Human papillomavirus (HPV) is a highly prevalent DNA oncogenic virus that is primarily transmitted through sexual contact. It is the most common sexually transmitted infection and can infect various mucosal and cutaneous membranes, including the anogenital region, upper aerodigestive tract, and other areas of the head and neck. While most HPV infections are asymptomatic and resolve spontaneously within 24 months, persistent infections with high-risk HPV types can lead to the development of cervical lesions and cancer. In fact, HPV is responsible for approximately 5% of all human cancers, including cervical cancer, which is the third most common cancer in women. The virus has also been linked to other malignancies such as oral and respiratory squamous cell carcinomas, and anogenital cancers. Due to its significant impact on public health, prevention strategies like vaccination and cervical screening have been developed to combat HPV-related diseases.
Differentiation between high-risk and low-risk Human papillomavirus types
Human papillomaviruses (HPVs) are categorized into high-risk (hrHPV) and low-risk (lrHPV) types based on their association with cancer and other diseases. High-risk HPVs, such as HPV16 and HPV18, are implicated in nearly 5% of all human cancers, including almost all cases of cervical cancer and a significant proportion of other anogenital and head and neck cancers. These types are characterized by their ability to cause persistent infections and deregulate viral gene expression, leading to excessive cell proliferation and genetic damage. In contrast, low-risk HPVs, such as HPV6 and HPV11, typically cause benign lesions like genital warts and recurrent respiratory papillomatosis, which rarely progress to cancer. Despite these differences, both high- and low-risk HPVs share similar molecular strategies for genome maintenance and persistence, although they differ in their regulatory controls and the extent to which they drive cell cycle entry and proliferation. The differentiation between these two groups is crucial for clinical diagnostics and treatment, as high-risk HPVs require more aggressive management due to their oncogenic potential.
How is Human papillomavirus Transmitted?
Human papillomavirus (HPV) is primarily transmitted through sexual contact, including vaginal, anal, and oral sex, as well as through skin-to-skin contact involving the genital areas. However, HPV can also be transmitted through non-penetrative sexual activities and other non-sexual routes. For instance, HPV DNA has been detected in the genital tract of female virgins, suggesting that non-penetrative sexual activities or contact with contaminated surfaces can lead to transmission. Additionally, vertical transmission from mother to child during childbirth has been documented, although it is considered less clinically significant. There