Herpes Simplex Virus (HSV) is a common and highly contagious viral infection that affects a significant portion of the global population. There are two main types of HSV: HSV-1, which primarily causes oral herpes, and HSV-2, which is typically associated with genital herpes. These viruses are characterized by their ability to establish lifelong latent infections in the host’s nervous system, leading to recurrent outbreaks triggered by various factors such as stress, illness, or environmental conditions. HSV infections manifest as painful lesions or sores on the skin and mucous membranes, most commonly around the mouth, lips, or genitals. While HSV infections are generally not life-threatening, they can cause significant discomfort and psychological distress, and in rare cases, may lead to more serious complications, particularly in immunocompromised individuals or newborns.
Types of Herpes Simplex Virus
Herpes Simplex Virus (HSV) is a common viral infection that manifests in two primary forms, each with distinct characteristics and implications. Understanding the types of HSV is crucial for diagnosis, treatment, and prevention. Below is a detailed overview of the different types of Herpes Simplex Virus:
1. HSV-1
Herpes Simplex Virus Type 1 (HSV-1) is primarily associated with oral herpes, which often manifests as cold sores or fever blisters around the mouth. HSV-1 is a lifelong infection typically acquired during childhood through non-sexual contact, such as kissing or sharing utensils. The virus establishes latency in the neurons and can reactivate, causing recurrent sores. HSV-1 is highly prevalent globally, with seroprevalence rates varying by region. For instance, in Australia, the seroprevalence among healthy adults is approximately 84.8%. In Europe, the seroprevalence is around 67.4%, with higher rates in older adults. Despite its high prevalence, many individuals remain asymptomatic, contributing to the virus’s widespread transmission.
2. HSV-2
Herpes Simplex Virus Type 2 (HSV-2) is primarily responsible for genital herpes, characterized by painful sores in the genital and anal areas. HSV-2 is a sexually transmitted infection with a significant global burden. In 2016, an estimated 491.5 million people aged 15-49 were living with HSV-2, representing 13.2% of the global population in this age group. The prevalence of HSV-2 is notably higher in sub-Saharan Africa, where seroprevalence rates can reach up to 71.3% among HIV-positive individuals. Unlike HSV-1, HSV-2 is less commonly acquired during childhood and is more prevalent among sexually active adults. The virus can also increase the risk of acquiring HIV, particularly in regions with high HSV-2 prevalence.
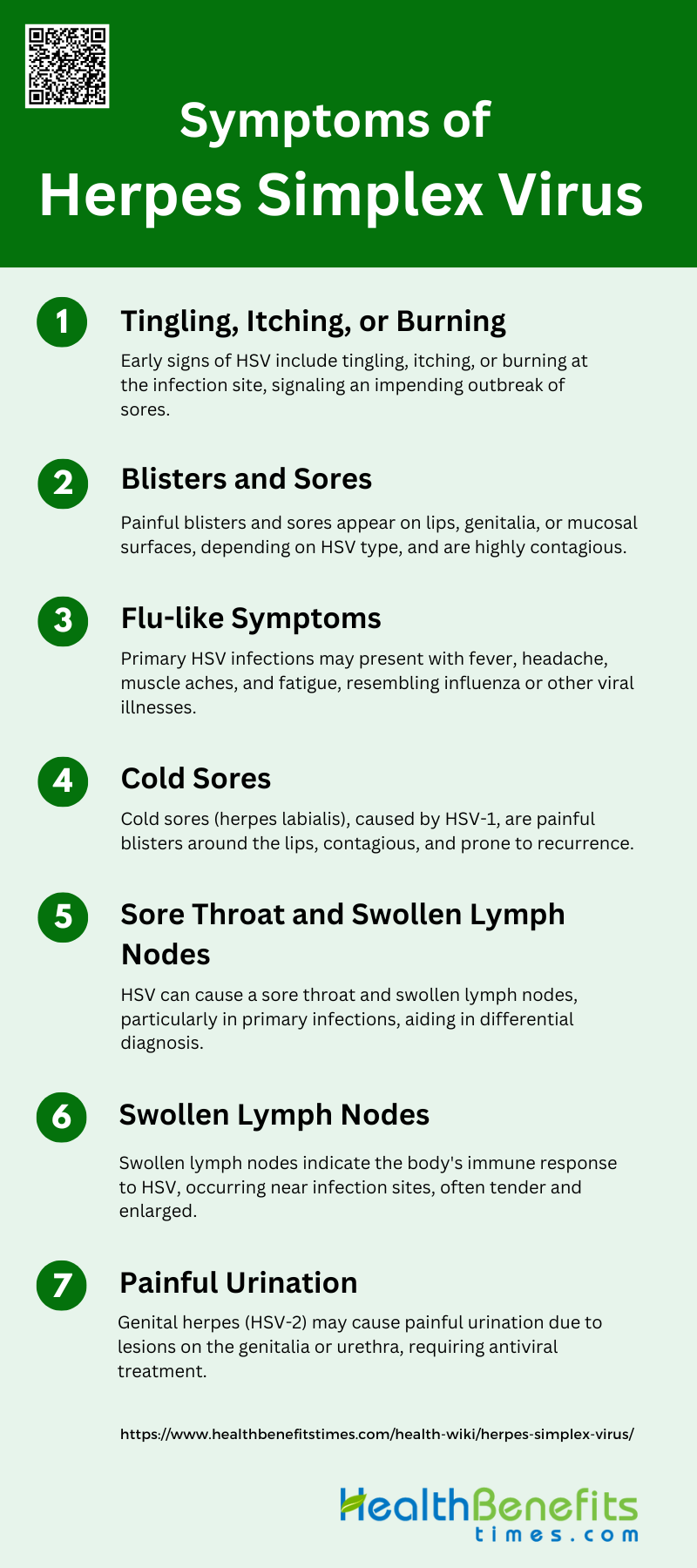
Symptoms of Herpes Simplex Virus
Herpes Simplex Virus (HSV) can cause a range of symptoms that vary depending on the type and location of the infection. Recognizing these symptoms is essential for timely diagnosis and management. Below is a list of common symptoms associated with HSV:
