A contusion is a type of injury that occurs when blood vessels beneath the skin are damaged, typically due to blunt force trauma, causing blood to leak into the surrounding tissues. This results in swelling, discoloration, and tenderness in the affected area. Contusions can occur in various parts of the body, including the brain and internal organs, not just on the skin’s surface. In the case of cerebral contusions, which are bruises on the brain tissue, they can lead to more severe consequences and may require careful medical management. The severity of a contusion can vary widely, from minor bruising that resolves on its own to more serious injuries that may require medical intervention, especially when involving vital organs or the brain.
Causes of Contusion
Contusions, or bruises, result from the rupture of small blood vessels beneath the skin due to various external factors. These factors can include direct trauma, sports injuries, repetitive pressure, and accidents. Below is a list of Contusion:
1. Trauma and Physical Impact
Contusions are often caused by direct trauma and physical impact, which can result in significant tissue damage. For instance, in the context of traumatic brain injury (TBI), the primary injury is caused by the kinetic energy delivered at the time of impact, leading to cerebral contusions. These contusions can progress and worsen due to secondary injury responses, such as hemorrhagic progression, which involves continued bleeding and microvascular failure. Similarly, blunt chest trauma can cause cardiac contusions, which are often seen in traffic accidents and can lead to severe outcomes like cardiogenic shock. The severity of contusions from physical impact is influenced by factors such as the force and angle of the impact, as well as the resilience of the affected tissues.
2. Sports and Recreational Injuries
Sports and recreational activities are common sources of contusion injuries, particularly in contact sports. Muscle contusions are second only to strains in terms of sports-related morbidity. The severity of these injuries depends on factors such as the site of impact, muscle activation status, and the presence of fatigue. In athletic competitions, contusions can occur from both contact and non-contact sports, leading to microscopic muscle cell ruptures, infiltrative bleeding, and inflammation. The physiological responses to such injuries include pain, edema, and loss of muscle function, which can be quantified using various diagnostic tools like MRI and ultrasonography. Preventive measures and appropriate treatment protocols are essential to manage these injuries and prevent complications like myositis ossificans.
3. Repetitive Pressure
Repetitive pressure can also lead to contusions, particularly in scenarios involving continuous or repeated impact on specific body parts. This type of injury is common in certain sports and occupational activities where specific muscles or tissues are subjected to repeated stress. The continuous pressure can cause microtrauma to the tissues, leading to inflammation, pain, and eventual contusion. For example, in the context of lung contusions, repetitive blunt chest trauma can result in significant pulmonary damage, characterized by inflammation, hypoxemia, and impaired lung mechanics. The body’s response to repetitive pressure involves a complex interplay of inflammatory mediators and cellular responses, which can exacerbate the injury over time.
4. Accidents and Falls
Accidents and falls are frequent causes of contusions, affecting both athletes and non-athletes alike. These incidents can lead to various types of contusions, including muscle, cerebral, and cardiac contusions. For instance, simple falls can cause muscle contusions characterized by microscopic muscle cell damage, bleeding, and inflammation. In more severe cases, such as falls resulting in head trauma, cerebral contusions can occur, leading to significant neurological impairment due to hemorrhagic progression and secondary injury responses. Similarly, falls impacting the chest can cause cardiac contusions, which may present with symptoms ranging from mild discomfort to severe cardiogenic shock. The diagnosis and management of contusions from accidents and falls require careful clinical evaluation and appropriate imaging techniques to assess the extent of the injury.
