Ablation is a minimally invasive treatment option for small renal cell carcinomas (RCC), particularly those classified as stage T1a (less than 4 cm in diameter). This nephron-sparing technique involves destroying cancer cells using either heat or cold, delivered through needles placed directly into the tumor under image guidance. Typically performed percutaneously in an interventional radiology suite, ablation has become an increasingly popular alternative to partial nephrectomy, especially for older or chronically ill patients who may not be suitable candidates for surgery. The procedure offers the advantage of preserving kidney function while effectively treating the cancer. However, it’s important to note that the success of ablation can be influenced by factors such as tumor size, with larger tumors presenting a higher risk of complications and treatment failure.
Types of Ablation Procedures
Ablation procedures are minimally invasive techniques used to treat various medical conditions, particularly cancers. Here are three common types of ablation procedures:
1. Radiofrequency Ablation (RFA)
Radiofrequency ablation works by delivering high-frequency electrical currents to the target tissue, causing localized heating and consequent necrosis. This technique is widely used for treating atrial fibrillation and various solid tumors. The benefits of RFA include its effectiveness in maintaining sinus rhythm, improved quality of life for patients, and relatively low complication rates. However, risks associated with RFA include pulmonary-vein stenosis and cardiac tamponade, which occur in less than 5% of patients. It’s important to note that most evidence for RFA comes from studies involving middle-aged adults with preserved left ventricular function and short follow-up periods.
2. Cryoablation
Cryoablation is a technique that uses extreme cold to destroy abnormal tissue. While not explicitly mentioned in the search results, cryoablation typically involves inserting a probe into or near the target tissue and circulating extremely cold gas or liquid to freeze and destroy the cells. The benefits of cryoablation include its precision in targeting specific areas and potentially less pain compared to heat-based ablation methods. Risks may include damage to nearby healthy tissue and temporary numbness or tingling in the treated area. However, as with any medical procedure, the specific benefits and risks can vary depending on the treated condition and individual patient factors.
3. Microwave Ablation
Microwave ablation (MWA) uses electromagnetic waves to generate heat and destroy target tissues. This technique is gaining popularity, particularly in the treatment of lung cancer and hepatocellular carcinoma (HCC). MWA offers benefits such as effective tumor control and a minimally invasive approach. For HCC, MWA has shown promising results, with some studies suggesting it may be non-inferior to laparoscopic liver resection for single tumors 3-5 cm in size. However, there are risks associated with MWA, including pneumothorax, which can be particularly serious in patients with compromised lung function. The National Institute for Health and Care Excellence (NICE) recommends that MWA should only be used with careful explanation of risks to patients and proper monitoring of outcomes.
Eligibility for Ablation
Criteria for Choosing Patients
When selecting patients for ablation, several criteria must be considered to ensure optimal outcomes. For renal tumors, candidates typically have tumors smaller than 3 cm, posterior, and completely exophytic, although guidelines suggest that tumors up to 4 cm (cT1a) can be considered for ablation. For colorectal liver metastases (CRLM), patients with an Eastern Cooperative Oncology Group (ECOG) performance status of ≤2, an American Society of Anesthesiologists (ASA) score of ≤3, and a Charlson comorbidity index of ≤8 are deemed fit for curative-intent local therapy. Additionally, the patient’s overall health, including factors like age, liver function, and comorbidities, plays a crucial role in determining eligibility for ablation.
Factors Affecting Suitability
1. Tumor Size
Tumor size is a critical factor affecting the suitability of ablation. For renal tumors, radiofrequency ablation (RFA) is most effective for tumors up to 3 cm, while cryoablation can be used for tumors up to 4 cm. In the case of CRLM, smaller tumors (typically less than 3 cm) are more amenable to ablation, with larger tumors often requiring more complex interventions. Studies have shown that larger tumors are associated with higher rates of local tumor progression and recurrence, making size a significant determinant in the decision-making process.
