Intravenous (IV) therapy is a common medical procedure that involves the administration of fluids, medications, or nutrients directly into a patient’s bloodstream through a vein. This method allows for rapid and efficient delivery of substances throughout the body, bypassing the digestive system. IV therapy is widely used in hospitals and healthcare settings for various purposes, including hydration, medication delivery, blood transfusions, and nutritional support. It typically involves inserting a small, flexible tube called a catheter into a vein, usually in the arm or hand, through which the prescribed fluids or medications can be infused. While IV therapy is an essential and often life-saving treatment, it requires careful management and monitoring by healthcare professionals to prevent complications such as infections, infiltration, or phlebitis.
Types of IV therapy
Intravenous (IV) therapy is a medical technique that delivers fluids, medications, and nutrients directly into a patient’s vein. This method ensures rapid absorption and immediate effect, making it crucial for various medical conditions and treatments. Below are some common types of IV therapy:
1. Fluid Replacement Therapy
Fluid replacement therapy is a critical component in both perioperative and critical care settings. It involves the administration of intravenous fluids to maintain adequate organ perfusion and prevent complications such as renal dysfunction and fluid overload. Balanced crystalloids are often preferred as they limit acid-base alterations and chloride load, potentially preventing renal issues. The R.O.S.E. model (Resuscitation, Optimization, Stabilization, and Evacuation) is a dynamic approach that maximizes benefits while minimizing harms. This therapy is particularly important for patients with trauma or burns, where maintaining peripheral oxygen delivery is crucial.
2. Nutritional IV Therapy
Nutritional IV therapy, also known as intravenous nutrition therapy (IVNT), is used to deliver essential nutrients directly into the bloodstream. This therapy can alleviate chronic fatigue, support liver detoxification, and provide anticancer effects in cancer patients. IVNT is distinct from total parenteral nutrition (TPN) and amino acid fluids, as it focuses on specific therapeutic outcomes such as reducing hepatic inflammation and restoring mitochondrial function. Clinicians must conduct appropriate tests and apply accurate differentiation diagnoses to administer IVNT safely and effectively.
3. Antibiotic Therapy
Intravenous antibiotic therapy is essential for treating severe infections, especially in critically ill patients. The administration of antibiotics via IV ensures rapid delivery and higher bioavailability compared to oral routes. This method is particularly useful in cases where oral administration is not feasible, such as in patients with severe mucositis or gastrointestinal issues. The four Ds—drug, dosing, duration, and de-escalation—are critical guidelines to follow for effective antibiotic therapy. Proper fluid management is also crucial to avoid complications like fluid overload and renal dysfunction.
4. Chemotherapy
Intravenous chemotherapy is a cornerstone in the treatment of various cancers. This method allows for the direct delivery of chemotherapeutic agents into the bloodstream, ensuring rapid and effective action against cancer cells. However, it can also lead to side effects such as oral mucositis, which may require supportive treatments like parenteral nutrition or fluid therapy. Studies have shown that while parenteral nutrition can lead to weight gain, it does not necessarily translate into clinical benefits such as faster recovery or reduced hospitalization time.
5. Hydration Therapy
Hydration therapy involves the intravenous administration of fluids to maintain adequate hydration levels, especially in patients who cannot consume fluids orally. This therapy is crucial in preventing dehydration and maintaining electrolyte balance. In surgical settings, an individualized perioperative IV fluid regimen can help reduce postoperative complications and shorten hospital stays. Avoiding unnecessary fasting and transitioning to oral fluids as soon as possible are recommended practices to enhance recovery.
6. Vitamin Therapy
Intravenous vitamin therapy (IVVT) has gained popularity for its purported benefits in enhancing wellness and treating various health conditions. Commonly administered vitamins include C and B12, along with other nutrients like glutathione and electrolytes. Despite its growing use in medical spas and integrative medicine practices, there is insufficient evidence to support the efficacy of IVVT. Moreover, these treatments are often expensive and may pose risks if not administered under proper medical supervision.