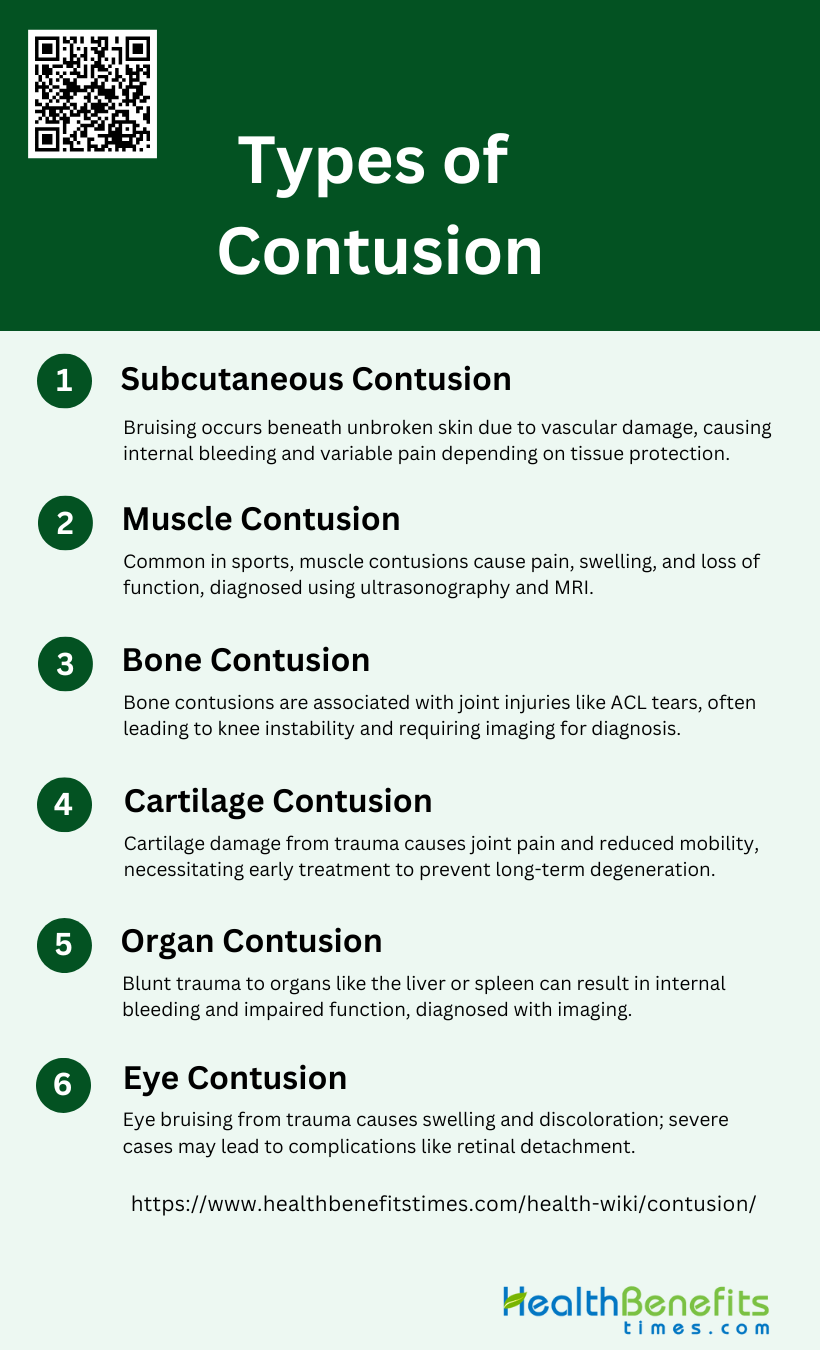
Types of Contusion
Contusions can occur in different parts of the body, each with distinct features and implications. Recognizing these types helps in understanding the severity and treatment required for each case. Below is a list of the primary types of contusions:
1. Subcutaneous Contusion
Subcutaneous contusions are injuries where the skin remains unbroken, but the underlying tissues, such as muscles, nerves, or bones, are damaged due to a blunt force. These injuries are characterized by vascular rupture, leading to internal bleeding and bruising. The severity of a subcutaneous contusion depends on the force of impact and the amount of fat or muscle cushioning the area. Symptoms often include numbness, followed by aching or throbbing pain during the inflammatory stage. The pain experienced is not always proportional to the injury’s severity, and the presence of fat or muscle can mitigate the impact’s effects.
2. Muscle Contusion
Muscle contusions are common sports-related injuries, second only to muscle strains. The severity of a muscle contusion depends on factors such as the impact site, muscle activation status, patient age, and fatigue levels. Diagnosis traditionally relies on clinical judgment, but modern imaging techniques like ultrasonography and MRI are increasingly used to assess the injury’s extent. The healing process involves a balance between muscle repair, regeneration, and scar tissue formation. Research is ongoing to evaluate treatments, including anti-inflammatory medications, corticosteroids, and exercise protocols, to prevent complications like myositis ossificans and improve recovery outcomes.
