Inflammation is a complex biological response of the body’s vascular tissues to harmful stimuli such as pathogens, damaged cells, or irritants. This process is crucial for initiating the healing process and involves a series of events including increased blood flow, the release of fluid and plasma proteins into the affected tissues, and the migration of white blood cells to the site of injury or infection. Inflammation can be classified as acute, which occurs over a short period and is characterized by the presence of neutrophils, or chronic, which persists for longer durations and involves various immune cells like monocytes and lymphocytes. While inflammation is fundamentally a protective mechanism, it can become pathological if it is excessive or prolonged, potentially leading to tissue damage and contributing to various chronic diseases.
Types of Inflammation
Inflammation is a complex biological response of body tissues to harmful stimuli such as pathogens, damaged cells, or irritants. It is a protective response involving immune cells, blood vessels, and molecular mediators. There are three primary types of inflammation, each with distinct characteristics and durations:
1. Acute Inflammation
Acute inflammation is an immediate and early response to tissue injury or infection, characterized by a series of well-coordinated events aimed at eliminating the initial cause of cell injury, clearing out necrotic cells and tissues, and establishing a repair process. This response involves the leakage of water, salt, and proteins from the vascular compartment, activation of endothelial cells, and recruitment of leukocytes to the site of injury. Neutrophils, or polymorphonuclear leukocytes (PMNs), are among the first responders, adhering to the vascular endothelium and migrating to the affected tissue. The process also includes the activation of tissue macrophages, platelets, and the complement system, as well as the release of proteases and oxidants from phagocytic cells, all of which help in coping with the injury.
2. Subacute Inflammation
Subacute inflammation represents a transitional phase between acute and chronic inflammation. It typically occurs when the acute inflammatory response is insufficient to completely resolve the injury or infection, leading to a prolonged but not yet chronic state. During this phase, the inflammatory response is still active, but the intensity and cellular composition may differ from the acute phase. Subacute inflammation often involves a mix of neutrophils, macrophages, and lymphocytes, and can be characterized by ongoing tissue repair and regeneration processes. The presence of subacute inflammation indicates that the body is still attempting to resolve the injury and restore homeostasis, but the process is taking longer than in the acute phase.
3. Chronic Inflammation
Chronic inflammation is a prolonged inflammatory response that can last for months or even years. Unlike acute inflammation, which is a rapid and self-limiting process, chronic inflammation is characterized by the continuous presence of inflammatory cells, such as macrophages, lymphocytes, and plasma cells, in the affected tissues. This type of inflammation often results from the failure to eliminate the initial cause of inflammation, persistent infections, autoimmune reactions, or prolonged exposure to irritants. Chronic inflammation can lead to tissue damage and fibrosis, and is associated with various diseases, including cardiovascular diseases, type 2 diabetes, and cancer. Key mediators of chronic inflammation include cytokines like TNF-α, IL-6, and TGF-β, which play roles in promoting tissue damage and disease progression.
Causes of Inflammation
Inflammation is a natural response of the body to injury or infection, aimed at removing harmful stimuli and initiating the healing process. Various factors can trigger inflammation, including pathogens, damaged cells, and toxic compounds. Below are some common causes of inflammation:
1. Infections
Infections caused by bacteria, viruses, and fungi are significant contributors to inflammation. The human body interacts with these pathogens at mucosal sites, where the immune system must balance tolerance and defense. Disruptions in this balance can lead to chronic inflammation and autoimmune diseases. For instance, variations in gut microbiota composition have been linked to inflammatory bowel diseases and rheumatoid arthritis (RA). Lyme arthritis, caused by Borrelia burgdorferi, exemplifies how bacterial infections can trigger persistent inflammatory responses even after the pathogen is eradicated. Additionally, the role of infections in autoimmune diseases like rheumatoid arthritis is well-documented, with various microorganisms suspected of provoking the disease.
2. Injuries
Physical trauma and chemical irritation are common causes of inflammation. When tissues are damaged, the body initiates an inflammatory response to repair the injury and prevent infection. This response involves the recruitment of immune cells to the site of injury, which release cytokines and other mediators to promote healing. However, chronic exposure to irritants or repeated injuries can lead to sustained inflammation, contributing to diseases such as rheumatoid arthritis and inflammatory bowel disease. Environmental factors, including industrial toxicants and pollutants, can also exacerbate inflammation by triggering immune responses and damaging tissues.
