularly reliable for consistent results across different settings.
Important Biomarkers
Malondialdehyde (MDA) and 4-hydroxynonenal (4-HNE) are among the most important biomarkers for assessing lipid peroxidation. MDA is a well-established marker, often measured as thiobarbituric acid reactive substances (TBARS), and is produced from the oxidation of polyunsaturated fatty acids (PUFAs). It forms Schiff-base adducts with lysine residues, which can be quantified using various analytical methods. 4-HNE, another significant biomarker, is a breakdown product of fatty acid hydroperoxides and reacts with lysine residues primarily via Michael addition reactions. F2-isoprostanes, derived from arachidonic acid, are considered highly specific markers of lipid peroxidation and oxidative stress, although their measurement can be technically challenging. These biomarkers are crucial for understanding the extent of oxidative stress in various pathological conditions and are often measured in biological fluids such as plasma and urine. The choice of biomarker and analytical method can significantly impact the reliability and specificity of lipid peroxidation assessments.
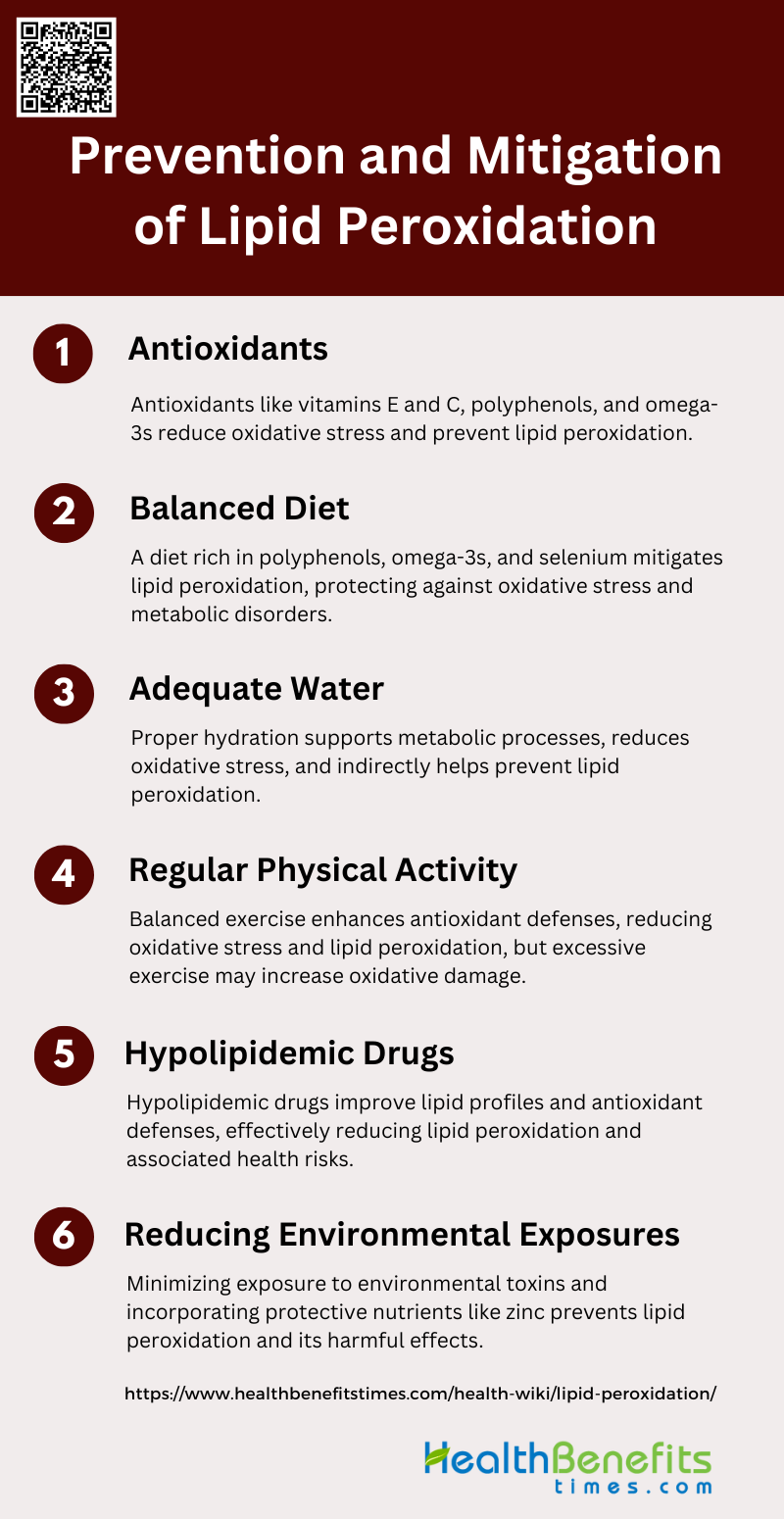
Prevention and Mitigation of Lipid Peroxidation
Preventing and mitigating lipid peroxidation is essential for maintaining cellular health and reducing the risk of chronic diseases. Effective strategies focus on enhancing antioxidant defenses and minimizing oxidative stress. Here are some key approaches:
1. Antioxidants
Antioxidants play a crucial role in preventing lipid peroxidation by neutralizing free radicals and reducing oxidative stress. For instance, pomegranate juice (PJ) supplementation has been shown to significantly reduce macrophage lipid peroxide content and oxidative stress in atherosclerotic mice, thereby attenuating the development of atherosclerosis. Similarly, vitamins E and C supplementation in ultramarathon runners prevented exercise-induced lipid peroxidation, although it did not affect inflammation markers. Additionally, a nutrient cocktail containing polyphenols, omega-3 fatty acids, vitamin E, and selenium was effective in preventing metabolic alterations and lipid peroxidation induced by physical inactivity and fructose overfeeding. These findings underscore the importance of antioxidants in mitigating lipid peroxidation and associated health risks.
2. Balanced Diet
A balanced diet rich in essential nutrients can significantly mitigate lipid peroxidation and its adverse effects. For example, a nutrient cocktail composed of polyphenols, omega-3 fatty acids, vitamin E, and selenium was found to prevent hypertriglyceridemia and lipid peroxidation in individuals subjected to physical inactivity and fructose overfeeding. Moreover, quercetin, a naturally occurring flavonoid, demonstrated protective effects against ethanol-induced dyslipidemia and oxidative damage, particularly in hepatic mitochondria. Enhanced zinc consumption also showed protective effects against cadmium-induced lipid peroxidation and hyperlipidemia in rats. These studies highlight the role of a balanced diet in maintaining lipid metabolism and preventing oxidative stress.
