Kidney disease, also known as renal disease, encompasses a range of conditions that impair kidney function. Chronic Kidney Disease (CKD) is characterized by a gradual loss of kidney function over time, typically defined by a decreased glomerular filtration rate (GFR) or evidence of kidney damage, such as albuminuria, persisting for at least three months. Acute Kidney Disease (AKD), on the other hand, involves a rapid decline in kidney function. CKD can lead to severe complications, including cardiovascular disease, kidney failure, and premature death. Early detection and management are crucial to slowing disease progression and mitigating associated health risks.
Basic anatomy of the kidneys and its functions
Each kidney contains over a million nephrons, which are the functional units that filter blood and produce urine. The kidneys regulate various bodily functions, including acid-base balance, blood pressure, and electrolyte balance, by filtering metabolic wastes and toxins from the blood and reabsorbing necessary substances. They also play a crucial role in the production of erythropoietin, which stimulates red blood cell production, and in the activation of vitamin D, which is essential for bone health. The kidneys receive a significant portion of the cardiac output, highlighting their importance in maintaining overall physiological balance.
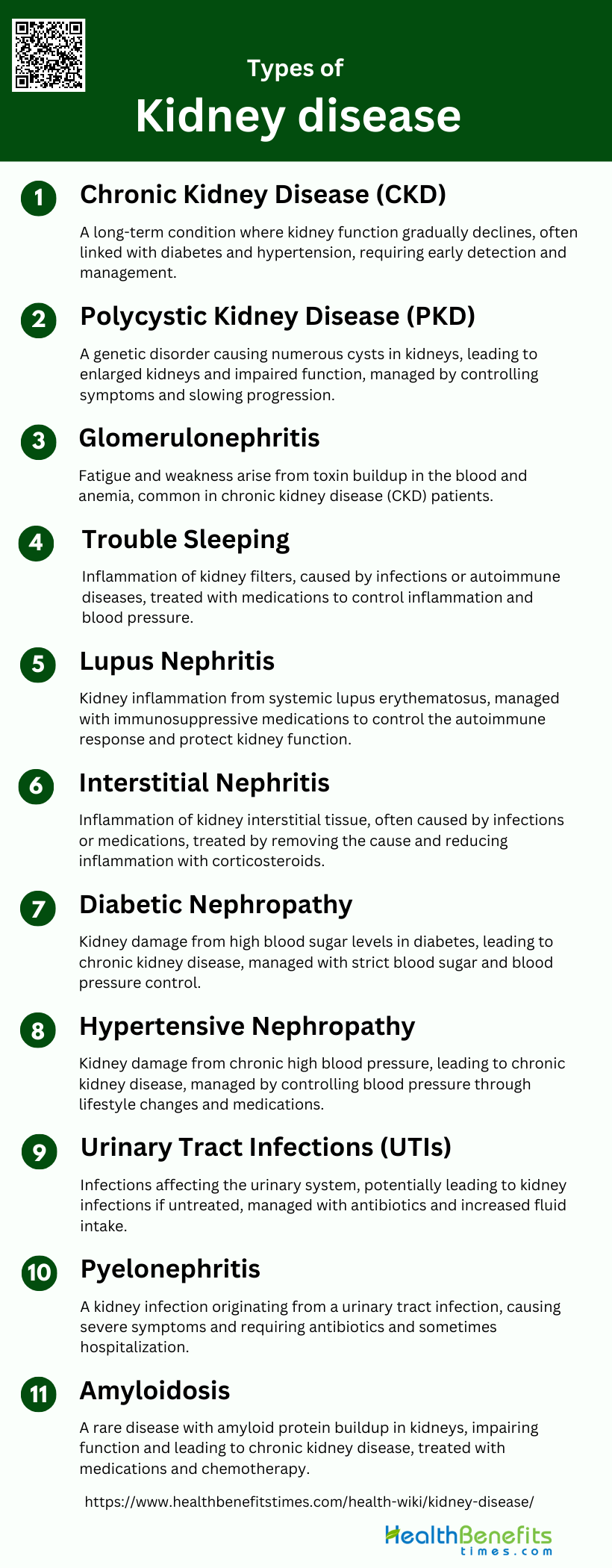
Types of kidney disease
Understanding the different types of kidney diseases is crucial for early diagnosis and effective management. Below are some of the most common types of kidney diseases:
1. Chronic Kidney Disease (CKD)
Chronic Kidney Disease (CKD) is a long-term condition characterized by a gradual loss of kidney function over time. It is often associated with other chronic conditions such as diabetes and hypertension. CKD can progress to end-stage renal disease (ESRD), requiring dialysis or kidney transplantation. The disease is typically asymptomatic in its early stages, making early detection through regular screening crucial. Management includes controlling underlying conditions, dietary modifications, and medications to slow progression and manage symptoms.