3. Autoimmune Diseases
Autoimmune diseases like rheumatoid arthritis (RA) and lupus are characterized by the immune system mistakenly attacking the body’s own tissues, leading to chronic inflammation. These diseases result from a complex interplay of genetic and environmental factors. For example, oxidative stress and lipid mediators can modulate immune cell functions, intensifying inflammation in autoimmune conditions. In RA, infections and dysbiosis of the microbiota can further exacerbate the disease by influencing immune responses and promoting chronic inflammation. The persistence of inflammation in autoimmune diseases often requires targeted therapeutic strategies to manage symptoms and prevent tissue damage.
4. Lifestyle Factors
Lifestyle factors such as diet, stress, and lack of exercise significantly influence inflammation. Poor diet and physical inactivity are known to promote systemic chronic inflammation (SCI), which is linked to various diseases, including cardiovascular disease, diabetes, and autoimmune disorders. Psychological stress can also trigger inflammatory responses by affecting the immune system’s regulation. Conversely, regular exercise has been shown to have anti-inflammatory effects, improving clinical outcomes in autoimmune rheumatic diseases by reducing systemic inflammation. Addressing these lifestyle factors through dietary modifications, stress management, and physical activity can help mitigate chronic inflammation and its associated health risks.
Symptoms of Inflammation
Inflammation manifests through various symptoms that can be categorized based on the duration and nature of the inflammatory response. These symptoms help in identifying the type and severity of inflammation. Below are the primary symptoms of inflammation:
1. Acute Symptoms
Acute inflammation is characterized by rapid onset and short duration, typically manifesting within minutes to hours. The cardinal signs of acute inflammation include redness, swelling, pain, heat, and loss of function, which are essential for pathogen control and tissue repair. For instance, in the context of pelvic inflammatory disease, acute symptoms can include severe abdominal pain, fever, and abnormal vaginal discharge, which require immediate medical attention to prevent complications such as infertility and ectopic pregnancy. Additionally, acute inflammation is often associated with systemic responses such as fever and elevated levels of inflammatory markers like C-reactive protein (CRP) and interleukin-6 (IL-6).
2. Chronic Symptoms
Chronic inflammation, on the other hand, is a prolonged inflammatory response that can last for months or even years, often leading to tissue damage and contributing to various chronic diseases. Chronic inflammation is commonly associated with conditions such as cardiovascular diseases, diabetes, cancer, and neurodegenerative disorders. For example, chronic prostate inflammation has been linked to the progression of benign prostatic hyperplasia and lower urinary tract symptoms, including increased urinary frequency, urgency, and nocturia. In elderly populations, low-level systemic inflammation is frequently observed and is associated with age-related diseases, highlighting the detrimental effects of chronic inflammatory processes on overall health. Chronic inflammation can also lead to persistent symptoms such as fatigue, pain, and cognitive impairments, significantly impacting the quality of life.
The Role of the Immune System
The immune system plays a crucial role in defending the body against infections and diseases. It identifies and neutralizes harmful pathogens, such as bacteria and viruses, and helps in the healing process. Below are the key functions of the immune system:
1. Defense against Pathogens
The immune system serves as the body’s primary defense mechanism against pathogens. The innate immune system, which includes pattern recognition receptors (PRRs) such as Toll-like receptors (TLRs), plays a crucial role in identifying and responding to microbial invaders. These receptors detect pathogen-associated molecular patterns (PAMPs) and initiate signaling pathways that lead to the production of antimicrobial genes and inflammatory cytokines, effectively orchestrating an early host response to infection. This initial response is essential for containing infections and preventing their spread, while also setting the stage for the activation of the adaptive immune system, which provides a more targeted and long-lasting defense.
