Clostridium botulinum is a gram-positive, rod-shaped, anaerobic bacterium that produces one of the most potent neurotoxins known to science: botulinum toxin. This bacterium is found naturally in soil and aquatic environments and is responsible for causing botulism, a rare but serious illness that affects the nervous system. C. botulinum is particularly notable for its ability to form highly resistant spores that can survive in extreme conditions, making it a significant concern in food safety. The toxin produced by C. botulinum, commonly known as Botox, has gained widespread recognition for its therapeutic and cosmetic applications. In medical settings, botulinum toxin is used to treat various conditions, including muscle spasms, excessive sweating, and chronic migraines, while in cosmetic procedures, it is employed to reduce the appearance of facial wrinkles.
Characteristics of Clostridium botulinum
Clostridium botulinum is a bacterium known for its significant impact on food safety and human health. It possesses several unique characteristics that contribute to its pathogenicity and resilience. Below are some of the key features of Clostridium botulinum:
1. Anaerobic Nature
Clostridium botulinum is a Gram-positive, anaerobic bacterium that thrives in environments devoid of oxygen. This characteristic is crucial for its survival and pathogenicity. The bacterium is ubiquitously distributed in soils and aquatic sediments, where anaerobic conditions are often created by the decomposition of organic matter such as plants, algae, and animals. In modern food processing, the anaerobic nature of C. botulinum poses significant safety hazards, especially in anaerobic packaging and extended shelf-life products, as these conditions favor the growth and toxin production of the bacterium. The ability to grow in anaerobic environments allows C. botulinum to colonize various niches, including the intestinal tracts of animals and humans, leading to severe diseases like botulism.
2. Spore-Forming Capabilities
Clostridium botulinum is a spore-forming bacterium, which significantly contributes to its persistence and resilience in various environments. The spores are highly resistant to adverse conditions, including heat and desiccation, allowing the bacterium to survive in harsh environments until favorable conditions for growth return. The sporulation process is tightly linked to toxin production, with both processes being regulated by the Spo0A regulator. This dual capability ensures that C. botulinum can remain dormant for extended periods and then rapidly germinate and proliferate when conditions become suitable, such as in nutrient-rich environments or anaerobic food packaging. The spore-forming ability also complicates efforts to eradicate the bacterium from contaminated environments, necessitating stringent control measures in food processing and storage.
3. Toxin Production
Clostridium botulinum is renowned for producing botulinum neurotoxin (BoNT), the most potent toxin known, which causes botulism, a life-threatening paralytic illness 4. The production of BoNT is regulated by complex genetic and environmental factors, including the Spo0A regulator, which also controls sporulation. The toxin is produced during the late exponential and early stationary phases of bacterial growth, and its synthesis is influenced by various environmental and nutritional factors. BoNT production is not only a key determinant of the bacterium’s pathogenicity but also has significant clinical applications, such as in the treatment of muscle disorders and cosmetic procedures. The genetic diversity among C. botulinum strains, including variations in BoNT gene clusters, further complicates the understanding and control of toxin production.
Classification of Clostridium botulinum
Clostridium botulinum is a bacterium that is classified based on various criteria, including its morphology, genetic makeup, and toxin production. Understanding its classification helps in identifying its different strains and their respective characteristics. Below are the key classifications of Clostridium botulinum:
1. Type A
Clostridium botulinum Type A is a proteolytic strain, meaning it can break down proteins, which is a characteristic shared with all known Type A strains. This type is often associated with foodborne botulism outbreaks due to its ability to produce highly potent neurotoxins. The genetic organization of Type A strains shows synteny among proteolytic strains, indicating a conserved genomic structure. Detection methods such as polymerase chain reaction have been developed to identify Type A neurotoxin genes rapidly and specifically, which is crucial for public health monitoring and outbreak response. The presence of insertion sequence elements and recombinases in Type A strains suggests a history of horizontal gene transfer, contributing to its genetic diversity and adaptability.