is also evidence of HPV transmission through fomites in medical settings and public environments, highlighting the need for stringent hygiene practices. Common misconceptions about HPV transmission include the belief that it can only be spread through penetrative sex or that it cannot be contracted from surfaces or through non-sexual means. These misconceptions can lead to inadequate preventive measures and a lack of awareness about the various transmission routes of HPV.
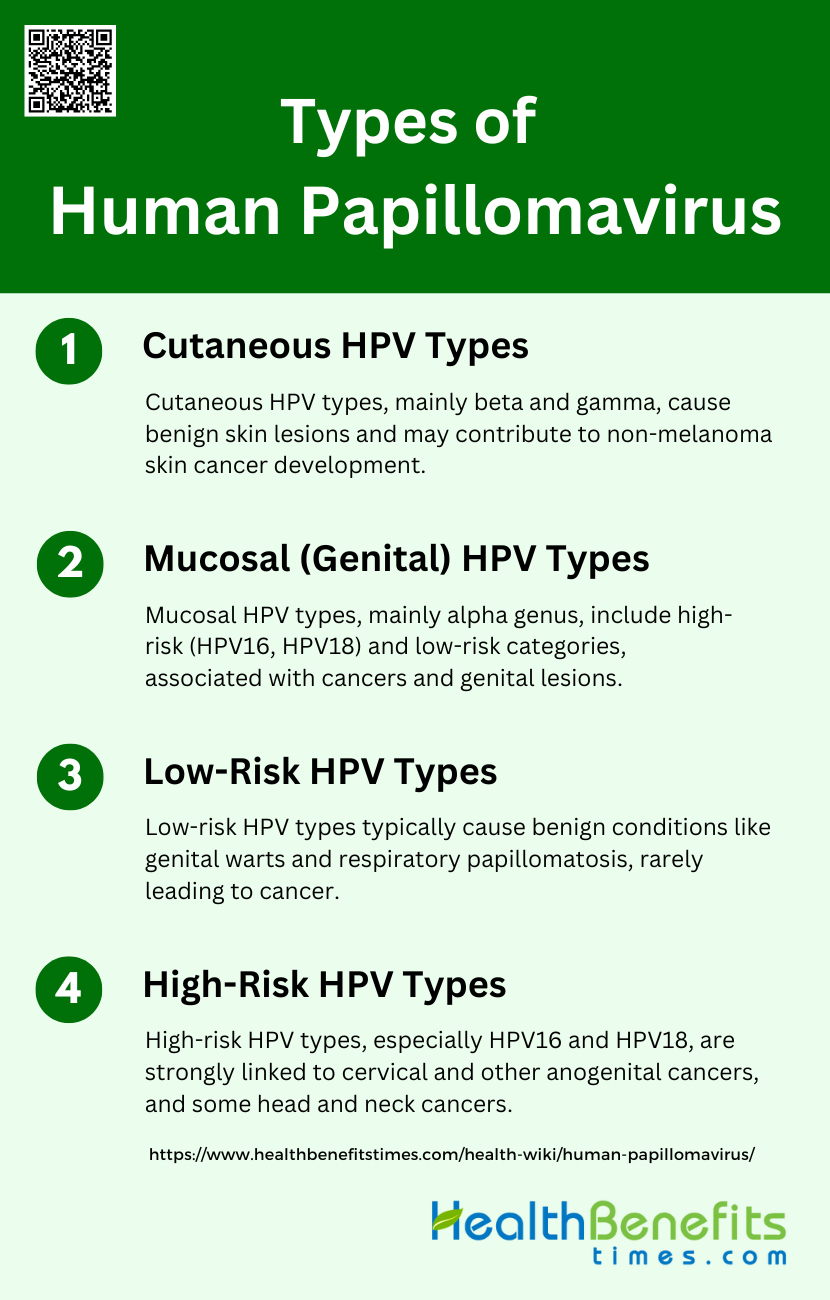
Types of Human papillomavirus
Human papillomavirus (HPV) is a diverse group of DNA viruses that infect the skin and mucous membranes of humans. There are over 200 different types of HPV, which are categorized based on their preferred tissue type and associated health risks. Below are the main types of HPV:
1. Cutaneous HPV Types
Cutaneous HPV types primarily belong to the beta and gamma genera and are commonly found on the skin’s surface in the general population. These types are generally associated with benign skin lesions, such as common warts. However, there is growing evidence that beta HPV types may play a role in the development of non-melanoma skin cancer (NMSC). These viruses can exacerbate the accumulation of UV radiation-induced DNA damage, acting as facilitators in the carcinogenesis process rather than direct causes. The expression of viral proteins E6 and E7 in cutaneous HPV types is not required for maintaining the skin cancer phenotype, unlike their role in mucosal HPV types.
2. Mucosal (Genital) HPV Types
Mucosal HPV types, particularly those from the alpha genus, infect the epithelial lining of the anogenital tract and other mucosal areas. These types are further classified into high-risk (HR) and low-risk (LR) categories based on their oncogenic potential. HR mucosal HPV types, such as HPV16 and HPV18, are strongly associated with cervical cancer and other anogenital cancers, as well as a subset of head and neck cancers. The viral oncoproteins E6 and E7 play crucial roles in cellular transformation by interfering with key regulatory proteins like p53 and retinoblastoma protein (pRB), leading to persistent infections and cancer development.
3. Low-Risk HPV Types
Low-risk HPV types are generally associated with benign epithelial lesions, such as genital warts and recurrent respiratory papillomatosis. These types rarely lead to cancer but can cause significant morbidity. For instance, HPV11, a low-risk type, can cause persistent laryngeal papillomas that require regular surgical intervention. Although these infections are typically resolved by the host immune system, they can persist and cause complications in immunosuppressed individuals. The molecular mechanisms of low-risk HPV types involve pathways that ensure persistent infection and virus shedding without leading to malignant transformation.