How IV Therapy Works
Intravenous (IV) therapy involves the administration of fluids, medications, or nutrients directly into a patient’s vein, typically through a vascular access device (VAD) such as a peripheral or central catheter. The procedure begins with the preparation of the patient, practitioner, environment, and equipment, ensuring aseptic techniques to prevent infections. Essential equipment includes IV catheters, infusion pumps, and monitoring systems, such as smart IV infusion dosing systems that detect and signal fluid levels remotely. Healthcare professionals, particularly nurses, play a crucial role in the prevention of infection, management of VADs, and monitoring for complications, ensuring the safe and effective delivery of IV therapy. Proper training and adherence to guidelines are vital to minimize errors and enhance patient safety.
Uses of IV Therapy
Intravenous (IV) therapy is a versatile medical treatment used to deliver fluids, medications, and nutrients directly into the bloodstream. This method ensures rapid absorption and immediate therapeutic effects, making it essential for various medical conditions. Below are some common uses of IV therapy:
1. Fluid Replacement and Hydration
Intravenous (IV) fluid therapy is a critical intervention for fluid replacement and hydration, especially in perioperative and critical care settings. It is used to resuscitate, replace, and maintain fluid balance in patients. Balanced solutions, such as crystalloids, are preferred to limit acid-base alterations and prevent renal dysfunction. Proper fluid management is essential to maintain adequate organ perfusion while avoiding fluid overload, which can lead to complications. Protocols like the R.O.S.E. model (Resuscitation, Optimization, Stabilization, Evacuation) help maximize the benefits of fluid therapy while minimizing potential harms.
2. Medication Administration
IV therapy is a common route for administering medications, especially in critical care. It allows for precise control over drug dosing and rapid onset of action. For instance, in the treatment of acute migraines, IV fluids are often used in conjunction with medications like metoclopramide to manage symptoms. However, studies have shown that IV fluids alone do not significantly improve pain outcomes in migraine patients, highlighting the importance of combining fluid therapy with appropriate medications for effective treatment.
3. Blood Product Administration
IV therapy is essential for the administration of blood products, which is crucial in managing conditions like severe anemia, trauma, and surgical blood loss. The administration of blood products via IV ensures rapid and controlled delivery, which is vital for stabilizing patients in critical conditions. This method is also used in treating patients with sickle cell disease during vaso-occlusive crises, where extra fluids are administered to alleviate pain and prevent complications, although the optimal route and type of fluid remain under investigation.
4. Nutritional Support
IV therapy plays a significant role in providing nutritional support, especially for patients who cannot consume food orally. Parenteral nutrition, which includes essential nutrients like vitamins, trace elements, and electrolytes, is administered intravenously to meet the nutritional needs of patients. This is particularly important in situations where oral or enteral feeding is not feasible, ensuring that patients receive the necessary nutrients to support recovery and maintain metabolic functions.
5. Electrolyte Imbalance Correction
Correcting electrolyte imbalances is another critical use of IV therapy. In critically ill patients, IV fluids are used to restore electrolyte balance and improve hemodynamics during shock states. Crystalloids, which are sodium salts, are commonly used to address electrolyte imbalances. Understanding the physiology of electrolyte management is essential for the rational use of IV fluids, as improper administration can lead to complications such as fluid overload or renal dysfunction.
6. Pain Management
IV fluid therapy is also employed in pain management, particularly in conditions like sickle cell disease. During acute painful episodes, extra fluids are administered to slow or stop the sickling process, thereby alleviating pain. Although the efficacy of different routes, types, and quantities of fluid administration is still under research, IV fluids remain a routine part of the treatment protocol for managing pain in such conditions.
7. Antibiotic Administration
Administering antibiotics via IV is a common practice in treating severe infections, ensuring rapid and effective delivery of the medication. This method is particularly useful in critical care settings where timely administration of antibiotics is crucial for patient outcomes. IV administration allows for precise control over the dosage and timing, which is essential for managing infections and preventing the development of antibiotic resistance.
8. Hangover Relief and Athletic Performance Recovery
IV therapy has gained popularity for hangover relief and athletic performance recovery. IV hydration therapy, often offered in boutique-style infusion clinics, includes cocktails of vitamins, trace elements, and other medications to alleviate symptoms of hangovers and improve athletic performance. Despite its growing popularity, the scientific merit of such treatments is still debated, and ethical concerns arise due to the ongoing IV drug shortage crisis, which affects the availability of essential nutrients and fluids for medical use.
