Clinical trials are carefully designed research studies that evaluate the safety and effectiveness of new medical interventions, such as drugs, treatments, or medical devices, in human participants. These trials are essential for advancing medical knowledge and improving patient care by systematically testing potential therapies before they can be approved for widespread use. Clinical trials typically progress through several phases, with each phase designed to answer specific questions about the intervention’s safety, efficacy, and optimal use. They often involve comparing the new intervention to existing treatments or placebos, which are inactive substances used as a control. The results of clinical trials provide crucial evidence that helps healthcare professionals, regulatory agencies, and patients make informed decisions about medical treatments and interventions.
Purpose of Clinical trials
Clinical trials are fundamental to the advancement of medical science and patient care. They serve multiple purposes, from evaluating the safety and efficacy of new treatments to exploring innovative uses for existing therapies. Below are the key purposes of clinical trials:
1. Evaluating Safety and Efficacy
Clinical trials are essential for evaluating the safety and efficacy of new treatments. Phase I trials, for instance, focus on determining the recommended dose and toxicity profile of investigational agents, ensuring that they are safe for further testing. These trials often use dose-escalation methods to identify the maximum tolerated dose while monitoring for adverse effects. The introduction of novel targeted therapies has led to improved response rates and reduced treatment-related deaths, highlighting the importance of these trials in modern oncology. Additionally, phase II trials further assess therapeutic efficacy by monitoring both antitumor activity and toxicity, ensuring a balanced evaluation of new treatments.
2. Advancing Medical Knowledge
Clinical trials play a pivotal role in advancing medical knowledge by providing robust data on the effectiveness and safety of new treatments. They help in understanding the biological mechanisms of diseases and the impact of various interventions. For example, the use of digital technologies in clinical trials has the potential to transform the way data is collected and analyzed, thereby enhancing our understanding of treatment outcomes. Moreover, subgroup analyses in confirmatory trials help in identifying specific patient populations that may benefit more from certain treatments, thereby refining therapeutic strategies and contributing to personalized medicine.
3. Developing New Therapies
The development of new therapies heavily relies on the structured and rigorous process of clinical trials. Early-phase trials are crucial for identifying optimal dosing and safety profiles of new drugs, particularly molecularly targeted agents and immunotherapies. These trials have led to significant improvements in response rates and clinical benefits for patients, as seen in recent studies involving targeted therapies and immunotherapy combinations. By systematically evaluating new treatments, clinical trials ensure that only the most promising therapies advance to later stages of development, ultimately leading to the approval of effective and safe treatments for various diseases.
4. Improving Patient Care
Clinical trials contribute to improving patient care by providing evidence-based data that inform clinical practice. The rigorous assessment of treatment efficacy and safety in clinical trials ensures that new therapies offer real benefits to patients. For instance, the use of standardized response criteria in lymphoma clinical trials has facilitated the evaluation and comparison of different therapies, leading to the rapid availability of improved treatments for patients. Additionally, the integration of biomarkers and personalized approaches in clinical trials has enhanced the precision of treatments, thereby improving patient outcomes and quality of life.
5. Exploring New Uses for Existing Treatments
Clinical trials also explore new uses for existing treatments, expanding their therapeutic potential. For example, phase I oncology trials have shown that using tumor biomarkers as eligibility criteria can significantly improve response rates, suggesting new applications for targeted therapies. Similarly, the rise in placebo responses in rheumatoid arthritis trials highlights the need to reassess existing treatments and their efficacy in different patient populations. By continuously evaluating and re-evaluating treatments through clinical trials, researchers can discover new indications and optimize the use of existing therapies, ultimately benefiting a broader range of patients.
