Cataracts are a common eye condition characterized by the clouding of the eye’s natural lens, leading to blurred or dimmed vision. This clouding occurs when proteins in the lens break down and clump together, causing the lens to become less transparent and interfering with the passage of light to the retina. Cataracts typically develop slowly over time and are most commonly associated with aging, although they can also be congenital or caused by other factors such as injury, certain medications, or medical conditions. The condition can affect one or both eyes and may result in symptoms such as difficulty seeing at night, sensitivity to glare, faded color perception, and the need for brighter light when reading or performing other visual tasks. While cataracts are a leading cause of preventable blindness worldwide, they are treatable through surgical intervention, which involves removing the clouded lens and replacing it with an artificial intraocular lens.
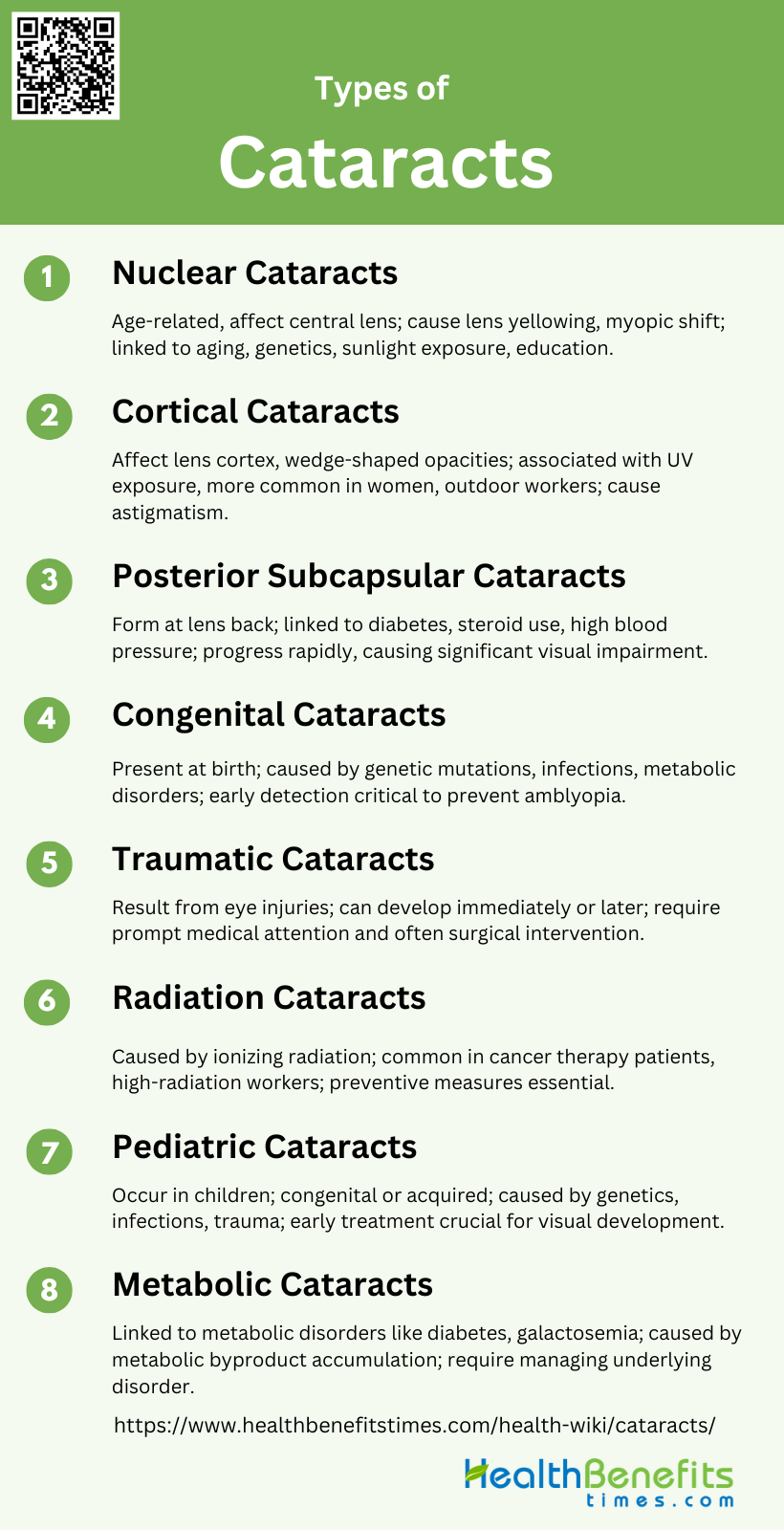
Types of cataracts
Cataracts are a common eye condition that can lead to vision impairment if left untreated. They occur when the lens of the eye becomes cloudy, affecting the passage of light. There are several types of cataracts, each with distinct characteristics and causes. Below is a list of the various types of cataracts:
1. Nuclear Cataracts
Nuclear cataracts are the most common type of age-related cataracts and primarily affect the central zone of the lens, known as the nucleus. They are characterized by a gradual hardening and yellowing of the lens nucleus, which can lead to a significant myopic shift in vision as the cataract progresses. This type of cataract is often associated with aging and has been linked to genetic factors, including common variants in genes related to congenital cataracts and eye development. Studies have shown that nuclear cataracts are more prevalent in older populations and can be influenced by factors such as sunlight exposure and educational status.