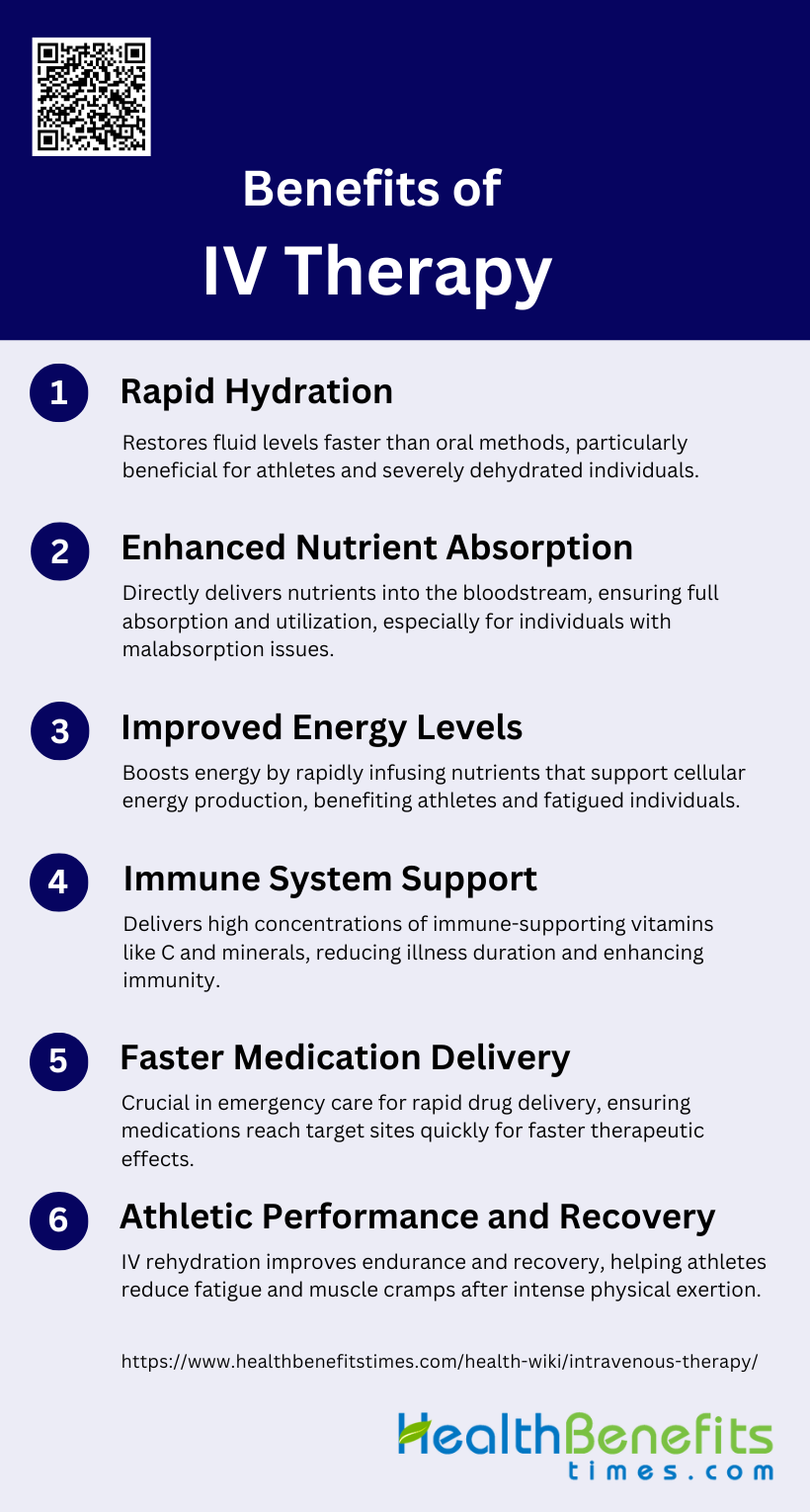
Benefits of IV Therapy
IV therapy offers numerous advantages by delivering fluids, medications, and nutrients directly into the bloodstream. This method ensures rapid absorption and immediate effects, making it a valuable treatment for various health conditions. Below are some key benefits of IV therapy:
1. Rapid Hydration
Intravenous (IV) therapy provides rapid hydration, which is particularly beneficial for athletes and individuals experiencing severe dehydration. Studies have shown that IV rehydration can restore plasma volume more effectively than oral rehydration methods. For instance, athletes who rehydrated with IV fluids demonstrated significant performance improvements in endurance activities compared to those who used oral rehydration methods. The rapid absorption of fluids directly into the bloodstream bypasses the gastrointestinal tract, making it an efficient method for quickly addressing dehydration, especially in cases where oral rehydration is not feasible due to gastrointestinal distress.