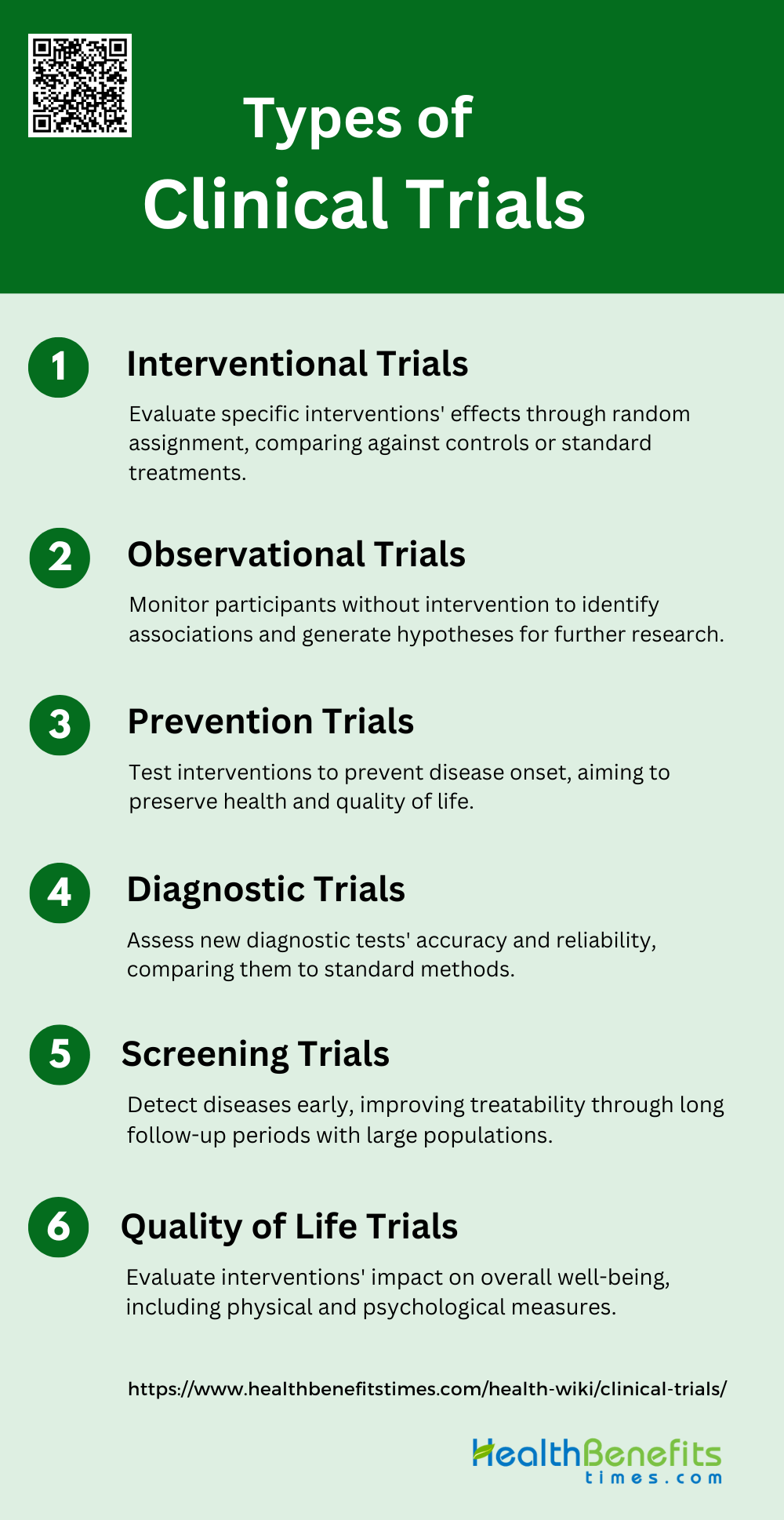
Types of Clinical Trials
Clinical trials come in various forms, each designed to answer specific research questions and address different aspects of medical science. These trials can range from testing new treatments to studying disease prevention methods. Below are the main types of clinical trials:
1. Interventional Trials
Interventional trials are designed to evaluate the effects of a specific intervention on a particular outcome. These trials often involve random assignment of participants to different groups to compare the intervention against a control or standard treatment. For example, the VOICE Randomized Clinical Trial aimed to improve patient-centered communication in advanced cancer patients through a combined intervention involving oncologists, patients, and caregivers. The study found significant improvements in patient-centered communication but did not observe significant changes in secondary outcomes such as quality of life and aggressive treatments. Another example is the ESCAPE trial, which focused on hypertensive patients and demonstrated that a multifaceted intervention targeting general practitioners significantly increased the proportion of patients achieving their therapeutic targets.
2. Observational Trials
Observational trials involve monitoring participants without manipulating the study environment. These trials are useful for identifying associations and generating hypotheses. For instance, the BETTER trial aimed to improve chronic disease prevention and screening in primary care through a practice facilitation intervention. The study found that a Prevention Practitioner could significantly improve the implementation of preventive and screening actions for chronic diseases in a cost-effective manner. Similarly, observational studies have shown links between patient-centered communication and quality of life in advanced cancer patients, although these findings were further validated through interventional trials like the VOICE study.
