Cartilage is a flexible, resilient connective tissue found in various parts of the human body, including joints, ears, nose, and airways. It serves as a crucial structural and functional component, providing support, cushioning, and smooth movement in articulating joints. Composed primarily of collagen fibers, proteoglycans, and specialized cells called chondrocytes, cartilage lacks blood vessels and nerves, which contributes to its limited capacity for self-repair. There are three main types of cartilage: hyaline cartilage (the most common, found in joints), fibrocartilage (present in intervertebral discs and menisci), and elastic cartilage (found in the ear and epiglottis). Each type has unique properties tailored to its specific function in the body. Due to its avascular nature and limited regenerative ability, cartilage damage or degeneration, such as in osteoarthritis, poses significant challenges in medical treatment and tissue engineering.
Types of Cartilage
Cartilage is a specialized connective tissue that plays a vital role in the human body by providing structural support and enabling smooth joint movements. There are three distinct types of cartilage, each with unique properties and functions tailored to specific locations and roles within the body:
1. Hyaline Cartilage
Hyaline cartilage is the most widespread type of cartilage in the human body. It is characterized by a translucent, firm tissue that is well-adapted for weight-bearing. The extracellular matrix (ECM) of hyaline cartilage is rich in type II collagen and proteoglycans, which provide it with a smooth, glassy appearance and high tensile strength. The surface of hyaline cartilage is typically surrounded by the perichondrium, except in articular cartilage, which lacks this layer. The perichondrium consists of an outer fibrous layer and an inner chondrogenic layer. Hyaline cartilage is found in several key locations within the body. It forms the articular surfaces of bones in synovial joints, providing a smooth, lubricated surface for joint movement. Additionally, it is present in the nose, larynx, trachea, and bronchi, where it provides structural support and maintains open airways. Hyaline cartilage also constitutes the costal cartilages at the ventral ends of the ribs, contributing to the flexibility and expansion of the rib cage during respiration.
2. Fibrocartilage
Fibrocartilage is a specialized type of cartilage that combines the properties of dense connective tissue and cartilage. It contains a high density of type I collagen fibers, which provide it with exceptional tensile strength and the ability to withstand compressive forces. Unlike hyaline cartilage, fibrocartilage lacks a perichondrium. The ECM of fibrocartilage is less homogeneous and more fibrous, contributing to its durability and resistance to mechanical stress. Fibrocartilage is found in areas of the body that require a combination of strength and flexibility. It is present in the intervertebral discs, where it acts as a shock absorber between the vertebrae. Other locations include the menisci of the knee, the temporomandibular joint disc, the pubic symphysis, and the insertion sites of tendons and ligaments into bone. These locations benefit from the robust and resilient nature of fibrocartilage, which helps to distribute loads and reduce wear and tear on the joints.
3. Elastic Cartilage
Elastic cartilage is distinguished by its high content of elastin fibers within the ECM, which provides it with remarkable flexibility and the ability to return to its original shape after deformation. The ECM also contains type II collagen; similar to hyaline cartilage, but the presence of elastin fibers gives it a more yellowish appearance. Elastic cartilage is covered by a perichondrium, which supplies nutrients and supports growth and repair. Elastic cartilage is found in structures that require both flexibility and strength. It is present in the external ear (auricle), the auditory tube (Eustachian tube), and the epiglottis. These locations benefit from the unique properties of elastic cartilage, which allow them to maintain their shape while being flexible enough to perform their functions effectively. For example, the epiglottis needs to bend to cover the trachea during swallowing, and the external ear must be flexible yet resilient to maintain its shape.
