Hematopoiesis is the process of blood cell formation and development that occurs throughout an organism’s lifetime. This complex biological process takes place primarily in the bone marrow and involves the production of all types of blood cells from hematopoietic stem cells (HSCs). These multipotent stem cells have the ability to self-renew and differentiate into various blood cell lineages, including red blood cells, white blood cells, and platelets. Hematopoiesis is tightly regulated by a network of growth factors, cytokines, and transcription factors that control the proliferation, differentiation, and maturation of blood cells. As individuals age, the hematopoietic system can undergo changes, such as the development of clonal hematopoiesis, where certain mutations in HSCs lead to the expansion of specific cell populations. Understanding hematopoiesis is crucial for comprehending normal blood cell production, as well as various hematological disorders and malignancies.
Stages of Hematopoiesis
Hematopoiesis is the process by which all blood cells are formed from hematopoietic stem cells. This complex process occurs in several stages, each characterized by the differentiation and maturation of specific cell types. Below are the primary stages of hematopoiesis:
1. Embryonic Hematopoiesis
Embryonic hematopoiesis is the initial stage of blood cell formation occurring in the early embryo. This process begins in the yolk sac around embryonic day 7.25 in mice, where the first wave of hematopoietic progenitors, including primitive erythroid, megakaryocyte, and macrophage progenitors, emerge. These progenitors are crucial for the survival and growth of the embryo, providing essential blood cells before the establishment of hematopoietic stem cells (HSCs). The yolk sac hematopoiesis is characterized by the formation of blood vessels and the simultaneous generation of red blood cells through a process known as hemo-vasculogenesis. This early hematopoietic activity is independent of HSCs and is necessary to support the embryo until the definitive hematopoietic system is established.
2. Fetal Hematopoiesis
Fetal hematopoiesis marks the transition from embryonic to more advanced blood cell development, primarily occurring in the fetal liver. This stage begins when HSCs emerge around mid-gestation and colonize the fetal liver, which becomes the main site of hematopoiesis until birth. During this period, erythro-myeloid progenitors (EMPs) from the yolk sac seed the fetal liver, initiating myelopoiesis and forming various blood cell lineages, including macrophages. The fetal liver hematopoiesis is crucial for the development of a diverse and functional hematopoietic system, which includes the production of multilineage hematopoietic cells that can repopulate the bone marrow and other tissues. Additionally, fetal HSCs exhibit unique migratory behaviors, responding to specific chemotactic signals that guide their homing to and seeding of hematopoietic tissues.
3. Adult Hematopoiesis
Adult hematopoiesis is the continuous production of blood cells throughout an individual’s life, primarily occurring in the bone marrow. This process is sustained by HSCs, which were initially established during fetal development and have the capacity for self-renewal and differentiation into various blood cell lineages. In adults, HSCs reside in specialized niches within the bone marrow, where they are regulated by a complex interplay of growth factors, cytokines, and the bone marrow microenvironment. Adult hematopoiesis ensures a steady supply of mature blood cells, including erythrocytes, leukocytes, and platelets, necessary for oxygen transport, immune defense, and hemostasis. The ability of HSCs to provide long-term hematopoietic repopulation following transplantation highlights their critical role in maintaining hematopoietic homeostasis throughout life.
Hematopoietic Organs
These organs play a crucial role in maintaining the body’s immune system and overall health. Below are the two types of Hematopoietic Organs:
1. Primary Hematopoietic Organs
The primary hematopoietic organ in adult mammals is the bone marrow, which serves as the main site for the maintenance and regulation of hematopoietic stem cells (HSCs) throughout an organism’s life. These HSCs are characterized by their ability to self-renew and differentiate into various blood cell types, ensuring the continuous replenishment of the blood system. The bone marrow provides a specialized microenvironment that supports HSC dormancy, quiescence, and differentiation through interactions with non-hematopoietic cells and various growth factors, transcription factors, and cytokines. Additionally, the spleen can serve as an alternative site for hematopoiesis, particularly under conditions of physiological stress or disease, where it can undergo extramedullary hematopoiesis (EMH).
