Infection is the invasion and multiplication of harmful microorganisms, such as bacteria, viruses, fungi, or parasites, within the body or a part of it. This process typically triggers the body’s immune response, leading to various symptoms and potential damage to tissues or organs. Infections can occur in different parts of the body, including the respiratory tract, gastrointestinal system, skin, or bloodstream, and can range from mild to severe in their impact. The severity and duration of an infection depend on factors such as the type of pathogen, the individual’s immune system, and the site of infection. Infections can be transmitted through various means, including person-to-person contact, contaminated surfaces, or exposure to infected bodily fluids. Understanding the nature of infections is crucial for developing effective prevention strategies, diagnostic methods, and treatment approaches in healthcare settings and public health initiatives.
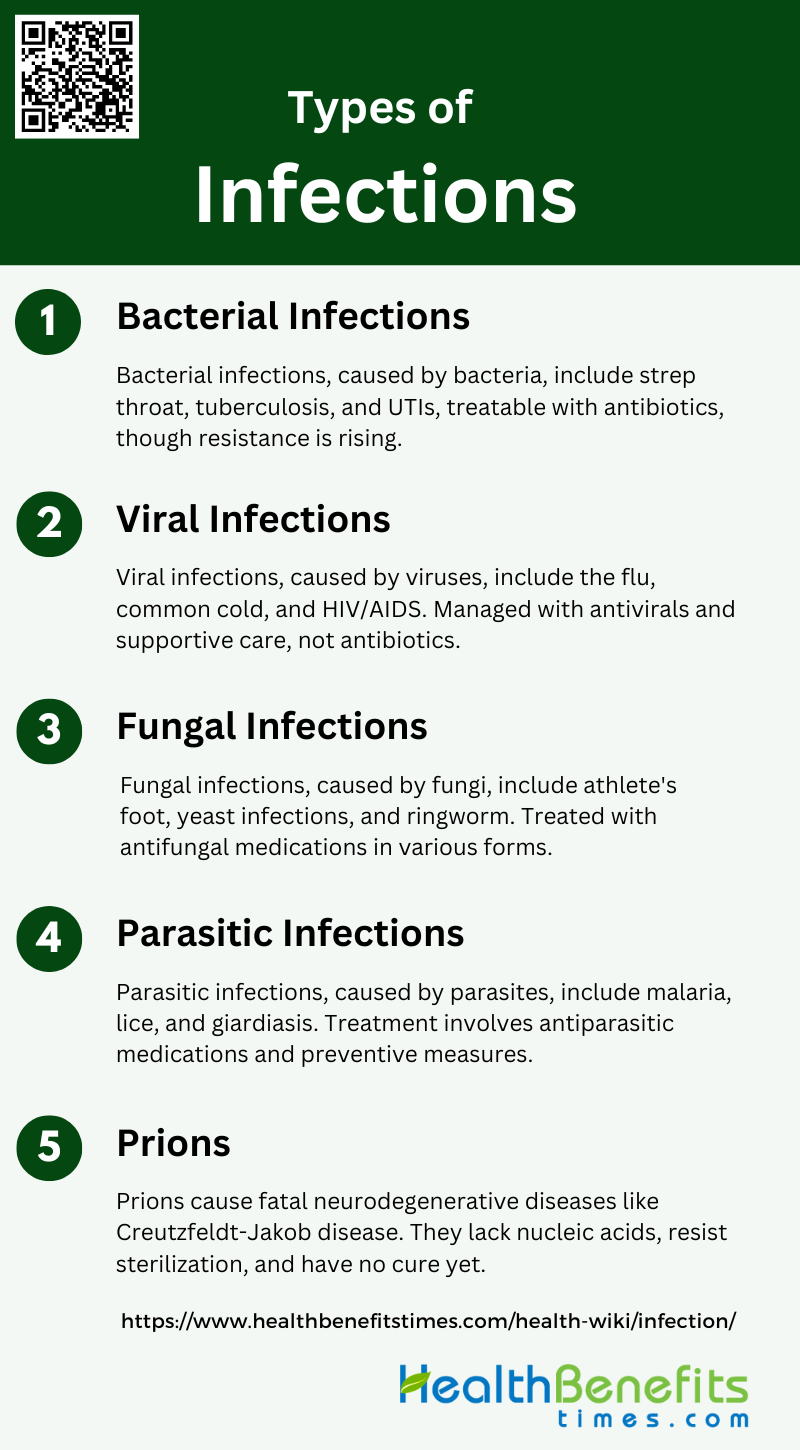
Types of Infections
Infections are caused by various pathogens, including bacteria, viruses, fungi, parasites, and prions. Each type of infection has unique characteristics, modes of transmission, and treatment methods. Below are some types of infections:
1. Bacterial Infections
Bacterial infections are caused by bacteria, single-celled microorganisms that thrive in diverse environments. Common examples include strep throat, tuberculosis, and urinary tract infections (UTIs). Strep throat, caused by Streptococcus bacteria, leads to a sore, scratchy throat and fever. Tuberculosis, a severe lung infection caused by Mycobacterium tuberculosis, can be life-threatening if untreated. UTIs, often caused by Escherichia coli, result in painful urination and frequent urges to urinate. Antibiotics are typically effective in treating bacterial infections, although antibiotic resistance is an increasing concern, necessitating careful use of these medications.