2. Cortical Cataracts
Cortical cataracts affect the lens cortex, which is the outer layer surrounding the central nucleus. These cataracts are characterized by white, wedge-like opacities that start in the periphery of the lens and work their way to the center in a spoke-like fashion. Cortical cataracts are often associated with long-term exposure to ultraviolet radiation, making outdoor workers particularly susceptible. They are also more common in women and individuals with lower educational attainment. Unlike nuclear cataracts, cortical cataracts do not typically cause a significant myopic shift but can lead to changes in astigmatism.
3. Posterior Subcapsular Cataracts
Posterior subcapsular cataracts (PSC) form at the back of the lens, directly in the path of light entering the eye, which can cause significant visual impairment, especially in bright light conditions. PSC cataracts are often associated with diabetes, steroid use, and high blood pressure. They tend to progress more rapidly than other types of cataracts and can cause a noticeable myopic shift as they advance. PSC cataracts are also more common in younger individuals compared to nuclear and cortical cataracts.
4. Congenital Cataracts
Congenital cataracts are present at birth and can affect one or both eyes. They can result from genetic mutations, intrauterine infections, or metabolic disorders. The morphology of congenital cataracts can vary widely, including types such as lamellar, nuclear, oil droplet, and cortical cataracts. Early detection and treatment are crucial to prevent amblyopia and ensure proper visual development. Advances in genetic markers have improved the identification and categorization of congenital cataracts, aiding in better management and prognosis.
5. Traumatic Cataracts
Traumatic cataracts result from direct injury to the eye, such as blunt trauma, penetrating injuries, or exposure to intense heat or chemicals. These cataracts can develop immediately after the injury or may appear years later. The morphology of traumatic cataracts can vary, with some presenting as rosette-shaped opacities. Prompt medical attention and surgical intervention are often required to restore vision and prevent further complications.
6. Radiation Cataracts
Radiation cataracts are caused by exposure to ionizing radiation, which can damage the lens fibers and lead to opacification. These cataracts are commonly seen in individuals who have undergone radiation therapy for cancer or those exposed to high levels of radiation in occupational settings. The development of radiation cataracts can be dose-dependent, with higher doses leading to more rapid onset and progression. Preventive measures, such as protective eyewear, are essential for individuals at risk.
7. Pediatric Cataracts
Pediatric cataracts refer to lens opacities that occur in children, either as congenital or acquired conditions. These cataracts can result from genetic factors, metabolic disorders, infections, or trauma. Early diagnosis and treatment are critical to prevent visual impairment and ensure normal visual development. Pediatric cataracts can present in various forms, including lamellar, nuclear, cortical, and posterior subcapsular types. Surgical intervention is often required, followed by visual rehabilitation to optimize outcomes.
8. Metabolic Cataracts
Metabolic cataracts are associated with systemic metabolic disorders, such as diabetes, galactosemia, and hypocalcemia. These cataracts can develop due to the accumulation of metabolic byproducts in the lens, leading to opacification. Diabetic cataracts, for example, are often characterized by posterior subcapsular opacities. Management of the underlying metabolic disorder is crucial to prevent the progression of cataracts and maintain overall eye health. Regular eye examinations are recommended for individuals with metabolic conditions to detect and address cataracts early.
