Dehydration is a condition characterized by a significant loss of body water, which can occur with or without the loss of electrolytes such as sodium. It can result from various factors including excessive sweating, inadequate fluid intake, or illnesses that cause vomiting or diarrhea. Dehydration can impair cognitive performance, particularly affecting tasks that require attention, executive function, and motor coordination, especially when body mass loss exceeds 2%. Clinically, dehydration is diagnosed through patient history, physical examination, and laboratory tests, and it can be categorized into water loss dehydration (hyperosmolar) and salt and water loss dehydration (hyponatremia). In the context of physical activity, dehydration can lead to reduced cardiac output and increased vascular resistance, which can compromise performance and increase the risk of heat-related illnesses. Effective management of dehydration involves rehydration strategies that may include oral or intravenous fluids, and in some cases, subcutaneous infusion of fluids. Understanding the physiological and clinical aspects of dehydration is crucial for preventing its adverse effects on health and performance.
Symptoms of Dehydration
Dehydration occurs when the body loses more fluids than it takes in, leading to a range of symptoms that can affect physical, cognitive, and overall health. Recognizing these symptoms early can help prevent more severe health issues. Below are the symptoms categorized into physical, severe, and cognitive manifestations:
1. Physical Symptoms
Dehydration manifests through various physical symptoms that can be easily observed. Some physical symptoms of dehydration are included in below:
- Dry mouth and skin: These symptoms occur because the body lacks sufficient fluids to maintain moisture levels.
- Feeling thirsty: This is a natural response to dehydration, signaling the need to replenish lost fluids.
- Dark yellow urine: The kidneys conserve water, resulting in more concentrated urine.
- Fatigue: Reduced blood volume and oxygen transport lead to feelings of tiredness.
- Dizziness or lightheadedness: Decreased blood pressure and reduced blood flow to the brain cause these symptoms.
2. Severe Symptoms
Severe dehydration can lead to more critical health issues. Below are the severe symptoms of dehydration:
- Rapid heartbeat: The heart works harder to pump a reduced volume of blood.
- Sunken eyes: This is a visible sign of severe fluid loss, often seen in extreme dehydration.
- Confusion or irritability: These occur due to the brain’s sensitivity to changes in electrolyte levels and reduced blood flow.
3. Cognitive Symptoms
Dehydration also affects cognitive functions. Some of cognitive symptoms of dehydration included in below:
- Headaches: Likely due to reduced blood flow and oxygen to the brain.
- Poor concentration: The brain’s decreased efficiency in processing information when dehydrated leads to this symptom.
- Mood swings: Dehydration can affect neurotransmitter function and overall brain health, causing mood changes.
Causes of Dehydration
Dehydration can result from various factors that either reduce fluid intake or increase fluid loss. Understanding these causes can help in preventing dehydration and maintaining optimal health. Below are some common causes of dehydration.
1. Inadequate Fluid Intake
Inadequate fluid intake is a primary cause of dehydration, particularly among the elderly and those with chronic illnesses. People continuously lose fluids through sweating, breathing, and urination, and failing to replenish these losses can lead to dehydration. This issue is exacerbated during hot weather or physical exercise, where fluid loss is more significant. Elderly individuals are especially vulnerable due to a diminished sense of thirst and potential mobility issues that make accessing fluids more challenging. Ensuring adequate fluid intake is crucial for maintaining hydration and preventing the adverse effects associated with dehydration.
2. Alcohol Consumption
Alcohol consumption can significantly impact the body’s ability to maintain fluid balance, particularly after exercise-induced dehydration. Studies have shown that beverages containing higher alcohol concentrations (e.g., 4%) can delay the recovery of blood and plasma volumes post-dehydration. This delay is due to alcohol’s diuretic effect, which increases urine production and hinders the body’s rehydration process. While moderate alcohol consumption (up to 2%) may not significantly affect rehydration, higher levels can exacerbate dehydration and slow recovery, making it essential to limit alcohol intake when rehydrating.