2. Viral Infections
Viral infections are illnesses caused by viruses, tiny infectious agents that require a host cell to replicate. Common viral infections include the flu, common cold, and HIV/AIDS. The flu, caused by influenza viruses, leads to fever, body aches, and respiratory symptoms. The common cold, often due to rhinoviruses, results in a runny nose, sore throat, and cough. HIV/AIDS, caused by the human immunodeficiency virus, attacks the immune system, leading to severe immunodeficiency. Unlike bacterial infections, viral infections cannot be treated with antibiotics; instead, antiviral medications and supportive care are used to manage symptoms and control the spread.
3. Fungal Infections
Fungal infections are caused by fungi, a group of organisms that include yeasts, molds, and mushrooms. Examples of fungal infections include athlete’s foot, yeast infections, and ringworm. Athlete’s foot, caused by Trichophyton fungi, affects the skin on the feet, leading to itching and scaling. Yeast infections, often due to Candida species, can occur in various body parts, including the mouth and genital areas, causing discomfort and discharge. Ringworm, a contagious fungal infection, results in ring-shaped, red, itchy patches on the skin. Antifungal medications, available as creams, ointments, or oral drugs, are used to treat these infections.
4. Parasitic Infections
Parasitic infections are caused by parasites, organisms that live on or inside a host and benefit at the host’s expense. Examples include malaria, lice, and giardiasis. Malaria, transmitted by Anopheles mosquitoes, is caused by Plasmodium parasites and leads to fever, chills, and anemia. Lice infestations, caused by tiny insects, result in itching and discomfort, particularly on the scalp. Giardiasis, a gastrointestinal infection caused by the Giardia parasite, leads to diarrhea, stomach cramps, and nausea. Treatment for parasitic infections varies but often includes antiparasitic medications and measures to prevent re-infestation or transmission.
5. Prions
Prions are infectious proteins that cause rare but fatal neurodegenerative diseases. Unlike other infectious agents, prions lack nucleic acids and replicate by inducing abnormal folding of normal cellular proteins. An example of a prion disease is Creutzfeldt-Jakob disease (CJD), which leads to rapid mental deterioration, movement disorders, and ultimately death. Prion diseases are characterized by long incubation periods and are resistant to standard sterilization processes. There is currently no cure for prion diseases, and treatment focuses on alleviating symptoms and providing supportive care. Research is ongoing to understand prion mechanisms and develop potential therapies.
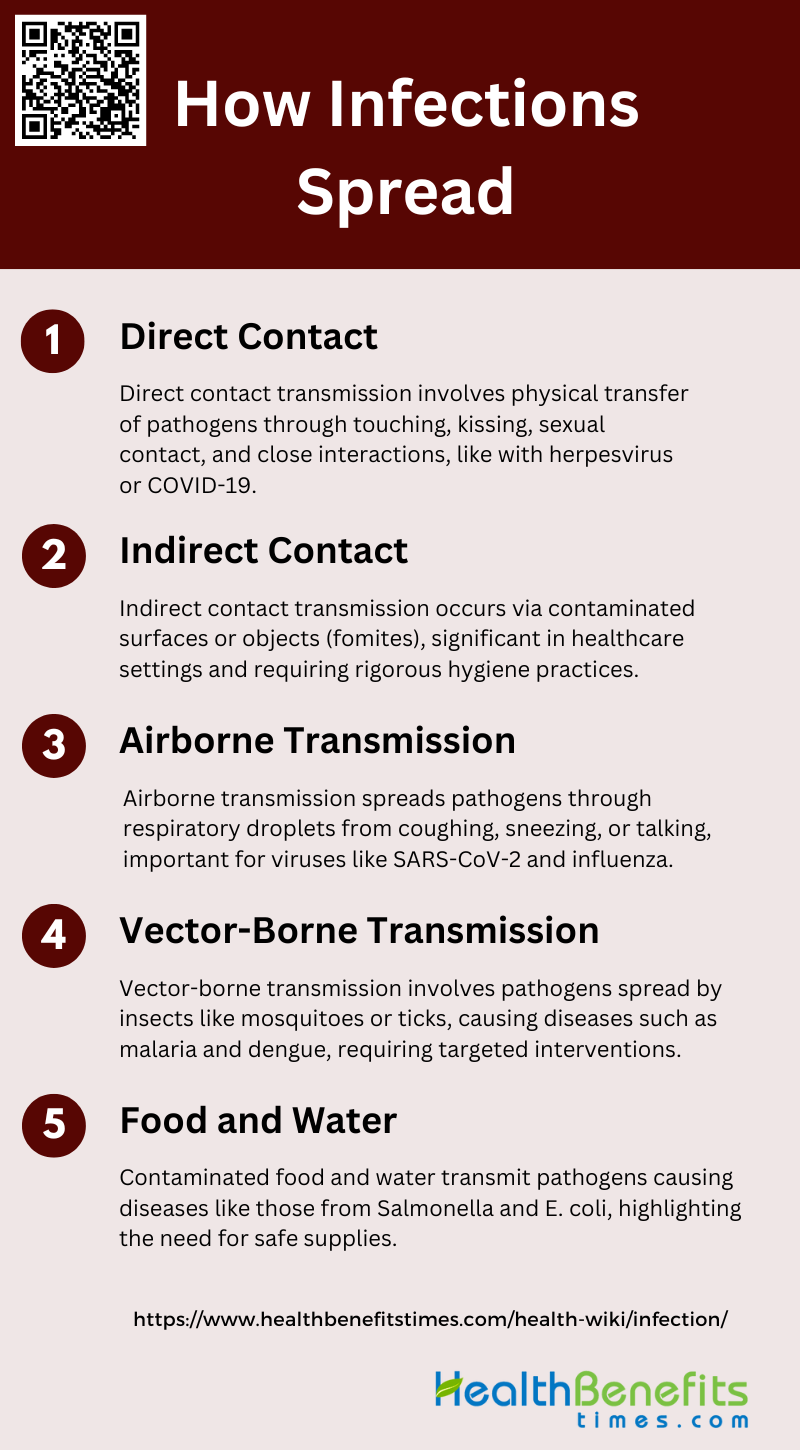
How Infections Spread