3. Prevention Trials
Prevention trials are designed to test interventions that aim to prevent the onset of diseases or conditions. The AgeWell.de trial is an example of a prevention trial targeting cognitive decline in older adults. This multi-component trial includes interventions such as nutritional counseling, physical activity, and cognitive training. The study aims to determine whether these interventions can preserve cognitive function and improve quality of life over a two-year follow-up period. Another example is the systematic review on oral health interventions, which found that fluoride supplements and varnishes significantly reduced dental caries in children and adolescents.
4. Diagnostic Trials
Diagnostic trials focus on evaluating the effectiveness of diagnostic tests or procedures. These trials often compare new diagnostic methods against standard ones to determine their accuracy and reliability. For example, a review on screening for hearing loss in adults found that common screening tests could help identify patients at higher risk for hearing loss. However, the study also noted that additional research is needed to understand the effects of screening on health outcomes. Another study on oral health screening in adults found that primary care screening instruments had moderate diagnostic accuracy for periodontal disease.
5. Screening Trials
Screening trials aim to detect diseases or conditions at an early stage when they are more treatable. These trials often involve large populations and long follow-up periods. For instance, a review on screening for hearing loss in adults aged 50 years or older found that screening was associated with increased hearing aid use but did not significantly improve hearing-related function. Another example is a systematic review on oral health screening in children and adolescents, which found that fluoride supplements and varnishes administered in dental or school settings significantly improved caries outcomes.
6. Quality of Life Trials
Quality of life (QoL) trials assess the impact of interventions on the overall well-being of participants. These trials often include both physical and psychological measures. For example, a trial on colorectal cancer patients found that diagnosing QoL deficits and providing tailored therapeutic options significantly improved the proportion of patients with a need for QoL therapy. Another study reviewed the effects of telehealth interventions on cancer survivors‘ quality of life and found that these interventions were effective in improving QoL, particularly for breast cancer survivors. The FICSIT trials also emphasized the importance of assessing QoL in elderly populations to evaluate the effectiveness of various interventions.
Phases of Clinical Trials
Clinical trials are conducted in sequential phases, each with distinct objectives and methodologies. These phases ensure that new treatments are thoroughly tested for safety, efficacy, and optimal usage. Below are the different phases of clinical trials:
1. Phase I
Phase I clinical trials primarily focus on assessing the safety of a new drug or treatment. These trials are conducted with a small group of participants, often healthy volunteers, to evaluate the drug’s pharmacokinetics, toxicity, and maximum tolerated dose. The primary goal is to determine whether the drug is safe for human use and to identify any potential side effects. This phase is crucial as it lays the groundwork for subsequent phases by ensuring that the drug does not pose significant risks to participants. The data collected in Phase I trials help researchers understand how the drug behaves in the human body, which is essential for designing further studies.
2. Phase II
Phase II clinical trials aim to assess the efficacy of the drug and further evaluate its safety. These trials involve a larger group of participants who have the condition that the drug is intended to treat6. The primary objectives are to determine the optimal dosage and to gather preliminary data on the drug’s effectiveness. Phase II trials also continue to monitor for adverse effects, but the focus shifts more towards understanding how well the drug works in treating the disease. This phase often involves hundreds of patients and uses various trial designs to compare the new treatment against a placebo or standard treatment.
3. Phase III
Phase III clinical trials are designed to confirm the findings from Phase I and II trials in a larger and more diverse population. These trials involve thousands of participants and are conducted across multiple sites to ensure that the results are generalizable. The primary goals are to establish the drug’s efficacy, monitor side effects, and compare it to existing treatments. Phase III trials are often randomized and double-blind to minimize bias and provide robust data for regulatory approval. The results from these trials are critical for seeking marketing authorization and are used to inform the drug’s labeling and usage guidelines.
4. Phase IV
Phase IV clinical trials, also known as post-marketing surveillance, occur after a drug has been approved and marketed. These trials aim to monitor the long-term safety and effectiveness of the drug in the general population. They help identify any rare or long-term adverse effects that may not have been apparent in earlier phases. Phase IV trials can also explore new uses for the drug and gather data on its performance in different populations and real-world settings. This phase is essential for ongoing pharmacovigilance and can lead to updates in the drug’s labeling, dosage recommendations, or even regulatory actions if significant safety concerns arise.