4. High-Risk HPV Types
High-risk HPV types are a subset of the alpha genus and are primarily responsible for several human cancers, including almost all cases of cervical cancer. HPV16 and HPV18 are the most studied high-risk types due to their significant role in carcinogenesis. These types are also linked to other anogenital cancers and a growing number of head and neck cancers. The E6 and E7 oncoproteins of high-risk HPVs disrupt critical cellular processes, such as cell cycle control and apoptosis, by targeting proteins like p53 and pRB. This disruption leads to uncontrolled cell proliferation and the accumulation of genetic damage, which are key steps in cancer development.
Common Symptoms of Human papillomavirus
Human papillomavirus (HPV) is a widespread virus with various strains that can cause different types of warts and lesions. While some infections are asymptomatic, others manifest in noticeable symptoms affecting different parts of the body. Below are some common symptoms of HPV:
1. Genital Warts
Genital warts are one of the most common symptoms of Human Papillomavirus (HPV) infection, particularly caused by low-risk HPV types. These warts appear as small bumps or groups of bumps in the genital area and can vary in size and shape. They are typically flesh-colored and can be flat or raised. Genital warts are not only a physical concern but also a significant source of psychosocial distress, leading to anxiety and depression in affected individuals. The treatment of genital warts often involves topical medications, cryotherapy, or surgical removal, but recurrence is common, which can further exacerbate the emotional burden on patients.
2. Common Warts
Common warts are benign skin growths caused by HPV, typically appearing on the hands and fingers. These warts are usually rough, raised, and can be painful or cause discomfort, especially if located in areas subject to frequent friction or pressure. They are caused by non-oncogenic HPV types and are generally harmless, although they can be a source of embarrassment and social stigma. Treatment options include over-the-counter salicylic acid preparations, cryotherapy, and laser treatments, but warts can be persistent and may require multiple treatment sessions to fully resolve.
3. Plantar Warts
Plantar warts are a type of common wart that occurs on the soles of the feet. They are caused by HPV and can be particularly painful due to their location, making walking or standing uncomfortable. These warts often appear as thickened, callus-like areas with small black dots on the surface, which are actually tiny blood vessels. Plantar warts can be challenging to treat because they grow inward due to the pressure from walking. Treatment options include salicylic acid, cryotherapy, and more aggressive methods like surgical removal or laser therapy.
4. Flat Warts
Flat warts are small, smooth, and slightly raised lesions that can appear anywhere on the body but are most commonly found on the face, neck, hands, and wrists. They are caused by HPV and are more common in children and young adults. Flat warts are usually flesh-colored or slightly darker and can occur in large numbers, often spreading through shaving or scratching. While they are generally harmless, their appearance can be distressing, especially when they occur on visible areas of the skin. Treatment options include topical retinoids, cryotherapy, and laser treatments.
5. Oral and Respiratory Lesions
HPV can also cause lesions in the oral and respiratory tracts, leading to conditions such as oral warts and recurrent respiratory papillomatosis (RRP). Oral warts can appear on the lips, inside the mouth, and on the tongue, while RRP involves the growth of warts in the respiratory tract, potentially causing breathing difficulties and voice changes. These lesions are typically caused by low-risk HPV types, but high-risk types can also be involved, particularly in cases of oropharyngeal cancers. Treatment often involves surgical removal of the lesions, but recurrence is common, necessitating ongoing medical management.
6. Asymptomatic Infections
A significant number of HPV infections are asymptomatic, meaning they do not cause any noticeable symptoms. These infections are often transient and are cleared by the immune system without causing any clinical manifestations. Asymptomatic infections are particularly common with low-risk HPV types, but even high-risk types can remain undetected for years. Despite the lack of symptoms, asymptomatic individuals can still transmit the virus to others, contributing to the widespread prevalence of HPV. Regular screening and vaccination are crucial in managing the spread of HPV and preventing the development of related cancers.
Who is at Risk of Contracting Human papillomavirus?