3. Bone Contusion
Bone contusions often occur in conjunction with other injuries, such as anterior cruciate ligament (ACL) tears. These contusions are identified using MRI and are commonly found in the lateral femoral condyle and lateral tibial plateau. The presence and severity of bone contusions are associated with high-grade pivot-shift injuries, concomitant lateral meniscal lesions, and abnormalities in the anterolateral ligament. These associations suggest that bone contusions can indicate more severe joint instability and damage. Understanding these relationships helps in diagnosing and managing knee injuries more effectively, particularly in athletes.
4. Cartilage Contusion
Cartilage contusions involve damage to the cartilage, often due to blunt trauma or joint injuries. These contusions can lead to cartilage softening, fissuring, or even fragmentation, which may compromise joint function. Symptoms typically include joint pain, swelling, and reduced mobility. Diagnosis is usually confirmed through imaging techniques like MRI, which can reveal the extent of cartilage damage. Treatment focuses on reducing inflammation and promoting cartilage healing, often involving rest, physical therapy, and sometimes surgical intervention. Early detection and management are crucial to prevent long-term joint degeneration and maintain mobility.
5. Organ Contusion
Organ contusions are serious injuries resulting from blunt trauma to internal organs such as the liver, spleen, or kidneys. These contusions can cause internal bleeding, swelling, and impaired organ function. Symptoms vary depending on the affected organ but often include pain, tenderness, and signs of internal bleeding like hypotension or shock. Diagnosis typically involves imaging studies such as CT scans to assess the extent of the injury. Treatment may range from conservative management with monitoring and supportive care to surgical intervention in severe cases. Prompt diagnosis and appropriate treatment are essential to prevent complications and ensure recovery.
6. Eye Contusion
Eye contusions, commonly known as black eyes, result from blunt trauma to the eye area, causing bruising and swelling. These injuries can affect the eyelids, surrounding tissues, and sometimes the eye itself. Symptoms include pain, swelling, discoloration, and sometimes vision disturbances. While most eye contusions are minor and heal with time, severe cases can lead to complications such as hyphema (bleeding in the eye), retinal detachment, or orbital fractures. Diagnosis involves a thorough eye examination and imaging if necessary. Treatment typically includes cold compresses, pain management, and monitoring for any signs of complications.
Symptoms of a Contusion
Contusions present with a range of symptoms that reflect the extent of the injury. Identifying these symptoms helps in evaluating the impact and guiding the healing process. Below is a list of typical symptoms experienced with contusions:
1. Pain and Discomfort at the Site of Injury
Pain and discomfort are common symptoms of a contusion, often resulting from the initial trauma that causes damage to the underlying tissues. This pain can vary in intensity depending on the severity of the injury and the extent of tissue damage. For instance, in cases of severe quadriceps muscle contusions, athletes may experience significant pain immediately after the injury, which can worsen over the next 24 hours due to swelling and increased intramuscular pressure. Similarly, a 16-year-old boy with a forearm contusion reported mild pain that persisted and gradually increased over five weeks, indicating the ongoing impact of the injury on the affected tissues.
2. Swelling and Tenderness
Swelling and tenderness are hallmark symptoms of contusions, resulting from the body’s inflammatory response to injury. Swelling occurs as blood and other fluids accumulate in the injured area, leading to increased pressure and discomfort. For example, in a case study of a 19-year-old girl with a quadriceps muscle contusion, significant swelling was observed, which limited her range of motion and contributed to her pain. Similarly, a 16-year-old boy with a forearm contusion experienced increased swelling over several weeks, accompanied by tenderness to palpation, highlighting the progressive nature of these symptoms.
3. Stiffness in the Injured Area
Stiffness in the injured area is another common symptom of contusions, often resulting from swelling and the body’s protective response to limit movement and prevent further injury. This stiffness can significantly impact the range of motion and functionality of the affected area. For instance, athletes with severe quadriceps muscle contusions may experience limited knee motion due to the stiffness and swelling in the thigh muscles. In another case, a 62-year-old woman with a knee contusion reported decreased pain but still experienced point tenderness and stiffness in the knee, affecting her overall mobility.