2. Enhanced Nutrient Absorption
IV therapy enhances nutrient absorption by delivering essential vitamins and minerals directly into the bloodstream, bypassing the digestive system. This method ensures that nutrients are fully absorbed and utilized by the body, which can be particularly beneficial for individuals with malabsorption issues or chronic illnesses. For example, IV administration of nutrients has been shown to improve nitrogen retention and overall nutritional status in patients recovering from major surgeries. Additionally, IV therapy can provide a more controlled and consistent delivery of nutrients, which is crucial for maintaining optimal health and recovery.
3. Improved Energy Levels
IV therapy can significantly improve energy levels by providing a direct infusion of essential nutrients and electrolytes that support cellular energy production. This method is particularly useful for individuals experiencing fatigue or those recovering from strenuous physical activities. Studies have indicated that IV nutrient therapy can enhance metabolic efficiency and support better energy balance in patients, leading to improved overall vitality and reduced feelings of fatigue. The immediate availability of nutrients in the bloodstream allows for quicker replenishment of energy stores, which can be especially beneficial for athletes and individuals with high energy demands.
4. Immune System Support
IV therapy can bolster the immune system by delivering high concentrations of vitamins and minerals that are crucial for immune function. For instance, IV infusions of vitamins such as vitamin C and trace elements like zinc and selenium have been shown to enhance immune responses and reduce the duration of illnesses. This method ensures that the immune-supporting nutrients are readily available in the bloodstream, providing a more immediate and potent effect compared to oral supplements. This can be particularly beneficial for individuals with compromised immune systems or those looking to prevent infections and illnesses.
5. Faster Medication Delivery
IV therapy allows for the rapid delivery of medications, which is essential in acute care settings where time is of the essence. The direct infusion of drugs into the bloodstream ensures that they reach their target sites quickly and efficiently, providing faster therapeutic effects. This is particularly important in emergency situations, such as severe infections or acute pain management, where immediate intervention is required. Additionally, IV administration can be more effective for medications that are poorly absorbed orally or that require precise dosing to achieve the desired therapeutic effect.
6. Athletic Performance and Recovery
IV therapy is widely used in sports medicine to enhance athletic performance and expedite recovery. By providing rapid rehydration and replenishment of electrolytes, IV therapy helps maintain optimal fluid balance and prevent dehydration-related performance declines. Studies have shown that athletes who receive IV rehydration perform better in endurance events and recover more quickly from intense physical exertion. The immediate availability of fluids and nutrients in the bloodstream helps reduce muscle cramps, fatigue, and the risk of heat-related illnesses, making IV therapy a valuable tool for athletes.