Human papillomavirus (HPV) is a highly prevalent sexually transmitted infection that affects both men and women. Factors that increase the risk of contracting HPV include sexual promiscuity, early initiation of sexual intercourse, lack of condom use, and smoking. Additionally, being uncircumcised and having a high number of lifetime sexual partners are significant risk factors for men. Women are also at risk, particularly those with a history of sexually transmitted infections, early age at first full-term pregnancy, and long-term use of oral contraceptives. Both genders are susceptible to HPV, and the infection can lead to various cancers, including cervical cancer in women and anogenital cancers in men. Therefore, it is crucial for both men and women to engage in protective sexual behaviors and consider vaccination to reduce the risk of HPV infection.
Diagnosis and Testing for Human papillomavirus
When to Get Tested
Testing for human papillomavirus (HPV) is crucial for the early detection and prevention of cervical cancer. Women aged 30 years and older are recommended to undergo primary screening for high-risk HPV (hrHPV) as it has been shown to detect more cases of cervical intraepithelial neoplasia (CIN) and cervical cancer compared to cytology alone. Additionally, HPV testing is advised for women with equivocal or low-grade cytologic abnormalities to better triage and manage their condition. For oropharyngeal squamous cell carcinoma, high-risk HPV testing is recommended for all newly diagnosed patients to guide clinical management. Regular screening and follow-up are essential, especially for those who have undergone treatment for cervical pre-cancer, as HPV testing can more accurately detect residual or recurrent high-grade CIN.
Types of Tests Available
1. Pap Smear
The Pap smear, also known as cytology, is a traditional method used to screen for cervical cancer by detecting abnormal cells in the cervix. It involves collecting cells from the cervix and examining them under a microscope. While Pap smears have been effective in reducing cervical cancer incidence, they are less sensitive compared to HPV testing. Studies have shown that HPV testing detects more cases of CIN2, CIN3, or cancer than cytology at the cut-off for atypical squamous cells of undetermined significance (ASC-US) or low-grade squamous intraepithelial lesions (LSIL). However, combining HPV testing with cytology can provide a small gain in sensitivity, albeit with a loss in specificity.