2. Patient Health Status
The general health status of the patient is another crucial factor in determining suitability for ablation. Patients with better overall health and fewer comorbidities are more likely to benefit from ablation. For instance, patients with a good performance status (ECOG ≤2) and lower ASA scores are considered better candidates for ablation. Additionally, factors such as liver function, age, and the presence of other health conditions significantly impact the decision. For example, patients with cirrhosis or poor liver function may face higher risks during ablation procedures. Therefore, a comprehensive assessment of the patient’s health status is essential to ensure the best possible outcomes.
3. Location of the Tumor
The location of the tumor significantly influences the feasibility and success of ablation. Tumors located in easily accessible areas, such as exophytic renal tumors or peripheral liver metastases, are more suitable for ablation. Conversely, tumors near critical structures like large blood vessels, bile ducts, or the hilum pose higher risks and may require alternative treatments. For instance, subcapsular tumors or those adjacent to large vessels often necessitate more precise and cautious approaches to avoid complications. Thus, the anatomical location of the tumor is a key consideration in the selection process for ablation therapy.
Why Choose Ablation for Kidney Cancer?
Ablation is increasingly chosen for kidney cancer due to its numerous benefits over traditional surgery, particularly for small tumors and early-stage cancer. Ablative therapies, such as radiofrequency ablation (RFA) and cryoablation, offer oncological effectiveness comparable to partial nephrectomy for tumors smaller than 3 cm, with fewer complications and a better postoperative profile. These minimally invasive procedures are ideal for patients who are unfit for surgery due to comorbidities or poor renal function, as they preserve kidney function and have lower morbidity rates. Additionally, ablation techniques result in shorter hospital stays, quicker recovery times, and less intraoperative blood loss compared to partial nephrectomy, making them a favorable option for patients with solitary small renal tumors. Overall, ablation provides a safe, effective, and less invasive alternative to traditional surgical methods for managing small renal masses.
Ablation Procedure for Kidney Cancer
Preparation for the Procedure
Before undergoing an ablation procedure for kidney cancer, patients typically undergo a series of imaging tests, such as CT scans or MRIs, to precisely locate and assess the tumor. These tests help the medical team determine the most suitable approach for the ablation. A consultation with a specialist, usually a urologist or interventional radiologist, is essential to discuss the procedure, its risks, and potential outcomes. During this consultation, the doctor will review the patient’s medical history, current medications, and overall health status to ensure they are suitable candidates for the ablation. Patients may be advised to stop certain medications or fast for a specific period before the procedure.
What Happens During the Ablation Procedure
The ablation procedure for kidney cancer is typically performed under general anesthesia or conscious sedation to ensure patient comfort. Once the patient is properly sedated, the medical team uses imaging guidance, such as ultrasound or CT, to precisely insert the ablation probe through a small incision in the skin. The probe is carefully guided to the tumor site within the kidney. Depending on the type of ablation technique used (e.g., radiofrequency, cryoablation, or microwave), the probe delivers either extreme heat or cold to destroy the cancerous cells. The procedure usually takes about 1-3 hours, during which the medical team closely monitors the patient’s vital signs and the progress of the ablation.
Post-Procedure Care and Monitoring
After the ablation procedure, patients are typically monitored in a recovery area for several hours to ensure there are no immediate complications. Pain medication may be administered to manage any discomfort. Patients are usually advised to rest and limit physical activities for a few days following the procedure. Follow-up imaging tests are scheduled to assess the effectiveness of the ablation and monitor for any signs of tumor recurrence. Patients will have regular check-ups with their healthcare provider to evaluate their recovery and overall health status. It’s important for patients to report any unusual symptoms, such as fever, increased pain, or changes in urination, to their doctor promptly.
Benefits of Ablation for Kidney Cancer
Ablation therapy has emerged as a promising treatment for kidney cancer, providing several advantages over conventional surgical methods. This technique is especially suitable for patients with small tumors or those who are considered high-risk for surgery. Here are some of the key benefits of ablation therapy for kidney cancer:
1. Minimally Invasive
Ablation techniques for kidney cancer, such as radiofrequency ablation (RFA) and cryoablation, are minimally invasive procedures that offer significant advantages over traditional surgical methods. These techniques involve the use of probes to deliver heat or cold to the tumor, causing cancer cell death without the need for large incisions. This minimally invasive nature results in fewer complications and a better postoperative profile compared to more invasive surgeries like partial nephrectomy. Additionally, these procedures can be performed percutaneously, further reducing the need for extensive surgical intervention and promoting quicker recovery.
