Bones are dynamic, living tissues that form the structural framework of the human body, providing support, protection, and enabling movement. Composed primarily of collagen and calcium phosphate, bones are remarkably strong yet lightweight. They house bone marrow, which produces blood cells, and serve as a reservoir for essential minerals like calcium and phosphorus. Contrary to the common misconception that bones are inert, they are highly active, constantly undergoing remodeling through the actions of osteoblasts (cells that build bone) and osteoclasts (cells that break down bone). This continuous process allows bones to adapt to stress, repair themselves, and maintain mineral homeostasis.
Anatomy of Bones
The human skeletal system is a complex framework of bones that provides structure, protection, and support to the body. Understanding the anatomy of bones involves exploring their structure, composition, and the various types of cells that contribute to bone health and function. Below is a detailed examination of these aspects:
1. Structure and Composition
Bone is a specialized connective tissue characterized by a mineralized organic matrix that provides both strength and flexibility. The primary components of bone include collagen, which forms the organic matrix, and hydroxyapatite, a crystalline mineral that provides rigidity. The bone matrix is produced by osteoblasts, which secrete collagen and other non-collagenous proteins, and subsequently mineralize the matrix with hydroxyapatite. The bone matrix is organized into a highly structured composite, with collagen fibers arranged in layers that alternate in orientation to withstand stress from various directions. This sophisticated structure allows bones to be strong and lightweight, capable of supporting the body’s weight while facilitating movement.
2. Bone Cells
Bone cells play crucial roles in the formation, maintenance, and remodeling of bone tissue. Osteoblasts are responsible for bone formation; they secrete the organic components of the bone matrix and initiate its mineralization. Once embedded in the matrix, osteoblasts differentiate into osteocytes, which are the most abundant bone cells and act as mechanosensors, regulating bone remodeling in response to mechanical stress. Osteocytes form an extensive network within the bone matrix, communicating with each other and with surface cells to maintain bone homeostasis. Osteoclasts, on the other hand, are large, multinucleated cells that resorb bone, breaking down the mineralized matrix to release calcium and phosphate into the bloodstream. The coordinated activity of these three cell types ensures the dynamic balance of bone formation and resorption, essential for bone health and adaptation to mechanical and physiological demands.
Types of bones
Bones in the human body come in various shapes and sizes, each serving unique functions. They can be classified into several categories based on their shapes and structures. Below is a detailed examination of these types:
1. Long Bones
Long bones are characterized by their elongated shape and are primarily found in the appendicular skeleton. They include bones such as the clavicles, humeri, radii, ulnae, metacarpals, femurs, tibiae, fibulae, metatarsals, and phalanges. These bones are crucial for movement and support, acting as levers that muscles pull on to produce motion. Structurally, long bones consist of a hollow shaft known as the diaphysis, flared metaphyses, and rounded epiphyses. The diaphysis is mainly composed of dense cortical bone, while the metaphysis and epiphysis contain trabecular bone surrounded by a thin layer of cortical bone. This composition allows long bones to withstand various mechanical stresses and contribute to the overall strength and stability of the skeleton.
2. Short Bones
Short bones are typically as wide as they are long, providing stability and support with little movement. Examples of short bones include the carpal bones in the wrist and the tarsal bones in the ankle. These bones are primarily composed of spongy bone covered by a thin layer of compact bone, which helps them absorb shock and distribute forces evenly. Short bones play a crucial role in complex joint movements and are essential for the fine motor skills of the hands and feet. Additionally, the patellae and sesamoid bones, which are embedded within tendons, are also classified as short bones due to their similar structure and function.
3. Flat Bones
Flat bones are thin, flattened, and usually curved, providing extensive surfaces for muscle attachment and protection for underlying organs. Examples include the skull, mandible, scapulae, sternum, and ribs. These bones are formed primarily through membranous ossification, a process where bone develops directly from sheets of mesenchymal connective tissue. Flat bones consist of two layers of compact bone with a layer of spongy bone in between, which helps absorb impact and protect vital organs such as the brain, heart, and lungs. Their structure also allows for the attachment of muscles that facilitate movement and maintain posture.
4. Irregular Bones
Irregular bones have complex shapes that do not fit into the other bone categories. They include the vertebrae, sacrum, coccyx, and hyoid bone. These bones are primarily composed of spongy bone enclosed by a thin layer of compact bone. Irregular bones serve various functions, such as protecting the spinal cord (vertebrae), supporting the weight of the body (sacrum), and providing attachment points for muscles and ligaments (hyoid bone). Their unique shapes are adapted to their specific roles in the body, contributing to the overall structural integrity and functionality of the skeletal system.