1. Tingling, Itching, or Burning
The initial symptoms of a herpes simplex virus (HSV) infection often include tingling, itching, or burning sensations at the site of infection. These prodromal symptoms typically precede the appearance of visible lesions and can serve as an early warning sign of an impending outbreak. The tingling or itching is caused by the virus traveling along the nerve pathways to the skin’s surface, where it will eventually form blisters or sores. Recognizing these early symptoms can be crucial for timely intervention and treatment, potentially reducing the severity and duration of the outbreak.
2. Blisters and Sores
Blisters and sores are hallmark symptoms of herpes simplex virus infections. These painful lesions can appear on the lips, genitalia, or other mucosal surfaces, depending on whether the infection is caused by HSV-1 or HSV-2. The blisters typically form clusters and eventually rupture, leaving behind open sores that can take several days to heal. These lesions are not only painful but also highly contagious, as the virus is present in the fluid within the blisters. Effective management often involves antiviral medications to reduce the duration and severity of the outbreak.
3. Flu-like Symptoms
During the initial outbreak of herpes simplex virus, individuals may experience flu-like symptoms such as fever, headache, muscle aches, and fatigue. These systemic symptoms are more common in primary infections and can be quite severe, sometimes leading to misdiagnosis as influenza or another viral illness. The body’s immune response to the virus is responsible for these symptoms, as it attempts to fight off the infection. Recognizing these flu-like symptoms in conjunction with localized lesions can aid in the accurate diagnosis of HSV.
4. Cold Sores
Cold sores, also known as herpes labialis, are a common manifestation of HSV-1 infection. These painful, fluid-filled blisters typically appear on or around the lips and can cause significant discomfort. Cold sores are highly contagious and can be transmitted through direct contact with the lesions or through saliva. The sores usually heal within two to four weeks, but the virus remains dormant in the body and can reactivate, leading to recurrent outbreaks. Topical treatments and antiviral medications can help manage the symptoms and reduce the frequency of recurrences.
5. Sore Throat and Swollen Lymph Nodes
In some cases, herpes simplex virus infections can cause a sore throat and swollen lymph nodes, particularly during the initial outbreak. These symptoms are more common in primary infections and can be accompanied by other systemic symptoms such as fever and malaise. The sore throat is often due to the presence of lesions in the oral cavity or pharynx, while the swollen lymph nodes are a result of the body’s immune response to the infection. These symptoms can help differentiate HSV from other viral infections and guide appropriate treatment.