2. HPV Test
HPV tests detect the presence of high-risk HPV DNA or RNA in cervical cells. These tests are more sensitive than Pap smears and can be used as a primary screening tool for cervical cancer. Several types of HPV tests are available, including the Hybrid Capture 2 (HC2) assay, APTIMA mRNA test, and various PCR-based tests like GP5+/6+ PCR and cobas 4800 PCR. HPV testing is also recommended for triaging women with abnormal cytology and for follow-up after treatment of CIN lesions. Self-collected samples for HPV testing have shown high concordance with clinician-collected samples, making them a reliable and accessible option for cervical cancer screening.
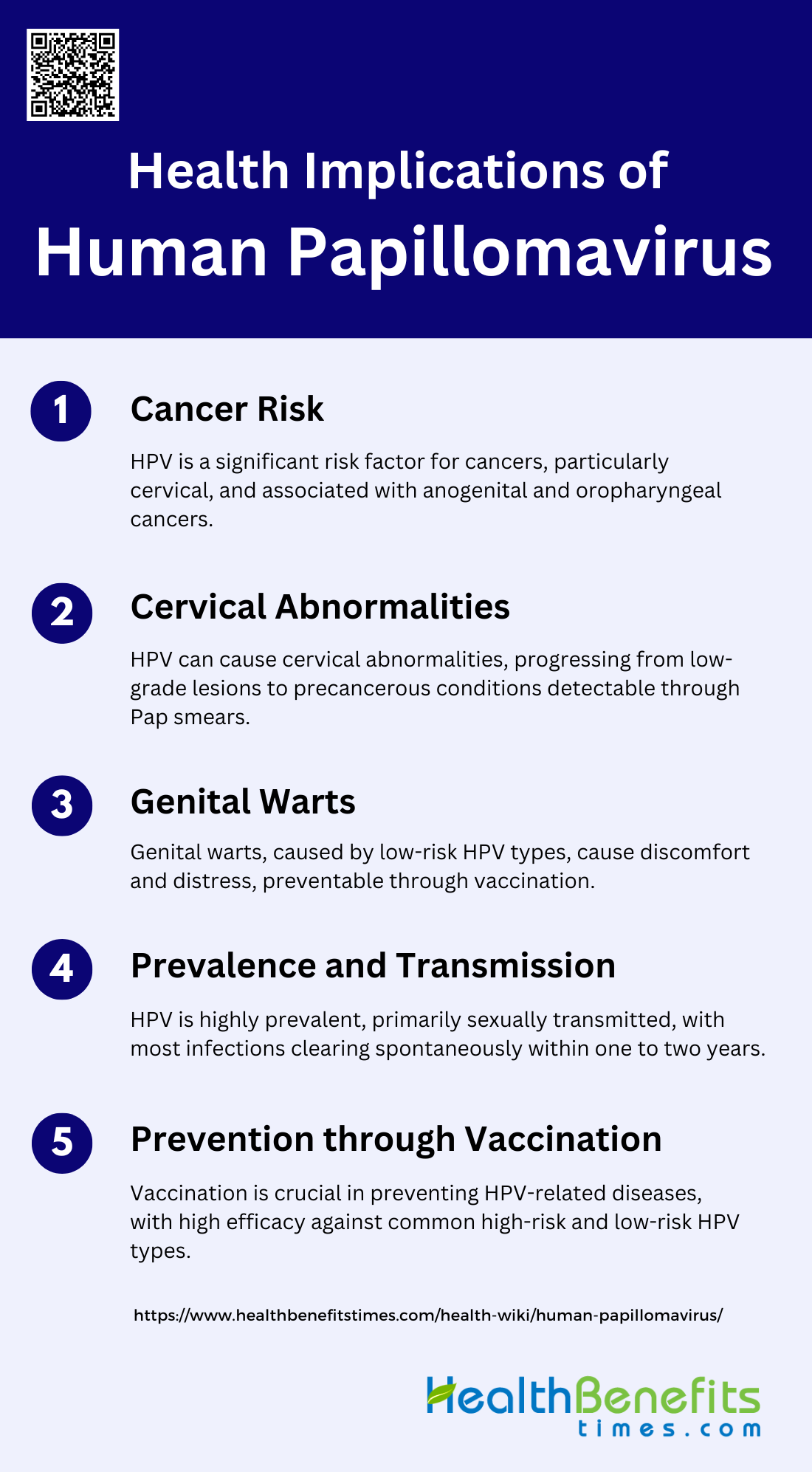
Health Implications of Human papillomavirus
Human papillomavirus (HPV) is a prevalent virus with significant health implications, ranging from benign warts to serious cancers. Understanding the various symptoms and potential outcomes of HPV infection is crucial for early detection and management. Below are some common Health Implications of Human papillomavirus:
1. Cancer Risk
Human papillomavirus (HPV) is a significant risk factor for various cancers, particularly cervical cancer, which is the fourth deadliest cancer in women globally. HPV is implicated in over 90% of cervical cancer cases and is also associated with cancers of the vagina, vulva, penis, anus, and oropharynx. Persistent infection with high-risk HPV types, such as HPV-16 and HPV-18, is a necessary cause of cervical cancer and contributes to other upper aerodigestive and anogenital tract cancers. The oncogenic potential of HPV is exacerbated in individuals with compromised immune systems, such as those co-infected with HIV.
2. Cervical Abnormalities
HPV infection can lead to various cervical abnormalities, ranging from low-grade lesions to high-grade precancerous lesions. High-risk HPV types are responsible for the development of cervical intraepithelial neoplasia (CIN), which can progress to cervical cancer if left untreated. Cytological screening, such as Pap smears, has been effective in detecting these abnormalities early, thereby preventing the progression to cancer. However, the management of HPV-associated cytologic abnormalities is costly and resource-intensive, highlighting the need for effective vaccination and screening programs.