2. Type B
Clostridium botulinum Type B includes both proteolytic and nonproteolytic strains, making it unique among the botulinum neurotoxin-producing clostridia. This type is also implicated in human botulism and can be detected using various PCR-based methods designed to identify its specific neurotoxin genes. The genomic organization of Type B strains reveals significant recombination events, including the integration of other toxin genes, which may enhance its virulence and adaptability. Environmental surveys have shown the presence of Type B in various sediments, indicating its widespread distribution and potential for causing outbreaks. The genetic diversity within Type B strains is further highlighted by their varying susceptibility to mitomycin C and the presence of bacteriophages.
3. Type E
Clostridium botulinum Type E is a nonproteolytic strain, which means it cannot break down proteins and requires external activation for its toxins. This type is commonly found in aquatic environments and is often associated with botulism cases linked to fish and marine products. The bont/e gene cluster in Type E strains is typically located due to insertion events, which split recombination-associated genes, indicating a complex evolutionary history. Detection methods such as multiplex PCR and GeneDisc Cycler have been developed to identify Type E neurotoxin genes with high sensitivity and specificity, aiding in the rapid diagnosis of botulism. The genetic relationship of Type E with other saccharolytic clostridia suggests it forms a distinct phylogenetic group, separate from proteolytic strains.
4. Type F
Clostridium botulinum Type F includes both proteolytic and nonproteolytic strains, similar to Type B. This type is less commonly associated with human botulism but still poses a significant health risk. The genomic organization of Type F strains shows homology with other botulinum toxin genes, indicating a history of recombination and horizontal gene transfer. Detection methods such as PCR and GeneDisc Cycler have been optimized to identify Type F neurotoxin genes, ensuring accurate and rapid diagnosis. The phylogenetic analysis reveals that proteolytic Type F is genetically distinct from saccharolytic strains, highlighting the diversity within the C. botulinum species. The presence of bacteriophages in Type F strains further underscores their genetic complexity and potential for horizontal gene transfer.
Common sources of Clostridium botulinum
Clostridium botulinum is commonly found in environments where oxygen is limited, making certain foods and conditions particularly susceptible to contamination. Identifying these sources is crucial for preventing botulism outbreaks. Below are some common sources of Clostridium botulinum:
1. Soil and Marine Sediments
Clostridium botulinum is ubiquitously found in soil and marine sediments. These environments provide the anaerobic conditions necessary for the bacteria to thrive and produce spores. Decomposition of organic matter such as plants, algae, and animals creates ideal conditions for the growth of C. botulinum. The bacteria can then enter food webs, leading to potential intoxication of animals and humans. The spores are highly robust and can persist in these environments for extended periods, creating a reservoir that can contaminate food sources.
2. Home-Canned Foods
Home-canned foods are a common source of Clostridium botulinum. The bacteria thrive in anaerobic conditions, which are often created during the canning process if not done correctly. Inadequate sterilization can lead to the survival of C. botulinum spores, which can then produce toxins in the sealed environment of the canned food. This is a significant risk factor for food-borne botulism, as the toxin can cause severe illness or even death if ingested.
3. Improperly Preserved or Fermented Foods
Improperly preserved or fermented foods are another significant source of Clostridium botulinum. The bacteria can grow and produce toxins in anaerobic conditions, which are often present in improperly preserved foods. This includes foods that have not been adequately sterilized or fermented under controlled conditions. The risk is particularly high in homemade or artisanal products where standardized safety measures may not be strictly followed.
4. Seafood, Including Canned Tuna
Seafood, including canned tuna, is a known source of Clostridium botulinum. The bacteria can be present in marine sediments and can contaminate seafood during harvesting and processing. If the seafood is not properly handled or preserved, C. botulinum can grow and produce toxins. This is particularly a concern in canned seafood, where the anaerobic conditions can facilitate the growth of the bacteria if the canning process is not adequately controlled.
5. Honey
Honey is a well-documented source of Clostridium botulinum, particularly for infants. The bacteria can be present in the environment and contaminate honey during production. Infants under one year old are especially susceptible to botulism from honey because their intestinal flora is not fully developed, allowing the bacteria to grow and produce toxins in their gut. This form of botulism, known as intestinal botulism, can be life-threatening and is a significant public health concern.
6. Baked Potatoes Wrapped in Aluminum Foil
Baked potatoes wrapped in aluminum foil can create an anaerobic environment conducive to the growth of Clostridium botulinum. If the potatoes are not kept hot after baking or are left at room temperature for extended periods, the bacteria can grow and produce toxins. This risk is particularly high in food service settings where large quantities of baked potatoes may be prepared in advance and improperly stored.