2. Shorter Recovery Time
Patients undergoing ablation for kidney cancer typically experience shorter recovery times compared to those who undergo partial nephrectomy. Studies have shown that ablation procedures result in significantly shorter hospital stays and quicker return to normal activities. For instance, one meta-analysis found that patients treated with ablation had hospital stays that were, on average, 2.37 days shorter than those who underwent partial nephrectomy. This reduced recovery time is attributed to the less invasive nature of ablation techniques, which cause less tissue damage and require smaller incisions.
3. Preservation of Kidney Function
Ablation techniques are particularly beneficial for preserving kidney function. These procedures are designed to target and destroy the tumor while sparing the surrounding healthy kidney tissue. Research indicates that ablation results in less postoperative creatinine increase and a smaller decrease in glomerular filtration rate (GFR) compared to partial nephrectomy. This makes ablation an excellent option for patients with preexisting renal insufficiency or those with a solitary kidney, as it minimizes the risk of further renal impairment.
4. Option for High-Risk Patients
Ablation is a viable treatment option for high-risk patients who may not be suitable candidates for traditional surgery due to comorbidities or poor overall health. These minimally invasive procedures are associated with lower perioperative risks and fewer complications, making them safer for patients with significant medical issues. For instance, patients with hereditary precancerous conditions or those who have already undergone multiple surgeries can benefit from the reduced physical stress associated with ablation.
5. Repeatable
One of the significant advantages of ablation is its repeatability. Unlike more invasive surgical options, ablation can be performed multiple times if necessary, allowing for the treatment of recurrent or residual tumors. This flexibility is particularly valuable for managing small renal masses (SRMs) and provides a means to maintain long-term control over the disease without resorting to more aggressive surgical interventions. The ability to repeat the procedure without significant additional risk makes ablation a versatile tool in the management of kidney cancer.
6. Effective for Small Tumors
Ablation is highly effective for treating small renal tumors, particularly those less than 3 cm in diameter. Studies have shown that the oncological outcomes of ablation for small tumors are comparable to those of partial nephrectomy, with high rates of complete tumor ablation and low rates of local recurrence. The primary technical success rate for ablation procedures ranges from 88% to 100%, and more than 95% of tumors under 3 cm can be completely ablated. This makes ablation a reliable and effective treatment option for small renal masses.
7. Less Pain and Complications
Patients undergoing ablation for kidney cancer generally experience less pain and fewer complications compared to those undergoing more invasive surgical procedures. Ablation techniques are associated with lower rates of intraoperative and postoperative complications, including less blood loss, lower transfusion rates, and fewer instances of new-onset chronic kidney disease. The minimally invasive nature of these procedures also results in less postoperative pain, contributing to a more comfortable recovery process for patients.
8. Cost-effective
Ablation is considered a cost-effective treatment option for kidney cancer, particularly for small renal masses. The reduced need for extensive surgical intervention, shorter hospital stays, and quicker recovery times all contribute to lower overall healthcare costs. Additionally, the fewer complications and reduced need for postoperative care further enhance the cost-effectiveness of ablation compared to traditional surgical methods. This makes ablation an attractive option not only from a clinical perspective but also from an economic standpoint, benefiting both patients and healthcare systems.