Who Participates in Clinical Trials?
Participation in clinical trials is governed by strict inclusion and exclusion criteria to ensure the safety and appropriateness of the study for potential participants. These criteria are designed to identify suitable candidates while minimizing risks and ensuring the reliability of the results. The rights and safety of participants are paramount, with informed consent being a critical component. This process ensures that participants are fully aware of the trial’s nature, potential risks, and benefits before agreeing to take part. Privacy and ethical considerations are also rigorously maintained to protect participants’ personal information and uphold ethical standards. Participants play a crucial role in advancing medical science by contributing to the development of new treatments and interventions, which can lead to improved healthcare outcomes for future patients.
Process of Conducting Clinical Trials
Conducting clinical trials involves a systematic and rigorous process to ensure the validity and reliability of the results. This process includes several key steps, from initial planning to final analysis. Below are the main steps in the process of conducting clinical trials:
1. Preclinical Research
Preclinical research forms the foundation of clinical trials, involving extensive laboratory and animal studies. Scientists conduct experiments to assess the potential therapeutic effects and safety profile of new drugs or treatments. This phase typically includes in vitro studies using cell cultures and in vivo studies on animal models. Researchers evaluate the compound’s pharmacokinetics, pharmacodynamics, and toxicity. The data collected during this stage helps determine appropriate dosing, potential side effects, and overall feasibility for human trials.
2. Designing the Trial
Designing a clinical trial is a complex process that requires careful planning and consideration. Researchers develop detailed protocols outlining the study’s objectives, methodology, participant criteria, and data collection methods. This stage also involves securing funding from various sources, such as pharmaceutical companies, government agencies, or academic institutions. The trial design must balance scientific rigor with ethical considerations and practical feasibility. Researchers often consult with statisticians to ensure the study has sufficient power to detect meaningful results.
3. Regulatory Approval
Before a clinical trial can begin, it must obtain regulatory approval from relevant authorities. In the United States, this primarily involves the Food and Drug Administration (FDA) and Institutional Review Boards (IRBs). The FDA reviews the trial design, preclinical data, and proposed human testing to ensure safety and scientific validity. IRBs, typically associated with research institutions, evaluate the ethical aspects of the trial, focusing on protecting participants’ rights and welfare. This process may involve multiple rounds of review and revisions to address any concerns raised by these regulatory bodies.
4. Recruitment and Enrollment
Participant recruitment and enrollment are crucial steps in conducting clinical trials. Researchers use various methods to identify and attract potential participants, including advertising, referrals from healthcare providers, and patient databases. Strict inclusion and exclusion criteria are applied to ensure the study population accurately represents the target patient group. Informed consent is a critical component of this phase, where potential participants are thoroughly educated about the trial’s purpose, procedures, risks, and benefits before deciding to enroll.
5. Data Collection and Monitoring
Throughout the clinical trial, researchers meticulously collect data on participants’ responses to the intervention. This may involve regular medical examinations, laboratory tests, questionnaires, and other assessment tools. Continuous monitoring of participants’ safety is paramount, with mechanisms in place to detect and address any adverse events promptly. Data safety monitoring boards (DSMBs) often oversee this process, conducting interim analyses to ensure the trial’s ongoing safety and validity. Adherence to Good Clinical Practice (GCP) guidelines is essential to maintain data integrity and participant well-being.
6. Analysis and Reporting
The final stage of a clinical trial involves comprehensive analysis of the collected data and reporting of findings. Statistical experts employ various methods to interpret the results, accounting for factors such as sample size, variability, and potential confounding variables. Researchers prepare detailed reports summarizing the trial’s outcomes, including efficacy, safety, and any unexpected findings. These results are typically published in peer-reviewed scientific journals and presented at medical conferences. The findings may inform future research directions, influence clinical practice guidelines, or support regulatory approval for new treatments.
Importance of Clinical Trials
Clinical trials are vital for the advancement of medical science and the improvement of patient care. They provide the evidence needed to develop new treatments and ensure their safety and efficacy. Below are the key reasons why clinical trials are important:
1. Developing New Treatments
Clinical trials are pivotal in the development of new treatments, serving as the bridge between preclinical research and market approval. They provide a structured environment to test the safety and efficacy of new drugs in humans, which is essential before any new treatment can be made available to the public. The transition from preclinical to clinical stages is a critical turning point in drug development, as it brings the potential new treatment closer to market authorization. Despite the high attrition rates, with less than 10% of drugs entering clinical trials eventually being approved, these trials are indispensable for identifying promising new therapies.