2. Recognition and Memory
The immune system’s ability to recognize and remember pathogens is fundamental to its effectiveness. The innate immune system uses PRRs to detect conserved microbial structures, while the adaptive immune system relies on the diversity of T and B cell receptors to recognize specific antigens. Memory cells, generated during the initial immune response, enable the immune system to respond more rapidly and robustly upon subsequent exposures to the same pathogen. This immunological memory is a cornerstone of vaccination strategies, which aim to prime the immune system against specific pathogens without causing disease. The interplay between innate and adaptive immunity ensures a comprehensive and efficient defense mechanism.
3. Healing and Repair
Beyond its role in pathogen defense, the immune system is also integral to tissue healing and repair. Immune cells, including macrophages and dendritic cells, interact with stem cells to regulate tissue regeneration and repair processes. Cytokines produced by immune cells can promote or inhibit these processes, depending on the context. For instance, cytokines like IL-6 and TNF-α are involved in both injury and repair, highlighting the dual role of the immune system in managing damage and facilitating recovery. Understanding these interactions is crucial for developing therapeutic strategies in regenerative medicine and for treating conditions where healing processes are dysregulated.
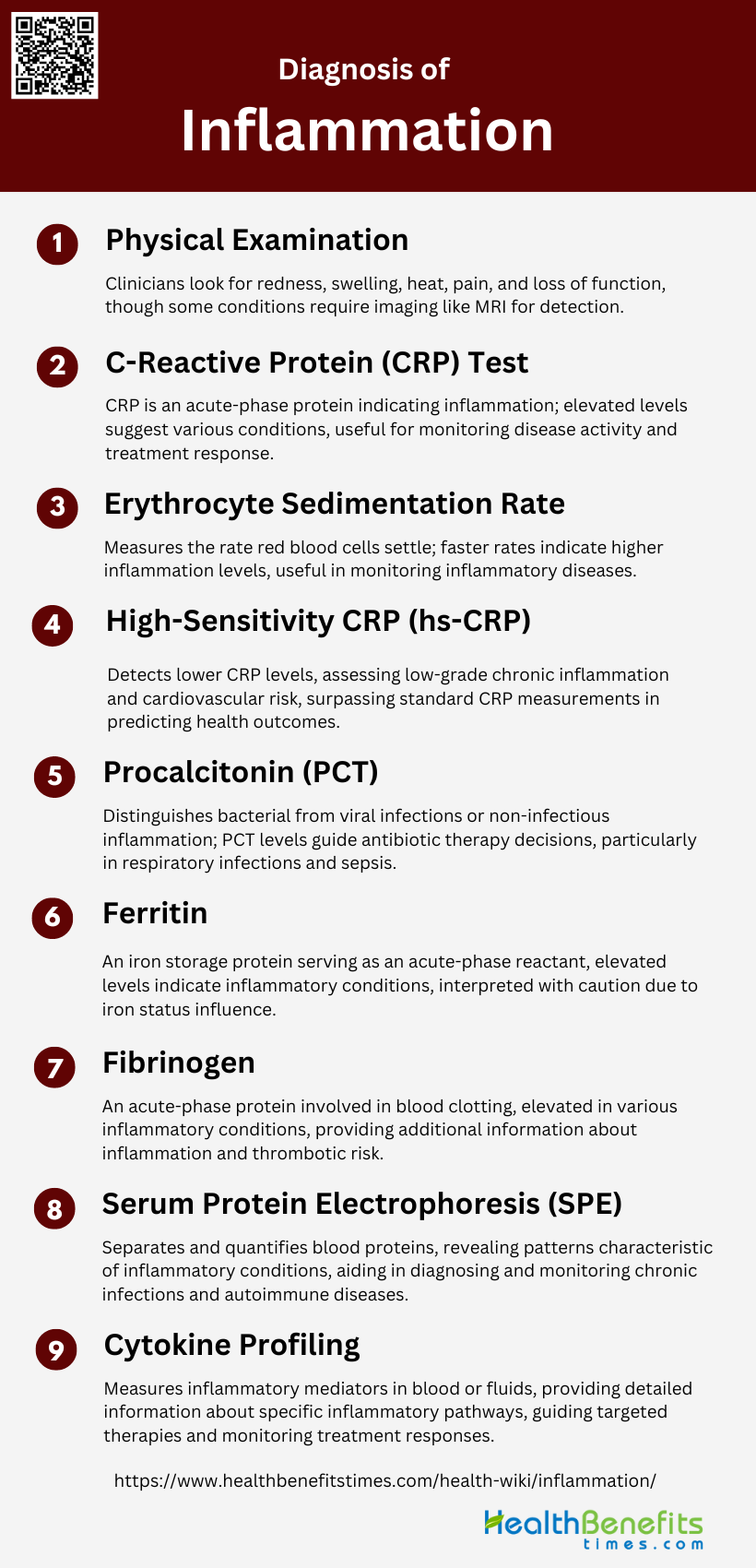
Diagnosis of Inflammation
Diagnosing inflammation involves a combination of clinical evaluation, laboratory tests, and imaging studies. Healthcare providers assess symptoms, medical history, and physical examination findings to identify the presence and cause of inflammation. Below are common methods used in the diagnosis of inflammation:
1. Physical Examination
Physical examination is a crucial first step in diagnosing inflammation. Clinicians look for cardinal signs such as redness, swelling, heat, pain, and loss of function in affected areas. Specific techniques like the “liver capsule irritation sign” can help identify conditions like perihepatitis. However, physical examination alone may not always detect inflammation, especially in deep tissues or early stages of disease. For example, in joint inflammation, MRI has been shown to be more sensitive than physical examination in detecting synovitis and bone marrow edema, particularly in metatarsophalangeal joints.
2. C-Reactive Protein (CRP) Test
The C-Reactive Protein (CRP) test is a widely used biomarker for inflammation. CRP is an acute-phase protein produced by the liver in response to inflammation. Elevated CRP levels can indicate various inflammatory conditions, infections, or tissue damage. However, CRP is non-specific and can be elevated in numerous conditions. Recent research has explored DNA methylation signatures of CRP as potentially more reliable markers of chronic inflammation. The CRP test is valuable for monitoring disease activity and treatment response in conditions like rheumatoid arthritis and cardiovascular diseases.