7. Commercially Prepared Foods
Commercially prepared foods can also be a source of Clostridium botulinum if proper food safety protocols are not followed. This includes foods that are inadequately sterilized, improperly stored, or contaminated during processing. The risk is particularly high in mass-produced foodstuffs where a single contamination event can affect a large number of products, leading to widespread outbreaks of food-borne botulism.
8. Fruits and Vegetables
Fruits and vegetables can be contaminated with Clostridium botulinum spores from soil. This is particularly a concern for raw or minimally processed produce. In a study of raw carrots and green beans used in the French canning industry, botulinum neurotoxin-producing Clostridia spores were detected, highlighting the potential for contamination in fresh produce. Proper washing and preparation can reduce but not entirely eliminate this risk.
9. Animal Intestinal Tracts
Clostridium botulinum can also be found in the intestinal tracts of animals. The bacteria can be ingested by animals from contaminated soil or water and then proliferate in their intestines. This can lead to contamination of meat products if proper hygiene and food safety practices are not followed during slaughter and processing. The presence of C. botulinum in animal intestines underscores the importance of stringent food safety measures in the meat industry.
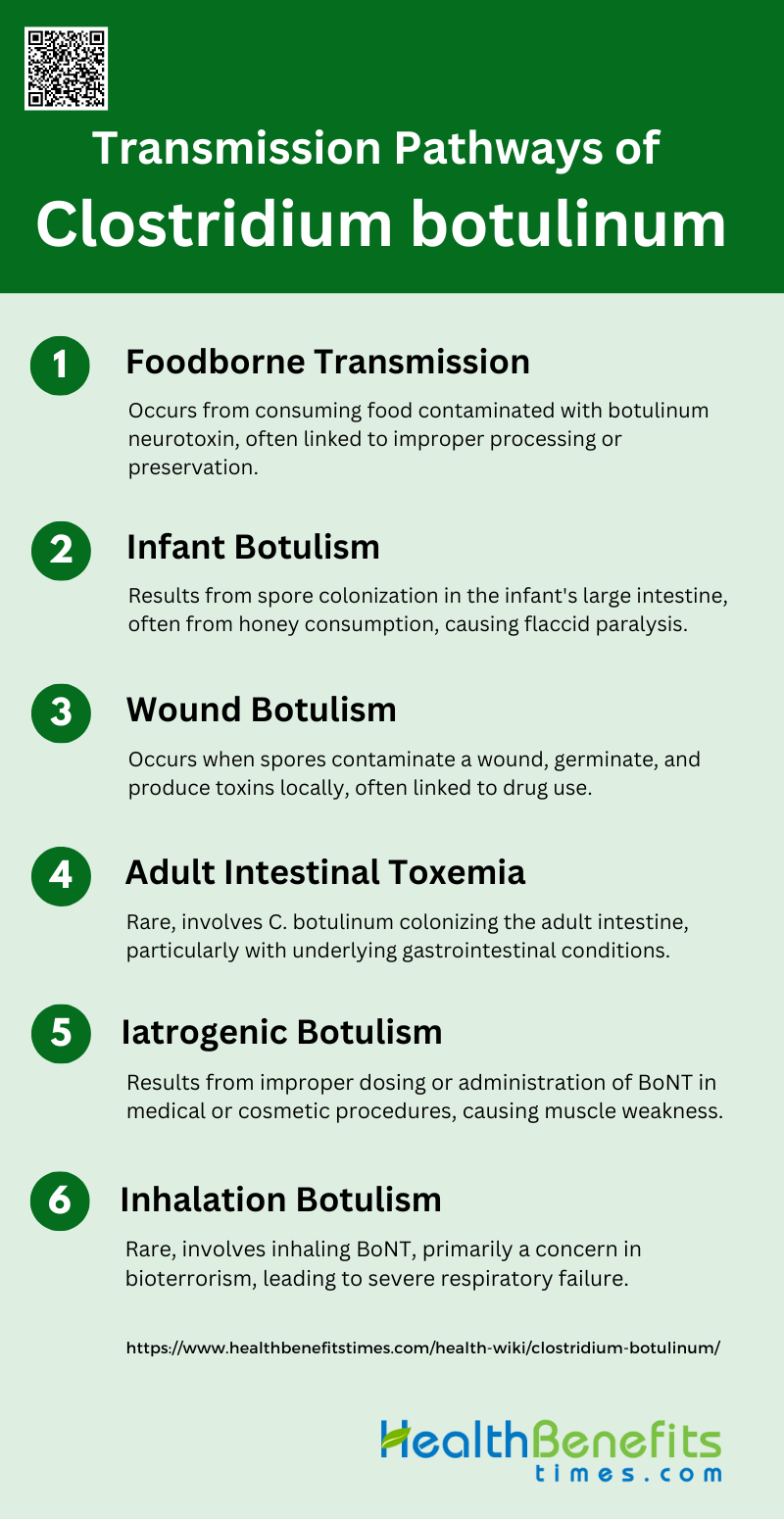
Transmission pathways of Clostridium botulinum
Clostridium botulinum can be transmitted through various pathways, each posing significant health risks if not properly managed. Understanding these pathways is essential for effective prevention and control measures. Below are the primary transmission pathways of Clostridium botulinum:
1. Foodborne Transmission
Foodborne botulism occurs when individuals consume food contaminated with preformed botulinum neurotoxin (BoNT). This form of botulism is often linked to improperly processed or preserved foods where C. botulinum spores can germinate and produce the toxin. The neurotoxin, once ingested, leads to a descending flaccid paralysis by inhibiting neurotransmitter release at neuromuscular junctions. The genetic diversity of C. botulinum strains associated with foodborne botulism has been extensively studied, revealing various neurotoxin subtypes and their epidemiological links to outbreaks. Preventive measures include proper food handling, preservation, and cooking techniques to inactivate the spores and toxin.
2. Infant Botulism