3. Excessive Fluid Loss
Excessive fluid loss, whether through sweating, urination, or other means, is a critical factor in dehydration. Activities that induce heavy sweating, such as prolonged exercise or exposure to high temperatures, can lead to significant fluid loss. Additionally, certain medical conditions and medications, such as diuretics, can increase urine output, further contributing to dehydration. Maintaining fluid balance in these situations requires proactive fluid intake to replace lost fluids and prevent the adverse effects of dehydration, such as impaired physical performance and cognitive function.
4. Diarrhea and Vomiting
Diarrhea and vomiting are common causes of dehydration, as they lead to rapid and significant fluid loss from the body. These conditions can result from various factors, including infections, food intolerances, and gastrointestinal disorders. The loss of fluids and electrolytes through diarrhea and vomiting can quickly deplete the body’s hydration levels, leading to symptoms such as dry mouth, decreased urine output, and dizziness. Prompt rehydration with fluids containing electrolytes is essential to restore balance and prevent severe dehydration and its complications.
5. Diabetes
Diabetes can contribute to dehydration due to the body’s increased need to eliminate excess glucose through urine. This process, known as osmotic diuresis, leads to higher urine output and fluid loss. Individuals with uncontrolled diabetes are particularly at risk, as elevated blood glucose levels exacerbate this effect. Additionally, some diabetes medications can increase the risk of dehydration. Managing blood glucose levels and ensuring adequate fluid intake are crucial for individuals with diabetes to prevent dehydration and maintain overall health.
6. Fever
Fever increases the body’s metabolic rate and leads to higher fluid loss through sweating and respiration. This elevated fluid loss can quickly result in dehydration, especially if fluid intake is not increased to compensate. Fever is often associated with infections and illnesses that can further contribute to fluid loss through symptoms like diarrhea and vomiting. Maintaining adequate hydration during episodes of fever is essential to support the body’s immune response and prevent the complications associated with dehydration.
7. Diuretics and Certain Blood Pressure Medications
Diuretics and certain blood pressure medications can increase the risk of dehydration by promoting fluid loss through increased urine production. These medications are often prescribed to manage conditions such as hypertension and heart failure, but they can lead to significant fluid and electrolyte imbalances if not monitored carefully. Patients taking these medications should be advised to maintain adequate fluid intake and monitor for signs of dehydration, such as dry mouth, dizziness, and decreased urine output, to prevent adverse health effects.
8. Prolonged Exposure to High Temperatures