Functions of Cartilage
Cartilage is a versatile and essential tissue in the human body, playing several critical roles in maintaining structural integrity and facilitating movement. Its unique properties enable it to function effectively in various capacities. The primary functions of cartilage include:
1. Provides Structural Support
Cartilage plays a crucial role in providing structural support to various parts of the body. It is a firm yet flexible tissue that maintain the shape and structure of organs such as the nose, ears, and trachea. In joints, cartilage supports the bones and helps maintain their alignment, ensuring proper joint function and stability. The extracellular matrix (ECM) of cartilage, composed mainly of collagen and proteoglycans, is essential for its structural integrity. This matrix allows cartilage to withstand compressive forces and maintain its shape under mechanical stress, which is vital for the proper functioning of joints and other structures.
2. Cushions Joints
Cartilage serves as a cushion in joints, reducing friction and absorbing shock during movement. Articular cartilage, in particular, covers the ends of bones in synovial joints, providing a smooth, lubricated surface for articulation. This cushioning effect is crucial for minimizing wear and tear on the bones and preventing joint pain and damage. The viscoelastic properties of cartilage enable it to deform under pressure and return to its original shape, effectively absorbing the impact of activities such as walking, running, and jumping. This function is vital for maintaining joint health and preventing conditions like osteoarthritis.
3. Facilitates Smooth Movement
Cartilage facilitates smooth movement by providing a low-friction surface in joints. The unique composition of articular cartilage, which includes a high concentration of water and a specialized arrangement of collagen fibers, allows it to create a nearly frictionless interface between bones. This smooth surface is essential for the efficient transmission of loads and the reduction of mechanical stress on the bones during movement. The lubrication provided by synovial fluid further enhances the smooth gliding of cartilage surfaces, ensuring that joints can move freely and without pain.
4. Supports Growth and Development
Cartilage is essential for skeletal growth and development, particularly during the early stages of life. In embryos and neonates, cartilage serves as a precursor to bone, forming the initial framework for the developing skeleton. This process, known as endochondral ossification, involves the gradual replacement of cartilage with bone tissue. Growth plate cartilage, located at the ends of long bones, is responsible for the longitudinal growth of bones during childhood and adolescence. The regulation of cartilage growth and development is a complex process involving various signaling pathways, including Wnt signaling, which plays a critical role in the progression of endochondral ossification and the maintenance of growth plate function.
5. Provides Flexibility
Cartilage provides flexibility to various structures in the body, allowing them to bend and move without breaking. This flexibility is particularly important in areas such as the rib cage, where cartilage connects the ribs to the sternum, allowing for the expansion and contraction of the chest during breathing. The elastic properties of cartilage are due to its unique composition, which includes a network of collagen fibers and proteoglycans that can stretch and compress. This flexibility is also crucial in joints, where it allows for a range of motion while maintaining the stability and integrity of the joint.
6. Connects Bones
Cartilage plays a vital role in connecting bones, particularly in joints and during the early stages of bone development. In synovial joints, articular cartilage covers the ends of bones, allowing them to move smoothly against each other. In the growth plates of long bones, cartilage cells proliferate and are gradually replaced by bone tissue, facilitating the elongation of bones during growth. Additionally, cartilage forms the initial template for many bones in the body, which are later ossified through the process of endochondral ossification. This connection between cartilage and bone is essential for the proper development and function of the skeletal system.
Cartilage in Different Parts of the Body
Cartilage is a flexible connective tissue found in various parts of the body. It plays a crucial role in providing structure and support while allowing for smooth movement at joints. Below is a list of different types of cartilage and their locations within the body.
1. Joints
Cartilage in joints, specifically articular cartilage, plays a crucial role in facilitating smooth movement and load transmission. Articular cartilage is a specialized connective tissue found in diarthrodial joints, such as the knee, hip, and shoulder. It provides a low-friction surface for articulation and helps distribute mechanical loads to prevent bone damage. This type of cartilage is composed of chondrocytes embedded in an extracellular matrix rich in collagen and proteoglycans, which give it its unique mechanical properties. However, due to its avascular nature, articular cartilage has limited self-repair capacity, making injuries and diseases like osteoarthritis particularly challenging to treat.