2. Acute Kidney Injury (AKI)
Acute Kidney Injury (AKI) is a sudden decline in kidney function, often occurring in hospitalized patients due to factors like sepsis, drugs, or. It is characterized by a rapid increase in serum creatinine and/or a decrease in urine output. AKI can lead to chronic kidney disease (CKD) if not properly managed. Early detection and management are crucial to prevent long-term damage.
3. Polycystic Kidney Disease (PKD)
Polycystic Kidney Disease (PKD) is a genetic disorder characterized by the growth of numerous cysts in the kidneys. These cysts can lead to enlarged kidneys and impaired kidney function. PKD can cause high blood pressure, kidney infections, and kidney stones. There are two main types: autosomal dominant PKD (ADPKD) and autosomal recessive PKD (ARPKD). Management focuses on controlling symptoms and slowing disease progression through medications, lifestyle changes, and sometimes surgical interventions.
4. Glomerulonephritis
Glomerulonephritis is an inflammation of the glomeruli, the tiny filters in the kidneys. It can be acute or chronic and is often caused by infections, autoimmune diseases, or other underlying conditions. Symptoms may include blood in the urine, proteinuria, and high blood pressure. Treatment depends on the underlying cause and may involve medications to control inflammation and blood pressure, as well as lifestyle changes to protect kidney function.
5. Lupus Nephritis
Lupus Nephritis is a type of kidney inflammation caused by systemic lupus erythematosus (SLE), an autoimmune disease. It occurs when the immune system attacks the kidneys, leading to inflammation and damage. Symptoms can include proteinuria, hematuria, and reduced kidney function. Treatment typically involves immunosuppressive medications to control the autoimmune response and protect kidney function.
6. Interstitial Nephritis
Interstitial Nephritis, also known as Tubulointerstitial Nephritis (TIN), is an inflammation of the kidney’s interstitial tissue, often caused by infections, medications, or autoimmune diseases. It can lead to acute kidney injury (AKI) and progress to chronic kidney disease (CKD) if not treated promptly. Symptoms are often nonspecific, making early diagnosis challenging. Treatment usually involves removing the offending agent and using corticosteroids to reduce inflammation.
7. Diabetic Nephropathy
Diabetic Nephropathy is a common complication of diabetes, characterized by damage to the kidney’s filtering units due to high blood sugar levels. It is a leading cause of chronic kidney disease (CKD) and end-stage renal disease (ESRD). Early stages may be asymptomatic, but as the disease progresses, symptoms like proteinuria, high blood pressure, and swelling may occur. Management includes strict blood sugar control, blood pressure management, and medications to protect kidney function.
8. Hypertensive Nephropathy
Hypertensive Nephropathy is kidney damage caused by chronic high blood pressure. It can lead to chronic kidney disease (CKD) and eventually end-stage renal disease (ESRD). High blood pressure damages the blood vessels in the kidneys, reducing their ability to filter waste and excess fluids. Management focuses on controlling blood pressure through lifestyle changes and medications to prevent further kidney damage.
9. Urinary Tract Infections (UTIs)
Urinary Tract Infections (UTIs) are infections that affect any part of the urinary system, including the kidneys, bladder, and urethra. They are more common in women and can cause symptoms like frequent urination, pain during urination, and cloudy or bloody urine. If left untreated, UTIs can lead to more serious kidney infections (pyelonephritis). Treatment typically involves antibiotics and increased fluid intake to flush out the bacteria.
10. Pyelonephritis
Pyelonephritis is a type of kidney infection that usually starts as a urinary tract infection (UTI) and spreads to the kidneys. It can cause symptoms like fever, chills, back pain, and nausea. If not treated promptly, pyelonephritis can lead to serious complications, including kidney damage and sepsis. Treatment involves antibiotics and sometimes hospitalization for severe cases.
11. Amyloidosis
Amyloidosis is a rare disease characterized by the buildup of amyloid proteins in organs, including the kidneys. This buildup can impair kidney function and lead to chronic kidney disease (CKD). Symptoms may include proteinuria, swelling, and fatigue. Treatment focuses on managing symptoms and slowing the production of amyloid proteins through medications and, in some cases, chemotherapy.
Early Symptoms of Kidney Disease
Recognizing the early symptoms of kidney disease is essential for timely intervention and treatment. These symptoms can often be subtle and easily overlooked, but early detection can significantly improve outcomes. Below are some of the common early symptoms of kidney disease:
1. Changes in Urination
Changes in urination are often one of the earliest signs of kidney disease. Patients may notice an increase or decrease in the frequency of urination, changes in the color of urine, or the presence of blood. These symptoms are indicative of the kidneys’ declining ability to filter waste and fluids effectively. In advanced stages, patients may experience nocturia, which is frequent urination at night, significantly disrupting sleep patterns.