2. Embryonic Hematopoietic Sites
During embryonic development, hematopoiesis occurs in several transitional sites before the bone marrow becomes the primary hematopoietic organ. Initially, hematopoiesis begins in the yolk sac, followed by the aorta-gonad-mesonephros (AGM) region, the placenta, and the fetal liver. These sites contribute to the formation and expansion of hematopoietic stem cells (HSCs) that will eventually colonize the bone marrow. The AGM region, in particular, has been identified as a critical site for the autonomous initiation of definitive hematopoiesis, which subsequently transitions to the fetal liver, where HSCs expand and establish the future adult hematopoietic hierarchy. Understanding the mechanisms and contributions of these embryonic hematopoietic sites is essential for advancing knowledge in hematopoietic system development and improving treatments for hematological diseases.
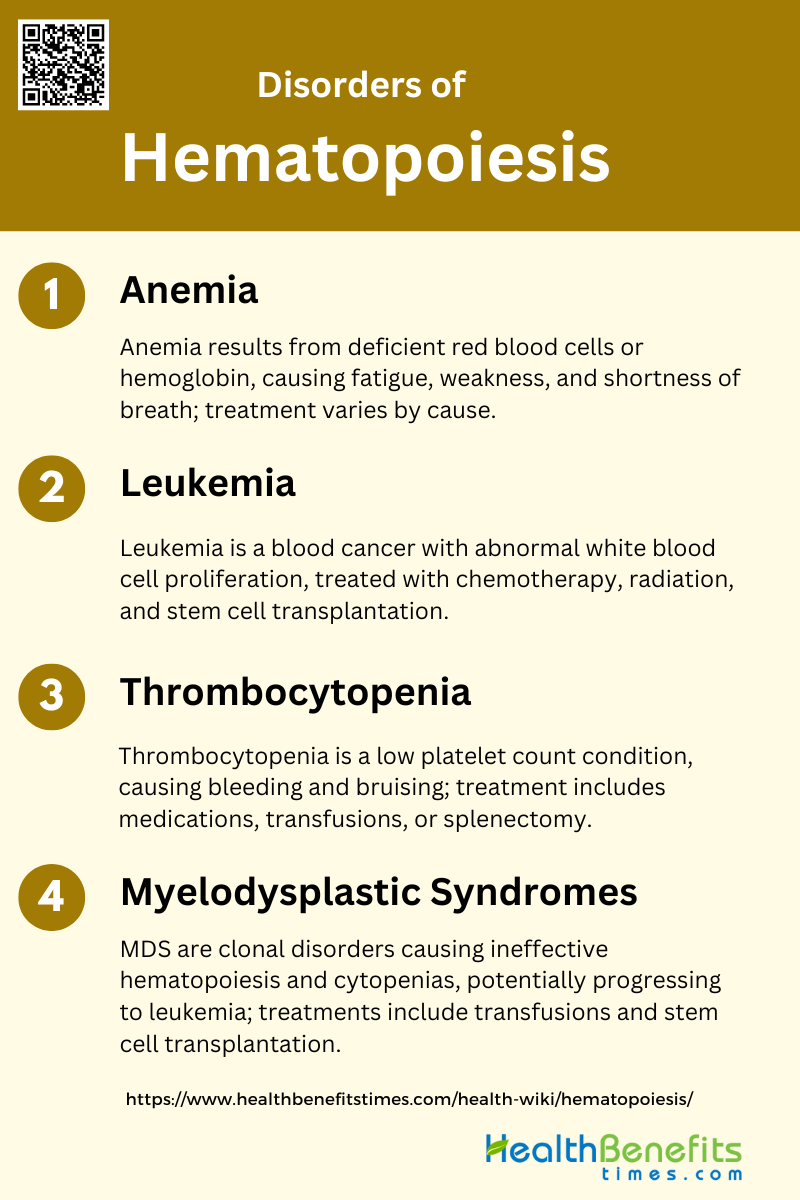
Disorders of Hematopoiesis
Disorders of hematopoiesis are conditions that affect the body’s ability to produce and regulate blood cells. These disorders can lead to a variety of health issues, including anemia, infections, and bleeding problems. Common disorders of hematopoiesis include:
1. Anemia
Anemia is a condition characterized by a deficiency of red blood cells or hemoglobin, leading to reduced oxygen transport in the body. Causes of anemia include nutritional deficiencies (iron, vitamin B12, folate), chronic diseases, genetic disorders, and bone marrow failure syndromes. Symptoms often include fatigue, weakness, pallor, and shortness of breath. Treatment varies based on the underlying cause and may involve dietary supplements, medications, or blood transfusions. In cases of aplastic anemia, clonal hematopoiesis can evolve into more severe conditions like myelodysplastic syndromes (MDS) or acute myeloid leukemia (AML).