2. Ribs
Cartilage in the rib cage, primarily hyaline cartilage, plays a vital role in providing structural support and flexibility. The rib cartilage connects the ribs to the sternum, allowing the rib cage to expand and contract during breathing. This type of cartilage is composed of chondrocytes surrounded by a matrix of collagen and proteoglycans, which provide both strength and elasticity. The rib cartilage also acts as a shock absorber, protecting the thoracic organs from mechanical impacts. Despite its resilience, rib cartilage shares the common challenge of limited regenerative capacity due to its avascular nature, complicating the repair of injuries.
3. Ears and Nose
The cartilage in the ears and nose is primarily elastic cartilage, which provides both structural support and flexibility. This type of cartilage contains a dense network of elastin fibers, allowing it to maintain its shape after deformation. In the ears, elastic cartilage forms the external ear structure, enabling it to capture sound waves effectively. In the nose, it shapes the nasal passages, facilitating airflow and olfaction. The unique properties of elastic cartilage make it essential for the functionality of these sensory organs. However, like other cartilage types, it has limited self-repair capabilities, posing challenges for treating injuries and deformities.
4. Spine
Cartilage in the spine, particularly in the intervertebral discs, is primarily fibrocartilage. This type of cartilage provides both cushioning and flexibility to the vertebral column, allowing it to bend and twist while absorbing mechanical shocks. The intervertebral discs consist of an outer fibrous ring, the annulus fibrosus, and an inner gel-like core, the nucleus pulposus, both of which are rich in collagen and proteoglycans. Degeneration of these discs is a common cause of low back pain and other spinal disorders. The limited regenerative capacity of spinal cartilage, due to its avascular nature, complicates the treatment of such conditions, highlighting the need for advanced therapeutic strategies.
Causes of cartilage damage
Cartilage damage can occur due to various factors, impacting joint function and overall mobility. Common causes include physical trauma, repetitive stress, and degenerative conditions like osteoarthritis. Below is a list of the primary causes of cartilage damage:
1. Direct Injury
Direct injury to cartilage often results from acute trauma, such as sports injuries or accidents, leading to immediate damage to the articular surface. This type of injury can cause mechanical disruption of the cartilage, which may extend to the subchondral bone, resulting in pain, joint dysfunction, and effusions. The body’s natural repair mechanisms are often insufficient to fully restore the damaged cartilage, leading to progressive joint degeneration and conditions like osteoarthritis (OA). In some cases, surgical interventions such as grafts or cell transplants are employed to repair the damage, but these methods have varying degrees of success.
2. Wear and Tear
Wear and tear, also known as degenerative joint disease, is a common cause of cartilage damage, particularly in older adults. Over time, the repetitive mechanical loading and stress on the joints lead to the gradual breakdown of the cartilage matrix. This process is exacerbated by factors such as age, obesity, and a sedentary lifestyle, which contribute to the deterioration of joint structure and function. The progressive loss of cartilage exposes the subchondral bone, triggering inflammation and osteophyte formation, which further accelerates joint degeneration and pain.
3. Overuse Injuries
Overuse injuries occur when repetitive stress and strain are placed on the joints without adequate recovery time, leading to microtrauma and eventual cartilage damage. This is commonly seen in athletes and individuals with physically demanding occupations. The continuous impact and torsional loading can cause chondral damage and may even affect the subchondral bone, resulting in joint pain and dysfunction. Overuse injuries can lead to chronic conditions like osteoarthritis if not properly managed, highlighting the importance of balanced activity and rest.
4. Genetic Factors
Genetic factors play a significant role in the susceptibility to cartilage damage and the development of osteoarthritis. Variations in genes related to cartilage structure, extracellular matrix production, and inflammatory responses can predispose individuals to joint degeneration. For instance, genetic mutations affecting the production of hyaluronan synthase can lead to chronic inflammation and impaired cartilage repair, as seen in certain murine models. Additionally, genetic predispositions can influence the severity and progression of osteoarthritis, making it a multifactorial disease with both genetic and environmental components.