Infant botulism results from the colonization of the infant’s large intestine by C. botulinum spores, which then germinate and produce BoNT in situ. This condition is often misdiagnosed initially as sepsis or meningitis due to its presentation with flaccid paralysis. The disease is particularly associated with honey consumption in infants under one year of age, as honey can contain C. botulinum spores. Treatment typically involves the administration of human botulism immune globulin (BIG-IV) to neutralize the toxin. The genetic diversity of strains causing infant botulism has been characterized, showing significant variability and horizontal gene transfer among strains.
3. Wound Botulism
Wound botulism occurs when C. botulinum spores contaminate a wound, germinate, and produce BoNT locally. This form of botulism is often associated with traumatic injuries or intravenous drug use, where the anaerobic conditions of the wound facilitate bacterial growth. The clinical presentation includes localized infection symptoms followed by systemic flaccid paralysis. Diagnosis is confirmed by detecting BoNT in serum or isolating the bacteria from the wound. Treatment involves wound debridement, administration of antitoxin, and supportive care. Genetic studies have shown that strains causing wound botulism are closely related to those causing foodborne and infant botulism.
4. Adult Intestinal Toxemia
Adult intestinal toxemia botulism, also known as adult intestinal colonization botulism, occurs when C. botulinum colonizes the adult intestine and produces BoNT in situ. This rare form of botulism is often associated with underlying gastrointestinal abnormalities, previous surgeries, or conditions like Crohn’s disease. The clinical presentation is similar to other forms of botulism, with flaccid paralysis being a key symptom. Diagnosis involves detecting BoNT in serum or stool and isolating neurotoxigenic clostridia from stool samples. The condition is underreported due to its rarity and the difficulty in diagnosis.
5. Iatrogenic Botulism
Iatrogenic botulism results from the medical or cosmetic use of BoNT. While BoNT is widely used to treat conditions involving muscle overactivity and in cosmetic procedures to reduce wrinkles, improper dosing or administration can lead to botulism. Symptoms include muscle weakness and paralysis, similar to other forms of botulism. The risk of iatrogenic botulism underscores the importance of proper training and adherence to dosing guidelines in medical and cosmetic practices. Regulatory networks controlling BoNT synthesis in C. botulinum are complex, and understanding these can help mitigate risks associated with its therapeutic use.