2. Swelling (Edema)
Swelling, or edema, is a common symptom of kidney disease, particularly in the legs, ankles, feet, and sometimes the face and hands. This occurs because the kidneys are unable to remove excess fluid and salt from the body, leading to fluid retention. Edema can be particularly distressing and is often one of the symptoms that prompt patients to seek medical attention.
3. Fatigue and Weakness
Fatigue and weakness are prevalent symptoms in chronic kidney disease (CKD) patients. These symptoms are often due to the buildup of toxins and waste products in the blood, which the kidneys can no longer filter effectively. Additionally, anemia, a common complication of CKD, can contribute to feelings of tiredness and weakness, significantly impacting the patient’s quality of life.
4. Trouble Sleeping
Patients with kidney disease frequently report trouble sleeping. This can be due to several factors, including nocturia, restless legs syndrome, and general discomfort. The accumulation of toxins in the blood can also lead to sleep disturbances. Addressing sleep issues is crucial as they can exacerbate other symptoms and negatively affect overall health.
5. Dry and Itchy Skin
Dry and itchy skin is a common symptom in patients with kidney disease, often resulting from the buildup of waste products in the blood that the kidneys can no longer filter out. This condition, known as pruritus, can be particularly bothersome and is often resistant to conventional treatments. It significantly impacts the patient’s quality of life and requires targeted management strategies.
6. Poor Appetite
A poor appetite is frequently observed in patients with kidney disease. This symptom can be attributed to the accumulation of waste products in the blood, which can cause nausea and a general feeling of malaise. Additionally, dietary restrictions often imposed on CKD patients can make eating less enjoyable, further contributing to a reduced appetite.
7. Muscle Cramps
Muscle cramps are a common complaint among CKD patients. These cramps can be caused by electrolyte imbalances, particularly low levels of calcium and magnesium, which are often seen in kidney disease. The discomfort from muscle cramps can significantly affect a patient’s ability to perform daily activities and overall quality of life.
8. Nausea and Vomiting
Nausea and vomiting are significant symptoms in kidney disease, often resulting from the buildup of uremic toxins in the blood. These symptoms can lead to poor nutritional intake and weight loss, further complicating the patient’s health status. Effective management of these symptoms is crucial to maintaining the patient’s nutritional status and overall well-being.
9. Difficulty Concentrating
Difficulty concentrating, or cognitive impairment, is a less commonly recognized symptom of kidney disease but can be quite debilitating. This symptom is often due to the buildup of toxins in the blood, which can affect brain function. Patients may experience memory problems, confusion, and difficulty focusing on tasks, impacting their daily lives and work performance.
10. Shortness of Breath
Shortness of breath can occur in kidney disease due to fluid buildup in the lungs (pulmonary edema) or anemia, which reduces the oxygen-carrying capacity of the blood. This symptom can be particularly distressing and may worsen with physical activity. It is essential to address the underlying causes to improve the patient’s respiratory function and overall quality of life.
Advanced symptoms of Kidney disease
As kidney disease progresses, the symptoms become more pronounced and can significantly impact daily life. Recognizing these advanced symptoms is crucial for seeking timely medical intervention. Below are some of the advanced symptoms of kidney disease:
1. Fluid Retention and Swelling (Edema)
Fluid retention and swelling, known as edema, are common symptoms in advanced kidney disease. Edema occurs due to the kidneys’ reduced ability to remove excess fluid from the body, leading to fluid accumulation in tissues. This symptom was reported by 58% of patients with stage 5 chronic kidney disease (CKD) managed conservatively. Edema can manifest in various parts of the body, including the legs, ankles, and around the eyes. It is often associated with other symptoms such as dyspnea (shortness of breath) and can significantly impact the quality of life. Effective management of fluid retention is crucial to alleviate discomfort and prevent further complications.
2. Urinary Changes
Patients with advanced kidney disease often experience significant changes in urinary patterns. These changes can include a decrease in urine output, dark or foamy urine, and the presence of blood in the urine. The reduction in urine output is a direct consequence of the kidneys’ declining ability to filter and excrete waste products and excess fluids. Additionally, urinary changes can be indicative of worsening kidney function and may be accompanied by other symptoms such as edema and hypertension. Monitoring and managing these changes are essential for preventing further kidney damage and maintaining overall health.