6. Swollen Lymph Nodes
Swollen lymph nodes are a common symptom of herpes simplex virus infections, particularly during the initial outbreak. The lymph nodes, which are part of the body’s immune system, become enlarged as they work to filter out the virus and other pathogens. This swelling is often accompanied by tenderness and can occur in the neck, groin, or other areas near the site of infection. Swollen lymph nodes are an indication that the body is actively fighting the infection and can be a useful diagnostic sign in conjunction with other symptoms.
7. Painful Urination
Painful urination, or dysuria, can occur in individuals with genital herpes caused by HSV-2. This symptom is due to the presence of lesions on the genitalia or urethra, which can cause significant discomfort during urination. The pain is often described as a burning or stinging sensation and can be severe enough to cause individuals to avoid urinating, leading to further complications. Antiviral medications and pain management strategies can help alleviate this symptom and promote healing of the lesions.
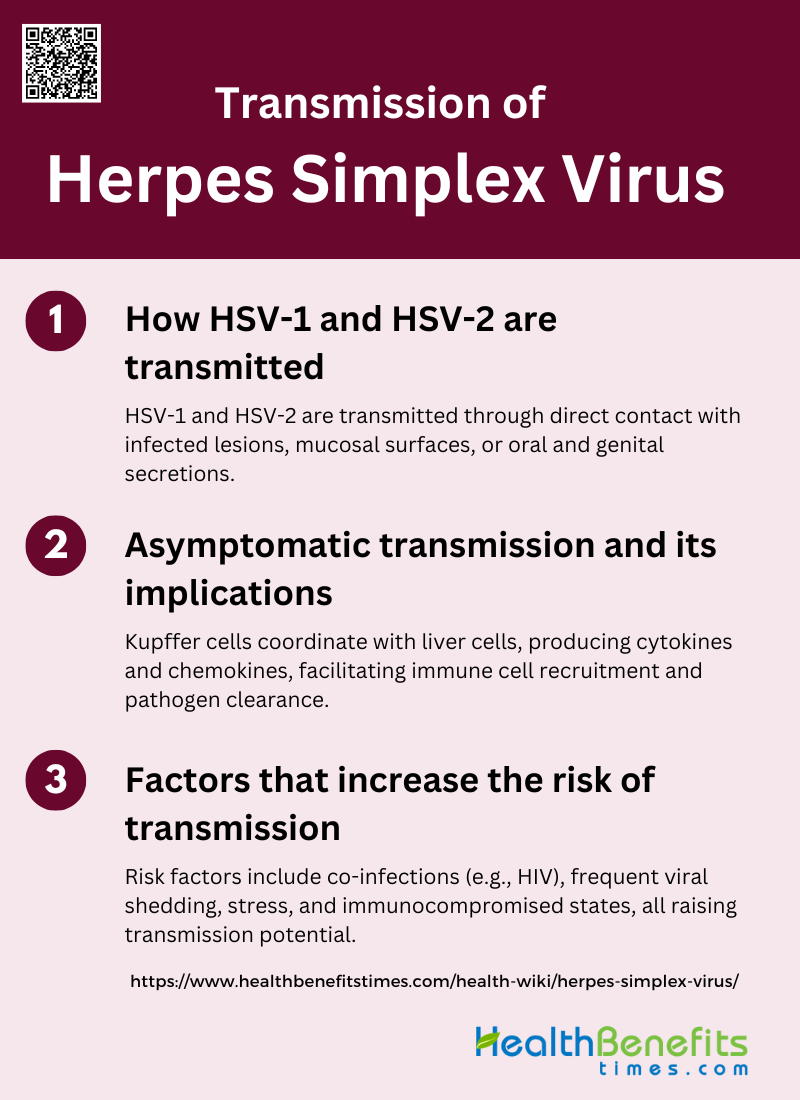
Transmission of Herpes Simplex Virus
Herpes Simplex Virus (HSV) is highly contagious and can be transmitted through various forms of contact. Understanding the modes of transmission is vital for preventing the spread of the virus. Below are the primary ways HSV can be transmitted:
1. How HSV-1 and HSV-2 are transmitted
Herpes simplex virus types 1 and 2 (HSV-1 and HSV-2) are transmitted through direct contact with an infected person’s lesion, mucosal surface, or genital or oral secretions. HSV-1 is commonly associated with oral infections, while HSV-2 is typically linked to genital infections. Both types of the virus can cause lifelong infections, often without symptoms, but can also lead to painful blisters or sores at the site of infection. The viruses establish latency in sensory neurons and can reactivate, leading to recurrent episodes of viral shedding and potential transmission.