2. Providing Scientific Evidence
Clinical trials are the gold standard for generating scientific evidence on the efficacy and safety of new treatments. They are meticulously designed to provide reliable data that can inform clinical practice and guide treatment decisions. The randomized clinical trial (RCT) is particularly significant, as it offers compelling evidence of a drug’s efficacy, which is crucial for regulatory approval and inclusion in treatment guidelines. The data collected from these trials form the basis of evidence-based medicine, ensuring that new treatments are both safe and effective for patient use.
3. Benefiting Participants
Participants in clinical trials often gain access to cutting-edge treatments before they are available to the general public. This can be particularly beneficial for patients with conditions that have limited treatment options. Additionally, participants receive close monitoring and care from leading medical experts, which can lead to a better understanding of their condition and potentially improved health outcomes. Moreover, participating in a clinical trial allows individuals to play an active role in their healthcare, contributing to the advancement of medical knowledge and potentially benefiting future patients.
4. Advancing Medical Knowledge
Clinical trials are essential for advancing medical knowledge by providing robust data on the effectiveness and safety of new treatments. They help to refine existing therapies and develop new ones, thereby enhancing the overall quality of healthcare. The information gathered from clinical trials is used to update clinical guidelines and inform best practices, ensuring that medical treatments are based on the latest scientific evidence. This continuous cycle of research and application helps to improve patient outcomes and advance the field of medicine.
5. Ensuring Safety and Efficacy
Ensuring the safety and efficacy of new treatments is a primary goal of clinical trials. These trials are designed with rigorous methodologies to minimize risks and maximize benefits for participants. They involve multiple phases, each with specific objectives to assess the drug’s pharmacokinetics, safety, and therapeutic efficacy. Post-marketing surveillance further ensures that any long-term or rare side effects are identified and managed appropriately. This comprehensive approach helps to protect patients and ensure that only safe and effective treatments reach the market.
Key Stakeholders of Clinical trials
Clinical trials involve a diverse group of stakeholders, each playing a crucial role in the successful execution and outcome of the research. These stakeholders ensure that trials are conducted ethically and efficiently. Below are the key stakeholders of clinical trials:
1. Researchers and Sponsors
Researchers and sponsors play a pivotal role in the design, implementation, and funding of clinical trials. They are responsible for ensuring that trials are scientifically sound, ethically conducted, and adequately resourced. Researchers must design trials that address pertinent clinical questions while maintaining rigorous standards to ensure the validity and reliability of the results. Sponsors, often pharmaceutical companies or academic institutions, provide the necessary financial support and resources to conduct these trials. They also have a responsibility to ensure that trials are inclusive and representative of diverse populations, as highlighted by the American Society of Clinical Oncology and the Association of Community Cancer Centers, which emphasize the need for equity, diversity, and inclusion in cancer clinical trials. Additionally, researchers and sponsors must navigate complex regulatory landscapes and address infrastructural barriers to facilitate the smooth conduct of trials.
2. Regulators
Regulators are essential stakeholders in clinical trials, ensuring that trials are conducted in compliance with legal and ethical standards. They are responsible for the approval and oversight of clinical trial protocols, safeguarding participant safety, and ensuring the scientific integrity of the research. Regulatory bodies, such as the European Medicines Agency (EMA), play a crucial role in promoting transparency and public trust in clinical trials by making trial data accessible to the public and researchers. They also work to streamline regulatory processes to reduce administrative burdens and facilitate the efficient conduct of trials. Regulators must balance the need for transparency with the protection of commercially confidential information, ensuring that the interests of both the public and sponsors are safeguarded.
3. Healthcare Professionals
Healthcare professionals, including doctors, nurses, and clinical trial coordinators, are integral to the successful execution of clinical trials. They are responsible for recruiting and enrolling patients, administering treatments, and monitoring patient outcomes. Their clinical expertise ensures that trials are conducted safely and that patient care is prioritized. Healthcare professionals also play a key role in educating patients about the trial process and obtaining informed consent, which is crucial for ethical trial conduct. They must be culturally competent and sensitive to the needs of diverse patient populations to enhance participation and retention in trials. Additionally, healthcare professionals can advocate for greater diversity in clinical trials and work to address barriers that may prevent underrepresented groups from participating.