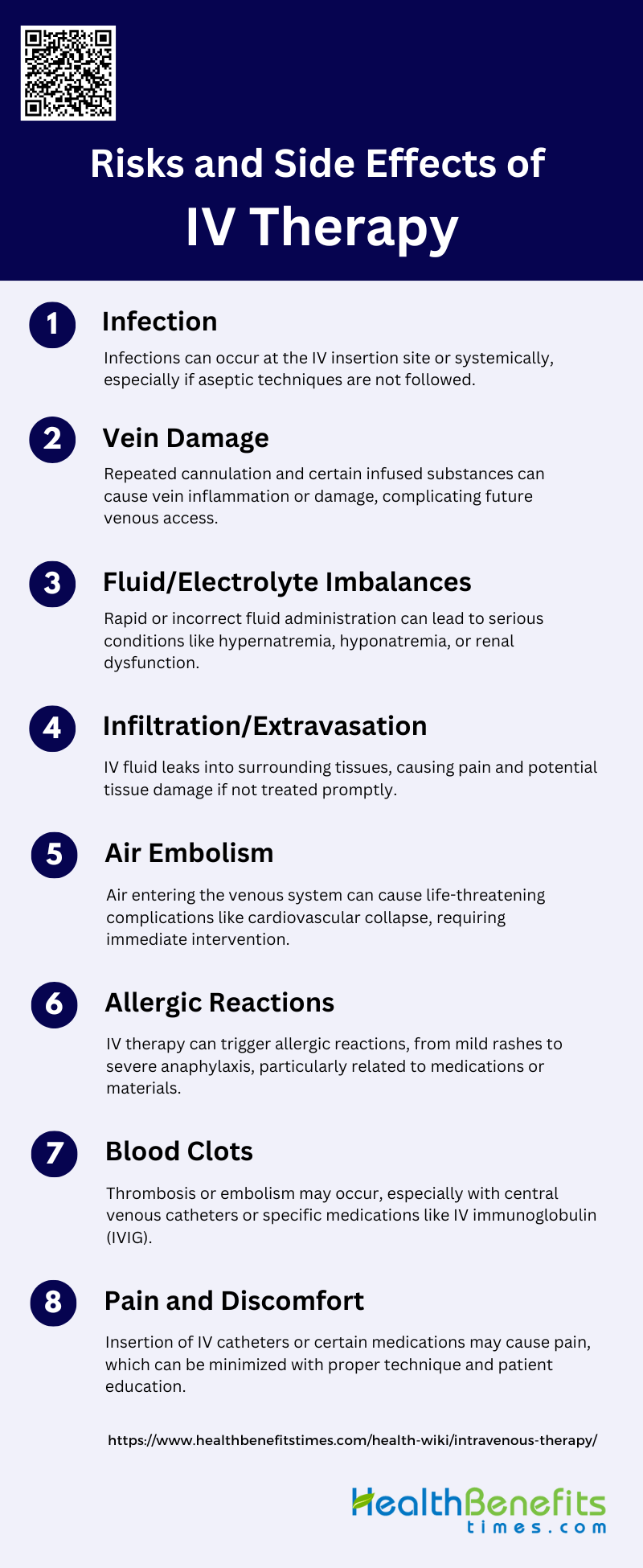
Risks and Side Effects of IV Therapy
While IV therapy offers numerous benefits, it also comes with potential risks and side effects. Understanding these risks is crucial for ensuring safe and effective treatment. Below are some common risks and side effects associated with IV therapy:
1. Infection
Intravenous (IV) therapy carries a risk of infection, which can occur at the site of catheter insertion or systemically. Infections are often due to improper aseptic techniques or prolonged use of the IV line. The risk of infection increases with the duration of catheter placement and the type of catheter used. For instance, central venous catheters are more prone to infections compared to peripheral lines. Symptoms of infection include redness, swelling, and pain at the insertion site, along with fever and chills. Prompt recognition and treatment are crucial to prevent severe complications such as sepsis.
2. Vein Damage
Vein damage is a common complication of IV therapy, often resulting from mechanical irritation or chemical injury caused by the infused substances. Thrombophlebitis, characterized by inflammation of the vein, can occur due to mechanical, chemical, or infectious causes, leading to pain, swelling, and redness along the vein. Repeated cannulation and the use of large-bore catheters can exacerbate vein damage, making future venous access more challenging. Proper technique and the use of appropriate catheter sizes can help minimize this risk.
3. Fluid/Electrolyte Imbalances
IV therapy can lead to fluid and electrolyte imbalances, particularly when large volumes of fluids are administered rapidly or when the electrolyte composition of the IV solution is not carefully monitored. Conditions such as hypernatremia, hyponatremia, hyperkalemia, and hypokalemia can occur, leading to symptoms ranging from mild discomfort to severe, life-threatening conditions. Monitoring electrolyte levels and adjusting the IV fluid composition accordingly are essential to prevent these imbalances.
4. Infiltration/Extravasation
Infiltration and extravasation are complications where the IV fluid leaks into the surrounding tissue instead of the vein. Infiltration involves non-vesicant fluids, while extravasation involves vesicant or irritant drugs, which can cause severe tissue damage. Early signs include pain, swelling, and a feeling of tightness around the IV site. Prompt recognition and intervention are crucial to minimize tissue damage and prevent complications such as nerve damage and tissue necrosis.
