Cancer is a group of diseases characterized by the uncontrolled growth and spread of abnormal cells in the body. Normally, cells grow and divide in a regulated manner, but cancerous cells defy these controls, leading to the formation of tumors, which can be benign (non-cancerous) or malignant (cancerous). Malignant tumors invade nearby tissues and can metastasize, or spread, to distant parts of the body through the bloodstream or lymphatic system. This abnormal cell growth is often triggered by genetic mutations caused by various factors, including environmental exposures, lifestyle choices, and inherited genetic predispositions. Cancer can affect almost any part of the body and is a leading cause of death worldwide, though advances in early detection, treatment, and prevention have improved survival rates for many types of cancer.
Types of Cancer
Cancer is a complex group of diseases with many different types, each characterized by the uncontrolled growth and spread of abnormal cells. Understanding the various types of cancer is crucial for diagnosis, treatment, and research. Below is a list of some common types of cancer:
1. Common types of cancer
Cancer is a leading cause of death worldwide, with various types affecting different parts of the body. Each type of cancer has unique characteristics, symptoms, and treatment options. Below is a list of some of the most common types of cancer:
- Breast Cancer: Breast cancer remains one of the most frequently diagnosed cancers and is projected to continue being a leading cancer diagnosis in the coming years. It is also a common primary site for metastasis to the uterine corpus.
- Lung and Bronchus Cancer: Lung cancer is the most common primary cancer that metastasizes to uncommon sites and is projected to remain the top cancer killer. It has a high incidence in older adults.
- Prostate Cancer: Prostate cancer is a leading cancer diagnosis and has significant heritability. It is less frequent in male patients with diabetes.
- Colorectal Cancer: Colorectal cancer is a common diagnosis but is projected to be surpassed by thyroid cancer by 2030. It is also a frequent primary site for metastasis to the uterine corpus.
- Melanoma of the Skin: Melanoma is projected to become one of the most common cancers by 2030 and has a significant genetic component. It can metastasize to the uterine corpus.
- Bladder Cancer: Bladder cancer has a lower relative risk in patients with diabetes and shows a small genetic component. It can also metastasize to the uterine corpus.
- Non-Hodgkin Lymphoma: Non-Hodgkin lymphoma is a common primary cancer that metastasizes to uncommon sites. The genetic component is less clear compared to other cancers.
- Kidney and Renal Pelvis Cancer: Kidney cancer has a significant genetic component and a moderate relative risk in patients with diabetes. It is a common urological tumor 4.
- Endometrial Cancer (Uterine Cancer): Endometrial cancer is projected to become one of the most common cancers by 2030 and has a significant genetic component. It has a high relative risk in patients with diabetes.
- Pancreatic Cancer: Pancreatic cancer is projected to become a leading cause of cancer-related death by 2030 and has a significant genetic component. It has a high relative risk in patients with diabetes.
- Thyroid Cancer: Thyroid cancer is projected to become the fourth leading cancer diagnosis by 2030. It can metastasize to the uterine corpus.
- Liver and Intrahepatic Bile Duct Cancer: Liver cancer is projected to become a leading cause of cancer-related death by 2030 and has the worst prognosis among cancers with metastasis to uncommon sites. It has a high relative risk in patients with diabetes.
2. Rare types of cancer
While common cancers like breast, lung, and prostate cancer are widely known, there are numerous rare types of cancer that affect fewer individuals but can be equally devastating. These rare cancers often require specialized treatment and research. Below is a list of some rare types of cancer:
- Pancreatic Cancer: Pancreatic gastrointestinal stromal tumors (PGISTs) are exceptionally rare, constituting less than 1% of malignant pancreatic neoplasms. A unique case involved a 46-year-old female with concurrent double primary malignancies, highlighting the clinical complexities and importance of early diagnosis and intervention.
- Leukemia: Leukemia, a type of blood cancer, is characterized by the rapid production of abnormal white blood cells. These cells crowd out normal blood cells, leading to severe health complications. Treatment often involves chemotherapy, radiation therapy, and sometimes stem cell transplants.
- Lymphoma: Lymphoma is a cancer of the lymphatic system, which includes the lymph nodes, spleen, and bone marrow. It is broadly categorized into Hodgkin and non-Hodgkin lymphoma. Treatment typically involves chemotherapy, radiation, and targeted therapies.
- Appendix Cancer: Appendiceal malignancies are rare, constituting about 2% of all gastrointestinal cancers. They vary in histology and clinical presentation, with neuroendocrine tumors being the most common. Early-stage tumors are usually treated by surgical resection, with adjuvant therapy dependent on histology and stage.
- Gastrointestinal Stromal Tumor (GIST): Gastrointestinal stromal tumors (GISTs) are rare mesenchymal tumors of the gastrointestinal tract. They are often diagnosed through immunohistochemical analysis, with CD117 expression being a key diagnostic marker. Treatment typically involves surgical resection and targeted therapy with imatinib.
- Ocular (Eye) Melanoma: Ocular melanoma is a rare cancer that develops in the cells that produce pigment in the eye. It is the most common primary eye cancer in adults. Treatment options include radiation therapy, laser therapy, and surgical removal of the tumor.
- Salivary Gland Cancer: Salivary gland cancer is a rare type of cancer that forms in the tissues of the salivary glands. It can present as a painless lump or swelling. Treatment often involves surgical resection, sometimes followed by radiation therapy or chemotherapy.
- Small Bowel Cancer: Small bowel cancers are rare, accounting for about 2% of all gastrointestinal malignancies. Neuroendocrine tumors are the most common type, followed by adenocarcinoma, lymphoma, and sarcoma. Treatment usually involves surgical resection, with adjuvant therapy based on histology and stage.
- Soft Tissue Sarcomas: Soft tissue sarcomas are a diverse group of rare cancers that arise in the connective tissues. They account for less than 1% of all cancers but are challenging to treat due to their varied histology. Treatment typically involves surgical resection, radiation, and sometimes chemotherapy.