6. Inhalation Botulism
Inhalation botulism is a rare form of botulism that occurs when BoNT is inhaled. This form is primarily of concern in the context of bioterrorism, as BoNT is one of the most potent toxins known. The clinical presentation includes respiratory failure and flaccid paralysis, similar to other forms of botulism. Diagnosis and treatment are challenging due to the rapid onset and severity of symptoms. Preventive measures include strict control and monitoring of BoNT production and handling, especially in research and industrial settings. The genetic and physiological variability of C. botulinum strains can impact the risk and management of inhalation botulism.
Symptoms of Clostridium Botulinum
Clostridium botulinum produces a potent neurotoxin that leads to a range of symptoms. These symptoms typically manifest 12 to 72 hours after ingestion of contaminated food. Below is a list of symptoms of clostridium botulinum:
- Muscle weakness, typically starting in the face and head and progressing downward
- Drooping eyelids
- Blurred or double vision
- Difficulty swallowing (dysphagia)
- Slurred speech
- Dry mouth
- Difficulty breathing
- Facial weakness
- Paralysis that spreads down the body
Other symptoms may include
- Nausea and vomiting (in foodborne botulism)
- Abdominal cramps and diarrhea (in foodborne botulism)
- Constipation (especially in infant botulism)
- Fatigue/weakness
- Dizziness
- Difficulty moving eyes
Diagnostic methods of Clostridium Botulinum
Diagnosing Clostridium botulinum infection requires a combination of clinical and laboratory approaches to ensure accurate identification and treatment. These methods help in confirming the presence of the bacteria and its toxins. Below are the primary diagnostic methods for Clostridium botulinum:
1. Laboratory Tests
Laboratory tests for diagnosing Clostridium botulinum infections are crucial due to the difficulty in clinical diagnosis based solely on symptoms. One of the primary methods involves the detection of botulinum neurotoxins in various samples such as serum, gastrointestinal contents, and tissues. Techniques like multiplex real-time PCR SYBR Green have been developed to detect and type C. botulinum, showing high selectivity, accuracy, and sensitivity. Another advanced method is micro-drop digital PCR (ddPCR), which offers higher sensitivity compared to traditional q-PCR, making it particularly useful for detecting low levels of the pathogen in clinical samples. Additionally, the mouse lethality assay remains a standard for neurotoxin detection, although it is time-consuming and requires specialized facilities. Immunofluorescence techniques have also been explored for rapid identification, although they are less commonly used due to the complexity of the procedures.
2. Clinical Evaluation
Clinical evaluation of botulism involves recognizing characteristic symptoms such as acute flaccid paralysis, cranial nerve involvement, and gastrointestinal issues like difficult defecation. These symptoms are often observed in cases of infant botulism, where detailed clinical histories and physical examinations are essential for diagnosis. Electromyograms can also aid in the clinical evaluation by showing reduced action potential amplitudes in motor nerves, which is indicative of botulism2. Despite these clinical signs, laboratory confirmation is often necessary to definitively diagnose botulism. The combination of clinical symptoms and laboratory tests, such as the detection of botulinum toxin in fecal samples and the isolation of C. botulinum from cultures, provides a comprehensive approach to diagnosing this potentially fatal condition.
Treatment options of Clostridium Botulinum
Treating Clostridium botulinum infection involves a multifaceted approach to neutralize the toxin and support the patient’s recovery. Early intervention is crucial for effective management. Below are the primary treatment options for Clostridium botulinum:
1. Botulinum Antitoxin
Botulinum antitoxin is a critical treatment for botulism, aimed at neutralizing the botulinum neurotoxin produced by Clostridium botulinum. Early administration of antitoxin is essential as it can limit the extent of paralysis, although it does not reverse existing paralysis. Various forms of antitoxin, including trivalent, pentavalent, and heptavalent, are used depending on the type of botulinum toxin involved. Studies have shown that timely administration of antitoxin significantly reduces mortality and the duration of hospitalization, mechanical ventilation, and tube or parenteral feeding. Despite its effectiveness, the role of antitoxin in treating inhaled botulism remains unproven.