5. Air Embolism
Air embolism is a rare but potentially fatal complication of IV therapy, occurring when air enters the venous system. This can happen during catheter insertion, removal, or when the IV system is not properly primed. Symptoms include sudden chest pain, shortness of breath, and hypotension. Immediate intervention is required to prevent serious outcomes, including cardiovascular collapse. Preventive measures include proper technique during catheter manipulation and ensuring the IV system is free of air.
6. Allergic Reactions
Allergic reactions to IV therapy can range from mild to severe and may include symptoms such as rash, itching, fever, and anaphylaxis. These reactions are often related to the IV medication or the materials used in the IV system. Anaphylactic reactions, although rare, require immediate treatment with epinephrine and other supportive measures. Monitoring patients for signs of allergic reactions during and after IV administration is essential for prompt management.
7. Blood Clots
Blood clots, or thromboembolic events, are a significant risk associated with IV therapy, particularly with the use of central venous catheters and certain medications like intravenous immunoglobulin (IVIG). These clots can lead to complications such as deep vein thrombosis (DVT) and pulmonary embolism. Risk factors include prolonged immobility, previous thromboembolic events, and certain medical conditions. Preventive measures include the use of anticoagulants and careful monitoring of patients at risk.
8. Pain and Discomfort
Pain and discomfort are common complaints associated with IV therapy, often resulting from the insertion of the catheter, the infusion of certain medications, or complications like infiltration and phlebitis. Proper technique during catheter insertion, the use of appropriate catheter sizes, and the administration of pain-relieving measures can help minimize these issues. Educating patients about what to expect and encouraging them to report any discomfort promptly can also aid in early intervention and management.
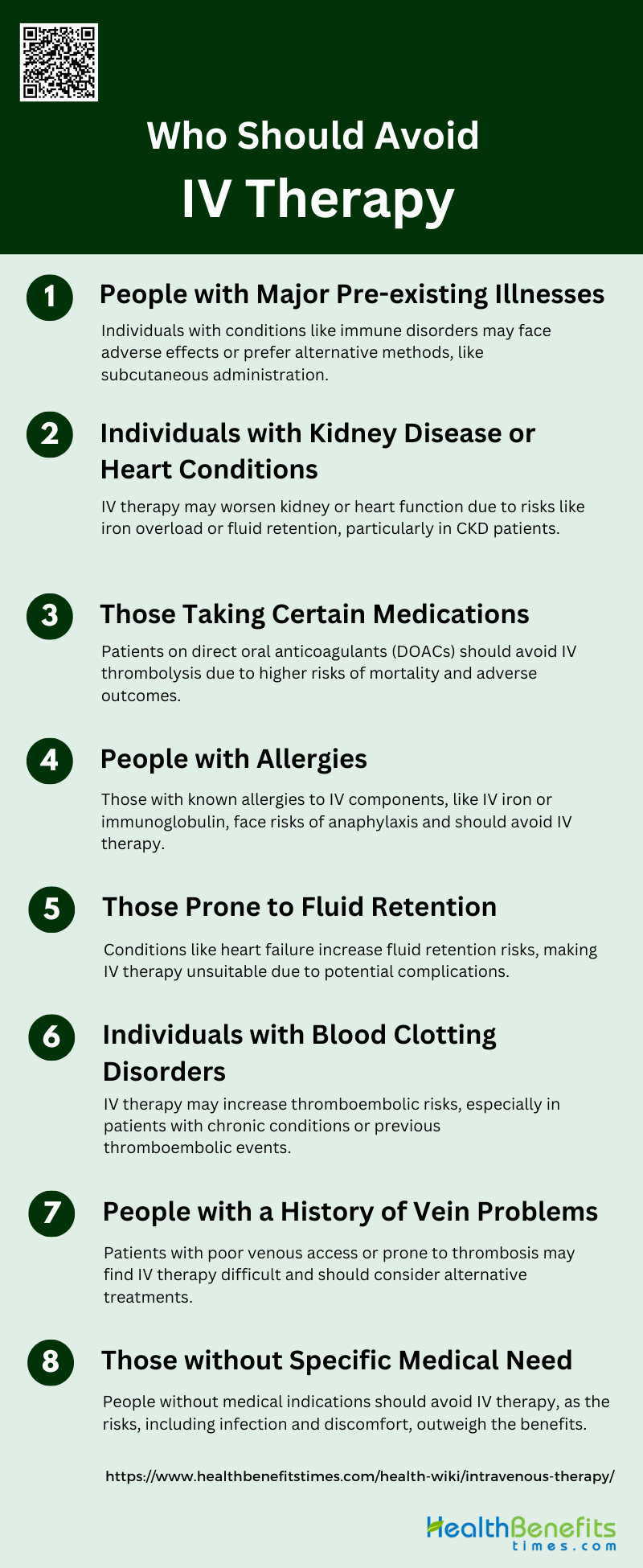
Who Should Avoid IV Therapy
While IV therapy can be beneficial for many, it is not suitable for everyone. Certain individuals may face increased risks or complications from this treatment. Below are some groups of people who should avoid IV therapy:
1. People with Major Pre-existing Illnesses
Individuals with significant pre-existing conditions, such as chronic immune system disorders, may have specific preferences and safety concerns regarding IV therapy. For example, patients with chronic immune system disorders often prefer subcutaneous administration over IV due to convenience and comfort, and to avoid frequent hospital visits. Additionally, those with conditions like multiple sclerosis may experience mild adverse effects from IV therapy, such as headaches and fatigue, which could exacerbate their existing health issues.