Causes of Cancer
Cancer can develop due to a variety of factors, ranging from genetic mutations to environmental exposures. Understanding these causes is essential for prevention, early detection, and effective treatment. Below is a list of some common causes of cancer:
1. Genetic factors of Cancer
Genetic factors play a significant role in the development of cancer, influencing an individual’s susceptibility to the disease. Mutations in specific genes can increase the risk of certain types of cancer, often running in families. Below is a list of some key genetic factors associated with cancer:
- Inherited Gene Mutations (e.g., BRCA1/BRCA2): Inherited mutations in the BRCA1 and BRCA2 genes significantly increase the risk of breast and ovarian cancers. Studies show that BRCA1 mutation carriers have a 65% risk of breast cancer and 39% risk of ovarian cancer by age 70, while BRCA2 mutation carriers have a 45% risk of breast cancer and 11% risk of ovarian cancer.
- Family History of Cancer: A family history of breast cancer or ovarian cancer is a well-recognized risk factor. Women with early-onset breast cancer often have a family history of these cancers, and BRCA mutations are more frequent among them. Almost half of early-onset breast cancer cases have some family history, with 9% associated with BRCA1 or BRCA2 mutations.
2. Environmental factors
Environmental factors significantly contribute to the development of cancer, influencing the risk through various external exposures. These factors can include lifestyle choices, pollutants, and occupational hazards, each playing a role in altering cellular processes. Understanding these factors is crucial for prevention and public health strategies. Below is a list of some key environmental factors associated with cancer:
1. Smoking: Smoking, particularly cigarette smoking, is a well-known risk factor for various cancers, including bladder cancer and pancreatic cancer. The inhalation of cigarette smoke introduces mutagenic nitrosamines and other harmful chemicals into the body, significantly increasing cancer risk.
2. Alcohol: Alcohol consumption is linked to an increased risk of several cancers, including melanoma and pancreatic cancer. Ethanol and its metabolites contribute to cancer development by inducing oxidative stress and DNA damage, which can lead to tumor formation.
3. Exposure to Harmful Chemicals: Exposure to harmful chemicals, such as aromatic amines and organochlorinated compounds, is strongly associated with cancers like bladder cancer and pancreatic cancer. These chemicals are found in various industrial products and can cause DNA mutations and oxidative stress.
4. Ultraviolet (UV) Radiation from Sun or Tanning Beds: UV radiation is a major risk factor for skin cancers, including melanoma, basal cell carcinoma, and squamous cell carcinoma. UVB radiation causes DNA damage, while UVA radiation induces oxidative stress, both contributing to skin carcinogenesis.
5. Air Pollution: Air pollution, including outdoor and indoor pollutants like asbestos and environmental tobacco smoke, is linked to increased risks of lung cancer and other cancers. Specific agents in air pollution, such as polycyclic aromatic hydrocarbons, are known carcinogens.
6. Arsenic in Drinking Water: High levels of arsenic in drinking water are associated with increased risks of bladder, skin, and lung cancers. Arsenic exposure can occur through contaminated water sources and occupational hazards, leading to significant health risks.
3. Lifestyle factors
Lifestyle choices can significantly impact the risk of developing cancer. Factors such as diet, physical activity play crucial roles in either increasing or decreasing cancer risk. Understanding these lifestyle factors can help in making informed decisions for better health. Below is a list of some key lifestyle factors associated with cancer:
- Poor Diet: A poor diet, characterized by low intake of fruits, vegetables, and whole grains, significantly increases cancer risk. High consumption of red and processed meats is particularly associated with colorectal cancer.
- Lack of Physical Activity: Physical inactivity is linked to an increased risk of various cancers, including colorectal and breast cancer. Regular physical activity can reduce cancer risk by promoting a healthy weight and reducing inflammation.
- Obesity and Overweight: Obesity and overweight are major risk factors for several cancers, including colorectal, breast, and endometrial cancers. Excess body weight leads to chronic inflammation and hormonal imbalances, which can promote cancer development.
- Alcohol Consumption: Alcohol consumption is a well-established risk factor for cancers of the oral cavity, pharynx, esophagus, liver, and breast. Even moderate alcohol intake can increase cancer risk, making it crucial to limit consumption.
4. Age (cancer risk increases with age)
Cancer risk increases with age due to a variety of biological and environmental factors. Studies have shown that epigenetic aging, measured through DNA methylation, is associated with increased cancer risk and shorter survival times post-diagnosis. The decline of the immune system, particularly the atrophy of the thymus and the resulting decrease in T cell production, also contributes significantly to the increased incidence of cancer in older individuals.
5. Hormonal factors
Hormones play a crucial role in regulating various bodily functions, and imbalances or prolonged exposure to certain hormones can increase the risk of developing cancer. These hormonal factors can influence the growth and proliferation of cancer cells, particularly in hormone-sensitive tissues. Understanding these factors is essential for prevention and treatment strategies. Below is a list of some key hormonal factors associated with cancer:
- Reproductive History: Reproductive history significantly influences cancer risk. For instance, increased parity is associated with a decreased risk of primary liver cancer(PLC). Conversely, late age at first birth is linked to a higher risk of melanoma. Additionally, early age at menarche and late age at menopause are associated with increased breast cancer risk.
- Hormone Replacement Therapy: Hormone replacement therapy (HRT) has complex effects on cancer risk. It increases the risk of breast cancer, particularly with long-term use. However, HRT is associated with a reduced risk of esophageal cancer and pancreatic cancer. The type and duration of HRT use are critical factors in determining its impact on cancer risk.
6. Certain Medical Treatments
Certain medical treatments, such as radiation therapy, have been linked to an increased risk of developing secondary cancers. Radiation therapy, while effective in treating primary tumors, can cause DNA damage in surrounding healthy tissues, potentially leading to carcinogenesis.
7. Stress and Lack of Sleep
Stress and lack of sleep may indirectly increase cancer risk by weakening the immune system and promoting chronic inflammation. Chronic stress can lead to hormonal imbalances and oxidative stress, which are associated with DNA damage and cancer development.
8. Radon Gas Exposure
Radon gas exposure is a significant cause of lung cancer, particularly in non-smokers. Radon, a radioactive gas, emits alpha particles that cause DNA damage and genomic instability, leading to lung cancer. It is the second leading cause of lung cancer after smoking.
General Symptoms of Cancer
Cancer can manifest through a variety of symptoms that may often be subtle or mistaken for other health issues. Recognizing these general symptoms early can be crucial for timely diagnosis and treatment. Common signs to watch for include:
- Fatigue: Fatigue is one of the most commonly reported symptoms among cancer patients, often appearing in various symptom clusters such as fatigue-pain and fatigue-insomnia.