2. Supportive Care
Supportive care is fundamental in the management of botulism, focusing on maintaining vital functions and preventing complications. This includes intensive care measures such as monitoring respiratory function, providing mechanical ventilation if necessary, and ensuring adequate nutrition and hydration. Supportive care also involves managing secondary infections and other complications that may arise during the course of the illness. The effectiveness of supportive care is well-documented, with studies highlighting its role in reducing mortality and improving patient outcomes.
3. Wound Care
Wound botulism requires specific wound care to eliminate the source of infection. This involves surgical debridement to remove necrotic tissue and drainage of abscesses, combined with antimicrobial therapy to control bacterial growth. Prompt administration of botulinum antitoxin is also crucial in these cases. Studies have shown that early wound care and antitoxin administration can significantly reduce the need for prolonged mechanical ventilation and improve recovery times. The management of wound botulism in injection drug users, who are at higher risk, underscores the importance of coordinated public health efforts to prevent outbreaks.
4. Gastrointestinal Decontamination
Gastrointestinal decontamination is a key treatment strategy for foodborne botulism, aimed at reducing the absorption of the toxin. This can be achieved through the administration of activated charcoal or gastric lavage, especially if the patient presents within a few hours of toxin ingestion. The goal is to remove as much of the ingested toxin as possible before it can be absorbed into the bloodstream. While the effectiveness of gastrointestinal decontamination varies, it is an important adjunctive treatment alongside antitoxin administration and supportive care.
5. Respiratory Support
Respiratory support is often necessary in severe cases of botulism due to the toxin’s effect on the neuromuscular junction, leading to respiratory muscle paralysis. Mechanical ventilation is the mainstay of respiratory support, and its timely initiation is critical for patient survival. Studies have shown that the duration of mechanical ventilation can be significantly reduced with early administration of botulinum antitoxin. Continuous monitoring and supportive care in an intensive care unit are essential to manage respiratory function and prevent complications.
6. Psychosocial Support
Psychosocial support is an important aspect of the comprehensive care for patients recovering from botulism. The prolonged hospitalization and recovery period can be mentally and emotionally challenging for patients and their families. Providing psychological counseling, social support, and rehabilitation services can help address the emotional and mental health needs of patients. This holistic approach to care ensures that patients receive not only medical treatment but also the necessary support to cope with the psychological impact of the illness.
7. Symptom Management
Symptom management in botulism involves addressing the various neurological and muscular symptoms caused by the toxin. This includes managing pain, muscle weakness, and other neuromuscular symptoms through physical therapy, medications, and other supportive measures. Early and effective symptom management can improve patient outcomes and reduce the duration of hospitalization and rehabilitation. Comprehensive care plans that include symptom management are essential for the recovery and rehabilitation of patients with botulism.
Preventive measures of Clostridium Botulinum
Preventing Clostridium botulinum infection involves implementing various strategies to inhibit bacterial growth and toxin production. These measures are essential for ensuring food safety and public health. Below are the primary preventive measures for Clostridium botulinum:
1. Safe Home Canning Practices
To prevent Clostridium botulinum contamination in home-canned foods, it is crucial to follow safe canning practices. Using a pressure canner is essential for low-acid foods, as it reaches temperatures high enough to destroy botulinum spores. Ensuring jars, lids, and utensils are sterilized before use can further reduce the risk. Additionally, following tested recipes from reliable sources can help maintain the correct acidity and processing times needed to prevent bacterial growth.
2. Food Storage and Handling
Proper food storage and handling are vital to prevent the growth of Clostridium botulinum. Foods should be stored at appropriate temperatures; for instance, perishable items should be refrigerated at or below 40°F. Avoid storing food in damaged or bulging cans, as these may indicate contamination. When handling food, ensure that surfaces and utensils are clean, and avoid cross-contamination by keeping raw and cooked foods separate.
3. Commercial Food Safety
In commercial settings, maintaining stringent food safety standards is crucial to prevent Clostridium botulinum outbreaks. This includes using pasteurization and sterilization processes to eliminate spores in food products. Regular testing and monitoring for botulinum toxins in food products can help identify potential contamination. Implementing Hazard Analysis and Critical Control Points (HACCP) plans can ensure that critical points in food production are controlled to prevent bacterial growth.