3. Erythrocyte Sedimentation Rate (ESR)
The Erythrocyte Sedimentation Rate (ESR) is a classic test for assessing inflammation. It measures the rate at which red blood cells settle in a tube over time, with faster sedimentation indicating higher levels of inflammation. ESR remains useful for monitoring inflammatory diseases, particularly rheumatoid arthritis, temporal arteritis, and polymyalgia rheumatica. While the traditional Westergren method is still considered the reference standard, automated closed systems have been developed to improve efficiency and reduce biohazard risks. Standardization efforts are ongoing to ensure comparability of results across different laboratories and methods.
4. High-Sensitivity CRP (hs-CRP)
High-sensitivity CRP (hs-CRP) is a more precise measurement of CRP levels, capable of detecting lower concentrations than standard CRP tests. This increased sensitivity makes hs-CRP particularly useful for assessing low-grade chronic inflammation and cardiovascular risk. Research has shown that hs-CRP can be a valuable predictor of various health outcomes, often surpassing standard CRP measurements and genetic scores in its associations with multiple health conditions. The hs-CRP test is increasingly used in cardiovascular risk assessment and monitoring of chronic inflammatory conditions.
5. Procalcitonin (PCT)
Procalcitonin (PCT) is a biomarker primarily used to distinguish between bacterial and viral infections or non-infectious causes of inflammation. PCT levels rise more quickly than CRP in response to bacterial infections and decrease rapidly with effective antibiotic treatment. While not mentioned explicitly in the search results, PCT is valuable in guiding antibiotic therapy decisions, particularly in respiratory infections and sepsis. It helps clinicians differentiate between bacterial infections requiring antibiotics and viral infections or non-infectious inflammatory conditions where antibiotics are unnecessary.
6. Ferritin
Ferritin, while primarily known as an iron storage protein, also serves as an acute-phase reactant in inflammation. Elevated ferritin levels can indicate various inflammatory conditions, including rheumatoid arthritis, still’s disease, and hemophagocytic lymphohistiocytosis. However, ferritin levels must be interpreted cautiously, as they can also be affected by iron status. In the context of inflammation diagnosis, ferritin is often used in conjunction with other markers to provide a more comprehensive assessment of inflammatory status and potential underlying causes.