Prolonged exposure to high temperatures can lead to significant fluid loss through sweating, increasing the risk of dehydration. This is particularly concerning during heatwaves or for individuals engaging in outdoor activities in hot climates. The body’s need to cool itself through sweating can deplete fluid levels rapidly, leading to symptoms such as dry skin, dizziness, and heat-related illnesses. Ensuring adequate fluid intake and taking measures to stay cool are essential strategies to prevent dehydration and maintain health during periods of high temperature exposure.
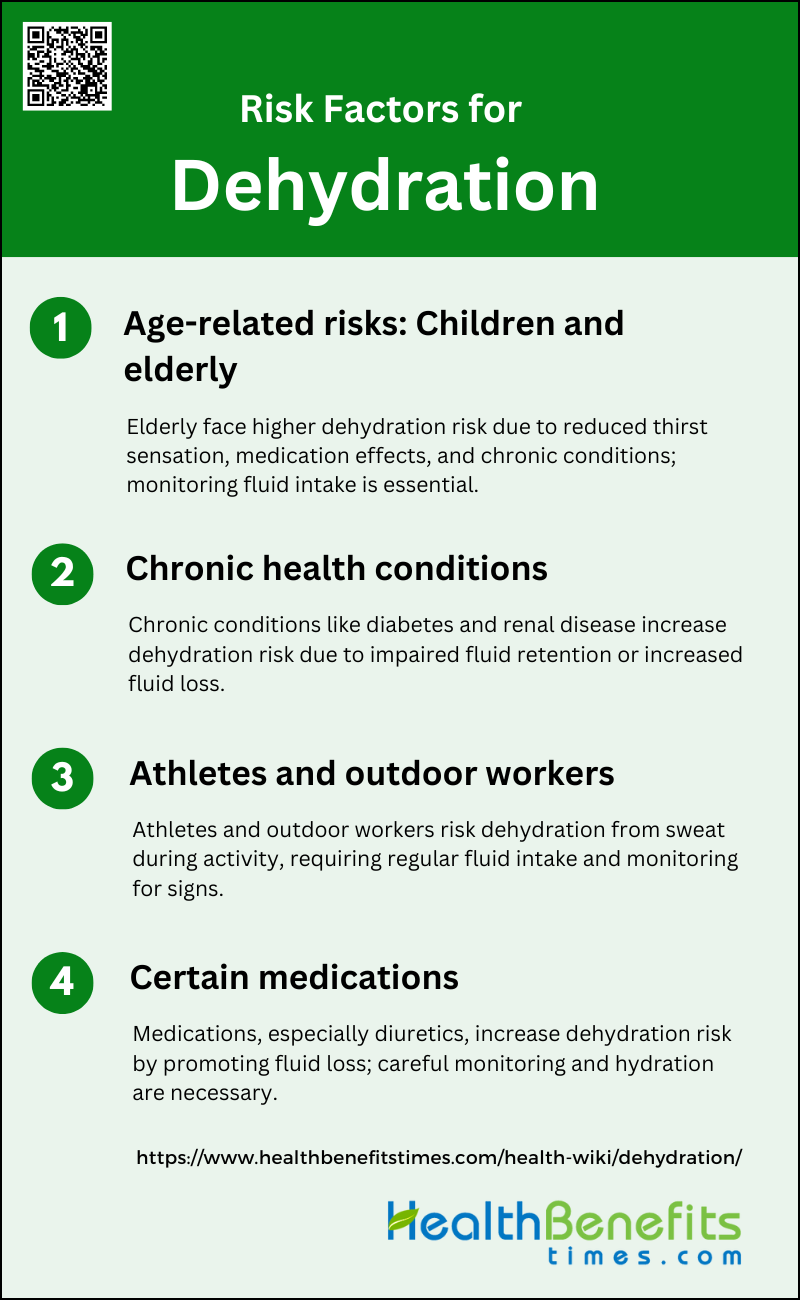
Risk Factors for Dehydration
Dehydration can affect anyone, but certain factors can increase the risk. Being aware of these risk factors can help in taking preventive measures to stay hydrated. Below are some common risk factors for dehydration:
1. Age-related risks: Children and elderly
The elderly are particularly vulnerable to dehydration due to several age-related factors. Changes in functional and mental status, medication effects, and alterations in the renal system contribute to this increased risk. Additionally, hypodipsia, or a reduced sensation of thirst, is a common physiological change in aging, making it harder for older adults to recognize their need for fluids. Studies have shown that elderly individuals, especially those in nursing homes, are at higher risk due to factors such as chronic conditions, polypharmacy, and physical limitations. Effective management strategies include ensuring adequate fluid intake and monitoring for signs of dehydration, particularly during illness or warm weather.
2. Chronic health conditions
Chronic health conditions significantly elevate the risk of dehydration. Conditions such as diabetes, renal diseases, and cardiovascular issues can exacerbate fluid loss or impair fluid intake. For instance, diabetes can lead to increased urination, while renal diseases affect the body’s ability to retain fluids. Additionally, chronic infections and the use of medications like diuretics and laxatives further increase dehydration risk. Effective management involves regular monitoring of fluid balance and adjusting treatment plans to mitigate these risks, especially in patients with multiple chronic conditions.
3. Athletes and outdoor workers
Athletes and outdoor workers are at a heightened risk of dehydration due to increased fluid loss through sweat during physical activity. This risk is exacerbated in hot and humid conditions, where the body loses fluids more rapidly. Maintaining hydration is crucial for these groups to prevent heat-related illnesses and maintain performance levels. Strategies include regular fluid intake before, during, and after physical activity, and monitoring for signs of dehydration such as dizziness, fatigue, and dark urine. Ensuring access to water and electrolyte solutions can help mitigate these risks and promote better hydration practices.