3. Gastrointestinal Symptoms
Gastrointestinal (GI) symptoms are prevalent in patients with advanced kidney disease, with gastroparesis being a notable condition. Gastroparesis involves delayed gastric emptying, leading to symptoms such as early satiety, nausea, vomiting, and epigastric pain. These symptoms can result in significant weight loss and malnutrition, further complicating the management of CKD. The pathogenesis of GI symptoms in CKD is multifactorial, involving electrolyte imbalances, gastric mucosal edema, and the direct toxicity of uremic retention molecules. Addressing these symptoms is crucial for improving patients’ nutritional status and overall quality of life.
4. Fatigue and Weakness
Fatigue and weakness are among the most common and debilitating symptoms experienced by patients with advanced kidney disease. The prevalence of fatigue ranges from 42% to 89%, depending on the treatment modality and measurement instruments used. Fatigue in CKD is a multifactorial issue, influenced by sociodemographic, biological, and psychological factors, including depression, anxiety, sleep disturbances, and inflammation. Effective management of fatigue requires a comprehensive approach, incorporating both pharmacological and nonpharmacological interventions such as physical exercise and cognitive-behavioral therapy.
5. Cognitive and Neurological Symptoms
Cognitive and neurological symptoms are significant concerns in advanced kidney disease. Patients often report poor concentration, drowsiness, and cognitive impairment, which can severely impact daily functioning and quality of life. These symptoms are likely related to the accumulation of uremic toxins and electrolyte imbalances affecting brain function. Additionally, the psychological burden of living with a chronic illness can exacerbate cognitive issues. Addressing these symptoms through routine assessment and appropriate interventions is essential for improving patients’ mental health and overall well-being.
6. Skin and Sensory Symptoms
Skin and sensory symptoms, such as pruritus (itching) and dry skin, are common in advanced kidney disease. Pruritus affects up to 74% of patients with stage 5 CKD managed conservatively, making it one of the most prevalent symptoms. These symptoms are often caused by the accumulation of uremic toxins and can lead to significant discomfort and sleep disturbances. Effective management strategies, including topical treatments and systemic medications, are necessary to alleviate these symptoms and improve patients’ quality of life.
7. Respiratory Symptoms
Respiratory symptoms, including dyspnea (shortness of breath), are frequently reported by patients with advanced kidney disease. Dyspnea affects approximately 61% of patients with stage 5 CKD managed conservatively. This symptom can result from fluid overload, anemia, and the presence of uremic toxins affecting respiratory function. Dyspnea is often distressing and can significantly impact physical activity and overall quality of life. Addressing the underlying causes, such as managing fluid balance and treating anemia, is crucial for alleviating respiratory symptoms in CKD patients.
8. Musculoskeletal Symptoms
Musculoskeletal symptoms, such as bone and joint pain, muscle cramps, and restless legs, are common in advanced kidney disease. These symptoms can result from mineral and bone disorders associated with CKD, including abnormalities in calcium, phosphate, and parathyroid hormone levels. Bone and joint pain were reported as severe symptoms by 37% of women and 32% of men with advanced CKD. Effective management of musculoskeletal symptoms involves addressing the underlying mineral imbalances and providing appropriate pain relief to improve patients’ mobility and quality of life.
9. Cardiovascular Symptoms
Cardiovascular symptoms are prevalent in patients with advanced kidney disease due to the high burden of cardiovascular comorbidities in this population. Symptoms such as chest pain, palpitations, and shortness of breath are common and can indicate underlying cardiovascular disease. The presence of cardiovascular symptoms is associated with a higher risk of adverse outcomes, including heart failure and sudden cardiac death. Managing cardiovascular risk factors, such as hypertension, diabetes, and dyslipidemia, is essential for reducing the burden of cardiovascular symptoms and improving overall prognosis in CKD patients.