Infections spread through various mechanisms, including direct contact, airborne transmission, contaminated surfaces, and vectors like insects. Understanding these pathways is crucial for implementing effective prevention and control measures. Below are the primary ways infections can spread:
1. Direct Contact
Transmission through direct contact involves the physical transfer of pathogens from an infected individual to a susceptible person. This can occur through touching, kissing, sexual contact, or any other form of close physical interaction. For instance, herpesvirus is commonly spread through direct contact with an infected person. In the context of livestock, direct contact such as animal exchanges is a significant route for the spread of infectious diseases. The COVID-19 virus also spreads through direct person-to-person contact, highlighting the importance of minimizing close interactions to control outbreaks.
2. Indirect Contact
Indirect contact transmission occurs when pathogens are transferred via contaminated surfaces or objects, known as fomites. This mode of transmission is significant in healthcare settings, where viruses like SARS-CoV and influenza can survive on surfaces for extended periods, leading to infections when individuals touch these surfaces and subsequently touch their face. In dairy farms, indirect contacts such as contaminated equipment and vehicles have been shown to play a crucial role in the spread of diseases. The COVID-19 virus can also spread through touching contaminated objects, emphasizing the need for rigorous hygiene practices.
3. Airborne Transmission
Airborne transmission involves the spread of pathogens through respiratory droplets that are expelled when an infected person coughs, sneezes, or talks. These droplets can remain suspended in the air and be inhaled by others, leading to new infections. Respiratory viruses like SARS-CoV-2, influenza, and RSV are known to spread through airborne transmission, which can occur over both short and long distances. In hospitals, controlling airborne transmission is challenging but crucial, as it can lead to significant morbidity and mortality. The COVID-19 pandemic has underscored the importance of understanding and mitigating airborne transmission to prevent widespread outbreaks.
4. Vector-Borne Transmission
Vector-borne transmission occurs when pathogens are transmitted through vectors such as mosquitoes, ticks, or other insects. Diseases like malaria, dengue, and yellow fever are spread by mosquitoes that breed in or near water. Modelling vector-borne diseases presents unique challenges, including understanding the roles of different hosts and the dynamics of transmission close to elimination. Effective control of vector-borne diseases often requires targeted interventions to reduce vector populations and interrupt transmission cycles.