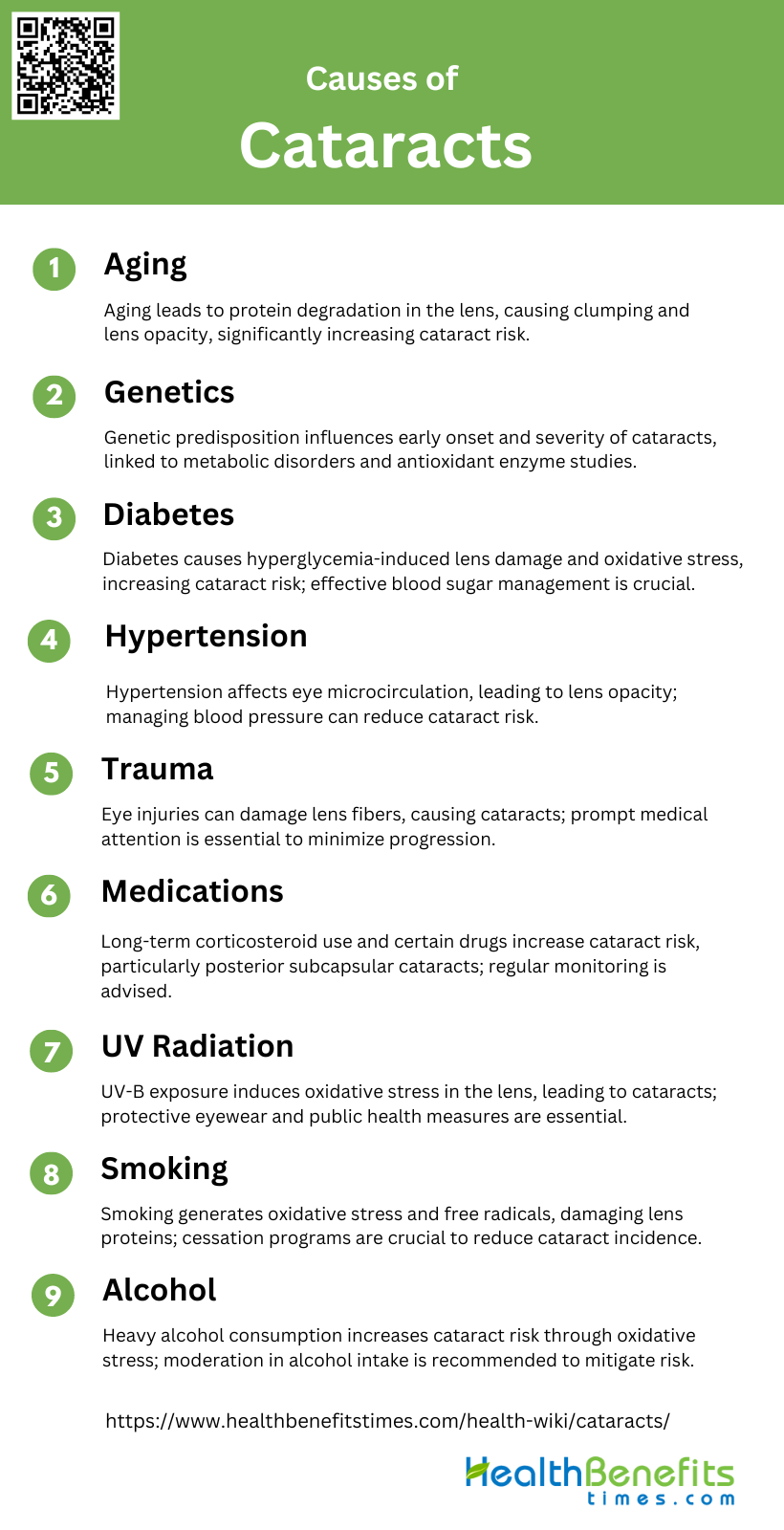
Causes of Cataracts
This condition can be influenced by various factors, ranging from age and genetics to lifestyle choices. Below are some of the primary causes of cataracts:
1. Aging
Aging is the most significant risk factor for cataract development. As individuals age, the proteins in the lens of the eye can degrade and clump together, leading to lens opacity and vision impairment. The prevalence of cataracts approximately doubles with each decade after the age of 30, making it a common condition among the elderly population. The aging process also involves oxidative stress and the accumulation of free radicals, which further contribute to the formation of cataracts. Despite advances in surgical treatments, the increasing proportion of the elderly population worldwide underscores the growing public health challenge posed by age-related cataracts.
2. Genetics
Genetic factors play a crucial role in the development of cataracts. Certain genetic compositions can predispose individuals to early onset and more severe forms of cataracts. Studies have shown that cataracts can be a hallmark of various metabolic disorders and syndromes, indicating a strong genetic component. Advances in genetic engineering and the study of antioxidant enzymes have shown promise in understanding and potentially mitigating the genetic risks associated with cataract formation. However, more research is needed to fully elucidate the genetic mechanisms and to develop targeted interventions.