2. Asymptomatic transmission and its implications
Asymptomatic shedding of HSV-1 and HSV-2 plays a significant role in the transmission of these viruses. Despite the higher viral titers and longer shedding duration associated with symptomatic lesions, most transmissions occur during asymptomatic periods. This phenomenon was highlighted by studies showing that recent sex partners of individuals with first-episode genital herpes often contracted the virus despite the absence of visible symptoms in the transmitting partner. Asymptomatic shedding complicates prevention efforts, as individuals may unknowingly transmit the virus, underscoring the need for effective public health strategies and education to mitigate the spread.
3. Factors that increase the risk of transmission
Several factors can increase the risk of HSV transmission. Coinfection with other sexually transmitted infections, such as HIV-1, significantly elevates the risk. HSV-2, in particular, has been shown to increase the susceptibility to HIV-1 acquisition by 2- to 4-fold, and HSV-2 seropositive individuals have a higher rate of HIV-1 transmission per sexual contact. Additionally, the frequency of viral shedding, both symptomatic and asymptomatic, contributes to the risk of transmission. Stress and immunocompromised states can trigger reactivation of the virus, leading to increased shedding and higher transmission potential. Understanding these risk factors is crucial for developing targeted interventions to reduce HSV spread.
Diagnosis of Herpes Simplex Virus
Methods for Diagnosing HSV
Diagnosing Herpes Simplex Virus (HSV) involves both clinical examination and laboratory tests. Clinically, HSV can present with characteristic lesions, but these are often nonspecific and can be mistaken for other conditions. Laboratory tests are therefore crucial for accurate diagnosis. Polymerase Chain Reaction (PCR) is the gold standard for detecting HSV DNA, especially in central nervous system infections, due to its high sensitivity and specificity. Viral culture, although previously common, is being replaced by PCR for genital infections. Serological tests, which detect antibodies to HSV glycoproteins, are useful when no active lesions are present and can distinguish between HSV-1 and HSV-2. Point-of-care tests, such as microfluidics-based assays, offer rapid results and are useful in clinical settings.
Importance of Early Diagnosis for Treatment and Management
Early diagnosis of HSV is critical for effective treatment and management. Prompt identification allows for timely antiviral therapy, which can reduce the severity and duration of symptoms, prevent complications, and decrease the risk of transmission. In cases of neonatal herpes or encephalitis, early diagnosis is particularly vital as these conditions can be severe and life-threatening. Accurate and early detection also aids in appropriate counseling and management of patients, helping to mitigate the psychological distress associated with HSV infections. Furthermore, early diagnosis can inform preventive measures, such as prenatal screening to prevent vertical transmission from mother to child.
Treatment and Management of Herpes Simplex Virus
Overview of Antiviral Medications and Their Role
Antiviral medications play a crucial role in the treatment and management of Herpes Simplex Virus (HSV) infections. The primary drugs used include acyclovir, valacyclovir, and famciclovir, which are nucleoside analogs that inhibit viral DNA replication. These medications are effective in reducing the severity and frequency of outbreaks, particularly in immunocompromised patients. Acyclovir has been shown to be particularly effective in preventing oral HSV infections in cancer patients undergoing treatment. Despite their efficacy, these drugs do not cure HSV but help manage symptoms and reduce transmission risk. Continuous research is being conducted to develop new antiviral agents and improve existing therapies to combat drug resistance and enhance treatment outcomes.
Tips for Managing Symptoms and Preventing Outbreaks
Managing symptoms and preventing outbreaks of HSV involves a combination of antiviral therapy and lifestyle adjustments. Antiviral medications like acyclovir, valacyclovir, and famciclovir can significantly reduce the frequency of outbreaks and the severity of symptoms. For pregnant women, antiviral prophylaxis in the third trimester can reduce the risk of neonatal herpes and the need for cesarean delivery due to genital herpes. Additionally, maintaining good hygiene, avoiding known triggers such as stress and illness, and using barrier protection during sexual activity can help prevent outbreaks and transmission. Regular medical consultations and adherence to prescribed antiviral regimens are essential for effective management.