7. Fibrinogen
Fibrinogen is another acute-phase protein that increases during inflammation. It plays a crucial role in blood clotting and is often elevated in various inflammatory conditions, including cardiovascular diseases, infections, and autoimmune disorders. While not specifically mentioned in the search results, fibrinogen levels can provide additional information about the inflammatory state and potential thrombotic risk. Elevated fibrinogen levels, along with other inflammatory markers, can help clinicians assess the severity and progression of inflammatory diseases.
8. Serum Protein Electrophoresis (SPE)
Serum Protein Electrophoresis (SPE) is a test that separates and quantifies different protein fractions in the blood. In the context of inflammation diagnosis, SPE can reveal changes in protein patterns characteristic of various inflammatory conditions. For example, it can show increased gamma globulins in chronic inflammation or monoclonal peaks in certain blood disorders. While not directly mentioned in the search results, SPE is valuable in diagnosing and monitoring conditions like multiple myeloma, chronic infections, and autoimmune diseases, providing insights into the underlying inflammatory processes.
9. Cytokine Profiling
Cytokine profiling involves measuring levels of various inflammatory mediators in the blood or other biological fluids. This advanced technique can provide detailed information about the specific inflammatory pathways activated in different conditions. While not explicitly discussed in the search results, cytokine profiling is increasingly used in research and clinical settings to understand complex inflammatory responses. It can help differentiate between different types of inflammation, guide targeted therapies, and monitor treatment responses in conditions like rheumatoid arthritis, inflammatory bowel disease, and certain cancers.
Treatments for Inflammation
Treating inflammation involves various approaches depending on the underlying cause and severity. The primary goal is to reduce inflammation, alleviate symptoms, and address the root cause. Below are common treatments for inflammation:
1. Medications
Medications are a primary treatment for inflammation, often involving non-steroidal anti-inflammatory drugs (NSAIDs) and corticosteroids. NSAIDs, such as aspirin and ibuprofen, work by inhibiting enzymes that contribute to inflammation, providing relief from pain and swelling. Corticosteroids, like prednisone, are potent anti-inflammatory agents that suppress the immune system to reduce inflammation. However, these medications can have significant side effects, including gastrointestinal issues and increased risk of infections. Recent advancements include the development of biologics and small molecules targeting specific inflammatory pathways, offering more targeted and potentially safer options for chronic inflammatory diseases.
2. Lifestyle Changes
Lifestyle changes play a crucial role in managing inflammation. Regular physical activity, a balanced diet rich in anti-inflammatory foods, and maintaining a healthy weight can significantly reduce inflammation. Smoking cessation and limiting alcohol intake are also vital, as both habits are linked to increased inflammation and related diseases. Stress management techniques, such as mindfulness and relaxation training, have shown promise in reducing inflammatory markers in the body. These lifestyle modifications not only help in managing inflammation but also improve overall health and reduce the risk of chronic diseases.
3. Alternative Therapies
Complementary and alternative therapies (CAM) offer natural and effective options for managing inflammation. Herbal medicines, such as curcumin, ginger, and evening primrose oil, have demonstrated anti-inflammatory properties in various studies. Acupuncture has also been shown to reduce inflammation and improve symptoms in conditions like rheumatoid arthritis. Mind-body interventions, including hypnotherapy and mindfulness, have been effective in managing inflammatory bowel diseases. These therapies provide a holistic approach to inflammation management, often with fewer side effects compared to conventional medications.
4. Physical Therapy
Physical therapy is an essential component of managing inflammation, particularly in musculoskeletal conditions. It helps restore function, improve mobility, and reduce pain through targeted exercises and manual therapies. Techniques such as stretching, strengthening exercises, and hydrotherapy can alleviate symptoms and enhance recovery. Physical therapists also educate patients on proper body mechanics and ergonomics to prevent further injury and manage chronic inflammation effectively. Combining physical therapy with other treatments, such as medications and lifestyle changes, can lead to better outcomes and improved overall health.
5. Surgery
Surgery is considered a last resort for treating inflammation, typically when other treatments have failed. Inflammatory bowel diseases, such as Crohn’s disease and ulcerative colitis, may require surgical intervention to remove damaged sections of the intestine. Joint replacement surgery is another option for severe cases of rheumatoid arthritis where joint damage is extensive. While surgery can provide significant relief and improve quality of life, it comes with risks and requires careful consideration and planning. Post-surgical rehabilitation is crucial to ensure successful recovery and minimize the risk of complications.