4. Patients and Advocacy Groups
Patients and advocacy groups are central to the clinical trial ecosystem, providing valuable insights into patient needs and preferences. Patients who participate in clinical trials contribute to the advancement of medical knowledge and the development of new treatments. Advocacy groups work to raise awareness about clinical trials, support patient recruitment, and ensure that patient voices are heard in the research process. They also advocate for policies that promote patient access to trials and post-trial care. Engaging patients and advocacy groups in the design and conduct of trials can lead to more patient-centered research and improve trial outcomes. Furthermore, involving patients in discussions about numerical aspects of trials can enhance transparency and trust in the research process.
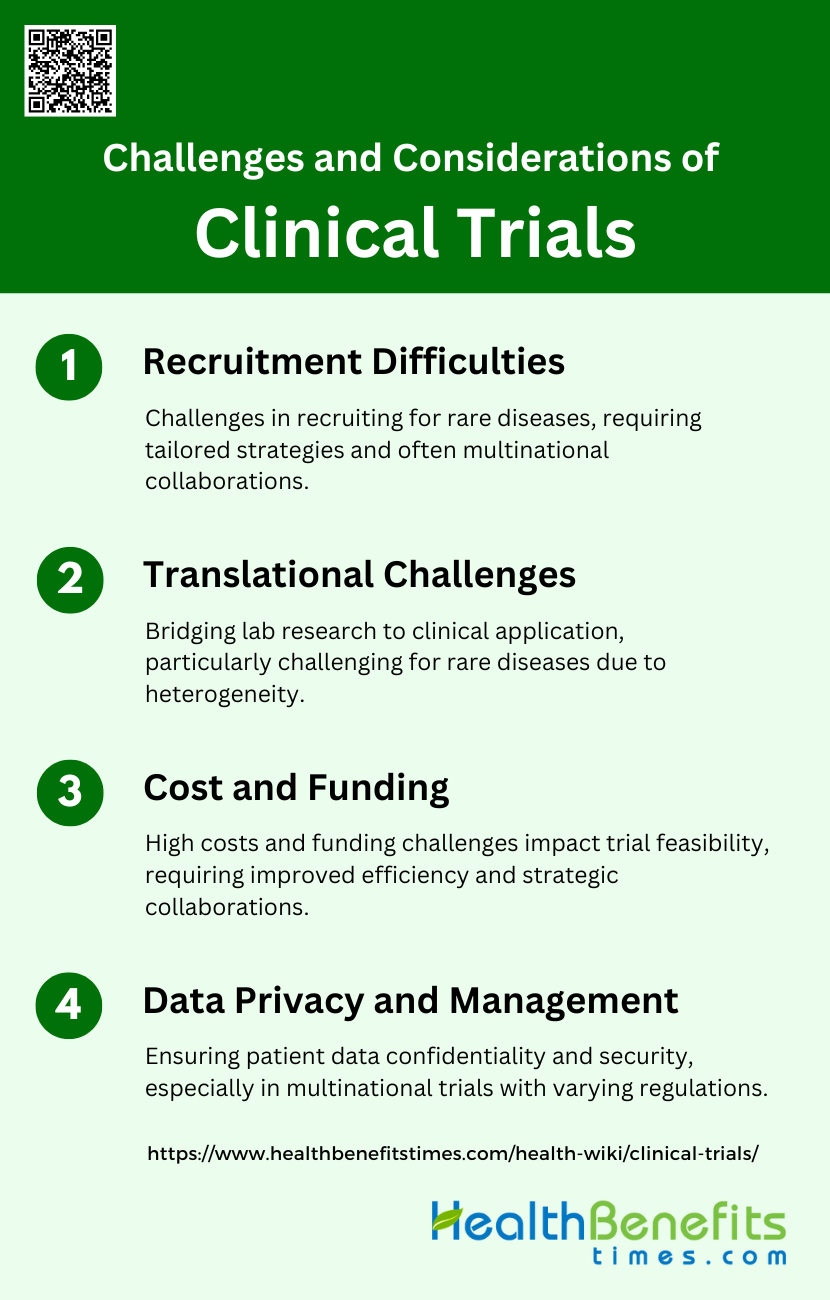
Challenges and Considerations of clinical trial
Conducting clinical trials involves navigating numerous challenges and considerations to ensure their success and integrity. These factors can impact the design, implementation, and outcomes of the trials. Below are the key challenges and considerations of clinical trials:
1. Recruitment Difficulties
Recruitment difficulties are a significant challenge in clinical trials, particularly for rare diseases and small patient populations. Trials often struggle to meet recruitment targets due to the limited number of eligible participants, geographical dispersion, and the burden of trial participation on patients. For instance, rare disease trials frequently require multicenter and multinational collaboration to gather sufficient participants, which complicates protocol harmonization and ethical review processes. Additionally, recruitment strategies must be tailored to specific populations, as demonstrated by studies targeting hard-to-reach groups like gay and bisexual prostate cancer patients or those with sexually transmissible diseases. Online recruitment methods have shown promise in improving recruitment rates and cost-effectiveness compared to traditional methods, although they may have lower conversion rates.