3. Diabetes
Diabetes is a well-established risk factor for cataract development. Hyperglycemia in diabetic patients leads to the accumulation of sorbitol in the lens, causing osmotic stress and lens opacity. Diabetic individuals are more prone to oxidative stress, which exacerbates the formation of cataracts. Epidemiological studies have consistently shown a higher prevalence of cataracts among diabetic patients, highlighting the need for effective management of blood sugar levels to reduce the risk. The association between diabetes and cataracts underscores the importance of regular eye examinations for diabetic patients to detect and treat cataracts early.
4. Hypertension
Hypertension has been identified as a significant risk factor for cataract development. Elevated blood pressure can lead to changes in the microcirculation of the eye, contributing to lens opacity. Studies have shown that individuals with hypertension are at an increased risk of developing cataracts, particularly in the lens nucleus. The exact mechanisms by which hypertension influences cataract formation are still being investigated, but it is believed that oxidative stress and vascular changes play a role. Managing hypertension through lifestyle modifications and medication can potentially reduce the risk of cataracts.
5. Trauma
Trauma to the eye can lead to the development of cataracts, often referred to as traumatic cataracts. Physical injury can cause direct damage to the lens fibers, leading to their opacification. The severity and location of the trauma can influence the type and progression of the cataract. Immediate medical attention and appropriate treatment are crucial to minimize the impact of trauma on the lens and to prevent the progression of cataracts. Understanding the mechanisms of traumatic cataract formation can aid in developing preventive and therapeutic strategies.
6. Medications
Certain medications, particularly corticosteroids, have been associated with an increased risk of cataract formation. Long-term use of corticosteroids can lead to posterior subcapsular cataracts, which significantly impair vision. Other medications, such as allopurinol and phenothiazines, have also been implicated in cataract development, although more research is needed to establish these associations. Patients on long-term corticosteroid therapy should be monitored regularly for signs of cataract development, and alternative treatments should be considered when possible to mitigate this risk.
7. UV Radiation
Exposure to ultraviolet (UV) radiation, particularly UV-B, is a well-documented risk factor for cataract formation. UV radiation can induce oxidative stress and damage the proteins in the lens, leading to lens opacity. The depletion of the ozone layer and increased UV exposure have heightened the public health significance of this risk factor. Protective measures, such as wearing UV-blocking sunglasses and hats, can help reduce the risk of cataracts associated with UV radiation. Public health interventions are essential to raise awareness and promote protective behaviors.
8. Smoking
Smoking is a significant modifiable risk factor for cataract development. The oxidative stress and free radicals generated by smoking can damage the lens proteins, leading to cataract formation. Studies have shown a strong correlation between smoking and the development of nuclear cataracts, with current smokers being at a higher risk than past smokers. The accumulation of heavy metals like cadmium in the lens due to smoking further exacerbates the risk. Smoking cessation programs and public health campaigns are crucial in reducing the incidence of cataracts related to smoking.
9. Alcohol
The relationship between alcohol consumption and cataract development is complex and appears to be dose-dependent. Moderate alcohol consumption has been associated with a reduced risk of cataract surgery, while heavy consumption increases the risk. The oxidative stress induced by heavy alcohol intake can lead to the aggregation of lens proteins and cataract formation. Different types of alcohol, such as wine versus spirits, may have varying effects on cataract risk. Public health guidelines should emphasize moderation in alcohol consumption to mitigate the risk of cataracts.
Symptoms of Cataracts
Cataracts can significantly affect vision, leading to various symptoms that may worsen over time. Recognizing these symptoms early can help in seeking timely treatment. Below are some common symptoms of cataracts:
1. Clouded, Blurred, or Dim Vision
Clouded, blurred, or dim vision is one of the most common symptoms of cataracts, significantly impacting the quality of life of affected individuals. This symptom is often reported by patients as a primary reason for seeking medical attention and is highly associated with decreased visual function and satisfaction. The opacification of the lens obstructs the passage of light, leading to a general reduction in visual clarity. This symptom can be particularly bothersome, as it affects daily activities such as reading, driving, and recognizing faces.
2. Difficulty Seeing at Night
Difficulty seeing at night, or nyctalopia, is another prevalent symptom of cataracts. This condition is exacerbated by the scattering of light within the eye due to lens opacities, which reduces contrast sensitivity and makes it challenging to see in low-light conditions. Patients often report increased difficulty with nighttime driving and navigating in dimly lit environments. This symptom can significantly impair independence and mobility, leading to a reduced quality of life.