4. Certain medications
Certain medications, particularly diuretics, significantly increase the risk of dehydration by promoting fluid loss through increased urination. Other medications, such as laxatives and anti-inflammatory drugs, can also contribute to fluid imbalance. Elderly individuals are particularly susceptible due to the high prevalence of polypharmacy, where multiple medications are used to manage various chronic conditions. Effective management includes regular monitoring of fluid status, adjusting medication dosages as necessary, and educating patients on the importance of maintaining adequate hydration while on these medications.
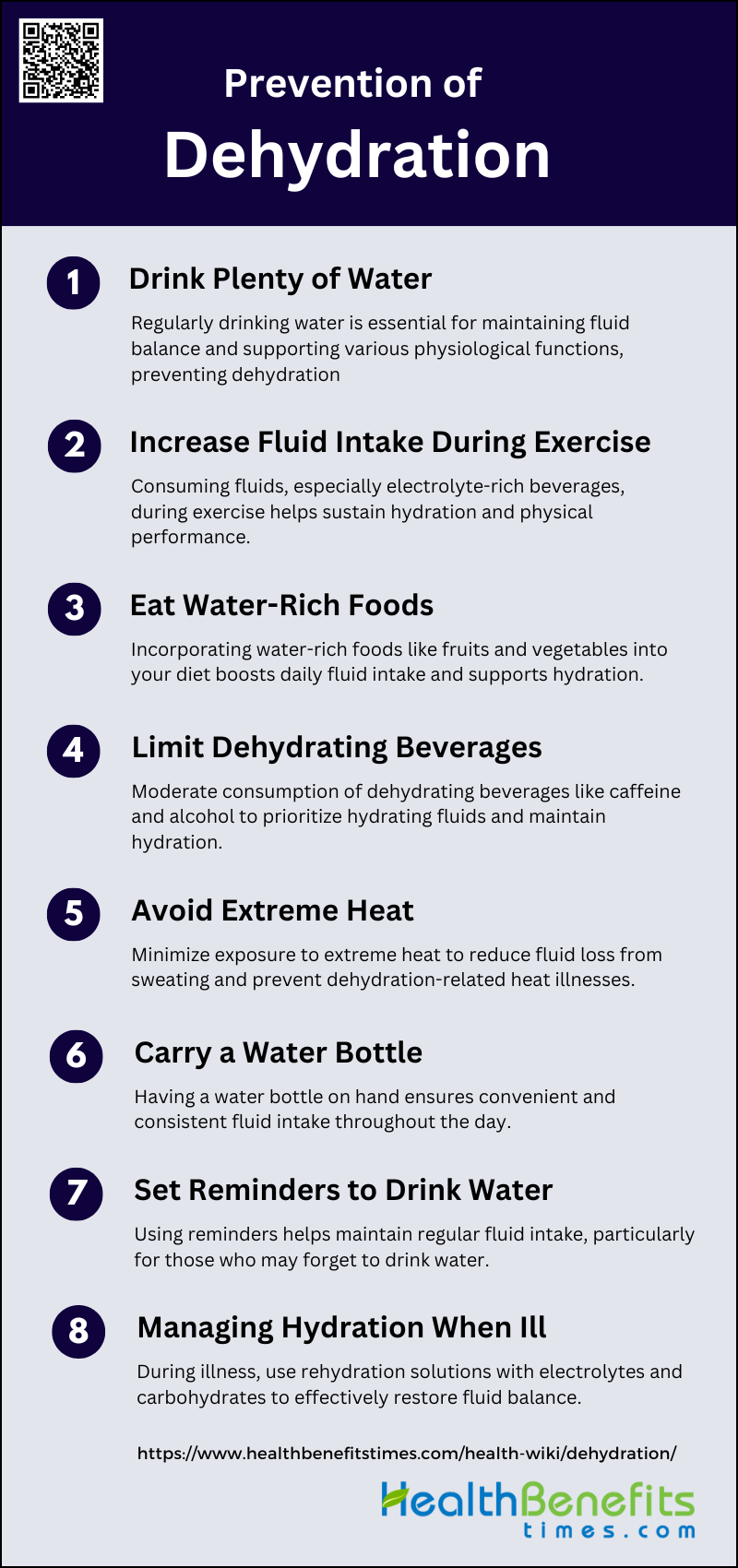
Prevention of Dehydration
Preventing dehydration involves proactive measures to ensure adequate fluid intake and minimize fluid loss. By adopting healthy habits and being mindful of certain activities, one can effectively reduce the risk of dehydration. Below are some strategies for preventing dehydration:
1. Drink Plenty of Water
Drinking plenty of water is essential for maintaining hydration and overall health. Water is the most effective and readily available fluid for rehydration. It helps in maintaining the balance of bodily fluids, which is crucial for various physiological functions such as digestion, absorption, circulation, and temperature regulation. Studies have shown that water is effective in rehydrating the body after exercise-induced dehydration, although it may not be as effective as carbohydrate-electrolyte solutions in retaining fluids over a longer period. Therefore, it is recommended to drink water regularly throughout the day to prevent dehydration.