3. Genital Warts
Genital warts, caused primarily by low-risk HPV types such as HPV-6 and HPV-11, represent a significant morbidity associated with HPV infection. These warts are highly contagious and can cause considerable discomfort and psychological distress. Although not oncogenic, genital warts contribute to the overall burden of HPV-related diseases. The quadrivalent HPV vaccine, which includes protection against HPV-6 and HPV-11, has been shown to be highly effective in preventing genital warts.
4. Prevalence and Transmission
HPV is the most common sexually transmitted infection worldwide, with more than 80% of sexually active individuals likely to acquire it at some point in their lives. The prevalence of HPV varies by region, with higher rates observed in developing countries. Transmission occurs primarily through sexual contact, and factors such as youth, multiple sexual partners, and immunosuppressive conditions increase the risk of acquiring and persisting HPV infections. Despite the high prevalence, most HPV infections are transient and asymptomatic, clearing spontaneously within one to two years.
5. Prevention through Vaccination
Vaccination is the most effective strategy for preventing HPV-related diseases. The available vaccines, including the 9-valent HPV vaccine, protect against the most common high-risk and low-risk HPV types. These vaccines have demonstrated high efficacy in preventing cervical cancer, genital warts, and other HPV-related diseases. However, challenges such as vaccine cost, cold chain requirements, and low vaccination coverage, particularly in developing countries, limit the global impact of these vaccines. Universal vaccination programs, including gender-neutral approaches, are essential to reduce the overall burden of HPV-related diseases.
Treatment Options for Human papillomavirus -Related Conditions
Human papillomavirus (HPV) infections can lead to various conditions, including warts, pre-cancerous lesions, and cancers. Treatment options for HPV-related warts include patient-applied therapies such as podofilox and salicylic acid, which are cost-effective and convenient. For more persistent warts, cryotherapy, imiquimod, and surgical options like electrosurgery and laser surgery are available. Pre-cancerous lesions, such as high-grade vulvar intraepithelial neoplasia (VIN), can be treated with topical agents like imiquimod and fluorouracil, although these treatments can cause significant morbidity. For HPV-related cancers, surgical excision is often successful, but chemoradiation therapy is also used, particularly for cervical cancer, which has a 5-year survival rate of 66-79%. Emerging treatments include immunotherapies and vaccines targeting HPV-specific pathways. Monitoring and follow-up care are crucial, as recurrence rates for warts can be as high as 30-40% after treatment. Regular follow-ups help in early detection of recurrences and management of any complications arising from the treatments.
Prevention Strategies for Human papillomavirus
Human papillomavirus (HPV) is a common virus with potentially serious health consequences, but there are effective strategies to prevent its transmission and impact. Implementing these measures can significantly reduce the risk of HPV-related diseases. Below are some key prevention strategies for HPV:
1. HPV Vaccine
The HPV vaccine is a critical tool in preventing HPV-related diseases, including cervical cancer and genital warts. Two primary vaccines, Gardasil and Cervarix, target the most common HPV types associated with cervical cancer, HPV-16 and HPV-18. Clinical trials have demonstrated that these vaccines are safe, immunogenic, and highly effective in preventing type-specific HPV infections. The quadrivalent vaccine, Gardasil, also targets HPV-6 and HPV-11, which are responsible for genital warts, and has shown significant efficacy in reducing the incidence of high-grade cervical lesions and other anogenital diseases. Routine vaccination is recommended for preteens, with catch-up vaccinations for young adults who missed the initial series.
2. Safe Sexual Practices
Safe sexual practices are essential in reducing the transmission of HPV. Health education measures that promote the use of condoms, reduce the number of sexual partners, and encourage safer sex strategies have been shown to decrease the risk of HPV infection. Condom use, in particular, has been identified as the most effective intervention among these strategies. Public health campaigns and educational programs aimed at promoting these practices can significantly contribute to lowering the incidence of HPV and related diseases. Additionally, regular communication and education about safe sexual behaviors are crucial in preventing the spread of HPV among sexually active individuals.