Lifestyle Adjustments to Help Manage the Condition
Lifestyle adjustments are vital in managing HSV and reducing the frequency of outbreaks. Stress management techniques such as yoga, meditation, and regular exercise can help lower the risk of outbreaks, as stress is a known trigger. A healthy diet rich in vitamins and minerals can boost the immune system, making it more effective at suppressing the virus. Avoiding excessive sun exposure and using sunscreen on affected areas can prevent reactivation of the virus, particularly for HSV-1. Additionally, maintaining good personal hygiene and avoiding sharing personal items like towels can reduce the risk of spreading the virus to others. Open communication with partners and using barrier protection during sexual activity are also crucial in managing the condition and preventing transmission.
Prevention Strategies of Herpes Simplex Virus
Herpes Simplex Virus (HSV) is a common viral infection that can cause sores on the mouth or genitals. Preventing the spread of HSV involves a combination of lifestyle changes, medical interventions, and awareness. Below are several effective strategies to reduce the risk of HSV transmission:
1. Safe Practices to Reduce Transmission
Safe practices to reduce the transmission of herpes simplex virus (HSV) are crucial in managing the spread of this prevalent sexually transmitted infection. The use of condoms has been shown to significantly lower the risk of HSV transmission by reducing direct skin-to-skin contact, which is the primary mode of transmission. Additionally, educating individuals about the importance of avoiding sexual contact during symptomatic outbreaks can further minimize the risk of spreading the virus. Public health strategies also emphasize the importance of regular screening and testing, especially among high-risk populations, to identify and manage infections early. These combined efforts are essential in reducing the overall transmission rates of HSV.
2. Use of Antiviral Therapies for Prevention
Antiviral therapies play a pivotal role in the prevention of HSV transmission. Medications such as valacyclovir and acyclovir have been shown to reduce the frequency of clinical recurrences and viral shedding, thereby lowering the risk of transmission to uninfected partners. For instance, daily suppressive therapy with valacyclovir has been demonstrated to reduce the risk of HSV-2 transmission by up to 48% and the risk of clinical disease in susceptible partners by 75%. Additionally, the use of antiviral microbicides like tenofovir gel has shown promise in reducing HSV-2 acquisition among women. These findings underscore the importance of antiviral therapies as a cornerstone in the prevention strategy for HSV.
3. Importance of Communication with Partners
Effective communication with sexual partners is essential in managing HSV and preventing its transmission. Disclosure of HSV status to partners allows for informed decision-making and the implementation of preventive measures such as condom use and antiviral therapy. Counseling and education about the nature of the infection, its transmission, and the importance of safe sexual practices can alleviate psychological distress and promote healthier relationships. Moreover, partner notification and mutual testing can help identify asymptomatic carriers and reduce the spread of the virus. Open and honest communication is thus a critical component in the comprehensive management of HSV.
Common Misunderstandings and Myths about Herpes Simplex Virus
Herpes Simplex Virus (HSV) is often surrounded by numerous misunderstandings and myths that can lead to unnecessary fear and stigma. It’s important to separate fact from fiction to better understand and manage this condition. Here are some common misconceptions about HSV:
1. Herpes is uncommon
Contrary to the belief that herpes is uncommon, it is actually a prevalent infection. Herpes simplex virus type 2 (HSV-2) alone has a significant presence, with a US prevalence of 11.9% among individuals aged 15 to 49 years. Additionally, a systematic review of HSV-2 epidemiology in the Middle East and North Africa (MENA) region found that 1 in 20 adults is chronically infected, despite conservative sexual norms. These statistics highlight that herpes is a common infection affecting a substantial portion of the global population.
2. Herpes is deadly
While herpes simplex virus (HSV) is a lifelong infection, it is not typically deadly. HSV-2, for instance, is a common pathogen that causes chronic illness but not fatal outcomes. The primary concerns with herpes are related to its management, prevention of transmission, and the social stigma associated with the infection. Although HSV can lead to complications in immunocompromised individuals or newborns, it is generally not considered a deadly virus for the majority of the population.