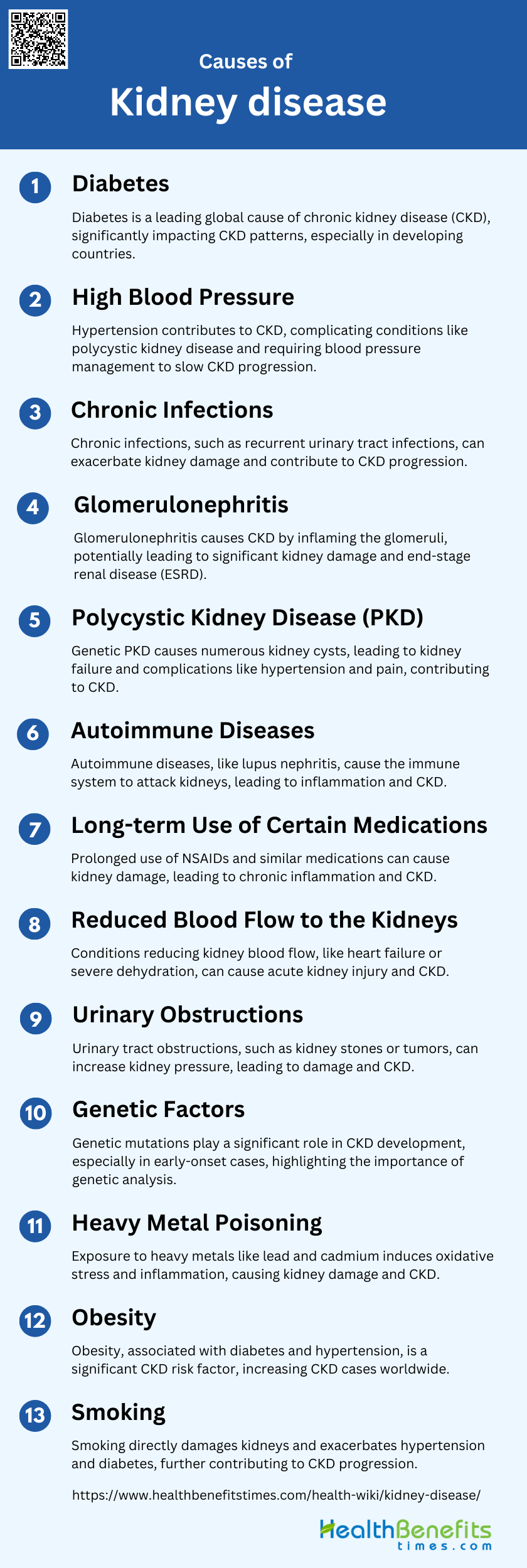
Causes of Kidney Disease
Understanding these causes is essential for prevention and early intervention. Below are some of the primary causes of kidney disease:
1. Diabetes
Diabetes is a leading cause of chronic kidney disease (CKD) globally. The prevalence of diabetes has increased dramatically, especially in developing countries, significantly affecting the patterns of CKD observed in these regions. Diabetes mellitus is commonly associated with CKD, contributing to the disease’s progression and severity.
2. High Blood Pressure
Hypertension is a significant contributor to CKD. It is often observed in patients with polycystic kidney disease (PKD) and other forms of CKD, leading to further complications such as cardiovascular issues and kidney failure. The management of blood pressure is crucial in slowing the progression of CKD.
3. Chronic Infections
Chronic infections can lead to kidney damage and contribute to the progression of CKD. Infections such as recurrent urinary tract infections are common in patients with PKD and can exacerbate kidney damage.
4. Glomerulonephritis
Glomerulonephritis is a common cause of CKD, particularly in developing countries. It involves inflammation of the glomeruli, which can lead to significant kidney damage and progression to end-stage renal disease (ESRD).
5. Polycystic Kidney Disease (PKD)
Polycystic Kidney Disease is a genetic disorder characterized by the growth of numerous cysts in the kidneys. It is a common cause of kidney failure and is associated with various complications, including hypertension, pain, and increased risk of aneurysms. Both autosomal dominant and recessive forms of PKD contribute to CKD.
6. Autoimmune Diseases
Autoimmune diseases such as lupus nephritis can lead to CKD. These conditions cause the immune system to attack the kidneys, leading to inflammation and damage.
7. Long-term Use of Certain Medications
Prolonged use of certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can cause kidney damage and contribute to the development of CKD. These medications can lead to chronic inflammation and oxidative stress, further damaging the kidneys.
8. Reduced Blood Flow to the Kidneys
Conditions that reduce blood flow to the kidneys, such as heart failure or severe dehydration, can cause acute kidney injury and contribute to the development of CKD. Chronic reduced blood flow can lead to ischemic damage and progressive kidney failure.
9. Urinary Obstructions
Obstructions in the urinary tract, such as kidney stones or tumors, can lead to kidney damage and CKD. These obstructions can cause increased pressure in the kidneys, leading to damage and reduced kidney function.
10. Genetic Factors
Genetic mutations play a significant role in the development of CKD, particularly in early-onset cases. Over 200 different monogenic genes have been identified as contributing to early-onset CKD, highlighting the importance of genetic analysis in diagnosing and managing the disease.
11. Heavy Metal Poisoning
Exposure to heavy metals such as lead and cadmium can cause kidney damage and contribute to CKD. These metals can induce oxidative stress and inflammation, leading to progressive kidney damage.
12. Obesity
Obesity is a significant risk factor for CKD. It is associated with conditions such as diabetes and hypertension, which are major contributors to kidney disease. The increasing prevalence of obesity has led to a rise in CKD cases worldwide.