5. Inflammatory Conditions
Inflammatory conditions such as rheumatoid arthritis (RA) and osteoarthritis (OA) are major contributors to cartilage damage. In RA, the immune system attacks the synovium, leading to inflammation and subsequent cartilage degradation. In OA, low-grade inflammation driven by cytokines and other inflammatory mediators plays a crucial role in the breakdown of the cartilage matrix. Pro-inflammatory cytokines like IL-1β, TNF-α, and IL-6 are particularly important in this process, as they promote the production of matrix metalloproteinases and other enzymes that degrade cartilage.
6. Poor Joint Alignment
Poor joint alignment, such as that seen in conditions like hip dysplasia or knee malalignment, can lead to uneven distribution of mechanical stress across the joint surface. This abnormal loading accelerates the wear and tear of cartilage, increasing the risk of damage and osteoarthritis. Misalignment alters the biomechanics of the joint, causing areas of high stress that the cartilage is not equipped to handle, leading to its breakdown over time. Corrective measures, including orthotics or surgical realignment, are often necessary to mitigate the impact of poor joint alignment on cartilage health.
7. Obesity
Obesity is a significant risk factor for cartilage damage due to both mechanical and biochemical factors. The excess body weight increases the mechanical load on weight-bearing joints, accelerating the wear and tear of cartilage. Additionally, adipose tissue produces pro-inflammatory cytokines such as TNF-α, IL-1β, and IL-6, which contribute to the inflammatory environment within the joint and promote cartilage degradation. The combination of increased mechanical stress and inflammation makes obesity a critical factor in the development and progression of osteoarthritis.
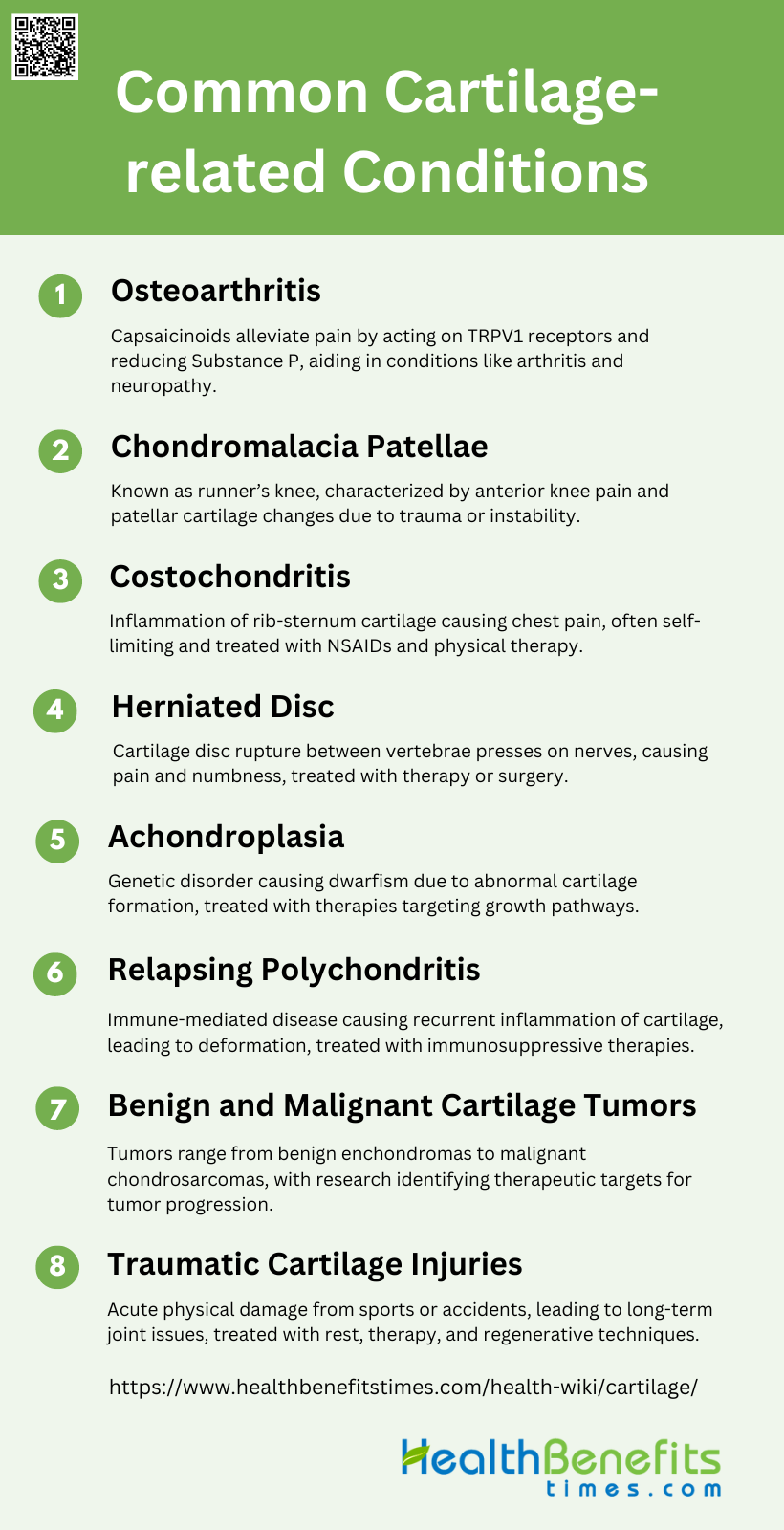
Common Cartilage-related Conditions
Cartilage-related conditions can significantly affect joint health and mobility, leading to pain and discomfort. These conditions often result from wear and tear, injuries, or genetic factors. Below is a list of common cartilage-related conditions:
1. Osteoarthritis