3. Healthy Lifestyle
Maintaining a healthy lifestyle can play a supportive role in preventing HPV infections and their progression to cancer. A robust immune system is essential for controlling and clearing HPV infections, and factors such as a balanced diet, regular exercise, and avoiding smoking can enhance immune function. Immunocompromised individuals, including those with rheumatic diseases, are at higher risk for persistent HPV infections and subsequent cervical cancer. Therefore, adopting a healthy lifestyle can help bolster the immune system’s ability to fight off infections, including HPV, and reduce the likelihood of persistent infections that can lead to malignancies.
4. Circumcision
Circumcision has been associated with a reduced risk of HPV transmission and infection. Studies have shown that circumcised men are less likely to acquire and transmit HPV to their sexual partners. This reduction in HPV prevalence among circumcised men can subsequently lower the risk of cervical cancer in their female partners. While circumcision alone is not a comprehensive prevention strategy, it can be a valuable component of a multifaceted approach to reducing HPV transmission, particularly in regions with high rates of HPV-related diseases.
5. Cervical Cancer Screening
Cervical cancer screening is a vital component of HPV prevention strategies. Regular Pap tests and HPV testing can detect precancerous lesions and early-stage cervical cancer, allowing for timely intervention and treatment. Screening programs have significantly reduced cervical cancer rates in countries where they are routinely implemented. For women with rheumatic diseases or other immunosuppressive conditions, more frequent screening may be necessary due to their increased risk of persistent HPV infections and cervical cancer. Adhering to recommended screening guidelines is crucial for early detection and prevention of cervical cancer.
6. Screening for High-Risk Groups
High-risk groups, such as individuals with immunosuppressive conditions, men who have sex with men (MSM), and people living with HIV/AIDS, require targeted screening and prevention efforts. These populations are at higher risk for persistent HPV infections and related cancers. Annual digital anorectal examinations and more frequent cervical cancer screenings are recommended for these groups to detect and manage HPV-related diseases early. Tailored screening protocols and preventive measures can help mitigate the elevated risks faced by these high-risk populations.
7. Public Awareness
Raising public awareness about HPV and its associated risks is crucial for effective prevention. Public health campaigns that educate people about the modes of HPV transmission, the importance of vaccination, and safe sexual practices can significantly reduce the incidence of HPV infections. Awareness initiatives should also emphasize the availability and benefits of cervical cancer screening and the importance of early detection. By increasing public knowledge and understanding of HPV, these campaigns can encourage proactive health behaviors and reduce the burden of HPV-related diseases.
8. Education on Safe Practices
Education on safe practices is a cornerstone of HPV prevention. Comprehensive sexual education programs that cover the use of condoms, the importance of limiting the number of sexual partners, and the benefits of HPV vaccination can empower individuals to make informed decisions about their sexual health. Schools, healthcare providers, and community organizations play a vital role in disseminating this information. By providing accurate and accessible education on safe practices, these programs can help prevent HPV transmission and protect public health.
Myths and Misconceptions about HPV
Human papillomavirus (HPV) is surrounded by numerous myths and misconceptions that can lead to misinformation and stigma. Dispelling these myths is essential for better understanding and managing HPV. Below are some common myths and misconceptions about HPV:
1. Only Women Can Get HPV
A common misconception is that only women can contract Human Papillomavirus (HPV). However, HPV is a sexually transmitted infection that affects both men and women. Men can acquire HPV through sexual contact and are at risk for HPV-related conditions such as genital warts and cancers of the oropharynx, anus, and penis. The prevalence of HPV in men is significant, and they can also act as carriers, transmitting the virus to their sexual partners. Therefore, it is crucial to recognize that HPV is not gender-specific and affects individuals regardless of their sex.
2. HPV Always Causes Symptoms
Another myth is that HPV always causes symptoms. In reality, most HPV infections are asymptomatic and go unnoticed. Many individuals with HPV do not develop any signs or symptoms, and the infection often clears on its own without causing any health problems. However, certain high-risk strains of HPV can persist and lead to serious conditions such as cervical cancer in women and other cancers in both men and women. Regular screening and vaccination are essential preventive measures to manage the risks associated with HPV.