13. Smoking
Smoking is a known risk factor for CKD. It can cause direct damage to the kidneys and exacerbate conditions such as hypertension and diabetes, further contributing to kidney disease progression.
Diagnosis of Kidney Disease
Early and accurate diagnosis of kidney disease is crucial for effective treatment and management. Various tests and procedures are used to identify kidney problems and assess their severity. Below are some common methods for diagnosing kidney disease:
1. Initial Assessment
The initial assessment of kidney disease involves a comprehensive evaluation of the patient’s overall health and kidney function. This includes a detailed review of symptoms, risk factors, and any previous medical conditions that may contribute to kidney disease. Laboratory tests, such as measuring serum creatinine and estimating glomerular filtration rate (GFR), are essential for detecting early-stage kidney disease, which is often asymptomatic. Additionally, urine tests for albumin and protein levels can provide critical information about kidney function and damage. Early detection through these assessments is crucial for timely intervention and management of kidney disease.
2. Medical History
A thorough medical history is vital for diagnosing kidney disease, as it can reveal underlying conditions and risk factors that contribute to renal dysfunction. This includes a history of hypertension, diabetes, cardiovascular disease, and any family history of kidney disease. Additionally, a detailed account of the patient’s medication use, lifestyle factors, and previous episodes of kidney-related symptoms can provide valuable insights. Understanding the patient’s medical history helps clinicians identify potential causes of kidney disease and tailor diagnostic and therapeutic approaches accordingly.
3. Physical Examination
The physical examination for kidney disease involves a systematic evaluation of the patient to identify signs that may indicate renal dysfunction. This includes checking for edema, hypertension, and abnormalities in the abdomen, such as palpable kidneys or bladder distension. A urine dipstick test is a crucial part of the physical examination, as it can detect proteinuria, hematuria, and other abnormalities that suggest kidney disease. The physical examination, combined with the patient’s medical history and laboratory tests, provides a comprehensive assessment of kidney health.
4. Blood Tests
Blood tests are essential for diagnosing and monitoring kidney disease. Key tests include measuring serum creatinine, blood urea nitrogen (BUN), and estimating the glomerular filtration rate (GFR). These tests help assess the kidneys’ ability to filter waste products from the blood. Additionally, blood tests for electrolytes, such as potassium and sodium, and markers of inflammation, such as C-reactive protein, can provide further information about kidney function and potential complications. Advanced biomarkers, like cystatin C and kidney injury molecule-1, are also being explored for their potential to improve early diagnosis and monitoring of kidney disease.
5. Urine Tests
Urine tests are a fundamental component of kidney disease diagnosis. They include measuring urine albumin, protein, and creatinine levels to assess kidney function and detect abnormalities. The albumin-to-creatinine ratio (ACR) from a spot urine sample is particularly useful for detecting and staging chronic kidney disease (CKD). Additionally, urine tests can identify the presence of blood, glucose, and other substances that may indicate kidney damage or underlying conditions. Urinary proteome analysis is an emerging technique that can discriminate different types of CKD by identifying specific peptide biomarkers.
6. Ultrasound
Ultrasound imaging is a non-invasive and widely used technique for evaluating kidney structure and function. It can detect abnormalities such as kidney stones, cysts, tumors, and changes in kidney size or shape. Doppler ultrasound, which assesses blood flow in the renal arteries and veins, can provide additional information about renal perfusion and vascular conditions. Ultrasound elastography, a newer technique, can measure tissue stiffness and help assess the degree of kidney fibrosis, which is a marker of chronic kidney disease progression.
7. CT Scan and MRI
Computed tomography (CT) scans and magnetic resonance imaging (MRI) are advanced imaging techniques used to obtain detailed images of the kidneys and surrounding structures. CT scans are particularly useful for detecting kidney stones, tumors, and vascular abnormalities. MRI, including multiparametric MRI, can provide detailed information about kidney tissue composition, perfusion, and fibrosis. These imaging modalities are valuable for diagnosing complex kidney conditions and guiding treatment decisions. However, their use may be limited by factors such as cost, availability, and patient contraindications.
8. Kidney Biopsy
A kidney biopsy is the gold standard for diagnosing many kidney diseases, providing critical information about the underlying pathology. The procedure involves obtaining a small sample of kidney tissue, typically using a needle guided by ultrasound or CT imaging. The tissue is then examined under a microscope to identify specific disease processes, such as glomerulonephritis, interstitial nephritis, or fibrosis. While kidney biopsy is highly informative, it carries risks such as bleeding and infection. Therefore, it is usually reserved for cases where non-invasive tests are inconclusive or when a precise diagnosis is essential for guiding treatment.