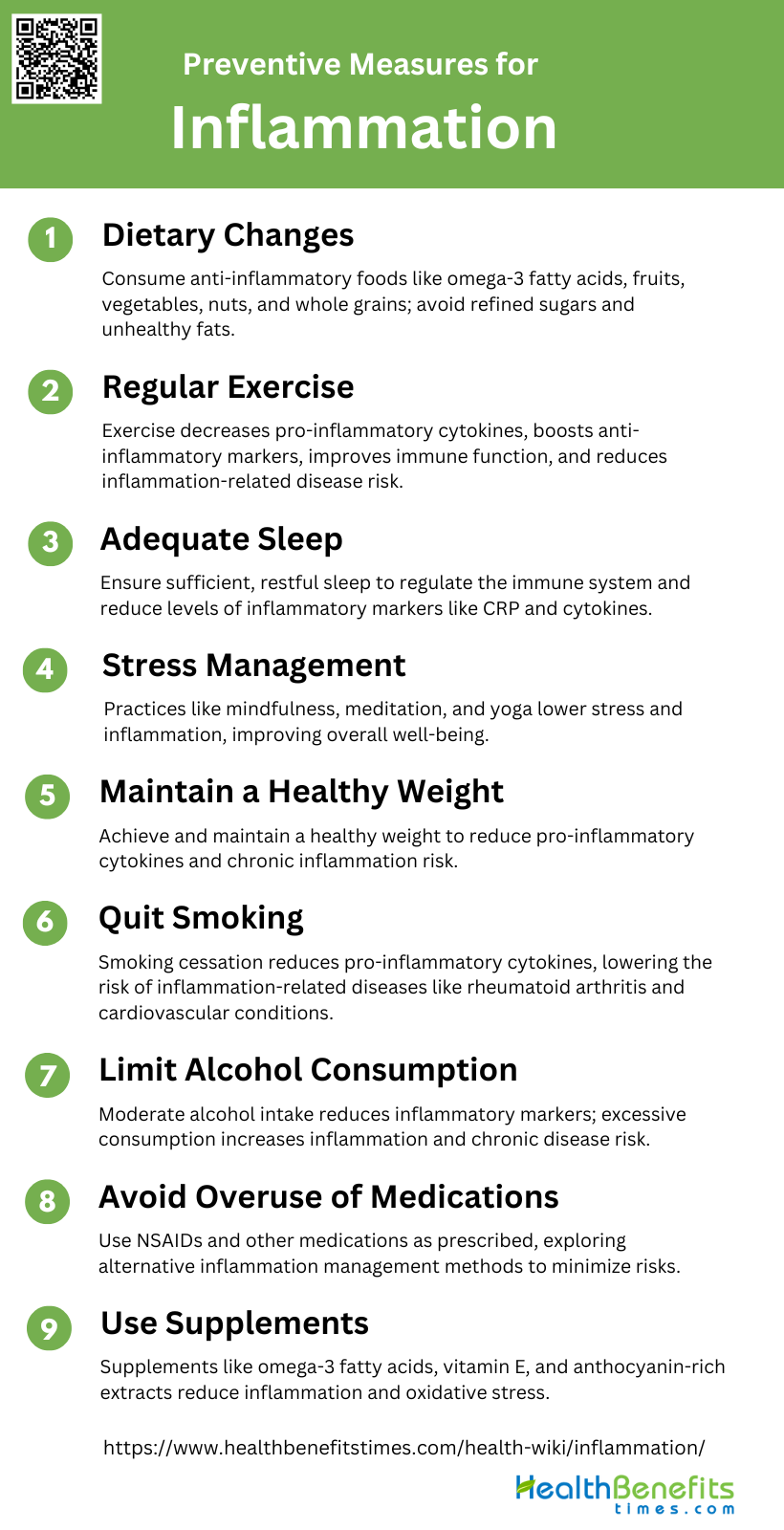
Preventive Measures for Inflammation
Preventing inflammation involves adopting healthy lifestyle habits and making informed choices to reduce risk factors. These measures can help maintain overall health and prevent chronic inflammatory conditions. Below are some effective preventive measures for inflammation:
1. Dietary Changes
Adopting a diet rich in anti-inflammatory foods can significantly reduce inflammation. Consuming omega-3 fatty acids, found in fish and flaxseeds, and increasing the intake of fruits, vegetables, nuts, and whole grains can lower the production of pro-inflammatory cytokines while boosting anti-inflammatory cytokines. Additionally, diets high in refined sugars, saturated fats, and trans fats can exacerbate inflammation, so these should be minimized. Studies have shown that dietary patterns emphasizing whole foods and balanced nutrition can help manage inflammation and reduce the risk of chronic diseases.