2. Increase Fluid Intake During Exercise
Increasing fluid intake during exercise is crucial to prevent dehydration and maintain performance. Dehydration can significantly impair physical performance, especially in hot environments. Consuming fluids before and during exercise can help maintain hydration levels and delay the onset of dehydration. Studies have shown that consuming beverages containing electrolytes and carbohydrates during exercise can provide additional benefits over water alone, as they help maintain electrolyte balance and provide energy. Therefore, it is important to drink fluids at regular intervals during exercise to stay hydrated and sustain performance.
3. Eat Water-Rich Foods
Eating water-rich foods is an effective way to boost hydration. Foods such as fruits and vegetables have high water content and can contribute significantly to daily fluid intake. For example, watermelon, cucumbers, and oranges are over 90% water. These foods not only provide hydration but also supply essential vitamins and minerals that support overall health. Incorporating water-rich foods into the diet can be particularly beneficial for individuals who may not drink enough water throughout the day. This approach complements fluid intake from beverages and helps maintain optimal hydration levels.
4. Limit Dehydrating Beverages
Limiting the intake of dehydrating beverages such as caffeinated drinks and alcohol is important for maintaining hydration. These beverages can increase urine output and contribute to fluid loss, potentially leading to dehydration. Studies have shown that beverages like caffeinated diet cola are less effective in rehydrating the body compared to water and carbohydrate-electrolyte solutions. Therefore, it is advisable to consume these beverages in moderation and prioritize water and other hydrating fluids to ensure adequate hydration.
5. Avoid Extreme Heat
Avoiding extreme heat is crucial for preventing dehydration, as high temperatures can increase sweat production and fluid loss. Engaging in physical activities in hot environments can exacerbate dehydration and negatively impact performance. It is important to take measures such as staying in shaded or air-conditioned areas, wearing lightweight and breathable clothing, and scheduling outdoor activities during cooler parts of the day. Additionally, prehydrating before exposure to heat and drinking fluids regularly can help maintain hydration levels and reduce the risk of heat-related illnesses.
6. Carry a Water Bottle
Carrying a water bottle is a practical strategy to ensure regular fluid intake throughout the day. Having a water bottle readily available serves as a constant reminder to drink water and makes it convenient to stay hydrated, especially when on the go. This habit can help individuals meet their daily hydration needs and prevent dehydration. Studies have shown that having easy access to fluids can increase voluntary water consumption and improve hydration status. Therefore, carrying a water bottle is a simple yet effective way to promote consistent hydration.
7. Set Reminders to Drink Water
Setting reminders to drink water can be an effective way to ensure adequate hydration, especially for individuals who may forget to drink fluids regularly. Using alarms, smartphone apps, or visual cues can prompt individuals to drink water at regular intervals throughout the day. This strategy can help maintain consistent fluid intake and prevent dehydration. Research has shown that structured hydration strategies, such as setting reminders, can improve fluid intake and hydration status in various populations, including older adults and athletes.