Prevention of Kidney Disease
Preventing kidney disease involves adopting a healthy lifestyle and managing underlying health conditions that can harm the kidneys. By taking proactive steps, individuals can significantly reduce their risk of developing kidney problems. Below are some key strategies for preventing kidney disease:
1. Regular Check-ups
Regular check-ups are crucial for the early detection and management of chronic kidney disease (CKD). Routine monitoring of kidney function through blood tests, urine tests, and blood pressure measurements can help identify CKD in its early stages when interventions are most effective. Early detection allows for timely lifestyle modifications and medical treatments that can slow the progression of the disease. Regular check-ups also provide an opportunity for healthcare providers to educate patients on risk factors and preventive measures, thereby reducing the incidence of CKD.
2. Control Blood Pressure
Controlling blood pressure is essential in preventing CKD. Hypertension is a significant risk factor for the development and progression of CKD. Effective blood pressure management can be achieved through lifestyle changes such as reducing sodium intake, maintaining a healthy weight, and regular physical activity. Medications may also be necessary to achieve target blood pressure levels. The Kidney Disease: Improving Global Outcomes (KDIGO) guidelines recommend blood pressure control of <140/90 mmHg in patients without albuminuria and <130/80 mmHg in patients with albuminuria to prevent CKD progression.
3. Manage Blood Sugar
Managing blood sugar levels is vital for preventing CKD, especially in individuals with diabetes. Hyperglycemia can damage the blood vessels in the kidneys, leading to CKD. Maintaining optimal blood sugar levels through diet, exercise, and medication can significantly reduce the risk of kidney damage. Regular monitoring of blood glucose levels and HbA1c can help in the early detection of diabetes-related kidney issues, allowing for timely interventions to prevent further damage.
4. Healthy Diet
A healthy diet plays a crucial role in preventing CKD. Diets rich in fruits, vegetables, whole grains, and low in processed meats and sugar-sweetened beverages are associated with a lower risk of CKD. The DASH (Dietary Approaches to Stop Hypertension) diet, which emphasizes the consumption of fruits, vegetables, low-fat dairy products, and whole grains, has been shown to lower the incidence of CKD. Reducing sodium intake and avoiding excessive protein consumption can also help maintain kidney health.
5. Exercise Regularly
Regular exercise is beneficial for kidney health and can help prevent CKD. Physical activity improves cardiovascular health, helps control blood pressure, and aids in maintaining a healthy weight, all of which are important factors in preventing CKD. Exercise also improves heart rate variability and baroreflex sensitivity, which are crucial for cardiovascular health. Engaging in regular physical activity can reduce the risk of CKD and improve overall health outcomes.
6. Avoid Smoking
Avoiding smoking is critical in preventing CKD. Smoking has been shown to accelerate the progression of CKD and is associated with an increased risk of developing the disease. Smoking can damage blood vessels, reduce blood flow to the kidneys, and exacerbate hypertension, all of which contribute to kidney damage. Quitting smoking can significantly reduce the risk of CKD and improve overall kidney function.
7. Limit Alcohol Intake
Limiting alcohol intake is important for kidney health. While moderate alcohol consumption may have some protective effects against CKD, excessive drinking can lead to kidney damage and other health issues. Studies have shown that mild-to-moderate alcohol consumption is associated with a lower risk of CKD, particularly in non-smokers. However, heavy drinking can exacerbate hypertension and liver disease, both of which are risk factors for CKD. It is important to consume alcohol in moderation to maintain kidney health.