5. Food and Water
Contaminated food and water can serve as vehicles for the transmission of various pathogens. Water-borne diseases such as those caused by Salmonella, Escherichia coli, and Vibrio are common examples. Viruses capable of being foodborne typically follow an anal-oral transmission cycle, where they enter the body through ingestion and are shed in feces, contaminating food and water sources. Ensuring the safety of food and water supplies is critical to preventing outbreaks of foodborne diseases, which can have significant public health impacts.
Symptoms of Infections
Infections can manifest through a variety of symptoms, which can be general or specific depending on the type of pathogen involved. Recognizing these symptoms is crucial for timely diagnosis and treatment. Below are the common symptoms associated with infections:
1. General Symptoms
Infections often present with a range of general symptoms that can affect multiple systems in the body. Common general symptoms include fever, which is an elevated body temperature indicating the body’s response to infection. Fatigue is another prevalent symptom, characterized by a persistent feeling of tiredness and lack of energy. Aches and pains, often referred to as myalgia, are also common and can affect muscles and joints. These symptoms are nonspecific and can be seen in various infections, making them important initial indicators but not definitive for diagnosing a specific type of infection.
2. Specific Symptoms Based on Infection Type
Different types of infections can present with specific symptoms that help in identifying the causative agent. For instance, respiratory infections like COVID-19 often manifest with symptoms such as cough, shortness of breath, and loss of taste or smell. Urinary tract infections (UTIs) typically present with symptoms like painful urination, frequent urge to urinate, and lower abdominal pain. Skin infections may show localized redness, swelling, and pus formation. In elderly individuals, infections can present with atypical symptoms such as confusion, restlessness, and decreased appetite, which are crucial for early detection and treatment. Understanding these specific symptoms aids in timely and accurate diagnosis, leading to better patient outcomes.
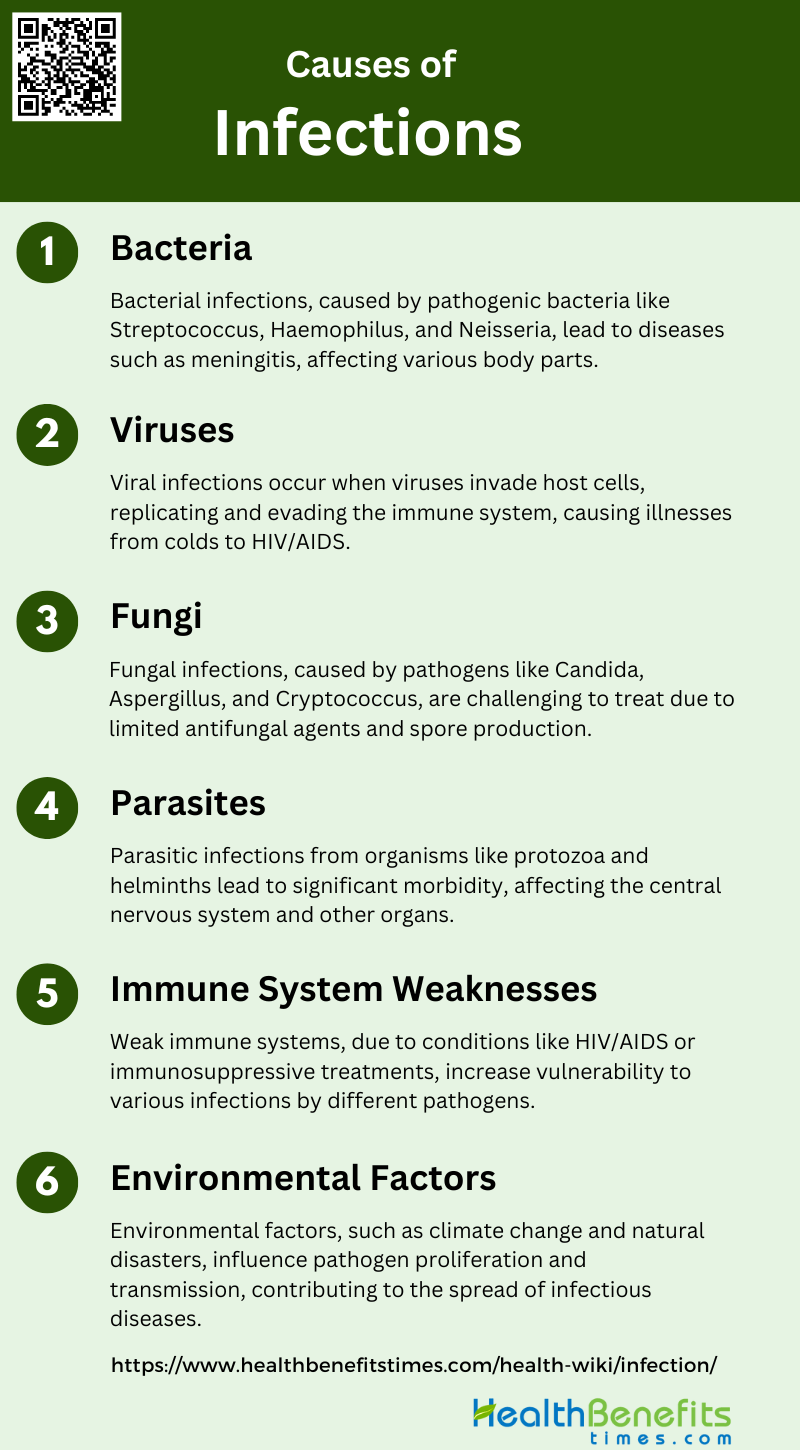
Causes of Infections
Infections are caused by various pathogens that invade the body and disrupt normal functions. These pathogens can be bacteria, viruses, fungi, parasites, or prions. Below are the primary causes of infections:
1. Bacteria
Bacterial infections are caused by pathogenic bacteria that invade the body and multiply, leading to diseases. Common bacterial pathogens include Streptococcus, Haemophilus, and Neisseria species, which are known to cause significant conditions such as meningitis. Bacterial infections can affect various parts of the body, including the central nervous system, where they can lead to severe complications like cerebritis and abscess formation. These infections are often diagnosed through neuroimaging techniques that reveal characteristic patterns. The immune system plays a crucial role in combating bacterial infections, utilizing both innate and adaptive responses to eliminate the pathogens.
2. Viruses
Viral infections occur when viruses invade host cells and hijack their machinery to replicate. These infections can range from mild illnesses like the common cold to severe diseases such as HIV/AIDS. Viruses are adept at evading the immune system, often establishing persistent infections that can be lifelong. The host immune system employs various effector functions to counteract viral infections, but viruses have evolved numerous strategies to evade these defenses, making treatment and eradication challenging. Understanding the interaction between viruses and the host immune system is essential for developing effective diagnostics and therapeutics.