2. Leukemia
Leukemia is a type of cancer that affects the blood and bone marrow, characterized by the uncontrolled proliferation of abnormal white blood cells. It can be classified into several types, including acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), chronic lymphocytic leukemia (CLL), and chronic myeloid leukemia (CML). The disease often presents with symptoms such as fatigue, frequent infections, and easy bruising or bleeding. Treatment options include chemotherapy, radiation therapy, targeted therapy, and hematopoietic stem cell transplantation. The prognosis and treatment plan depend on the specific type and stage of leukemia.
3. Thrombocytopenia
Thrombocytopenia is a condition characterized by an abnormally low number of platelets in the blood, which can lead to increased bleeding and bruising. Causes include bone marrow disorders, autoimmune diseases, infections, and certain medications. Symptoms may include easy bruising, prolonged bleeding from cuts, spontaneous bleeding from gums or nose, and petechiae (small red spots on the skin). Treatment depends on the underlying cause and may involve medications to boost platelet production, blood or platelet transfusions, or treating the underlying condition. In severe cases, splenectomy or immunosuppressive therapy may be considered.
4. Myelodysplastic Syndromes (MDS)
Myelodysplastic syndromes (MDS) are a group of clonal hematopoietic disorders characterized by ineffective hematopoiesis, leading to cytopenias and dysplasia in the bone marrow. MDS can progress to acute myeloid leukemia (AML) and is more common in the elderly. Symptoms include anemia, neutropenia, and thrombocytopenia, which can result in fatigue, increased risk of infections, and bleeding. Treatment options include supportive care, such as blood transfusions and growth factors, as well as disease-modifying therapies like hypomethylating agents and hematopoietic stem cell transplantation. Recent advances in understanding the molecular pathogenesis of MDS have led to the development of novel therapeutic approaches.
Diagnostic Methods of Hematopoiesis
Diagnostic methods of hematopoiesis are essential for identifying and understanding disorders related to blood cell production. These methods help in the early detection and management of various hematologic conditions. Common diagnostic techniques include:
1. Blood Tests
Blood tests are fundamental in diagnosing hematopoiesis-related disorders. They provide critical information about the different types of blood cells and their quantities, which can indicate underlying conditions such as anemia, leukemia, and other hematologic malignancies. For instance, peripheral blood smears can reveal abnormalities in blood cell morphology, prompting further investigation through bone marrow examination. Blood tests are often the first step in diagnosing hematopoietic disorders, as they can detect variations in red and white blood cell counts and platelet levels, which are indicative of various diseases. These tests are essential for monitoring disease progression and response to treatment, making them indispensable in clinical practice.
2. Bone Marrow Biopsy
Bone marrow biopsy is a critical diagnostic tool for evaluating hematopoiesis. It involves extracting a small sample of bone marrow tissue, usually from the iliac crest, to examine the architecture and cellularity of the marrow. This procedure is particularly useful for diagnosing conditions like aplastic anemia, myeloproliferative neoplasms, and hematologic malignancies such as leukemia and lymphoma. Bone marrow biopsy provides detailed information about the bone marrow microenvironment, including the presence of abnormal cells, fibrosis, and infiltration by malignant cells. It is often performed alongside bone marrow aspiration to provide a comprehensive view of the marrow’s health and is crucial for accurate diagnosis and treatment planning.