4. Infant Safety
Infant botulism is primarily caused by ingesting Clostridium botulinum spores, often found in honey. To prevent this, avoid giving honey to infants under 12 months old. Breastfeeding can provide antibodies that help protect against infections. Ensure that infant food is prepared and stored safely, avoiding any homemade or untested food products that may harbor spores. Awareness and education about the risks of botulism in infants are essential for prevention.
5. Home Food Preparation
When preparing food at home, it is important to follow safe practices to prevent Clostridium botulinum contamination. This includes cooking foods to the appropriate temperatures to kill any potential spores. Avoid leaving perishable foods at room temperature for extended periods. Use clean utensils and surfaces to prevent cross-contamination, and ensure that leftovers are stored properly in the refrigerator or freezer to inhibit bacterial growth.
6. Wound Care
Proper wound care is essential to prevent wound botulism, which can occur if Clostridium botulinum spores enter a wound. Clean wounds thoroughly with soap and water, and cover them with sterile bandages to prevent infection. Seek medical attention for deep or contaminated wounds. Avoid injecting drugs, especially with non-sterile needles, as this can introduce spores into the body, increasing the risk of wound botulism.
7. Practice Good Hand Hygiene
Good hand hygiene is a fundamental practice to prevent the spread of Clostridium botulinum and other pathogens. Wash hands thoroughly with soap and water, especially before handling food and after using the restroom. Hand sanitizers can be used when soap and water are unavailable, but they are not effective against spores. Regular handwashing can significantly reduce the risk of contamination and transmission of bacteria.
FAQs
1. Can Clostridium botulinum be transmitted from person to person?
No, Clostridium botulinum is not contagious and cannot be transmitted directly from person to person. Botulism is usually caused by ingestion of contaminated food, wound contamination, or, in rare cases, inhalation.
2. What should I do if I suspect a case of botulism?
If you suspect botulism, seek immediate medical attention. Botulism is a medical emergency that requires prompt treatment, which may include administration of antitoxin and supportive care in a hospital setting.
3. How can I tell if canned food is contaminated with Clostridium botulinum?
Signs that canned food might be contaminated with Clostridium botulinum include bulging or leaking cans, an off smell, or spurting liquid when the can is opened. Discard any food from cans that show these signs without tasting it, as botulinum toxin can be extremely dangerous even in small amounts.
4. Is botulinum toxin destroyed by cooking?
Botulinum toxin can be destroyed by boiling food for at least 10 minutes. However, the spores of Clostridium botulinum are highly resistant to heat and require temperatures above 120°C (248°F), typically achieved only in pressure canning, to be effectively killed.
5. Can botulinum toxin survive in acidic foods?
Clostridium botulinum does not grow well in acidic environments (with a pH below 4.6). Foods that are naturally acidic or acidified (like pickles or tomatoes with added vinegar) are less likely to support the growth of the bacteria and production of its toxin.
6. What are some common misconceptions about Clostridium botulinum and botulism?
Common misconceptions include the belief that botulism can be spread through the air under normal conditions (it cannot, except in rare inhalation cases) and that all cases of botulism are linked to home-canned foods (botulism can also result from commercially prepared foods, wounds, or infant exposure to honey).
7. How long does it take to recover from botulism?
Recovery time from botulism can vary widely depending on the severity of the symptoms, the speed of diagnosis and treatment, and the individual’s overall health. Some patients may recover in a few weeks, while others may require months of intensive care and rehabilitation.
8. Can I use botulinum antitoxin at home if I suspect botulism?
No, botulinum antitoxin is a prescription medication that must be administered by healthcare professionals. It is not available for home use and must be given in a medical setting to monitor for possible side effects and to provide supportive care.
9. Are there any populations at higher risk for botulism?
Infants, people who inject drugs, and individuals consuming improperly home-canned or preserved foods are at higher risk for different types of botulism. Additionally, individuals with gastrointestinal disorders may be more susceptible to rare forms like adult intestinal toxemia botulism.
10. Can Clostridium botulinum spores be killed by freezing food?
Freezing does not kill Clostridium botulinum spores; it only prevents the growth of the bacteria. The spores remain dormant and can become active again if conditions become favorable, such as during thawing and improper handling.