2. Individuals with Kidney Disease or Heart Conditions
Patients with chronic kidney disease (CKD) should be cautious with IV therapy, particularly IV iron, due to potential risks such as iron overload, cardiovascular events, and infections. Excessive iron therapy can lead to oxidative stress and tissue damage, which are particularly concerning for CKD patients. Similarly, individuals with heart conditions, such as those with MIS-C, may experience worsened cardiac function due to the large fluid volumes required for IV therapy.
3. Those Taking Certain Medications
Patients on direct oral anticoagulants (DOACs) should avoid IV thrombolysis due to the increased risk of adverse outcomes, including higher overall mortality rates and potentially lower functional neurological outcomes. The interaction between IV therapy and DOACs can complicate treatment and increase the risk of complications, making it crucial for these patients to seek alternative therapies.
4. People with Allergies
Individuals with known allergies, particularly to components of IV therapy, should avoid this treatment. For instance, patients with IgA deficiency may experience anaphylactic reactions to IV immunoglobulin (IVIg), although these reactions are largely preventable with proper precautions. Additionally, hypersensitivity reactions to IV iron have been reported, raising safety concerns for patients with chronic kidney disease.
5. Those Prone to Fluid Retention
Patients prone to fluid retention, such as those with heart conditions or certain inflammatory syndromes like MIS-C, should avoid IV therapy due to the risk of exacerbating their condition. The large fluid volumes required for IVIg can worsen cardiac function, making it necessary to consider alternative treatments that do not involve significant fluid administration.
6. Individuals with Blood Clotting Disorders
Individuals with blood clotting disorders or those at risk of thromboembolic events should be cautious with IV therapy. IVIg can increase the risk of thromboembolic complications, particularly in patients with risk factors such as advanced age, previous thromboembolic events, and certain chronic conditions. Proper hydration and slow infusion rates can mitigate some risks, but alternative therapies may be safer for these patients.
7. People with a History of Vein Problems
Patients with a history of vein problems, such as those prone to thrombosis or with poor venous access, may find IV therapy challenging and risky. The administration of IV treatments can exacerbate vein issues, leading to complications such as thrombophlebitis or difficulty in maintaining IV access. These patients may benefit from alternative routes of administration, such as subcutaneous injections, which are often preferred for their convenience and reduced risk of vein-related complications.
8. Those That Don’t Have a Specific Medical Need
Individuals without a specific medical need for IV therapy should avoid it due to the potential risks and discomfort associated with the treatment. IV therapy can cause mild to severe adverse effects, including headaches, fatigue, and more serious complications like renal failure and thromboembolic events. Without a clear medical indication, the risks may outweigh the benefits, making it prudent to consider less invasive treatment options.