3. Imaging Tests
Imaging tests, such as MRI and PET scans, play a significant role in diagnosing and monitoring hematopoiesis. These non-invasive techniques allow for the visualization of bone marrow and other tissues, providing valuable information about the extent and activity of hematopoietic processes. For example, 18F-FLT PET/MRI can assess whole-body bone marrow activity and detect residual disease in patients with hematologic malignancies. Imaging tests are particularly useful for identifying extramedullary hematopoiesis, where hematopoietic activity occurs outside the bone marrow, often in response to bone marrow failure or ineffective erythropoiesis. These tests complement blood tests and bone marrow biopsies by offering a broader perspective on the patient’s condition, aiding in comprehensive diagnosis and management.
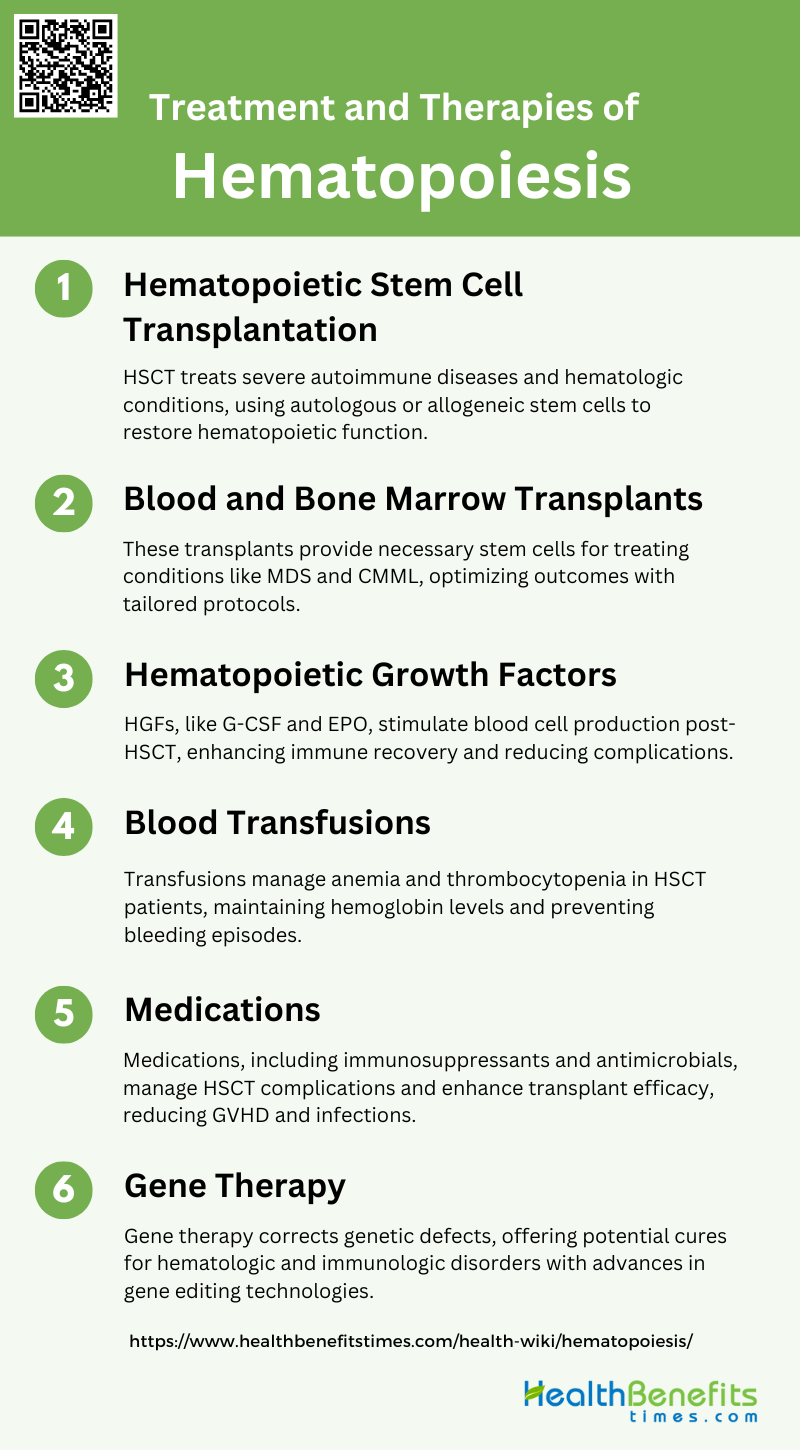
Treatment and Therapies of Hematopoiesis
Treatment and therapies of hematopoiesis focus on addressing disorders related to blood cell production and function. These treatments aim to restore normal hematopoietic activity and improve patient outcomes. Common treatment options include:
1. Hematopoietic Stem Cell Transplantation (HSCT)
Hematopoietic Stem Cell Transplantation (HSCT) has evolved significantly over the past two decades as a treatment for various severe autoimmune diseases (ADs) and hematologic conditions. Autologous HSCT, where the patient’s own stem cells are used, has shown improved outcomes in diseases like multiple sclerosis and systemic sclerosis, with better progression-free survival and reduced relapse rates over time. Allogeneic HSCT, using donor cells, remains a critical option for conditions like juvenile myelomonocytic leukemia (JMML) and primary immunodeficiencies, offering curative potential despite the associated risks of graft-versus-host disease (GVHD) and other complications. The development of non-genotoxic conditioning methods, such as the use of CD45-saporin immunotoxin, has shown promise in reducing the toxicity associated with traditional conditioning regimens, potentially broadening the applicability of HSCT.
2. Blood and Bone Marrow Transplants
Blood and bone marrow transplants are essential components of HSCT, providing the necessary stem cells for engraftment. Allogeneic transplants, where stem cells are sourced from a donor, are particularly crucial for treating conditions like myelodysplastic syndromes (MDS) and chronic myelomonocytic leukemia (CMML). Recommendations from international expert panels emphasize the importance of disease risk scoring and comorbidity assessment in determining transplant eligibility and optimizing outcomes. For patients with Fanconi anemia, a radiation-free, reduced-intensity conditioning regimen has shown excellent results, particularly with matched related donors, highlighting the importance of tailored conditioning protocols.