3. Fungi
Fungal infections are caused by pathogenic fungi, which can be environmental organisms, opportunistic pathogens, or commensal organisms. These infections are particularly challenging to treat due to the limited availability of antifungal agents and the ability of fungi to produce large quantities of infectious spores. Fungal pathogens such as Candida, Aspergillus, and Cryptococcus can cause severe diseases, especially in immunocompromised individuals. Climate change is also contributing to the emergence of new fungal pathogens by altering environmental conditions and increasing the geographic range of these organisms. The immune system’s response to fungal infections involves both innate and adaptive mechanisms, but much remains to be understood about effective antifungal immunity.
4. Parasites
Parasitic infections are caused by organisms such as protozoa, helminths, and ectoparasites that live on or inside the host. These infections can lead to significant morbidity and mortality, particularly in less-developed countries. Common parasitic infections include neurocysticercosis, toxoplasmosis, and malaria, which can affect the central nervous system and other organs. Parasitic infections often coexist with other types of infections, complicating diagnosis and treatment. The immune system’s response to parasitic infections involves a complex interplay of innate and adaptive mechanisms aimed at eliminating the parasites and preventing chronic disease.
5. Immune System Weaknesses
Weaknesses in the immune system, whether acquired or inherited, can significantly increase susceptibility to infections. Conditions such as HIV/AIDS, aging, and immunosuppressive treatments can compromise the immune system, making individuals more vulnerable to infections by bacteria, viruses, fungi, and parasites. Inborn errors of immunity, such as defects in the IL-17 or CARD9 pathways, can also predispose otherwise healthy individuals to severe fungal infections. Understanding these immune deficiencies is crucial for developing targeted therapies and improving patient outcomes.
6. Environmental Factors
Environmental factors play a significant role in the emergence and spread of infectious diseases. Climate change, for instance, can create conditions that favor the proliferation of pathogens and their vectors, leading to new or reemerging infections. Environmental disruptions such as floods, storms, and hurricanes can disperse pathogens and increase the risk of infections. Additionally, changes in temperature and humidity can affect the survival and transmission of pathogens, contributing to the geographic spread of diseases. Addressing environmental factors is essential for preventing and controlling infectious diseases.
Diagnosis of Infections
Diagnosing infections involves identifying the pathogen responsible for the illness through various medical tests and examinations. Accurate diagnosis is essential for effective treatment and management. Below are the common methods used for diagnosing infections:
1. Common Diagnostic Techniques
Common diagnostic techniques for infections include blood tests, imaging, and cultures. Blood tests are often the first step, providing information on the presence of pathogens and the body’s immune response. Imaging techniques, such as X-rays, CT scans, and MRIs, help visualize internal structures and identify areas of infection. Cultures, particularly blood cultures, remain the gold standard for diagnosing bloodstream infections, although they are time-consuming. Recent advancements have introduced molecular methods to complement traditional cultures, significantly reducing the turnaround time for pathogen identification and antimicrobial susceptibility testing.