4. Discoloration of the Skin
Discoloration of the skin is a visible symptom of contusions, caused by the leakage of blood from damaged capillaries into the surrounding tissues. This discoloration typically progresses through various stages, starting with black or blue hues and eventually fading to purple, yellow, and green as the body reabsorbs the blood. For example, a 39-year-old female farmer with a finger injury exhibited a reddish-blue discoloration at the site of the contusion, which is characteristic of the early stages of bruising. Similarly, in cases of muscle contusions, the skin over the injured area may show significant discoloration, reflecting the extent of underlying tissue damage and bleeding.
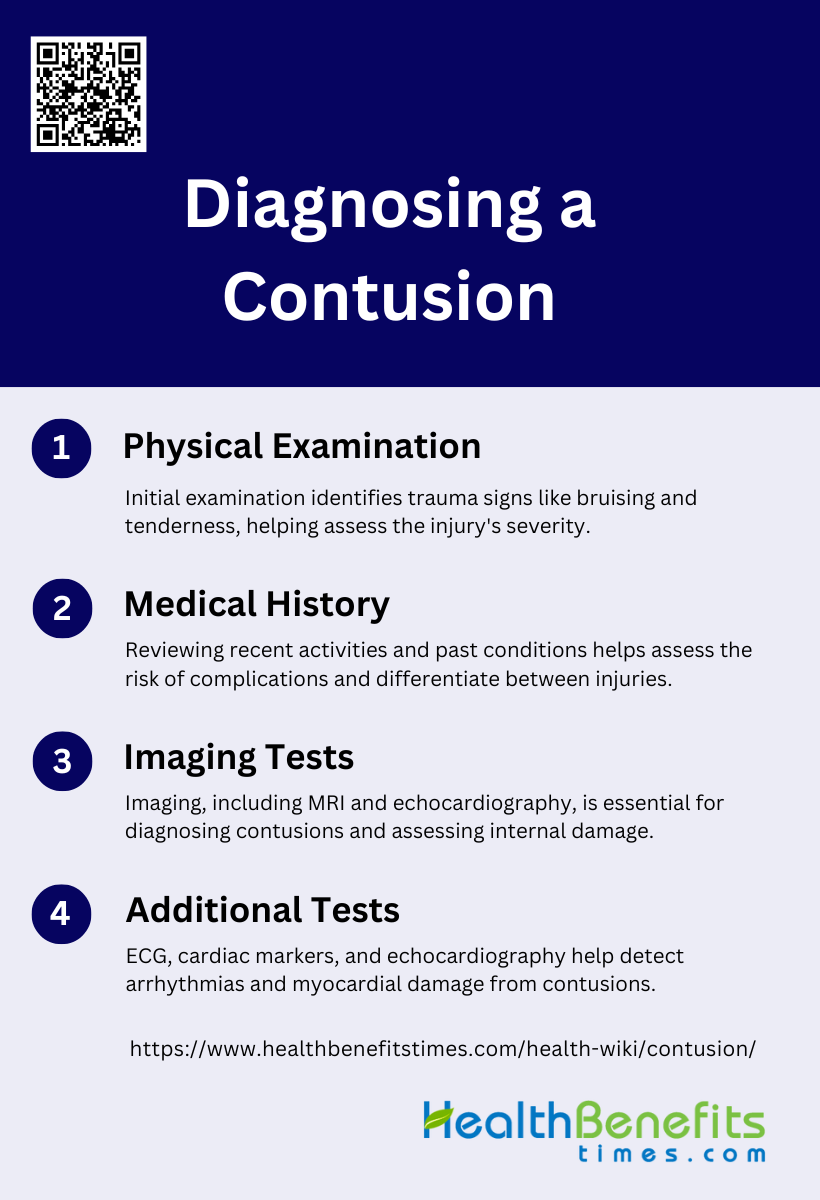
Diagnosing a Contusion
Diagnosing a contusion requires a systematic approach to assess the injury’s severity and rule out other potential complications. This involves a combination of physical examination, medical history review, and diagnostic tests. Below are the primary methods used in diagnosing a contusion:
1. Physical Examination
Diagnosing a contusion, particularly a cardiac contusion, begins with a thorough physical examination. This step is crucial as it helps identify any immediate signs of trauma, such as bruising, tenderness, or swelling in the chest area. Physical examination can also reveal signs of more severe complications, such as irregular heartbeats or abnormal heart sounds, which may indicate underlying cardiac issues. According to recent studies, physical examination remains a simple yet effective method for initial screening, especially when combined with other diagnostic tools like electrocardiography (ECG). However, it is important to note that physical examination alone may not be sufficient to diagnose myocardial contusion definitively, necessitating further diagnostic tests.