Safety and Considerations of IV therapy
Ensuring the safety and effectiveness of IV therapy involves several critical factors. Proper administration, sterility, and professional guidance are essential to minimize risks and maximize benefits. Below are key safety considerations for IV therapy:
1. Licensed Professionals
Administering intravenous (IV) therapy requires a high level of expertise and precision, making it essential for certified healthcare providers to perform this task. Proper administration involves not only the correct insertion of the IV line but also the accurate calculation and delivery of medication dosages. Inadequate training or lack of certification can lead to severe complications, including infections, incorrect dosages, and even fatal outcomes. According to a systematic review, the safe preparation and administration of IV therapy are critical to patient safety, emphasizing the need for adherence to best practice standards by trained professionals. Additionally, the UK National Institute for Health and Care Excellence (NICE) highlights the importance of proper education for doctors in administering IV fluids to prevent complications.
2. Sterility and Monitoring
Maintaining sterility during IV therapy is crucial to prevent infections and other complications. The process involves using sterile equipment and following strict hygiene protocols. Continuous patient monitoring is equally important to detect any adverse reactions or complications early. A systematic review underscores the necessity of best practice standards in the preparation and administration of IV therapy to ensure patient safety. Furthermore, the NICE guidelines stress the importance of proper assessment and monitoring to avoid complications arising from incorrect fluid administration. These measures are vital in minimizing risks and ensuring the effective and safe delivery of IV therapy.
3. Consulting with a Doctor
Before considering wellness IV therapy, it is crucial to consult with a healthcare provider to ensure it is appropriate for your specific health needs. Wellness IV therapies often promise benefits like improved hydration, enhanced energy, and better overall health, but they are not without risks. Medical consultation helps in assessing whether the therapy is necessary and safe, considering your medical history and current health status. The NICE guidelines emphasize the importance of proper assessment by healthcare professionals to determine the need for IV therapy and to tailor the treatment to individual patient needs. This step is essential to avoid potential complications and to ensure that the therapy will be beneficial rather than harmful.
FAQs
1. How long does an IV therapy session typically last?
The duration of an IV therapy session can vary depending on the type of therapy being administered. Hydration or vitamin therapy can take anywhere from 30 minutes to an hour, while more complex treatments like chemotherapy or blood transfusions may last several hours.
2. Can IV therapy be done at home?
Yes, some types of IV therapy, like hydration or nutritional support, can be administered at home under the supervision of a trained healthcare provider. However, more complex therapies like chemotherapy or certain medications usually require a clinical setting for safety.
3. What is the difference between IV therapy and oral medication?
IV therapy delivers medications, fluids, or nutrients directly into the bloodstream, allowing for faster absorption and immediate effects. Oral medications must pass through the digestive system, which can delay their effectiveness and reduce absorption.
4. Is IV therapy covered by insurance?
Many IV therapies, especially those administered in a hospital or for critical treatments like chemotherapy or hydration after surgery, are covered by insurance. However, wellness or vitamin IV treatments are typically not covered by insurance as they are considered elective or non-essential.
5. Can IV therapy be used to treat chronic conditions?
Yes, IV therapy is often used to manage chronic conditions such as autoimmune diseases, cancer, and nutritional deficiencies. For example, IV infusions of immunoglobulins or certain medications may be part of long-term treatment plans.
6. How do I know if I need IV therapy?
A healthcare professional can evaluate your condition to determine if IV therapy is necessary. Indications for IV therapy can include severe dehydration, nutrient deficiencies, the need for rapid medication delivery, or ongoing chronic illness management.
7. Are there alternative treatments to IV therapy?
In some cases, alternatives like oral medications, subcutaneous injections, or intramuscular injections can be used instead of IV therapy, depending on the specific condition and the patient’s needs. Always consult with a healthcare provider to determine the best treatment option.
8. How do healthcare providers ensure IV therapy is administered safely?
Healthcare providers use sterile techniques, monitor the IV site regularly, and ensure that the proper dosage and fluid rates are maintained. They also closely observe for any adverse reactions or complications such as infections, infiltration, or blood clots.
9. Can children receive IV therapy?
Yes, children can receive IV therapy, particularly in cases of dehydration, severe infections, or to deliver medications that cannot be taken orally. Pediatric IV therapy is administered with special care to ensure the correct dosage and minimize discomfort.
10. Can I eat or drink before IV therapy?
Whether or not you can eat or drink before IV therapy depends on the type of treatment being administered. For simple hydration or vitamin infusions, eating or drinking may be allowed. However, for certain medications or surgeries requiring IV therapy, fasting might be necessary. Always follow the guidance of your healthcare provider.