Osteoarthritis (OA) is a chronic joint disease characterized by the progressive degeneration of articular cartilage, subchondral bone sclerosis, and osteophyte formation. It affects over 200 million people globally. Key pathological features include cartilage roughening, thinning, and erosion, often accompanied by chondrocyte proliferation and metabolic changes in the cartilage matrix. The pericellular matrix (PCM) surrounding chondrocytes plays a critical role in disease progression, acting as a transducer of biochemical and biomechanical signals. Subchondral bone remodeling is also implicated in OA pathogenesis, with early bone resorption preceding significant cartilage thinning.
2. Chondromalacia Patellae
Chondromalacia patellae (CMP), also known as runner’s knee, is characterized by anterior knee pain and visible changes in patellar cartilage, such as softening, swelling, and edema. It is caused by factors like trauma, patellofemoral instability, and abnormal patellar kinematics. CMP can be reversible or progress to patellofemoral osteoarthritis. Diagnosis often involves MRI, and treatments include conventional modalities and emerging cell therapies, particularly mesenchymal stem cell (MSC) injections, which show promise in reducing inflammation and improving clinical outcomes.
3. Costochondritis
Costochondritis is an inflammation of the cartilage that connects the ribs to the sternum, causing localized chest pain. It is often self-limiting and can be triggered by physical strain or injury. The condition is typically diagnosed based on clinical examination, and treatment focuses on pain relief through medications like NSAIDs and physical therapy. There is limited specific research data on costochondritis in the provided abstracts.
4. Herniated Disc
A herniated disc occurs when the cartilage disc between spinal vertebrae ruptures or slips, pressing on nearby nerves and causing pain, numbness, or weakness. This condition is often due to age-related degeneration or injury. Diagnosis is usually confirmed through imaging techniques like MRI. Treatment options range from conservative approaches, such as physical therapy and pain management, to surgical interventions in severe cases. There is limited specific research data on herniated discs in the provided abstracts.