2. Medical History
Taking a detailed medical history is another essential step in diagnosing a contusion. This involves gathering information about the patient’s recent activities, any incidents of blunt chest trauma, and pre-existing medical conditions. For instance, a history of involvement in car or motorcycle accidents can raise the suspicion of a cardiac contusion. Additionally, understanding the patient’s past medical history, including any previous cardiac issues, can help in assessing the risk and potential complications. Medical history also aids in differentiating between cardiac contusion and other conditions that may present with similar symptoms, such as myocardial infarction. Therefore, a comprehensive medical history is indispensable for accurate diagnosis and effective management.
3. Imaging Tests
Imaging tests play a pivotal role in diagnosing contusions, especially cardiac contusions. Techniques such as chest X-rays, computed tomography (CT) scans, and magnetic resonance imaging (MRI) are commonly used. While chest X-rays and CT scans can identify associated thoracic injuries, they provide limited information on myocardial damage. Cardiac MRI, on the other hand, offers detailed visualization of myocardial abnormalities and is particularly useful in detecting myocardial hemorrhage and fibrosis. Echocardiography, including transthoracic and transesophageal methods, is also valuable for assessing wall motion abnormalities and other structural changes in the heart. These imaging modalities, when used in conjunction, enhance the accuracy of diagnosing cardiac contusions.
4. Additional Tests
Additional tests such as electrocardiography (ECG), cardiac markers (e.g., troponin), and echocardiography are critical in diagnosing cardiac contusions. ECG is a primary tool for detecting arrhythmias and other electrical abnormalities in the heart. Cardiac markers like troponin I and T are highly sensitive and specific for myocardial injury, making them essential for identifying myocardial contusions. Echocardiography provides real-time images of the heart, helping to detect wall motion abnormalities and other structural issues. These tests, when combined, offer a comprehensive assessment of cardiac function and are crucial for early detection and management of life-threatening complications associated with cardiac contusions.
Treatment for Contusions
Treating contusions effectively involves a combination of basic care techniques and medical interventions to alleviate symptoms and promote healing. Understanding the appropriate treatment options can significantly enhance recovery and prevent complications. Below are the primary Treatment for Contusions:
1. Basic Care
The R.I.C.E. method is a cornerstone in the initial management of acute soft-tissue injuries, including contusions. This approach involves Rest, Ice, Compression, and Elevation to minimize swelling and pain. Ice therapy, or cryotherapy, should be applied as soon as possible after the injury and continued several times a day for 20 minutes over several days to reduce inflammation and pain. Compression and elevation help to limit swelling and support the injured area, promoting faster recovery. Despite its widespread recommendation, studies indicate that the complete R.I.C.E. protocol is not always fully implemented in clinical settings, suggesting a need for better adherence and education on its benefits.
2. Medication
Pain management is a critical component of treating contusions. Mild pain can be effectively managed with over-the-counter pain relievers such as acetaminophen, which is preferred over aspirin due to its lack of effect on blood coagulation. In more severe cases, nonsteroidal anti-inflammatory drugs (NSAIDs) may be prescribed to reduce pain and inflammation. However, the use of medication should be carefully monitored to avoid potential side effects and interactions with other treatments. The goal is to alleviate pain while minimizing the risk of complications, allowing the patient to engage in other therapeutic activities that promote healing.
3. Physical Therapy
Physical therapy plays a vital role in the rehabilitation of contusions, especially after the initial acute phase has passed. It involves targeted exercises to restore strength, flexibility, and range of motion to the affected area. Early mobilization is crucial to prevent muscle atrophy and loss of function, which can occur with prolonged immobilization. Techniques such as stretching, strengthening exercises, and functional training are tailored to the severity and location of the injury. Additionally, protective measures, such as wearing a thigh pad during activities, can help prevent re-injury and support the healing process. Physical therapy not only aids in recovery but also helps in preventing future injuries by improving overall muscle function and resilience.