2. Rapid Diagnostic Tests
Rapid diagnostic tests (RDTs) have revolutionized the field of infectious disease diagnosis by providing quick and accurate results. These tests are particularly useful in settings where timely decision-making is crucial. For instance, rapid molecular assays like the Luminex® VERIGENE® panels can identify common bloodstream pathogens and their resistance genes within hours, compared to days required for traditional cultures. Additionally, microfluidics and biosensor-based devices are emerging as promising tools for the rapid detection of viral respiratory infections, offering portability and automation.
3. Serological Tests
Serological tests detect antibodies or antigens in the blood, providing evidence of current or past infections. These tests are essential for diagnosing viral infections like hepatitis A, where serological markers indicate the presence of the virus or the body’s immune response to it. Serological tests are also valuable in epidemiological studies and for monitoring the spread of infections. Despite their utility, these tests may sometimes lack specificity and sensitivity, necessitating the use of more advanced molecular techniques for confirmation.
4. Advanced Molecular Techniques
Advanced molecular techniques have significantly enhanced the diagnosis of infectious diseases. Methods such as polymerase chain reaction (PCR), real-time PCR, and nucleic acid amplification allow for the rapid and sensitive detection of pathogens directly from clinical samples, bypassing the need for culture. These techniques can identify unculturable or fastidious microorganisms and provide information on genetic mutations responsible for drug resistance. High-throughput sequencing and microarray technologies further enable the simultaneous detection of multiple pathogens, offering comprehensive diagnostic solutions. The integration of these advanced methods into routine clinical practice is transforming the landscape of infectious disease diagnostics, improving patient outcomes and antimicrobial stewardship.
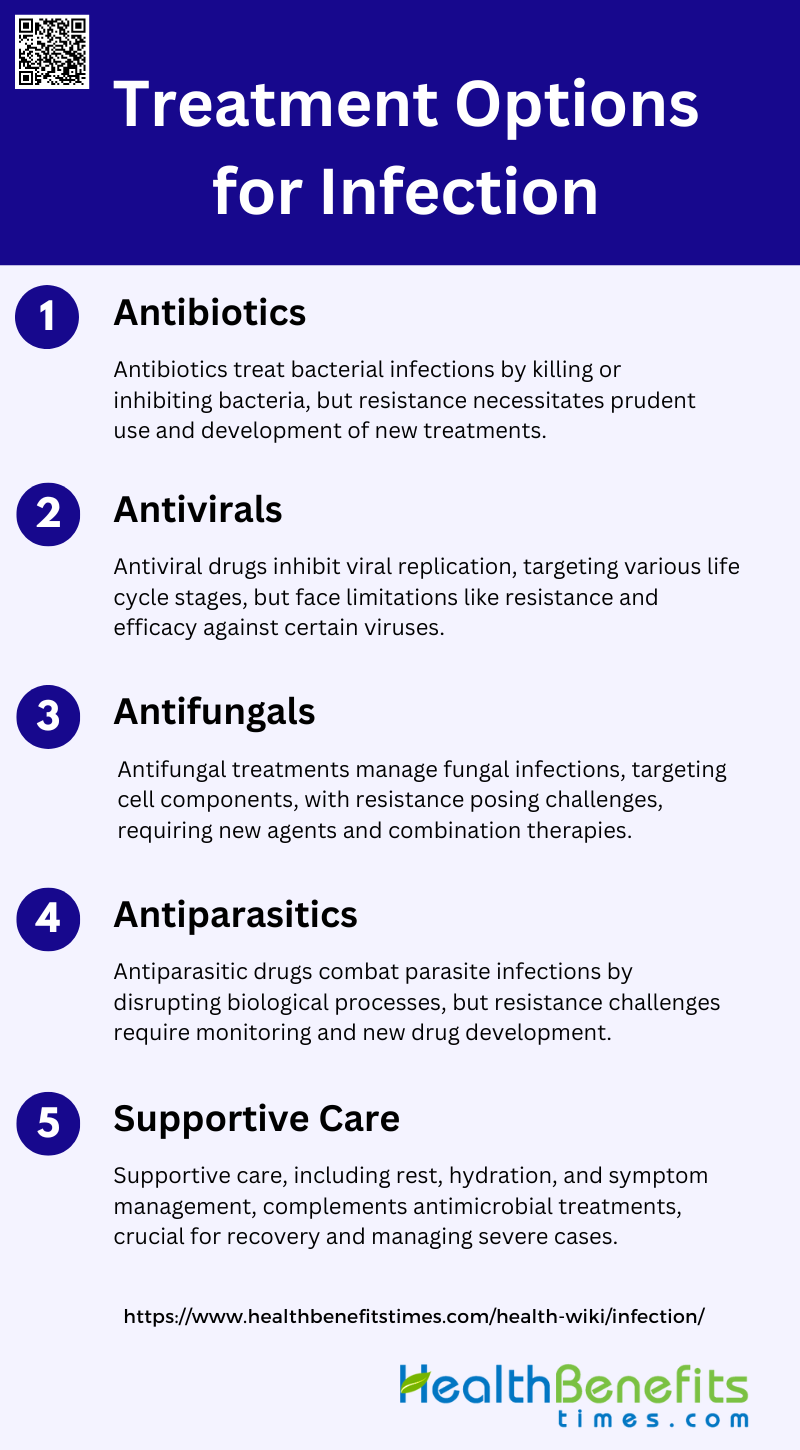
Treatment Options for Infection
Treating infections involves using various medical interventions tailored to the type of pathogen causing the illness. Effective treatment can alleviate symptoms and eliminate the infection. Below are the primary treatment options for infections:
1. Antibiotics
Antibiotics are crucial for treating bacterial infections by either killing bacteria (bactericidal) or inhibiting their growth (bacteriostatic). However, the overuse and misuse of antibiotics have led to the emergence of antibiotic-resistant bacteria, posing a significant public health threat. Resistance mechanisms include the production of enzymes that degrade antibiotics, changes in bacterial cell walls that prevent antibiotic entry, and efflux pumps that expel antibiotics from bacterial cells. Addressing antibiotic resistance requires prudent use of existing antibiotics, development of new antibiotics, and alternative treatment strategies.
2. Antivirals
Antiviral medications are designed to treat viral infections by inhibiting the replication of viruses. These drugs target various stages of the viral life cycle, such as entry into host cells, replication of viral RNA or DNA, and assembly of new viral particles. However, antiviral drugs often face limitations, including the rapid development of viral resistance and limited efficacy against certain viruses. Additionally, the high mutation rates of viruses can lead to the emergence of resistant strains, necessitating the continuous development of new antiviral agents.