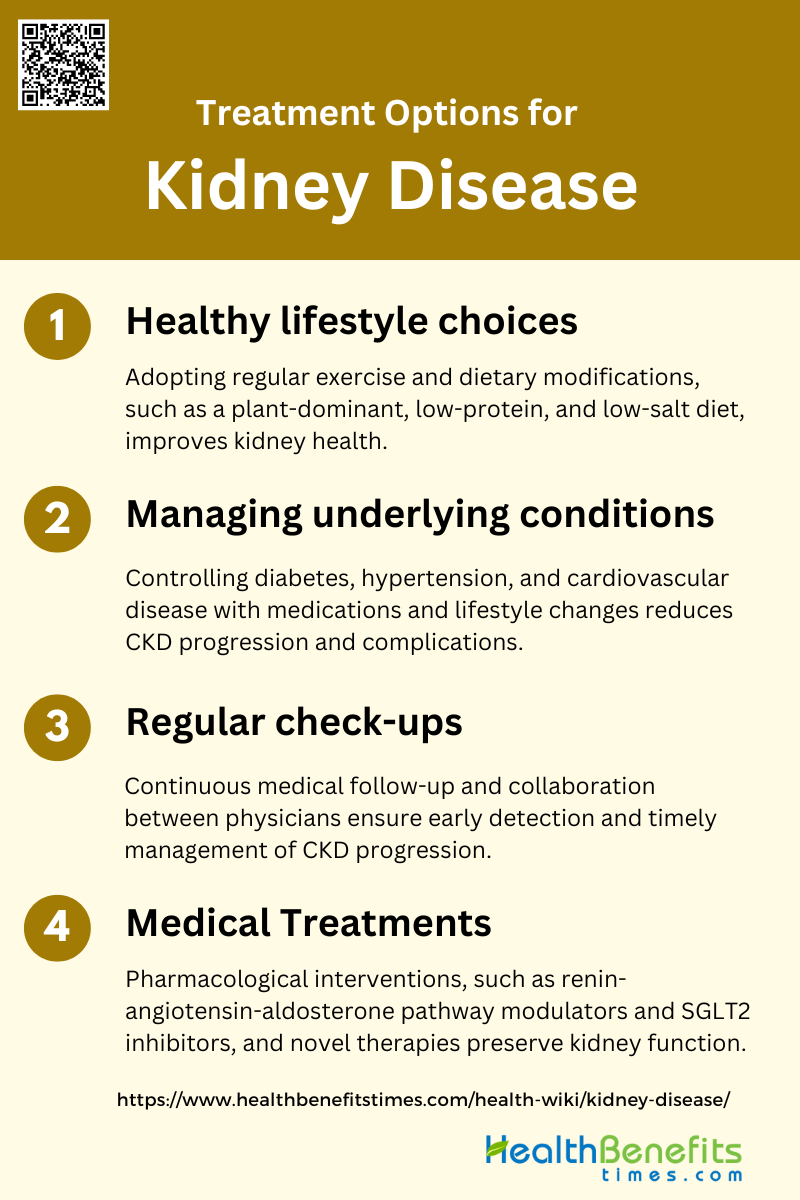
Treatment Options for Kidney disease
Effective management of kidney disease often requires a combination of treatments tailored to the individual’s specific condition. These treatments aim to slow the progression of the disease, manage symptoms, and improve quality of life. Below are some common treatment options for kidney disease:
1. Healthy lifestyle choices
Adopting healthy lifestyle choices is crucial for managing chronic kidney disease (CKD). Regular physical exercise, such as walking, has been shown to improve cardiovascular health, reduce exertion, and enhance overall quality of life in CKD patients. Dietary modifications, including a plant-dominant, low-protein, and low-salt diet, can help mitigate glomerular hyperfiltration and preserve renal function. Additionally, weight loss through lifestyle changes can improve metabolic parameters and reduce proteinuria, which is beneficial for kidney health. These lifestyle interventions not only slow the progression of CKD but also improve patients’ overall well-being and quality of life.
2. Managing underlying conditions
Managing underlying conditions such as diabetes, hypertension, and cardiovascular disease is essential for CKD patients. Effective control of these conditions can significantly reduce the risk of CKD progression and associated complications. Pharmacotherapies that alter intrarenal hemodynamics, such as renin-angiotensin-aldosterone pathway modulators and SGLT2 inhibitors, can preserve kidney function by reducing intraglomerular pressure. Additionally, lifestyle changes, including smoking cessation, weight reduction, and regular physical exercise, are recommended to manage these underlying conditions and improve both cardiovascular and kidney health. Collaborative care involving general physicians and nephrologists is also crucial for optimal management.
3. Regular check-ups
Regular check-ups are vital for early detection and management of CKD progression. Continuous medical follow-up and collaboration between general physicians and nephrologists can help in timely interventions and better management of the disease. Regular monitoring of kidney function, blood pressure, and other relevant parameters allows for the adjustment of treatment plans and lifestyle modifications as needed. Patient education and empowerment are also important, as they encourage adherence to treatment plans and lifestyle changes, ultimately leading to better health outcomes. Regular check-ups ensure that any complications or changes in the disease status are promptly addressed.
4. Medical Treatments
Medical treatments for CKD include a range of pharmacological and non-pharmacological interventions. Pharmacotherapies such as renin-angiotensin-aldosterone pathway modulators, SGLT2 inhibitors, and non-steroidal mineralocorticoid receptor antagonists can help preserve kidney function and reduce inflammation and fibrosis. Novel therapeutic approaches targeting cytokines, transcription factors, and epigenetic modulators are also being explored to reduce kidney fibrosis and improve outcomes. Additionally, conservative management strategies, including dietary-nutritional therapy and symptom management, can optimize quality of life and delay the need for dialysis. These medical treatments, combined with lifestyle modifications, offer a comprehensive approach to managing CKD.