- Unexplained Weight Loss: Weight loss is frequently observed in cancer patients, particularly those with lung cancer, and is often associated with other symptoms like anorexia and loss of appetite.
- Persistent Pain: Pain is a prevalent and distressing symptom in cancer patients, often reported alongside other symptoms like fatigue and insomnia.
- Fever or Night Sweats: Fever and night sweats can occur in cancer patients, although they are less commonly highlighted in symptom studies compared to other symptoms like pain and fatigue.
- Changes in Skin Colors: Changes in skin color, such as jaundice or darkening, can be indicative of certain types of cancer, although this symptom is less frequently discussed in general cancer symptom literature.
- Sores that Don’t Heal: Non-healing sores are one of the American Cancer Society’s warning signs of cancer and can be an early indicator of the disease.
- Changes in Moles or New Skin Marks: Changes in moles or new skin marks are significant indicators of skin cancer and are part of the early warning signs for cancer detection.
- Persistent Pain or Aches without Known Cause: Persistent, unexplained pain is a common symptom in cancer patients and is often part of symptom clusters with fatigue and insomnia.
- Persistent Cough or Hoarseness: Persistent cough and hoarseness are particularly common in lung cancer patients and can be part of a symptom cluster with dyspnea and fatigue.
- Difficulty Swallowing: Difficulty swallowing is a symptom often associated with cancers of the throat or esophagus and can significantly impact a patient’s quality of life.
- Persistent Indigestion or Discomfort after Eating: Indigestion and discomfort after eating can be symptoms of gastrointestinal cancers and are included in the American Cancer Society’s warning signs.
- Changes in Bowel or Bladder Habits: Changes in bowel or bladder habits are critical symptoms for cancers of the digestive and urinary systems and are part of the early warning signs.
- Unusual Bleeding or Bruising: Unusual bleeding or bruising is a significant symptom that can indicate various types of cancer and is one of the American Cancer Society’s warning signs.
- Persistent Bloating: Persistent bloating can be a symptom of ovarian or gastrointestinal cancers and is often reported by patients with these types of cancer.
- Unexplained Lumps or Swelling in Any Part of the Body: Unexplained lumps or swelling are critical indicators of cancer and are part of the early warning signs for cancer detection.
- Headaches: Headaches can be a symptom of brain cancer or metastasis to the brain, although they are less frequently highlighted in general cancer symptom literature.
- Vision or Hearing Problems: Vision or hearing problems can be symptoms of cancers affecting the brain or sensory organs, although they are less commonly discussed in general cancer symptom studies.
- Mouth Changes Such as Sores, Bleeding, Pain, or Numbness: Changes in the mouth, such as sores, bleeding, pain, or numbness, can be indicative of oral cancers and are part of the early warning signs.
- Persistent Nausea or Vomiting: Nausea and vomiting are common symptoms in cancer patients, often appearing in symptom clusters with other gastrointestinal symptoms.
- Loss of Appetite: Loss of appetite is frequently reported in cancer patients, particularly those with lung cancer, and is often associated with weight loss and anorexia.
- Difficulty Breathing or Shortness of Breath: Difficulty breathing or shortness of breath is a common symptom in lung cancer patients and can be part of a symptom cluster with fatigue and cough.
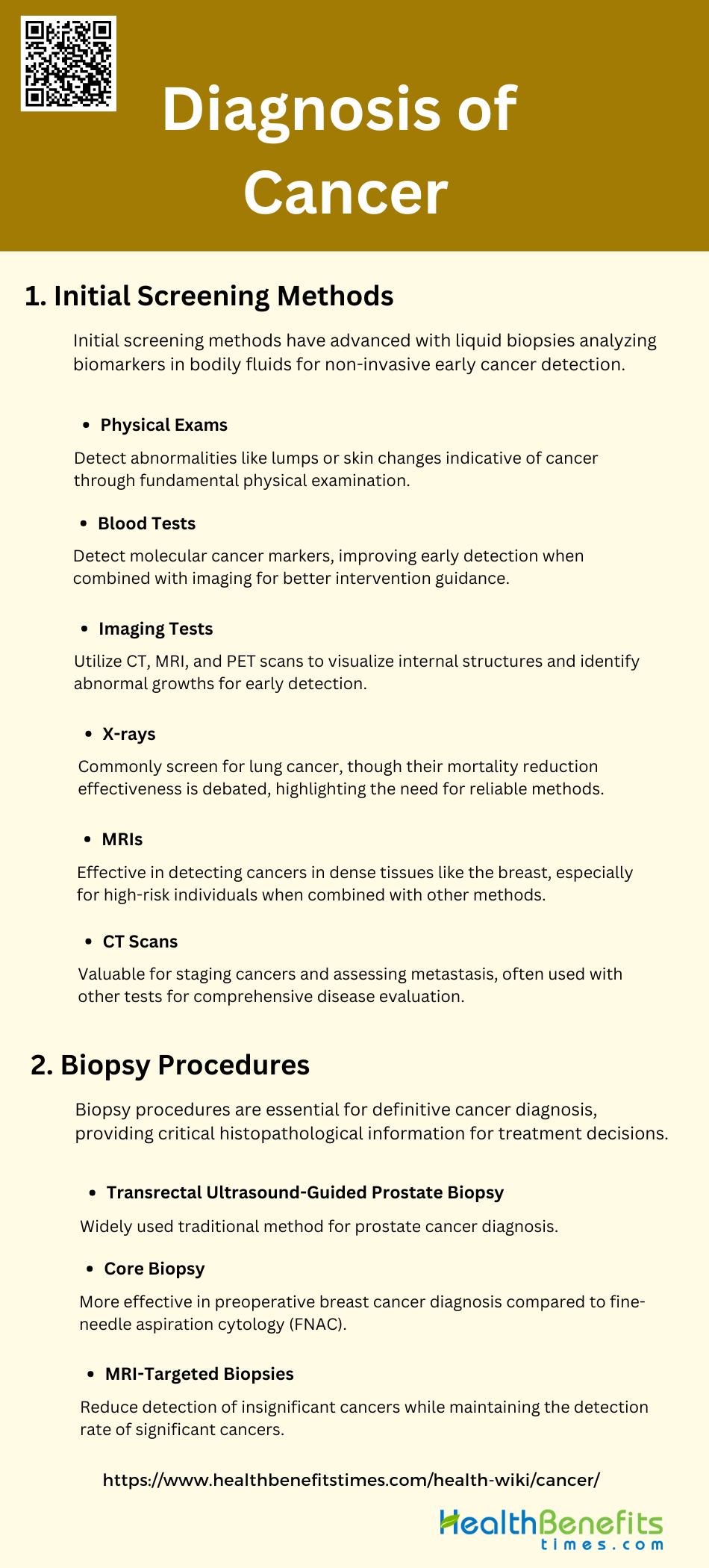
Diagnosis of Cancer
The diagnosis of cancer involves a series of steps to accurately identify the presence and type of cancer in a patient. This process is critical for determining the appropriate treatment plan and improving patient outcomes. Below are the key steps involved in the diagnosis of cancer:
1. Initial screening methods
Initial screening methods for cancer have evolved significantly with the advent of liquid biopsy techniques. Liquid biopsies, which analyze circulating tumor DNA (ctDNA), circulating tumor cells (CTCs), and other biomarkers in blood, urine, or saliva, offer a non-invasive, rapid, and dynamic approach to cancer detection. These methods are particularly advantageous for early diagnosis and monitoring of disease progression, as they can capture the genetic profile of tumors and detect minimal residual disease post-treatment. The use of next-generation sequencing (NGS) in liquid biopsies has further enhanced the sensitivity and specificity of these tests, making them a promising tool for early cancer screening. Below are some common initial screening methods for cancer:
- Physical Exams: Physical exams are a fundamental method for initial cancer screening, allowing healthcare providers to detect abnormalities such as lumps or skin changes that may indicate cancer.