3. Antifungals
Antifungal treatments are essential for managing fungal infections, which can range from superficial to life-threatening systemic infections. Current antifungal drugs include azoles, echinocandins, and polyenes, each targeting different components of fungal cells. However, the effectiveness of these treatments is compromised by the development of antifungal resistance, particularly in species like Candida and Aspergillus. Resistance mechanisms include alterations in drug targets, efflux pump overexpression, and biofilm formation. New antifungal agents and strategies, such as combination therapies and novel drug formulations, are being explored to overcome these challenges.
4. Antiparasitics
Antiparasitic treatments are used to combat infections caused by parasites, including protozoa, helminths, and ectoparasites. These drugs work by disrupting various biological processes in the parasites, such as DNA replication, protein synthesis, and metabolic pathways. However, the emergence of drug-resistant parasites poses a significant challenge to effective treatment. Resistance can arise through genetic mutations, changes in drug uptake, and metabolic adaptations. Continuous monitoring of resistance patterns and the development of new antiparasitic agents are crucial for maintaining effective treatment options.
5. Supportive Care
Supportive care plays a vital role in the management of infections, complementing specific antimicrobial treatments. Key components of supportive care include adequate rest, hydration, and nutritional support, which help the body’s immune system fight off infections. Additionally, managing symptoms such as fever and pain, and monitoring for potential complications, are essential aspects of supportive care. In severe cases, hospitalization and intensive care may be required to provide advanced supportive measures, such as intravenous fluids, oxygen therapy, and mechanical ventilation.
Prevention Strategies for Infection
Preventing infections involves adopting measures that reduce the risk of pathogen transmission and infection. These strategies are crucial for maintaining public health and personal well-being. Below are the key prevention strategies for infections:
1. Hygiene Practices
Hygiene practices, particularly hand-washing and sanitizing, are fundamental in preventing infections. Hand hygiene is a primary strategy to prevent healthcare-associated infections (HCAIs) and is crucial in both healthcare and community settings. Studies have shown that proper hand hygiene can significantly reduce the transmission of infectious diseases, including multidrug-resistant organisms. In healthcare settings, compliance with hand hygiene protocols is essential to minimize the spread of pathogens from patient to patient and within the healthcare environment. Effective hand hygiene practices, including the use of alcohol-based hand rubs, have been shown to reduce the incidence of diarrheal and respiratory infections among schoolchildren in developing countries. Therefore, promoting and adhering to hand hygiene practices is a critical component of infection prevention strategies.