3. Adequate Water
Adequate water intake is essential for maintaining overall health, including lipid metabolism and oxidative stress management. While specific studies directly linking water intake to lipid peroxidation are limited, hydration is known to support metabolic processes and the elimination of toxins, which can indirectly reduce oxidative stress. For instance, pomegranate juice, which is primarily water, was effective in reducing oxidative stress and lipid peroxidation in atherosclerotic mice. Proper hydration ensures efficient cellular function and can help mitigate the effects of oxidative stress, thereby preventing lipid peroxidation.
4. Regular Physical Activity
Regular physical activity is a well-established method for reducing oxidative stress and lipid peroxidation. A systematic review and network meta-analysis found that a combination of aerobic exercise and low-intensity resistance training significantly dampened cellular lipid peroxidation in elderly individuals. Exercise enhances antioxidant defenses and improves lipid metabolism, thereby reducing the risk of oxidative damage. However, it is important to note that excessive exercise without adequate antioxidant support can increase lipid peroxidation, as observed in ultramarathon runners. Therefore, balanced physical activity combined with proper nutrition is essential for optimal health.
5. Hypolipidemic Drugs
Hypolipidemic drugs can effectively reduce lipid peroxidation by improving lipid profiles and enhancing antioxidant defenses. For instance, lipoic acid (LA) supplementation in high-fat diet-fed mice resulted in decreased lipid peroxidation and improved lipid profiles by modulating gene expression related to lipid metabolism and antioxidant enzymes. Similarly, quercetin demonstrated hypolipidemic and antioxidative effects in ethanol-induced dyslipidemia and oxidative damage. These drugs can be a valuable addition to lifestyle modifications for preventing lipid peroxidation and associated diseases.
6. Reducing Environmental Exposures
Reducing environmental exposures to toxic substances can significantly prevent lipid peroxidation and its harmful effects. Enhanced zinc consumption was shown to prevent cadmium-induced alterations in lipid metabolism and lipid peroxidation in rats, highlighting the protective role of zinc against environmental toxins. Additionally, a study on overweight and obese individuals found that supplementation with epigallo catechin-3-gallate (EGCG) and N-oleoyl-phosphatidylethanolamine (NOPE) improved oxidative stress markers, suggesting that dietary interventions can mitigate the effects of environmental stressors. These findings emphasize the importance of minimizing exposure to environmental toxins to protect against oxidative damage and lipid peroxidation.