3. HPV Infection Means You Will Get Cancer
While HPV infection is a risk factor for certain types of cancer, it does not mean that everyone with HPV will develop cancer. Most HPV infections are transient and are cleared by the immune system. Persistent infection with high-risk HPV types can lead to cellular changes and, over time, may progress to cancer if not detected and treated early. Regular screening, such as Pap smears and HPV tests, can help detect precancerous changes, allowing for early intervention and reducing the risk of cancer development.
4. Only Promiscuous People Get HPV
The belief that only promiscuous individuals get HPV is a harmful misconception. HPV is highly prevalent and can be transmitted through any sexual activity involving skin-to-skin contact, not just through intercourse. It is one of the most common sexually transmitted infections, and most sexually active people will contract HPV at some point in their lives. The virus does not discriminate based on the number of sexual partners, and even individuals with a single lifetime partner can acquire HPV. Public health efforts emphasize the importance of vaccination and regular screening for everyone, regardless of their sexual history.
5. HPV Can Be Cured with Antibiotics
A widespread myth is that HPV can be cured with antibiotics. HPV is a viral infection, and antibiotics are ineffective against viruses. There is currently no cure for HPV, but the body’s immune system often clears the infection naturally. Preventive measures such as vaccination can protect against the most harmful strains of HPV. For those with persistent infections, regular monitoring and treatment of any precancerous lesions are crucial to prevent the progression to cancer. Public health education is essential to dispel this myth and promote appropriate preventive and management strategies.
FAQs
1. Can HPV be prevented if a person is already sexually active?
Yes, even if a person is already sexually active, HPV vaccination can still provide protection against strains they haven’t been exposed to. Additionally, practicing safe sex, such as using condoms, can help reduce the risk of transmission, although it does not provide complete protection against HPV.
2. Are there any non-sexual ways to prevent HPV transmission?
Yes, maintaining good personal hygiene and avoiding the sharing of personal items like towels or razors can help reduce the risk of HPV transmission. Additionally, awareness of proper sterilization practices in medical and cosmetic settings (like nail salons) is important.
3. How does HPV affect men, and what cancers are they at risk for?
HPV can affect men and lead to conditions like genital warts. It can also cause cancers such as penile, anal, and oropharyngeal cancers (cancers of the throat and mouth). Vaccination and safe sexual practices are important preventive measures for men as well.
4. Is there an age limit for receiving the HPV vaccine?
While the HPV vaccine is most effective when given before exposure to the virus (typically in preteens), it is recommended for people up to the age of 26. Some adults aged 27 through 45 who have not been vaccinated may also choose to get the vaccine after consulting with their healthcare provider.
5. Can HPV be transmitted through casual contact like hugging or sharing utensils?
No, HPV is not spread through casual contact such as hugging, shaking hands, or sharing utensils. The virus is primarily transmitted through direct skin-to-skin contact during sexual activity.
6. Can someone who has received the HPV vaccine still contract HPV?
While the HPV vaccine is highly effective against the most common and high-risk types of HPV, it does not protect against all types. Therefore, it is still possible, although less likely, to contract a strain of HPV not covered by the vaccine.
7. What is the role of the immune system in clearing HPV infections?
The immune system plays a crucial role in clearing HPV infections. Most HPV infections are transient and are cleared by the body’s immune response within 1 to 2 years without causing any symptoms or health problems.
8. How can I know if I have HPV if there are no symptoms?
Most HPV infections do not cause noticeable symptoms. Regular screening, such as Pap smears and HPV testing, is the only way to detect HPV-related cellular changes or infections in asymptomatic individuals.
9. What should I do if I test positive for HPV?
If you test positive for HPV, your healthcare provider may recommend further testing or monitoring depending on the specific type of HPV and your health history. It’s important to follow their guidance on next steps, which may include repeat testing, colposcopy, or treatment of any abnormal cervical cells.
10. Can HPV affect fertility or pregnancy?
HPV does not directly affect fertility, but certain treatments for HPV-related conditions, such as surgical procedures on the cervix, may impact cervical competency, potentially affecting pregnancy. Pregnant women with HPV should consult their healthcare provider for appropriate management.