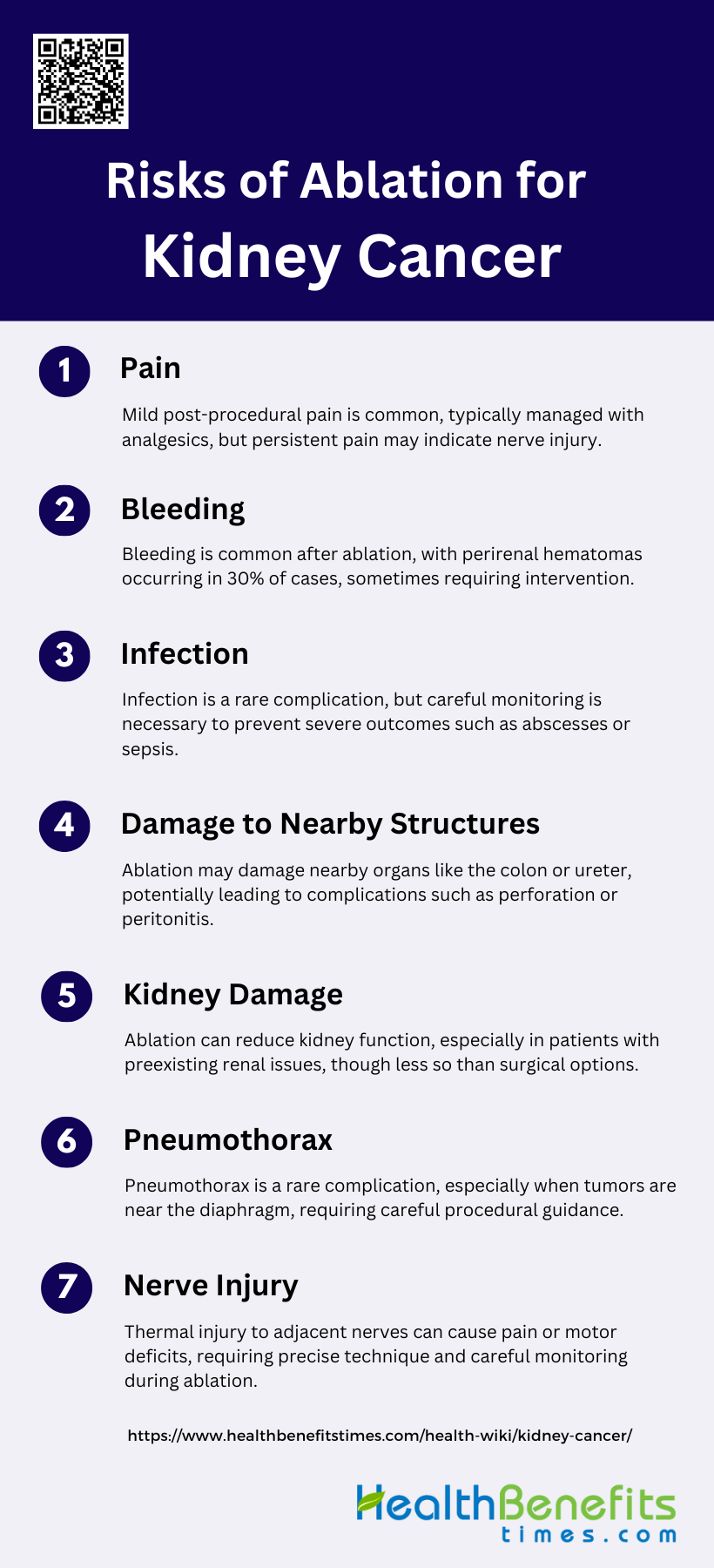
Risks of Ablation for Kidney Cancer
Ablation is a minimally invasive procedure used to treat kidney cancer by destroying cancerous tissue. While it offers benefits such as reduced recovery time and less impact on surrounding healthy tissue, it is not without risks. Patients should be aware of potential complications, including:
1. Pain
Pain is a common complication following ablation for kidney cancer, typically occurring within the first two days post-treatment. This pain is usually mild and manageable with standard analgesics. However, persistent or severe pain may indicate nerve injury, which requires further medical evaluation and intervention. The pain can be attributed to the thermal effects of the ablation process on surrounding tissues and nerves. Effective pain management strategies and careful monitoring are essential to ensure patient comfort and to identify any underlying complications early.
2. Bleeding
Bleeding is the most frequent complication associated with ablation for kidney cancer. Patients undergoing this procedure are often on antiplatelet or anticoagulant therapy, increasing their risk of bleeding. The formation of a perirenal hematoma is reported in up to 30% of cases, with larger-scale bleeding requiring transfusion or embolization occurring in up to 2% of cases. Hematuria, or blood in the urine, is another manifestation of bleeding, particularly when central lesions are treated, although it usually resolves within 24-48 hours. Careful patient selection and pre-procedural planning are crucial to minimize this risk.