3. Sensitivity to Light and Glare
Sensitivity to light and glare, also known as photophobia, is frequently reported by cataract patients. This symptom occurs because the opacified lens scatters incoming light, causing discomfort and difficulty in bright environments. Patients may find it challenging to be outdoors on sunny days or in brightly lit rooms. This increased sensitivity can also lead to ocular pain and fatigue, further impacting daily activities and overall well-being.
4. Seeing Halos around Lights
Seeing halos around lights is a common visual disturbance experienced by individuals with cataracts. This phenomenon is caused by the diffraction of light as it passes through the cloudy lens, creating ring-like patterns around light sources. Patients often report seeing halos around streetlights, headlights, and other bright lights, which can be particularly troublesome while driving at night. This symptom can contribute to visual discomfort and decreased confidence in performing tasks that require clear vision.
5. Frequent Changes in Eyeglass or Contact Lens Prescription
Frequent changes in eyeglass or contact lens prescription are indicative of the progressive nature of cataracts. As the lens continues to opacify, the refractive properties of the eye change, necessitating regular updates to corrective lenses. Patients may notice that their vision fluctuates and that their current prescription no longer provides adequate clarity. This ongoing need for adjustments can be frustrating and costly, further emphasizing the impact of cataracts on daily life.
6. Fading or Yellowing of Colors
Fading or yellowing of colors is a symptom that significantly affects the perception of the visual world for cataract patients. The accumulation of pigments within the lens causes colors to appear less vibrant and more yellowish. This alteration in color vision can affect activities that rely on accurate color discrimination, such as cooking, dressing, and appreciating art. Patients often report that their environment looks duller and less colorful, which can diminish their overall enjoyment of life.
7. Double Vision in One Eye
Double vision in one eye, or monocular diplopia, is a less common but notable symptom of cataracts. This occurs when the irregularities in the lens cause light to split into multiple images, leading to the perception of double vision. This symptom can be particularly disorienting and may interfere with tasks that require precise vision, such as reading and driving. Monocular diplopia is often resolved by cataract surgery, which restores the clarity of the lens.
8. Need for Brighter Light for Reading and Other Activities
The need for brighter light for reading and other activities is a common complaint among cataract patients. As the lens becomes clouded, more light is required to achieve the same level of visual acuity. Patients may find themselves needing to use stronger lighting or magnifying devices to read comfortably or perform detailed tasks. This increased dependency on bright light can be inconvenient and may limit the ability to engage in activities in dimly lit environments.