- Blood Tests: Blood tests can detect molecular markers of cancer, offering a minimally invasive method for early detection. Studies show that combining blood tests with imaging can improve detection rates and guide interventions.
- Imaging Tests: Imaging tests, including CT, MRI, and PET scans, are crucial for cancer screening. They help in visualizing internal structures and identifying abnormal growths, enhancing early detection and treatment planning.
- X-rays: X-rays are commonly used for lung cancer screening, although their effectiveness in reducing mortality is debated. Frequent chest X-rays may even be harmful, highlighting the need for more reliable methods.
- MRIs: MRI is highly effective for detecting cancers, especially in dense tissues like the breast. It is recommended for high-risk individuals and can be combined with other screening methods for better accuracy.
- CT Scans: CT scans are valuable for staging cancers and assessing metastasis. They are often used in conjunction with other tests to provide a comprehensive evaluation of the disease.
2. Biopsy procedures
Biopsy procedures remain a cornerstone in the definitive diagnosis of cancer. Traditional methods such as transrectal ultrasound-guided prostate biopsy and core biopsy are widely used, with the latter being more effective in preoperative diagnosis of breast cancer compared to fine-needle aspiration cytology (FNAC). Recent advancements include MRI-targeted biopsies, which have shown to reduce the detection of clinically insignificant cancers while maintaining the detection rate of significant cancers. These procedures, although invasive, provide critical histopathological information that guides treatment decisions and prognostication.
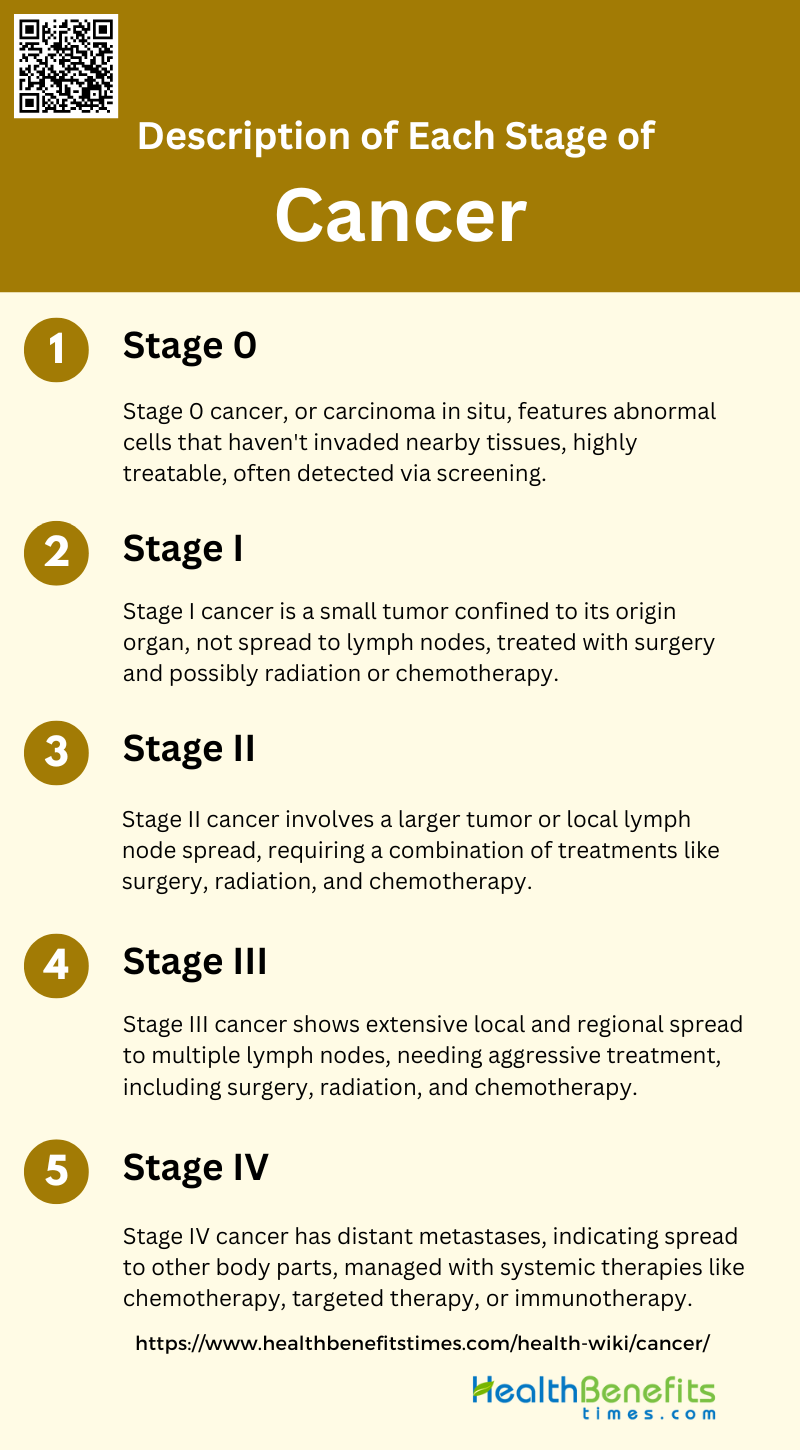
Stages of Cancer
Explanation of staging
Cancer staging is a critical process in oncology that involves determining the extent of cancer within the body, which is essential for guiding treatment decisions and predicting patient outcomes. The most widely used system for staging various cancers is the Tumor, Node, Metastasis (TNM) system, which classifies cancer based on the size and extent of the primary tumor (T), the involvement of regional lymph nodes (N), and the presence of distant metastasis (M). Accurate staging is crucial as it influences treatment strategies and helps in evaluating the effectiveness of therapies. For instance, in lung cancer, preoperative staging using advanced imaging techniques like PET-CT can reduce unnecessary surgeries and improve patient management. Similarly, in cervical cancer, surgical staging can provide more precise information on lymph node involvement compared to clinical staging, potentially impacting disease-free survival and overall survival. The continuous evolution of staging systems, incorporating nonanatomic prognostic factors and molecular markers, aims to enhance the personalization of cancer care, ensuring that patients receive the most appropriate and effective treatments.