3. Infection
Infection is a relatively rare but significant complication of kidney cancer ablation, occurring in up to 2% of cases. The risk of infection can be minimized through sterile techniques and, in some cases, prophylactic antibiotics, although these are not routinely administered. Infections can manifest as localized abscesses or systemic sepsis, requiring prompt medical intervention. Early detection and treatment are essential to prevent severe outcomes. Monitoring for signs of infection, such as fever and localized pain, is critical in the post-procedural period.
4. Damage to Nearby Structures
Damage to nearby structures, such as the colon, ureter, or other adjacent organs, is a potential risk during kidney cancer ablation. Thermal injury to the colon can lead to perforation and peritonitis, occurring in up to 1% of cases. Techniques such as hydrodissection with glucose or CO2 dissection can help prevent this complication. Additionally, thermal injury to the renal tract may result in the formation of a urinoma. Protective measures, such as using cold solutions through an antegrade ureteric stent, are recommended when treating central lesions.
5. Kidney Damage
Kidney damage is a concern during ablation procedures, particularly in patients with pre-existing renal impairment. Ablation can lead to a decrease in renal function, as evidenced by increases in serum creatinine and decreases in glomerular filtration rate. However, studies have shown that ablation generally results in less postoperative renal function decline compared to partial nephrectomy. Careful patient selection and monitoring of renal function before and after the procedure are essential to minimize the risk of significant kidney damage.
6. Pneumothorax
Pneumothorax, or the presence of air in the pleural cavity, is a rare but possible complication of kidney cancer ablation, particularly when the tumor is located near the diaphragm. This condition can occur due to inadvertent puncture of the pleura during the procedure. Symptoms include sudden chest pain and shortness of breath, and it may require intervention such as chest tube placement. Preventive measures include careful imaging guidance and technique during the procedure to avoid pleural injury.
7. Nerve Injury
Nerve injury is a potential complication of kidney cancer ablation, often resulting from thermal damage to nerves adjacent to the treatment site. This can lead to persistent pain, numbness, or motor deficits in the affected area. The risk of nerve injury can be minimized by using precise imaging guidance and techniques to protect critical structures during the procedure. Early recognition and management of nerve injury are crucial to prevent long-term functional impairment.
Effectiveness of Ablation for Kidney Cancer
Success Rates of Ablation for Small Kidney Tumors
Radiofrequency ablation (RFA) has demonstrated high success rates for small renal masses, particularly those less than 3 cm in diameter. Initial technical success rates are reported to be as high as 97%. Long-term studies have shown that the disease-free survival rate for tumors smaller than 3 cm is around 96% at 3 and 5 years. Additionally, a meta-analysis comparing ablation to partial nephrectomy found that ablation had shorter hospital stays, less postoperative creatinine increase, and lower rates of new-onset chronic kidney disease, although it did have a higher risk of local recurrence. Overall, RFA is considered a highly effective treatment for small renal tumors, with excellent initial success and favorable long-term outcomes.
Long-Term Outcomes and Follow-Up Care
Long-term outcomes of RFA for small renal tumors are generally favorable, with high rates of disease-free and cancer-specific survival. Studies have shown that the 10-year disease-free survival rate is around 82%, and cancer-specific survival is approximately 94%. Another study reported a 15-year local-recurrence-free survival rate of 96.5% and a disease-free survival rate of 88.6%. Follow-up care typically involves regular imaging and serum creatinine measurements to monitor for recurrence and renal function. The recurrence rate is low, and most recurrences occur within the first few years post-treatment, emphasizing the importance of meticulous long-term follow-up6. Overall survival rates are also comparable to other treatment modalities, making RFA a viable long-term option for patients with small renal masses9.
How Ablation Fits into Overall Cancer Treatment Plans
Ablation, particularly RFA, is increasingly being integrated into the treatment plans for small renal tumors, especially for patients who are poor surgical candidates due to comorbidities or limited renal function. It offers a minimally invasive alternative with lower complication rates and less impact on renal function compared to surgical options like partial nephrectomy. The American and European urological guidelines now list thermoablation as a treatment option for small renal tumors with curative intent. While ablation has a higher local recurrence rate compared to partial nephrectomy, it provides excellent cancer-specific survival and is particularly beneficial for elderly patients or those with multiple comorbidities. Thus, ablation is a critical component of personalized treatment strategies for kidney cancer, offering a balance between efficacy and quality of life.