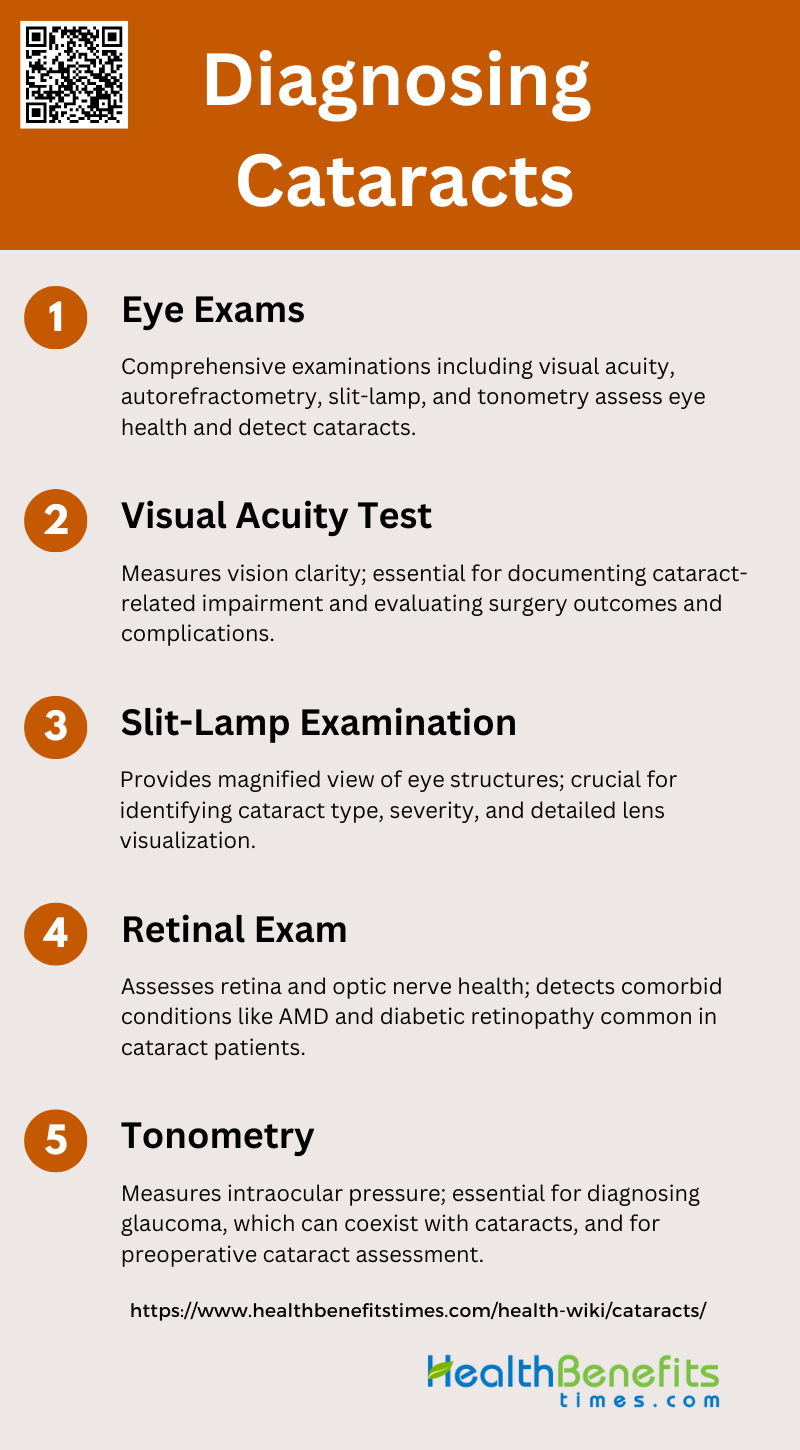
Diagnosing Cataracts
Diagnosing cataracts involves a comprehensive eye examination by an eye care professional. This process includes various tests to assess the clarity of the lens and the overall health of the eye. Below are the key steps involved in diagnosing cataracts:
1. Eye Exams
Eye exams are crucial for diagnosing cataracts and other eye conditions. Comprehensive eye examinations typically include a variety of tests such as visual acuity measurements, autorefractometry, slit-lamp examination, and tonometry. These tests help in assessing the overall health of the eye and identifying any abnormalities. For instance, the Ural Eye and Medical Study (UEMS) included a range of eye examinations to diagnose cataracts and other comorbidities, revealing that 44.3% of the studied population had cataracts. Additionally, the Framingham Eye Study emphasized the importance of detailed ophthalmologic examinations for diagnosing cataracts, glaucoma, diabetic retinopathy, and other eye diseases.
2. Visual Acuity Test
The visual acuity test is a fundamental part of diagnosing cataracts, as it measures the clarity or sharpness of vision. This test involves reading letters on a chart from a specific distance to determine how well one can see. Visual acuity tests are essential for documenting the extent of vision impairment caused by cataracts. For example, a study assessing the outcomes of cataract surgery in South India found that visual acuity tests were crucial in determining the success of the surgery and identifying complications such as cystoid macular edema and posterior capsule opacification. Another study highlighted that visual acuity screening had a high sensitivity (89%) for detecting cataracts.
3. Slit-Lamp Examination
The slit-lamp examination is a critical diagnostic tool for cataracts, providing a magnified view of the eye’s structures, including the cornea, lens, and retina. This examination helps in identifying the type and severity of cataracts. For instance, a study on the accuracy of an AI-based mobile application for detecting cataracts used slit-lamp examinations as the gold standard for comparison, demonstrating the importance of this method in accurate diagnosis. Additionally, slit-lamp images are essential for diagnosing pediatric cataracts, as they allow for detailed visualization of the lens and other eye structures.
4. Retinal Exam
A retinal exam is vital for diagnosing cataracts and assessing the overall health of the retina. This exam involves dilating the pupils and using specialized instruments to examine the retina and optic nerve. Retinal exams can reveal comorbid conditions such as age-related macular degeneration (AMD) and diabetic retinopathy, which are common in patients with cataracts. The UEMS study found that retinal diseases were prevalent among cataract patients, with AMD being the most common. Additionally, the Framingham Eye Study included detailed retinal examinations to screen for various eye diseases, highlighting the importance of this diagnostic tool.