Description of each stage
1. Stage 0
Stage 0 cancer, also known as carcinoma in situ, is characterized by the presence of abnormal cells that have not yet invaded nearby tissues. This stage is often considered highly treatable and is typically detected through screening methods. For instance, in breast cancer, ductal carcinoma in situ (DCIS) is a common form of Stage 0 cancer.
2. Stage I
Stage I cancer is defined by a small tumor that is confined to the organ of origin and has not spread to lymph nodes or distant sites. This stage is often associated with a high survival rate and is usually treated with surgery, sometimes followed by radiation or chemotherapy. For example, in lung cancer, Stage I is divided into IA and IB based on tumor size and extent.
3. Stage II
Stage II cancer involves a larger tumor or one that has begun to spread to nearby lymph nodes but not to distant sites. This stage is more complex and may require a combination of treatments, including surgery, radiation, and chemotherapy. In colon cancer, the inclusion of carcinoembryonic antigen (CEA) levels can further refine prognosis and treatment strategies for Stage II patients.
4. Stage III
Stage III cancer is characterized by more extensive local and regional spread, often involving multiple lymph nodes. This stage typically requires aggressive treatment, including surgery, radiation, and chemotherapy. For instance, in cervical cancer, the FIGO 2018 staging system shows a significant increase in Stage III cases due to better detection of lymph node involvement.
5. Stage IV
Stage IV cancer is defined by the presence of distant metastases, indicating that the cancer has spread to other parts of the body. This stage is often considered advanced and may be managed with systemic therapies such as chemotherapy, targeted therapy, or immunotherapy. In breast cancer, Stage IV is determined solely by the presence of metastatic disease, regardless of tumor size or lymph node involvement.
Treatment Options for Cancer
Cancer treatment encompasses a wide range of modalities, each with unique mechanisms and applications. This synthesis explores various treatment options, including traditional methods like surgery and chemotherapy, as well as advanced therapies such as immunotherapy and gene therapy.
- Surgery: Surgery remains a cornerstone for solid tumors, often used in combination with other treatments to improve outcomes.
- Radiation Therapy: Radiation therapy is a long-standing treatment that uses high-energy particles to destroy cancer cells, often combined with other therapies for enhanced efficacy.
- Chemotherapy: Chemotherapy involves the use of cytotoxic drugs to kill rapidly dividing cancer cells, but it is often associated with significant side effects and drug resistance.
- Targeted Therapy: Targeted therapy uses drugs designed to specifically target cancer cell molecules, offering a more precise treatment with potentially fewer side effects compared to traditional chemotherapy.
- Immunotherapy: Immunotherapy has emerged as a crucial treatment, leveraging the body’s immune system to fight cancer. It is now a first-line treatment in many cases.
- Hormone Therapy: Hormone therapy is used for cancers that are sensitive to hormones, such as breast and prostate cancer, by blocking the body’s ability to produce hormones or interfering with hormone action.
- Stem Cell Transplant (Bone Marrow Transplant): Stem cell transplants replace damaged bone marrow with healthy cells, often used after high-dose chemotherapy or radiation therapy to restore the body’s ability to produce blood cells.
- Photodynamic Therapy: Photodynamic therapy (PDT) uses light-activated drugs to produce reactive oxygen species that kill cancer cells. It is minimally invasive and can be combined with other treatments to enhance efficacy.
- Gene Therapy: Gene therapy introduces genetic material into cells to fight or prevent disease, offering promising new methods for cancer treatment by targeting the genetic basis of cancer.
- Interventional Radiology: Interventional radiology uses imaging techniques to guide minimally invasive procedures for diagnosing and treating cancer, often used in combination with other therapies.
- Hyperthermia: Hyperthermia involves heating body tissues to damage and kill cancer cells, often used in conjunction with other treatments like radiation therapy to enhance their effectiveness.
- Cryoablation: Cryoablation uses extreme cold to destroy cancer cells, providing a minimally invasive option for treating certain types of tumors.
- Radiofrequency Ablation; Radiofrequency ablation uses high-frequency electrical currents to heat and destroy cancer cells, often used for tumors that are difficult to remove surgically.
- Biological Therapy (Biotherapy): Biological therapy uses living organisms, substances derived from living organisms, or synthetic versions to treat cancer, often enhancing the body’s natural defenses against cancer.
- Proton Therapy: Proton therapy is a type of radiation therapy that uses protons instead of X-rays, allowing for more precise targeting of tumors with potentially fewer side effects.
- Complementary and Alternative Medicine (CAM): CAM includes a variety of non-mainstream practices used alongside conventional treatments, such as acupuncture, herbal medicine, and dietary supplements, to support overall well-being.