2. Translational Challenges
Translational challenges in clinical trials involve bridging the gap between laboratory research and clinical application. These challenges are particularly pronounced in rare diseases due to the heterogeneity and complexity of these conditions. Selecting meaningful and relevant endpoints is crucial but difficult, as the natural history of many rare diseases is not well understood, and disease mechanisms can vary significantly even within subtypes. Innovative study designs, such as adaptive trials and the use of historical controls, can help address these challenges by allowing for more flexible and efficient trial processes. However, these approaches require robust statistical methods and careful consideration of ethical implications, especially when dealing with small patient populations.
3. Cost and Funding
The high cost of conducting clinical trials is a major barrier, driven by the extensive resources needed for trial activation, patient management, and data collection. Delayed trial activation and poor patient accrual can lead to wasted resources and low-value trials, impacting the feasibility and scope of clinical research. Industry sponsorship can provide necessary funding but may introduce conflicts of interest and affect research integrity. Recommendations to reduce trial costs include improving operational efficiencies, enhancing patient accrual strategies, and increasing transparency in trial reporting. Additionally, clinical trials networks can offer organizational support and facilitate successful research collaborations, ultimately reducing costs and improving trial outcomes.
4. Data Privacy and Management
Data privacy and management are critical considerations in clinical trials, particularly with the increasing use of digital technologies for data collection and patient monitoring. Ensuring the confidentiality and security of patient data is essential to maintain trust and comply with regulatory requirements. Multinational trials face additional challenges due to varying data protection laws and standards across countries. Effective data management strategies include the use of secure, centralized databases, robust data encryption methods, and clear protocols for data access and sharing. Additionally, the integration of patient-reported outcomes (PROs) into clinical trials requires careful consideration of data privacy, as these measures often involve sensitive personal information.
FAQs
1. What is the difference between a clinical trial and an observational study?
Observational studies involve monitoring participants without manipulating the study environment, while clinical trials actively intervene with treatments to test their safety and efficacy.
2. Are there any costs associated with participating in a clinical trial?
Participation in clinical trials is typically free, and some trials may even provide compensation for time and travel. However, it’s important to ask the trial organizers about any potential costs.
3. How do I find clinical trials that I may be eligible for?
You can find clinical trials through websites like ClinicalTrials.gov, by speaking with your healthcare provider, or by contacting medical institutions and advocacy groups.
4. What is a placebo, and why is it used in clinical trials?
A placebo is an inactive substance that has no therapeutic effect. It is used as a control in clinical trials to help determine the true efficacy of the treatment being tested.
5. How is my privacy protected during a clinical trial?
Clinical trials adhere to strict confidentiality rules and regulations to protect your personal information. This includes data encryption, secure databases, and restricted access to sensitive information.
6. Can I leave a clinical trial once I’ve started?
Yes, participants can leave a clinical trial at any time for any reason. Leaving a trial will not affect your future medical care.
7. What should I consider before joining a clinical trial?
Consider factors such as the purpose of the trial, the potential risks and benefits, your eligibility, the commitment required, and how the trial might affect your daily life.
8. How long do clinical trials typically last?
The duration of clinical trials varies depending on the phase and type of trial. Some may last a few months, while others can continue for several years.
9. What happens if a participant experiences side effects during a clinical trial?
Participants are closely monitored for side effects, and appropriate medical care will be provided if adverse effects occur. The trial may be adjusted or stopped to protect participant safety.
10. How do clinical trials address diversity and inclusion among participants?
Clinical trials aim to include diverse populations to ensure that the results are applicable to a wide range of people. Efforts are made to recruit participants from various demographics, but challenges remain in achieving full diversity.