2. Vaccinations
Vaccinations play a pivotal role in preventing infections by inducing immunity against specific pathogens. They are a cornerstone of public health strategies to control infectious diseases. Vaccination programs have been shown to improve healthcare workers’ adherence to infection prevention and control (IPC) guidelines, thereby reducing the risk of disease transmission in healthcare settings. For instance, combined dissemination strategies that include educational materials and vaccination campaigns have been effective in increasing vaccination uptake among healthcare workers, which in turn helps prevent the spread of respiratory infectious diseases. Vaccinations not only protect individuals but also contribute to herd immunity, reducing the overall prevalence of infectious diseases in the community.
3. Safe Food and Water Practices
Safe food and water practices are essential to prevent foodborne and waterborne infections. In the home setting, proper hygiene practices, including the cleaning and disinfection of surfaces and utensils, are crucial to reduce the risk of cross-contamination and the spread of pathogens. Ensuring the safety of food and water supplies involves multiple strategies, such as proper cooking, storage, and handling of food, as well as the use of clean water for drinking and food preparation. These practices are particularly important in preventing infections in both domestic and healthcare environments, where the risk of exposure to pathogens can be high. By implementing safe food and water practices, the incidence of infections can be significantly reduced, contributing to overall public health.
4. Avoiding Exposure to Known Sources
Avoiding exposure to known sources of infection is a key strategy in preventing the spread of infectious diseases. This involves measures such as isolating infected individuals, using personal protective equipment (PPE), and adhering to standard and transmission-based precautions in healthcare settings. In the context of the COVID-19 pandemic, compliance with IPC guidelines, including the use of PPE and maintaining physical distance, has been critical in protecting healthcare workers and patients from infection. Additionally, public health campaigns that educate individuals on how to avoid exposure to infectious agents, such as avoiding contact with sick individuals and practicing good respiratory hygiene, are essential in controlling the spread of infections in the community.
5. Strengthening the Immune System
Strengthening the immune system is an important aspect of infection prevention. This can be achieved through various means, including proper nutrition, regular exercise, adequate sleep, and stress management. Vaccinations also play a crucial role in boosting the immune system by providing immunity against specific pathogens. In healthcare settings, measures to strengthen the immune system of patients and healthcare workers, such as ensuring proper nutrition and providing vaccinations, are essential to reduce the risk of infections. Additionally, public health initiatives that promote healthy lifestyles and provide access to preventive healthcare services can help strengthen the immune system of the population, thereby reducing the overall burden of infectious diseases.
Impact of Infections
On Individual Health
Infectious diseases significantly impact individual health, leading to substantial morbidity and mortality. For instance, the Ontario Burden of Infectious Diseases Study highlights that infections such as hepatitis C, Streptococcus pneumoniae, and human immunodeficiency virus (HIV) contribute to a high number of health-adjusted life years (HALYs) lost, indicating both premature mortality and reduced quality of life due to disease. Additionally, infections with multidrug-resistant (MDR) bacteria in hospital settings are associated with increased healthcare costs, prolonged hospital stays, and higher mortality rates, further exacerbating the health burden on individuals. The social determinants of health, such as socioeconomic status and access to healthcare, also play a crucial role in the prevalence and impact of infectious diseases, influencing individual health outcomes.
Societal and Economic Impact
Infectious diseases have far-reaching socioeconomic consequences that extend beyond the immediate health sector. The economic burden includes direct costs such as healthcare expenses and indirect costs like productivity losses due to illness. For example, the COVID-19 pandemic caused significant global economic disruptions, highlighting the vulnerability of interconnected economies to infectious disease outbreaks. The financial burden of antibiotic resistance in European hospitals underscores the economic strain on healthcare systems, with increased morbidity and mortality leading to higher healthcare costs and reduced workforce productivity. Moreover, the broader economic impact includes disruptions in international travel and trade, which can lead to economic shock waves affecting various sectors.
Public Health Measures
Effective public health measures are essential to mitigate the impact of infectious diseases. The World Health Organization (WHO) emphasizes the importance of infection prevention and control (IPC) programs to reduce healthcare-associated infections (HAIs) and combat antimicrobial resistance5. Comprehensive approaches that address social determinants of health, such as improving living conditions and access to healthcare, are crucial for the prevention and control of diseases like HIV, viral hepatitis, and tuberculosis. Additionally, the use of probiotics has been shown to reduce the incidence and duration of respiratory tract infections, leading to significant cost savings for healthcare systems and society. These measures highlight the need for coordinated efforts at local, national, and international levels to effectively manage and prevent infectious diseases.