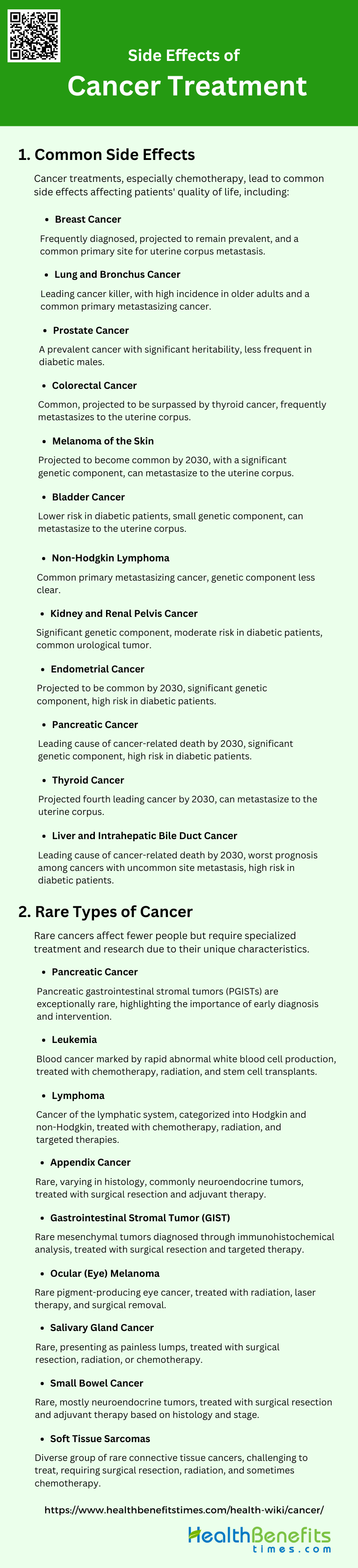
Side Effects of Cancer Treatment
Cancer treatments, while essential for combating the disease, often come with a range of side effects that can impact a patient’s quality of life. These side effects vary depending on the type of treatment and individual patient factors. Below are some common side effects associated with cancer treatment:
1. Common side effects
Cancer treatments, particularly chemotherapy, often result in a range of common side effects that significantly impact patients’ quality of life. These include nausea, fever, pain, weight loss, hair loss, and gastrointestinal issues such as bone marrow suppression and hepatotoxicity. Additionally, patients frequently experience fatigue, depression, sleep disturbances, and peripheral neuropathy, which are particularly prevalent in breast cancer survivors. Below are some common side effects of cancer treatment:
- Hair Loss: Chemotherapy often leads to hair loss, which is one of the most common and visible side effects reported by patients.
- Fatigue: Prevalent long-term side effect of chemotherapy, significantly affecting patients’ daily activities and quality of life.
- Nausea and Vomiting: Nausea and vomiting are well-recognized side effects of chemotherapy, with effective anti-emesis treatments developed over decades.
- Loss of Appetite and Weight Changes: Chemotherapy can lead to loss of appetite and subsequent weight changes, impacting patients’ nutritional status and overall health.
- Skin Reactions: Skin reactions such as redness, itching, dryness, and peeling are common side effects of cancer treatments, particularly chemotherapy.
- Mouth Sores and Dental Problems: Chemotherapy can cause mouth sores and dental problems, which can affect eating and oral hygiene.
- Diarrhea or Constipation: Gastrointestinal issues like diarrhea and constipation are frequent side effects of chemotherapy, affecting patients’ comfort and health.
- Increased Risk of Infections: Chemotherapy can suppress the immune system, increasing the risk of infections.
- Anemia (Low Red Blood Cell Count): Anemia is a common side effect of chemotherapy, leading to fatigue and weakness.
- Easy Bruising and Bleeding: Chemotherapy can cause easy bruising and bleeding due to its impact on blood cell production.
- Pain: including neuropathic pain, is a significant side effect of cancer treatments, affecting patients’ quality of life.
- Nerve Problems (Peripheral Neuropathy): Peripheral neuropathy, characterized by nerve damage and pain, is a common side effect of chemotherapy.
- Cognitive Changes (“Chemo Brain”): Cognitive dysfunction, often referred to as “chemo brain,” includes memory loss and difficulty concentrating, and is a well-documented side effect of chemotherapy.
- Mood Changes and Emotional Distress: Cancer treatments can lead to mood changes and emotional distress, impacting mental health and well-being.
- Sleep Problems: Sleep disorders are common among cancer patients undergoing chemotherapy, affecting overall health and recovery.
- Fertility Issues: Chemotherapy can impact fertility, which is a significant concern for many patients.
- Sexual Health Problems: Sexual health problems, including decreased libido and sexual dysfunction, are reported by patients undergoing cancer treatments.
- Lymphedema (Swelling): Lymphedema, or swelling, can occur as a side effect of cancer treatments, particularly surgery and radiation.
- Heart Problems: Certain chemotherapy agents are associated with cardiotoxicity, leading to heart problems.
- Lung Problems: Chemotherapy can cause lung issues, including inflammation and reduced lung function.
- Kidney and Bladder Issues: Kidney and bladder problems are potential side effects of chemotherapy, affecting renal function.
- Bone and Joint Pain: Bone and joint pain are common side effects of cancer treatments, impacting mobility and comfort.
- Muscle Weakness: Muscle weakness is a frequent side effect of chemotherapy, affecting physical strength and endurance.
- Changes in Taste and Smell: Chemotherapy can alter taste and smell, affecting appetite and enjoyment of food.
- Eye and Vision Changes: Vision changes and eye problems can occur as side effects of chemotherapy5.
- Hearing Problems: Some chemotherapy agents can cause hearing problems, including tinnitus and hearing loss.
- Hormone Changes: Hormonal changes are common in patients undergoing cancer treatments, affecting various bodily functions.
- Swallowing Difficulties: Swallowing difficulties can arise from chemotherapy, impacting nutrition and comfort.
- Shortness of Breath: Shortness of breath is a potential side effect of chemotherapy, affecting respiratory function.
- Edema: Edema, or swelling, can occur as a side effect of cancer treatments, impacting comfort and mobility.
2. Long-term side effects
Long-term side effects of cancer treatment can persist for years and may include severe conditions such as cardiotoxicity, secondary cancers, cognitive impairments, and neurotoxicity. These chronic toxicities can lead to accelerated aging and significantly reduce the quality of life for survivors. For instance, prostate cancer survivors often face persistent urinary, sexual, and bowel dysfunctions, which are strongly associated with poorer quality of life even a decade after diagnosis. Below are some common long-term side effects of cancer treatment:
- Secondary Cancers: Cancer treatments, particularly chemotherapy and radiation, can increase the risk of developing secondary cancers later in life.