5. Achondroplasia
Achondroplasia is a genetic disorder characterized by dwarfism due to abnormal cartilage formation. It is caused by mutations in the FGFR3 gene, leading to disrupted bone growth. Current promising therapies include C-type natriuretic peptide, which targets the underlying genetic pathways to improve growth outcomes. Research into molecular and cellular mechanisms continues to inform potential treatments for this and related conditions.
6. Relapsing Polychondritis
Relapsing polychondritis (RP) is an immune-mediated systemic disease marked by recurrent inflammation of cartilaginous tissues, leading to anatomical deformation and functional impairment. Commonly affected areas include the ears, nose, and joints. Diagnosis is often delayed due to the disease’s pleomorphic nature and non-specific initial symptoms. Treatment focuses on managing inflammation and preventing disease progression through immunosuppressive therapies.
7. Benign and Malignant Cartilage Tumors
Cartilage tumors range from benign lesions like enchondromas and osteochondromas to malignant chondrosarcomas. Benign tumors often result from deregulation of the hedgehog signaling pathway, while malignant chondrosarcomas are resistant to conventional therapies. Research is identifying genes and pathways involved in tumor progression, such as p53, insulin-like growth factor, and matrix metalloproteinases, suggesting new therapeutic targets.
8. Traumatic Cartilage Injuries
Traumatic cartilage injuries result from acute physical damage to the cartilage, often due to sports or accidents. These injuries can lead to long-term joint issues, including osteoarthritis. Treatment typically involves rest, physical therapy, and in some cases, surgical repair. Emerging therapies focus on cartilage regeneration and repair, including the use of stem cells and tissue engineering techniques. There is limited specific research data on traumatic cartilage injuries in the provided abstracts.
Treatment Options for Cartilage related injury
Cartilage injuries can be challenging to treat due to the limited healing capacity of this tissue. However, there are various treatment options available, ranging from conservative approaches to surgical interventions. These treatments aim to alleviate pain, improve joint function, and potentially stimulate cartilage repair or regeneration. Let’s explore the main categories of treatment options for cartilage-related injuries:
1. Nonsurgical Treatments
Nonsurgical treatments for cartilage injuries primarily focus on symptom management and include anti-inflammatory medications, viscosupplementation, bracing, orthotics, and activity modification. These approaches aim to control pain and improve joint function without addressing the underlying cartilage damage. While these methods can provide temporary relief, they do not facilitate cartilage repair or regeneration. Below included some Nonsurgical Treatments option:
1. Rest, Ice, Compression, and Elevation (RICE): RICE is a common initial approach to manage symptoms and reduce inflammation in cartilage injuries.
2. Medications: Analgesics and oral anti-inflammatory medications are frequently used to manage pain and inflammation associated with cartilage injuries.
3. Physical Therapy: Physical therapy is essential for improving joint function and mobility, and it plays a critical role in the rehabilitation process following cartilage injury.
4. Injections: Injections such as hyaluronic acid and platelet-rich plasma (PRP) are used to provide symptomatic relief and potentially promote cartilage healing.
2. Surgical Treatments
Surgical treatments for cartilage injuries vary based on the size and location of the defect. Despite advancements, no single surgical technique has emerged as superior and long-term outcomes remain a subject of ongoing research. Below are included some Surgical Treatments option:
1. Debridement and Lavage (Chondroplasty): Arthroscopic debridement and lavage can offer temporary pain relief but do not provide a long-term solution for cartilage repair.
2. Marrow Stimulation Techniques: Techniques like microfracture and subchondral drilling stimulate the formation of fibrocartilage, which is less durable than hyaline cartilage.
3. Osteochondral Grafting: Osteochondral autograft and allograft transplantation restore the normal cartilage surface and are used for larger defects, with both showing favorable outcomes.
4. Autologous Chondrocyte Implantation (ACI): ACI, including its matrix-induced variant (MACI), is effective for large chondral lesions and offers good long-term durability.
5. Mosaicplasty: Mosaicplasty involves transferring small osteochondral plugs to the defect site and is suitable for smaller lesions, providing a durable repair.