When is Ablation Recommended?
Ablation therapy is often considered for kidney cancer patients when traditional surgical options are not suitable or when specific clinical goals need to be met. This approach provides a targeted treatment with minimal invasiveness, making it an attractive option in certain cases. Below, we outline the key situations where ablation is typically recommended.
1. Early-stage or small tumors
Ablation is often recommended for early-stage or small tumors, particularly when the tumors are less than 3 cm in size. This minimally invasive procedure is considered effective for small renal masses (SRMs) and offers a favorable profile in terms of renal function preservation and perioperative outcomes. Studies have shown that ablation techniques, such as radiofrequency ablation (RFA) and cryoablation, provide comparable oncological outcomes to partial nephrectomy (PN) for tumors smaller than 3 cm, with fewer complications and better postoperative profiles. Additionally, image-guided ablation (IGA) is increasingly used for small primary cancers of the kidney, demonstrating robust oncological outcomes and potential as a standard-of-care treatment.
2. Inoperable tumors due to patient’s health or age
Ablation is particularly recommended for patients with inoperable tumors due to health conditions or advanced age. For patients who are poor candidates for surgery, ablative therapies offer a minimally invasive alternative that can effectively manage renal tumors while preserving kidney function. Studies have shown that ablation has shorter hospital stays, less intraoperative blood loss, and fewer complications compared to partial nephrectomy, making it a suitable option for patients with poor preoperative physical conditions or poor renal function. The American Society of Clinical Oncology also recommends percutaneous thermal ablation for patients with significant comorbidities and limited life expectancy, as it can achieve complete ablation reliably.
3. Kidney preservation (avoiding removal of the entire kidney)
Ablation is recommended for kidney preservation, particularly in patients where it is crucial to avoid the removal of the entire kidney. This approach is beneficial for patients with a solitary kidney or those at risk of chronic kidney disease. Studies have demonstrated that ablation techniques, such as RFA and cryoablation, provide excellent renal preservation outcomes while achieving appropriate cancer control. Compared to radical nephrectomy, ablation offers the most favorable perioperative outcomes and the lowest rate of renal impairment, making it an effective nephron-sparing approach. This is particularly important for patients with pre-existing renal impairment or those who require maximal preservation of renal function.
FAQs
1. What types of imaging are used to guide ablation procedures?
Imaging techniques like ultrasound, CT, or MRI are used to precisely target tumors during the ablation procedure, ensuring accuracy.
2. Can ablation be combined with other cancer treatments?
Yes, ablation can be combined with chemotherapy, immunotherapy, or radiation in some treatment plans, depending on the patient’s condition.
3. How long does it take to recover from ablation?
Most patients recover within a few days to a week, though recovery time may vary based on the individual’s health and tumor size.
4. How often should follow-up imaging be performed after ablation?
Follow-up imaging is typically scheduled at regular intervals, often starting at 3 to 6 months post-procedure, to monitor for recurrence.
5. Is ablation an option for recurring kidney cancer?
Yes, ablation is a repeatable procedure and can be used for treating recurrent tumors without significantly increasing risks.
6. What is the likelihood of tumor recurrence after ablation?
The recurrence rate depends on factors like tumor size and location, but ablation is generally effective for small renal tumors with low recurrence.
7. How does ablation compare to other nephron-sparing techniques?
Ablation offers a minimally invasive alternative to partial nephrectomy, with comparable cancer control for small tumors and fewer complications.
8. Are there specific dietary or lifestyle recommendations after ablation?
Patients are generally advised to maintain a healthy lifestyle post-procedure, though specific recommendations should be provided by the healthcare team.
9. Is ablation covered by health insurance?
Most health insurance plans cover ablation for kidney cancer, but coverage may vary depending on the plan and specific case details.
10. Can ablation be used for metastatic kidney cancer?
Ablation is usually reserved for localized tumors, but in some cases, it may be used for treating isolated metastatic lesions.