- Organ Damage: Chemotherapy and radiation can cause long-term damage to organs such as the heart, lungs, and liver, affecting their function.
- Nerve Damage: Peripheral neuropathy, a common side effect of cancer treatment, can result in long-term nerve damage, causing pain and functional impairment.
- Lymphedema (Swelling): Radiation and surgery, especially in breast cancer treatment, can lead to lymphedema, a chronic condition characterized by swelling.
- Liver Problems: Cancer treatments, including chemotherapy, can lead to liver toxicity, resulting in long-term liver problems and impaired liver function.
- Kidney and Bladder Issues
- Nephrotoxic treatments can cause chronic kidney disease, proteinuria, and other renal dysfunctions, impacting long-term kidney and bladder health.
- Sleep Problems: Cancer survivors often experience long-term sleep disturbances, including insomnia, which significantly affects their quality of life.
- Weight Changes: Cancer treatments can lead to significant weight changes, including weight gain or loss, impacting overall health and recovery.
- Adrenal Insufficiency: Radiation and chemotherapy can cause adrenal insufficiency, leading to hormonal imbalances and requiring lifelong management.
- Chronic Inflammation: Cancer treatments can induce chronic inflammation, contributing to various long-term health issues and impacting overall well-being.
Living with Cancer
Living with cancer involves navigating a complex journey that affects various aspects of life. From managing medical treatments to seeking emotional support, it’s crucial to adopt strategies that can help improve overall well-being. Here are some key considerations for living with cancer:
1. Emotional Impact
Living with cancer profoundly affects individuals emotionally, often leading to increased levels of anxiety, depression, and uncertainty about the future. Emotional competence, which includes the ability to manage and express emotions effectively, plays a crucial role in how patients adjust to their diagnosis and treatment. For instance, young women with breast cancer who exhibit higher emotional competence tends to experience fewer symptoms of anxiety and depression, which in turn positively impacts their quality of life. Additionally, the emotional support received from family and friends significantly influences the psychological well-being of cancer patients, helping them cope better with the stress and emotional turmoil associated with the disease. The ongoing fear of disease progression or death, coupled with the hope for successful treatment outcomes, further underscores the complex emotional landscape that cancer patients navigate.
2. Support Systems
Support systems are vital for cancer patients, providing both emotional and practical assistance that can significantly improve their quality of life. Social support, particularly from family and friends, has been shown to enhance coping mechanisms and reduce psychological distress. Emotional support is especially crucial, as it directly impacts the patient’s sense of well-being and ability to manage the disease. Health care providers also play a critical role, offering not only medical care but also emotional and psychological support, which patients find particularly beneficial. The perception of family cohesiveness and the amount of social contact are key indicators of effective support systems, which help mediate the relationship between social support and overall adjustment to the illness. Interventions aimed at increasing emotional support can lead to significant improvements in the quality of life for cancer survivors.
3. Lifestyle Adjustments
These adjustments often include changes in diet, physical activity, and daily routines to accommodate treatment schedules and manage side effects. A whole person approach to cancer care, which addresses psychological, emotional, physical, and social needs, has been shown to facilitate these lifestyle changes and improve health-related quality of life. However, barriers such as lack of support from family and friends, time constraints, and the demands of returning to work can hinder the maintenance of healthy lifestyle changes. For family caregivers, providing end-of-life care at home can also lead to lifestyle interference and emotional distress, highlighting the need for comprehensive support systems that address both patient and caregiver needs. Understanding these challenges and providing targeted support can help cancer patients and their families better navigate the necessary lifestyle adjustments.
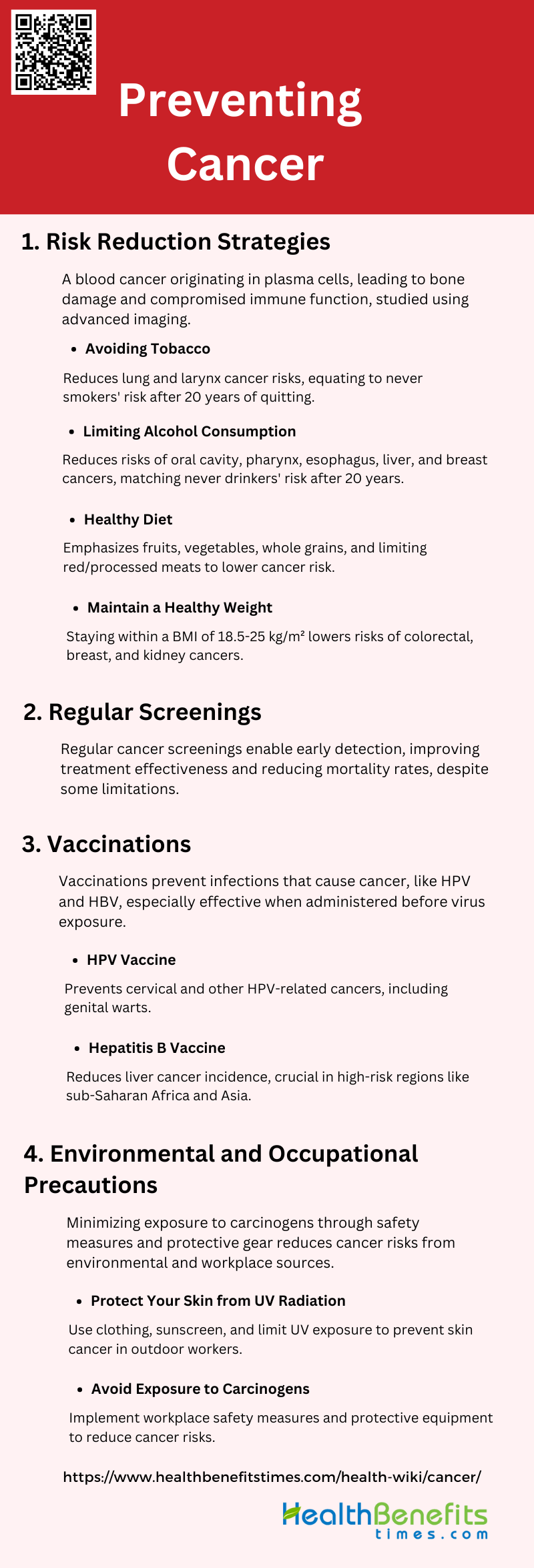
Preventing Cancer
Preventing cancer involves adopting lifestyle changes and practices that reduce the risk of developing the disease. These preventive measures can significantly lower the incidence of cancer and improve overall health. Below are some key strategies for preventing cancer:
1. Risk reduction strategies
Adopting a healthy lifestyle is crucial for reducing cancer risk. This includes maintaining a normal weight, following a plant-based diet, engaging in regular physical activity, and avoiding alcohol and tobacco. These measures can significantly lower the incidence of various cancers, including breast and colorectal cancer. Below are some risk reduction strategies:
- Avoiding Tobacco: Avoiding tobacco significantly reduces the risk of cancers, particularly lung and larynx cancers, with high attributable fractions. Quitting smoking can lower head and neck cancer risk to the level of never smokers after 20 years.