3. You can only spread herpes if you have symptoms
A common misconception is that herpes can only be spread when symptoms are present. However, asymptomatic shedding of the virus can occur, meaning individuals can transmit HSV even when they do not have visible sores or symptoms. This asymptomatic transmission contributes to the high prevalence of the virus, as many individuals are unaware they are infected and can unknowingly spread the virus to others. Therefore, it is crucial to understand that herpes can be transmitted even in the absence of symptoms.
4. Herpes is only a sexually transmitted infection
While herpes simplex virus is commonly associated with sexual transmission, it is not exclusively a sexually transmitted infection. HSV-1, for example, is often transmitted through non-sexual means such as oral contact, leading to oral herpes. Additionally, HSV can be transmitted from mother to child during childbirth, which is a non-sexual mode of transmission. Thus, herpes can spread through various routes, not limited to sexual contact.
5. Herpes can be diagnosed through a routine STI test
Another myth is that herpes can be diagnosed through a routine STI test. In reality, specific tests are required to diagnose herpes simplex virus infections. Standard STI panels do not typically include HSV testing unless specifically requested. Advanced diagnostic tools, such as serological tests and lateral-flow assays, are necessary to accurately detect HSV infections. Therefore, individuals seeking a herpes diagnosis should consult healthcare providers for appropriate testing beyond routine STI screenings.
FAQs
1. Can HSV be transmitted through objects, such as towels or utensils?
While HSV is primarily transmitted through direct contact with infected skin or mucous membranes, it is less likely to be spread through inanimate objects like towels, utensils, or bedding. The virus does not survive well outside the human body, making such transmission routes uncommon. However, sharing personal items during an active outbreak should still be avoided as a precaution.
2. Are there any over-the-counter treatments for managing HSV symptoms?
Over-the-counter treatments like topical creams (e.g., docosanol) can help alleviate some symptoms of HSV, particularly for cold sores caused by HSV-1. However, these treatments do not cure the virus or prevent transmission. For more severe or frequent outbreaks, prescription antiviral medications are typically more effective.
3. Can herpes simplex virus affect other parts of the body besides the mouth and genitals?
Yes, HSV can affect other parts of the body. For example, HSV-1 can cause herpetic whitlow, a painful infection of the fingers, or herpes gladiatorum, which affects the skin of athletes in contact sports. Ocular herpes, caused by HSV-1, can also affect the eyes, potentially leading to vision problems if untreated.
4. How does HSV affect pregnancy and childbirth?
HSV can pose risks during pregnancy and childbirth, particularly if a woman acquires HSV for the first time during pregnancy. Neonatal herpes, which occurs when an infant is exposed to the virus during delivery, can be severe and life-threatening. Pregnant women with HSV are often prescribed antiviral medications in the third trimester to reduce the risk of an outbreak and transmission during childbirth.
5. Can lifestyle changes prevent HSV outbreaks entirely?
While lifestyle changes such as stress management, adequate sleep, a balanced diet, and avoiding known triggers can help reduce the frequency and severity of HSV outbreaks, they cannot prevent them entirely. HSV remains in the body for life, and outbreaks can still occur despite these efforts.
6. Are there vaccines available for HSV?
Currently, there is no approved vaccine for HSV. Research is ongoing to develop a vaccine that could prevent HSV infection or reduce the severity of outbreaks in those already infected. Clinical trials are being conducted to evaluate potential vaccine candidates.
7. How can someone with HSV reduce the risk of spreading it to a partner?
People with HSV can reduce the risk of transmitting the virus to a partner by using condoms consistently, taking antiviral medications as suppressive therapy, avoiding sexual contact during outbreaks, and communicating openly with their partner about their HSV status.
8. Can HSV be cured?
There is no cure for HSV. The virus establishes lifelong latency in the body and can reactivate intermittently. While antiviral medications can help manage symptoms and reduce the frequency of outbreaks, they do not eliminate the virus.
9. Is HSV linked to other health conditions?
HSV-2, in particular, has been linked to an increased risk of acquiring HIV. The presence of genital sores from HSV-2 can make it easier for HIV to enter the body. Additionally, HSV infections can be more severe in people with weakened immune systems, such as those with HIV/AIDS or undergoing immunosuppressive therapy.
10. Can HSV be transmitted through kissing if there are no visible sores?
Yes, HSV-1 can be transmitted through kissing even if there are no visible sores. Asymptomatic viral shedding can occur, meaning the virus can be present on the skin or in saliva even in the absence of active lesions. This is why HSV is so easily spread.