Prevention of Contusions
Preventing contusions requires a combination of protective measures and mindful practices to reduce the risk of injury. By implementing these strategies, individuals can safeguard themselves against bruises and maintain a safer environment. Below is the Prevention of Contusions:
1. Use Protective Equipment
Using protective equipment is essential in preventing contusions and other injuries. Protective gear such as helmets, knee pads, elbow pads, and shin guards can significantly reduce the risk of injury during physical activities. For instance, the use of patellofemoral braces has been shown to be effective in preventing anterior knee pain in runners and military recruits. Additionally, custom-made biomechanical insoles can help reduce the incidence of shin splints, particularly in high-risk groups like military personnel. Overall, the consistent use of appropriate protective equipment can mitigate the impact of falls and collisions, thereby preventing contusions and other injuries.
2. Proper Footwear
Wearing proper footwear is crucial for preventing contusions and other lower limb injuries. Footwear that provides adequate support and cushioning can help absorb impact and reduce stress on the feet and legs. Studies have shown that therapeutic footwear with plantar pressure-relieving effects can prevent foot ulcers in diabetic patients. Similarly, custom-made insoles have been found to reduce the risk of bone stress injuries in military settings. Ensuring that footwear is well-fitted and appropriate for the activity can significantly lower the risk of injuries, including contusions, by providing the necessary support and protection.
3. Prepare for Physical Activity
Proper preparation for physical activity is essential to prevent contusions and other injuries. This includes engaging in warm-up exercises, stretching, and conditioning to improve flexibility, strength, and coordination. Multicomponent injury-prevention training programs, which include exercises for strength, plyometrics, agility, balance, and flexibility, have been shown to reduce the risk of injuries such as anterior cruciate ligament (ACL) tears. Additionally, modifying training schedules to include gradual increases in intensity and duration can help prevent overuse injuries. Adequate preparation ensures that the body is ready for physical exertion, thereby reducing the likelihood of contusions.
4. Exercise Caution
Exercising caution during physical activities is vital for preventing contusions. This involves being aware of one’s surroundings, avoiding risky behaviors, and using proper techniques. For example, neuromuscular training programs that focus on improving balance and proprioception can help individuals avoid falls and awkward landings, thereby reducing the risk of contusions. Additionally, adhering to safety guidelines and protocols, such as those recommended for preventing anterior cruciate ligament injuries, can further minimize the risk of injury. By exercising caution and being mindful of potential hazards, individuals can significantly reduce their risk of contusions.
5. Safe Driving Practices
Safe driving practices are essential for preventing contusions and other injuries resulting from vehicular accidents. This includes wearing seat belts, adhering to speed limits, avoiding distractions, and not driving under the influence of alcohol or drugs. Implementing these practices can significantly reduce the risk of collisions and the severity of injuries sustained. While the provided research does not directly address safe driving practices, the principles of injury prevention, such as using protective equipment and exercising caution, are applicable in the context of driving as well. Adopting safe driving habits is crucial for minimizing the risk of contusions and other injuries.
6. Proper Technique and Training
Using proper technique and undergoing appropriate training are critical for preventing contusions and other injuries. Training programs that focus on correct movement patterns, strength, and flexibility can help reduce the risk of injury. For instance, ACL injury-prevention programs that include feedback on movement techniques have been shown to improve neuromuscular control and lower extremity biomechanics, thereby reducing injury risk. Additionally, training interventions that emphasize balance and coordination can help prevent falls and related injuries. Ensuring that individuals are trained in proper techniques can significantly lower the risk of contusions and other injuries.
7. Maintain a Safe Environment
Maintaining a safe environment is crucial for preventing contusions and other injuries. This involves ensuring that physical activity areas are free of hazards, well-lit, and properly maintained. For example, providing integrated foot care and appropriate footwear for diabetic patients can help prevent foot ulcers by creating a safer walking environment. Similarly, modifying training environments to reduce the risk of overuse injuries in runners and military personnel can contribute to a safer exercise setting. By maintaining a safe environment, the risk of contusions and other injuries can be significantly reduced.