5. Tonometry
Tonometry measures the intraocular pressure (IOP) within the eye, which is essential for diagnosing glaucoma, a condition that can coexist with cataracts. Elevated IOP can indicate the presence of glaucoma, necessitating further investigation and management. A study on clinic-based eye disease screening found that tonometry had a sensitivity of 25% for detecting glaucoma, underscoring its role in comprehensive eye exams. Additionally, tonometry is part of the standard preoperative assessment for cataract surgery, as it helps in planning the surgical approach and managing potential complications.
Treatment option for Cataracts
Treating cataracts typically involves surgical intervention to restore clear vision. The type of treatment recommended depends on the severity of the cataract and the patient’s overall eye health. Below are the main treatment options for cataracts:
1. Surgical Treatment Options
Cataract surgery remains the primary and most effective treatment for cataracts, significantly improving visual outcomes and quality of life for patients. Phacoemulsification, a technique that uses ultrasound to emulsify the lens before removal, is widely regarded as the gold standard due to its superior visual outcomes and lower complication rates compared to extracapsular cataract extraction (ECCE). In developing countries, manual small incision cataract surgery (MSICS) is often preferred due to its cost-effectiveness and comparable visual outcomes to phacoemulsification. Additionally, advancements in intraocular lens (IOL) technology, including premium lenses that correct for astigmatism and presbyopia, offer patients the potential for spectacle independence post-surgery. However, the accessibility and affordability of these advanced surgical options remain a challenge in poorer regions.
2. Non-Surgical Management
Non-surgical management of cataracts is an area of ongoing research, with the aim of finding effective medical treatments to delay or reverse lens opacification. Currently, surgical intervention remains the only proven treatment for cataracts. However, promising developments in pharmacological treatments, such as the use of carnosine and rosmarinic acid, have shown potential in clinical trials to reduce lens opacity and delay cataract progression. These treatments work by targeting the abnormal aggregation of crystallin proteins in the lens, which is the primary cause of cataract formation. While these non-surgical options are not yet widely available or fully validated, they represent a significant step towards more accessible and less invasive treatment alternatives for cataract patients, particularly in regions where surgical options are limited.
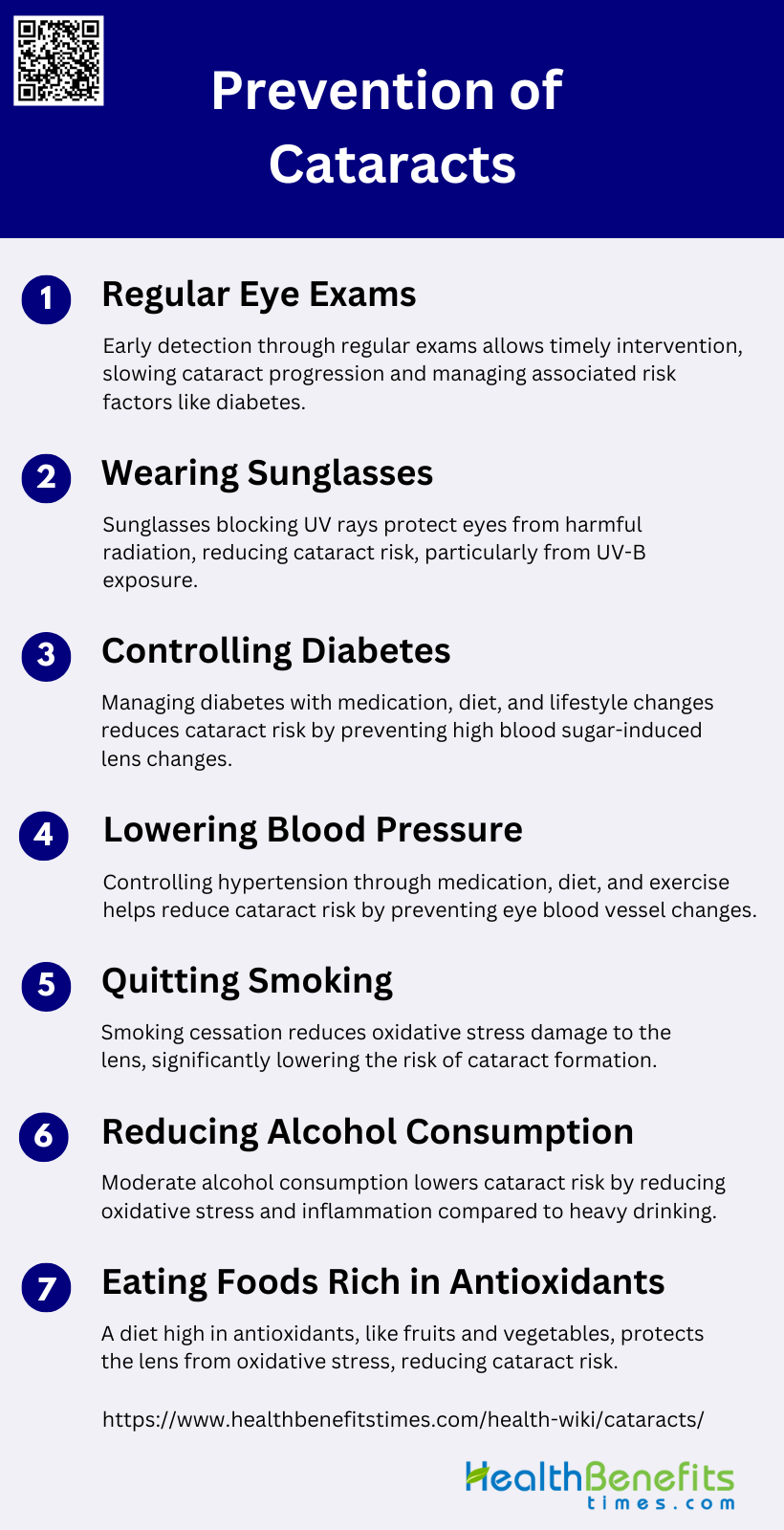
Prevention of Cataracts
Preventing cataracts involves adopting a healthy lifestyle and protecting your eyes from potential damage. While some risk factors like age and genetics cannot be controlled, others can be managed to reduce the likelihood of developing cataracts. Below are some effective strategies for preventing cataracts:
1. Regular Eye Exams