2. Regular Exercise
Regular physical activity is a powerful tool for reducing inflammation. Exercise has been shown to decrease levels of pro-inflammatory cytokines and increase anti-inflammatory markers in the body. Engaging in both aerobic and strength-training exercises can help manage chronic inflammation, particularly in older adults. Moreover, exercise can improve overall immune function and reduce the risk of inflammation-related diseases, making it an essential component of a healthy lifestyle.
3. Adequate Sleep
Getting sufficient sleep is vital for controlling inflammation. Poor sleep quality and sleep deprivation can lead to increased levels of inflammatory markers such as C-reactive protein (CRP) and cytokines. Ensuring adequate and restful sleep helps regulate the immune system and reduce chronic inflammation. Studies have shown that individuals who maintain good sleep hygiene have lower levels of inflammation and a reduced risk of developing chronic diseases.
4. Stress Management
Effective stress management techniques can significantly reduce inflammation. Chronic stress is associated with elevated levels of inflammatory markers, which can contribute to various health issues. Practices such as mindfulness, meditation, and yoga have been shown to lower stress and decrease inflammation. By incorporating stress-reducing activities into daily routines, individuals can improve their overall well-being and reduce the risk of inflammation-related conditions.
7. Maintain a Healthy Weight
Maintaining a healthy weight is crucial for reducing inflammation. Excess body fat, particularly visceral fat, is a significant source of pro-inflammatory cytokines. Weight loss through controlled diets or surgical interventions has been shown to reduce levels of inflammatory markers in obese and overweight individuals. By achieving and maintaining a healthy weight, individuals can lower their risk of chronic inflammation and related diseases.
6. Quit Smoking
Smoking cessation is one of the most effective ways to reduce inflammation. Smoking is a major risk factor for increased levels of pro-inflammatory cytokines and other inflammatory markers. Prolonged smoking cessation can significantly reduce the risk of inflammation-related diseases, including rheumatoid arthritis and cardiovascular conditions. Encouraging individuals to quit smoking can lead to substantial public health benefits by lowering the prevalence of chronic inflammation.
7. Limit Alcohol Consumption
Moderate alcohol consumption can have anti-inflammatory effects, but excessive intake can increase inflammation. Studies have shown that moderate alcohol consumption, particularly of beverages like red wine, can reduce levels of inflammatory markers. However, excessive alcohol intake is associated with increased inflammation and a higher risk of chronic diseases. Limiting alcohol consumption to moderate levels can help manage inflammation and promote overall health.
8. Avoid Overuse of Medications
Overuse of certain medications, particularly nonsteroidal anti-inflammatory drugs (NSAIDs), can lead to increased inflammation and other health issues. While NSAIDs can reduce inflammation in the short term, their long-term use can have adverse effects. It is essential to use medications as prescribed and explore alternative methods for managing inflammation, such as lifestyle changes and natural supplements. Consulting healthcare professionals for appropriate medication use is crucial for minimizing inflammation-related risks.
9. Use Supplements
Certain supplements can help reduce inflammation. Omega-3 fatty acids, vitamin E, and other anti-inflammatory supplements have been shown to lower levels of inflammatory markers. Additionally, plant-based supplements like anthocyanin-rich extracts from blackcurrants can support exercise recovery and reduce oxidative stress and inflammation. Incorporating these supplements into a balanced diet can enhance the body’s ability to manage inflammation and improve overall health.