8. Improve Balance and Coordination to Avoid Falls
Improving balance and coordination is essential for preventing falls and related contusions. Balance training and neuromuscular exercises can enhance proprioception and stability, reducing the likelihood of falls. Studies have shown that balance training alone can significantly reduce the risk of ankle sprain injuries. Additionally, multicomponent injury-prevention programs that include balance exercises have been effective in reducing lower limb injuries. By focusing on exercises that improve balance and coordination, individuals can enhance their stability and reduce the risk of falls and contusions.
When to Seek Medical Help
Signs that a Contusion May Be More Serious
A contusion can sometimes lead to severe complications such as deep tissue damage or compartment syndrome. Deep tissue damage is often indicated by persistent pain, swelling, and bruising that do not improve over time. Compartment syndrome, a potentially devastating condition, occurs when the pressure within a muscle compartment rises to a level that decreases blood flow, leading to muscle and nerve damage. Symptoms include severe pain, numbness, and decreased range of motion. Immediate medical intervention, such as fasciotomy, is crucial to prevent permanent damage. Recognizing these signs early and seeking prompt medical help can significantly improve outcomes.
Explanation of Underlying Conditions that Could Worsen a Contusion
Certain underlying conditions can exacerbate the severity of a contusion. Blood clotting disorders, for instance, can lead to excessive bleeding and prolonged healing times. Conditions like hemophilia or the use of anticoagulant medications can increase the risk of hemorrhagic progression of a contusion (HPC), where the initial injury worsens due to continued bleeding. Additionally, microvascular alterations, such as those seen in diabetes or hypertension, can impair blood flow and tissue repair, leading to more severe outcomes. Understanding these risks is essential for managing contusions effectively and preventing complications.
FAQs
1. Can a contusion lead to long-term complications?
While most contusions heal without long-term effects, severe contusions, especially those affecting internal organs, muscles, or the brain, can lead to complications like compartment syndrome, scarring, or chronic pain. Cerebral contusions, in particular, may result in long-term neurological issues.
2. How can I differentiate between a bruise and a more severe contusion?
A typical bruise may present with minor pain and discoloration but resolves within a few days. In contrast, a severe contusion involves significant swelling, persistent pain, loss of function, or deeper tissue damage, and it may take weeks to heal. If symptoms worsen or persist, medical attention is needed.
3. Can I still exercise with a muscle contusion?
It’s important to rest the affected area initially to avoid further injury. Light activity may be resumed after swelling and pain decrease, but it’s best to consult a healthcare professional or physical therapist to ensure safe recovery and avoid complications like myositis ossificans.
4. Is there a way to speed up the healing process of a contusion?
The R.I.C.E. method (Rest, Ice, Compression, Elevation) is effective for speeding up healing. Additionally, staying hydrated, eating a balanced diet rich in vitamins (like vitamin C and K), and avoiding activities that might aggravate the injury can help.
5. How do I prevent complications such as infection in contusions?
Although infections are rare in simple contusions since the skin is typically not broken, secondary issues like hematoma (a collection of blood under the skin) or deep tissue damage may pose risks. Keep an eye on increasing pain, swelling, or warmth, which may indicate infection or other complications.
6. Can a contusion cause permanent damage?
In rare cases, contusions, especially those affecting organs like the brain or heart, can cause permanent damage. Cerebral contusions, if untreated, may lead to cognitive issues, seizures, or other neurological problems. Always seek medical attention if contusions affect critical organs.
7. What role does age play in the recovery from a contusion?
Older individuals may experience slower healing and a higher risk of complications, such as deeper tissue damage or reduced circulation. Younger people often heal faster, but those involved in high-impact sports or activities are also more prone to severe injuries.
8. Are there any supplements or nutrients that help heal contusions faster?
Supplements rich in vitamin C, zinc, and amino acids (like L-arginine) may help promote tissue repair and reduce inflammation. However, it’s essential to consult with a healthcare provider before starting any supplement regimen.
9. Can massage therapy help with contusions?
After the acute phase of injury (once swelling subsides), gentle massage therapy may help improve circulation and reduce stiffness. However, it should be done by a professional to avoid aggravating the injury.
10. How long does it take for a bone contusion to heal compared to other types of contusions?
Bone contusions tend to heal more slowly, sometimes taking several months, depending on the severity and location. In contrast, muscle and skin contusions usually heal within a few weeks with proper care.