3. Hematopoietic Growth Factors
Agents like granulocyte colony-stimulating factor (G-CSF) and erythropoietin (EPO) are commonly used to stimulate the production of white and red blood cells, respectively, reducing the risk of infections and anemia. Additionally, keratinocyte growth factor (KGF) and other cytokines have been explored to promote thymic-dependent development of naive T cells, potentially improving long-term immune recovery and reducing the incidence of GVHD and other post-transplant complications.
4. Blood Transfusions
Blood transfusions are a critical supportive therapy in the management of patients undergoing HSCT. They are used to manage anemia and thrombocytopenia, common complications of both the underlying disease and the conditioning regimens used in HSCT. Regular transfusions of red blood cells and platelets help maintain adequate hemoglobin levels and prevent bleeding episodes, thereby improving patient outcomes and quality of life during the transplant process.
5. Medications
Medications play a crucial role in the success of HSCT by managing complications and enhancing the efficacy of the transplant. Immunosuppressive drugs are essential to prevent and treat GVHD, a common and serious complication of allogeneic HSCT. Additionally, antimicrobial prophylaxis and treatment are critical to managing infections, which are a significant cause of morbidity and mortality in HSCT patients. The use of targeted biologic therapies has also been integrated into HSCT protocols to improve outcomes in autoimmune diseases and hematologic malignancies.
6. Gene Therapy
Gene therapy represents a promising frontier in the treatment of hematologic and immunologic disorders. By correcting genetic defects at the molecular level, gene therapy aims to provide a permanent cure for conditions like hemoglobinopathies and congenital immunodeficiencies. Autologous HSCT using genetically corrected cells can potentially eliminate the risks associated with allogeneic transplants, such as GVHD. Advances in gene editing technologies, such as CRISPR/Cas9, are paving the way for more precise and effective gene therapy approaches, offering hope for patients with previously untreatable genetic disorders.