8. Managing Hydration When Ill
Managing hydration when ill is critical, as illnesses such as fever, vomiting, and diarrhea can lead to significant fluid loss. Using rehydration solutions that contain electrolytes and carbohydrates can be more effective than water alone in restoring fluid balance. These solutions help replace lost electrolytes and provide energy, which is essential for recovery. Studies have demonstrated the effectiveness of carbohydrate-electrolyte solutions in rehydrating individuals after exercise-induced dehydration and other conditions that cause fluid loss. Therefore, using rehydration solutions can be a valuable strategy for managing hydration during illness.
When to Seek Medical Help for Dehydration
Signs of Severe Dehydration That Require Medical Attention
Severe dehydration manifests through various clinical symptoms and signs that necessitate immediate medical intervention. In older adults, critical indicators include extreme fatigue, missing drinks between meals, and specific bioelectrical impedance analysis (BIA) resistance values. Additionally, physical signs such as low systolic blood pressure, dry mucous membranes, poor skin turgor, and sunken eyes are significant markers. In children, the presence of three or more clinical signs such as capillary refill time greater than two seconds, absence of tears, dry mucous membranes, and an ill general appearance are reliable indicators of severe dehydration. These symptoms, if observed, should prompt urgent medical evaluation to prevent further health complications.
The Importance of Early Intervention
Early intervention in cases of dehydration is crucial to mitigate the associated morbidity and mortality, especially in vulnerable populations such as older adults and children. Prompt diagnosis and treatment can significantly improve patient outcomes and reduce the burden on healthcare systems. For instance, early identification of dehydration through reliable markers like saliva osmolality can aid in timely rehydration, thereby preventing severe complications. In pediatric cases, recognizing and addressing dehydration early, based on clinical signs, can prevent the progression to more severe states that are harder to manage. Therefore, early intervention is essential to ensure better health outcomes and prevent the escalation of dehydration-related health issues.
Dehydration Myths and Facts
There are many misconceptions about dehydration that can lead to confusion and improper hydration practices. Understanding the myths and facts about dehydration can help you stay properly hydrated and maintain your health. Below are some common myths and facts about dehydration.
1. Myth: Everyone Needs to Drink Eight Glasses of Water a Day
The recommendation to drink eight glasses of water daily for proper hydration and skin health is widely circulated but lacks scientific backing. Studies have found no evidence supporting the necessity of this specific amount for maintaining skin hydration or overall health. The idea remains a myth, as scientific validation is still pending.
2. Myth: Caffeine Causes Dehydration
Contrary to popular belief, moderate coffee consumption does not lead to dehydration. Research comparing water and coffee intake found no significant differences in hydration markers, such as total body water, urine volume, and haematological parameters. This suggests that coffee, when consumed in moderation, hydrates similarly to water.
3. Myth Dark-Colored Urine Always Indicates Dehydration
While dark-colored urine can be a sign of dehydration, it is not a definitive indicator. Studies have shown that factors like diet, medication, and certain health conditions can also affect urine color. Therefore, relying solely on urine color to assess hydration status can be misleading.
4. Myth: Thirst is the Best Indicator of Dehydration
Thirst is not always a reliable indicator of dehydration. Research indicates that by the time you feel thirsty, you may already be mildly dehydrated. Additionally, factors like age and physical activity can affect thirst perception, making it an inconsistent measure of hydration status.
5. Myth: Drinking Water is the Only Way to Stay Hydrated
Hydration can be maintained through various fluids and foods, not just water. Beverages like milk, juice, and even coffee contribute to daily fluid intake. Additionally, many fruits and vegetables have high water content, which helps in maintaining hydration.
6. Myth: Alcohol Dehydrates You
Alcohol does have a diuretic effect, which can lead to increased urine production and potential dehydration. However, the extent of dehydration depends on the amount and type of alcohol consumed. Moderate alcohol intake may not significantly impact overall hydration status.
7. Myth: Drinking Water Before Bed Prevents Dehydration Overnight
Drinking water before bed does not necessarily prevent dehydration overnight. While it can help maintain hydration, it may also lead to frequent urination, disrupting sleep. The body’s homeostatic mechanisms generally manage hydration levels effectively during sleep.