Regular eye exams are crucial for the early detection and management of cataracts. Early diagnosis allows for timely intervention, which can slow the progression of the disease and improve outcomes. Regular check-ups can help identify other risk factors such as diabetes and hypertension, which are associated with cataract development. Studies have shown that early detection through regular eye exams can significantly reduce the risk of severe visual impairment and the need for cataract surgery.
2. Wearing Sunglasses
Exposure to ultraviolet (UV) radiation is a well-documented risk factor for cataract formation. Wearing sunglasses that block UV rays can protect the eyes from harmful radiation and reduce the risk of cataracts. Research indicates that UV-B exposure is particularly harmful and that protective eyewear can mitigate this risk. Therefore, wearing sunglasses is a simple yet effective preventive measure against cataracts.
3. Controlling Diabetes
Diabetes is a significant risk factor for cataract development. High blood sugar levels can lead to changes in the lens of the eye, accelerating cataract formation. Controlling diabetes through medication, diet, and lifestyle changes can significantly reduce the risk of cataracts. Studies have shown that individuals with well-managed diabetes have a lower incidence of cataracts compared to those with poorly controlled diabetes.
4. Lowering Blood Pressure
High blood pressure is another risk factor for cataracts. Hypertension can lead to changes in the blood vessels of the eye, contributing to cataract formation. Lowering blood pressure through medication, diet, and exercise can help reduce this risk. Research has shown that individuals with controlled blood pressure have a lower incidence of cataracts, highlighting the importance of managing hypertension for eye health.
5. Quitting Smoking
Smoking is a well-known risk factor for cataracts. The oxidative stress caused by smoking can damage the lens of the eye, leading to cataract formation. Quitting smoking can significantly reduce this risk. Studies have shown that smokers are at a higher risk of developing cataracts compared to non-smokers, and quitting smoking can help mitigate this risk.
6. Reducing Alcohol Consumption
Excessive alcohol consumption has been linked to an increased risk of cataracts. Alcohol can contribute to oxidative stress and inflammation, which can damage the lens of the eye. Reducing alcohol intake can help lower this risk. Research indicates that moderate alcohol consumption is associated with a lower risk of cataracts compared to heavy drinking.
7. Eating Foods Rich in Antioxidants
A diet rich in antioxidants can help prevent cataracts by reducing oxidative stress in the eye. Foods high in antioxidants, such as fruits and vegetables, can protect the lens from damage. Studies have shown that individuals who consume a diet rich in antioxidants have a lower risk of cataracts. Specific antioxidants like lutein, zeaxanthin, and vitamins A, C, and E have been found to be particularly beneficial in reducing the risk of cataract formation.