- Limiting Alcohol Consumption: Limiting alcohol consumption is crucial as it is linked to cancers of the oral cavity, pharynx, esophagus, liver, and breast. Quitting alcohol for over 20 years can reduce head and neck cancer risk to that of never drinkers.
- Healthy Diet: A healthy diet rich in fruits, vegetables, and whole grains, while limiting red and processed meats, can reduce cancer risk. Nutritional prevention is a priority, emphasizing balanced and diversified diets.
- Maintain a Healthy Weight: Maintaining a healthy weight within the BMI range of 18.5-25 kg/m² is essential to lower the risk of various cancers, including colorectal, breast, and kidney cancers. Overweight and obesity are significant risk factors.
2. Regular screenings
Regular cancer screenings are essential for early detection and reducing mortality rates. Screening methods for colorectal and gastric cancers, among others, can identify neoplastic lesions at early stages, making treatment more effective. Despite their limitations, these screenings are a powerful public health tool.
3. Vaccinations
Vaccinations play a significant role in cancer prevention. Universal vaccination against human papillomavirus (HPV) and hepatitis B virus (HBV) can prevent cancers associated with these infections. These vaccines are particularly effective when administered before exposure to the viruses, typically in adolescence. Below is common two types list of Vaccinations:
- HPV Vaccine: The HPV vaccine is highly effective in preventing cervical and other HPV-related cancers, including genital warts.
- Hepatitis B Vaccine: The Hepatitis B vaccine significantly reduces liver cancer incidence, especially in high-risk regions like sub-Saharan Africa and Asia.
4. Environmental and Occupational Precautions
Reducing exposure to environmental and occupational carcinogens is vital for cancer prevention. This includes avoiding harmful chemicals, using protective gear, and adhering to safety regulations. Public health policies and educational campaigns can further support these efforts, minimizing cancer risk from environmental sources. Below is common two types list of Environmental and Occupational Precautions:
- Protect Your Skin from UV Radiation: Outdoor workers are at a high risk of developing skin cancer due to prolonged exposure to solar ultraviolet radiation (UVR). Effective prevention strategies include wearing suitable clothing, using sunscreen, and reducing direct UV exposure.
- Avoid Exposure to Carcinogens: Minimizing exposure to carcinogens in the workplace is crucial for cancer prevention. Employers should implement safety measures, provide protective equipment, and conduct regular screenings to identify and mitigate risks.
Info-graphics
Types of Cancer
1. Common Types of Cancer: Several cancers are prevalent, each affecting different body parts, with unique symptoms and treatments.
- Breast Cancer: Frequently diagnosed, projected to remain prevalent, and a common primary site for uterine corpus metastasis.
- Lung and Bronchus Cancer: Leading cancer killer, with high incidence in older adults and a common primary metastasizing cancer.
- Prostate Cancer: A prevalent cancer with significant heritability, less frequent in diabetic males.
- Colorectal Cancer: Common, projected to be surpassed by thyroid cancer, frequently metastasizes to the uterine corpus.
- Melanoma of the Skin: Projected to become common by 2030, with a significant genetic component, can metastasize to the uterine corpus.
- Bladder Cancer: Lower risk in diabetic patients, small genetic component, can metastasize to the uterine corpus.
- Non-Hodgkin Lymphoma: Common primary metastasizing cancer, genetic component less clear.
- Kidney and Renal Pelvis Cancer: Significant genetic component, moderate risk in diabetic patients, common urological tumor.
- Endometrial Cancer: Projected to be common by 2030, significant genetic component, high risk in diabetic patients.
- Pancreatic Cancer: Leading cause of cancer-related death by 2030, significant genetic component, high risk in diabetic patients.
- Thyroid Cancer: Projected fourth leading cancer by 2030, can metastasize to the uterine corpus.
- Liver and Intrahepatic Bile Duct Cancer: Leading cause of cancer-related death by 2030, worst prognosis among cancers with uncommon site metastasis, high risk in diabetic patients.
2. Rare Types of Cancer: Rare cancers affect fewer people but require specialized treatment and research due to their unique characteristics.
- Pancreatic Cancer: Pancreatic gastrointestinal stromal tumors (PGISTs) are exceptionally rare, highlighting the importance of early diagnosis and intervention.
- Leukemia: Blood cancer marked by rapid abnormal white blood cell production, treated with chemotherapy, radiation, and stem cell transplants.
- Lymphoma: Cancer of the lymphatic system, categorized into Hodgkin and non-Hodgkin, treated with chemotherapy, radiation, and targeted therapies.
- Appendix Cancer: Rare, varying in histology, commonly neuroendocrine tumors, treated with surgical resection and adjuvant therapy.
- Gastrointestinal Stromal Tumor (GIST): Rare mesenchymal tumors diagnosed through immunohistochemical analysis, treated with surgical resection and targeted therapy.
- Ocular (Eye) Melanoma: Rare pigment-producing eye cancer, treated with radiation, laser therapy, and surgical removal.
- Salivary Gland Cancer: Rare, presenting as painless lumps, treated with surgical resection, radiation, or chemotherapy.
- Small Bowel Cancer: Rare, mostly neuroendocrine tumors, treated with surgical resection and adjuvant therapy based on histology and stage.
- Soft Tissue Sarcomas: Diverse group of rare connective tissue cancers, challenging to treat, requiring surgical resection, radiation, and sometimes chemotherapy.