5. Sesamoid Bones
Sesamoid bones are small, round bones embedded within tendons, typically found near joints. The most well-known sesamoid bone is the patella (kneecap), but others include the pisiform in the wrist and various small sesamoids in the hands and feet. These bones form in response to mechanical stress and help reduce friction, modify pressure, and protect tendons from wear and tear. Sesamoid bones originate from Sox9+/Scx+ progenitors and develop under the regulation of TGFβ, independent of mechanical stimuli from muscles. They play a crucial role in joint stability and function, highlighting their evolutionary plasticity and importance in the musculoskeletal system.
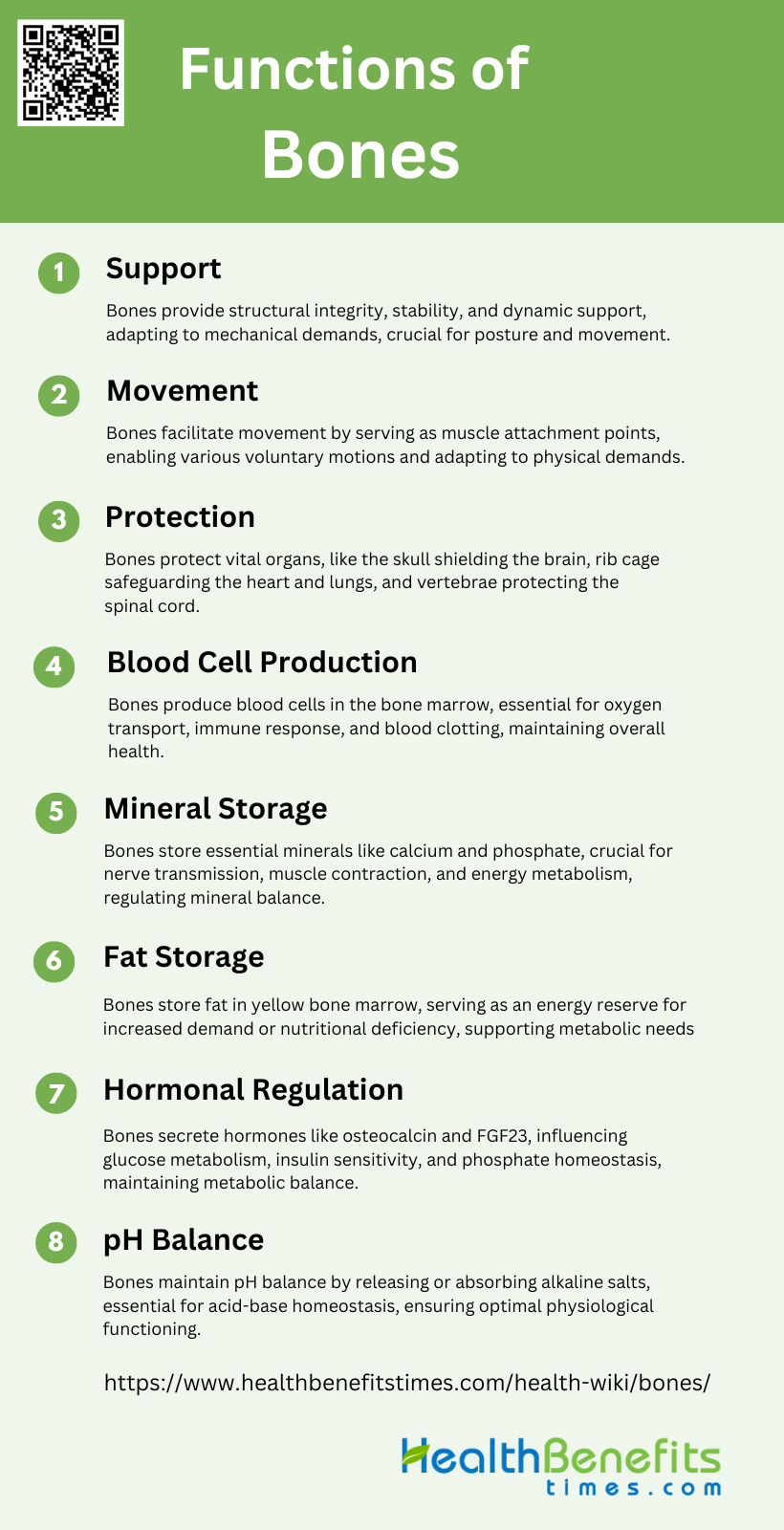
Functions of Bones
Bones play several critical roles in the human body, from providing structural support to facilitating movement and protecting vital organs. They also serve as a reservoir for minerals and play a key role in blood cell production. Below is a detailed examination of these functions:
1. Support
Bones provide the fundamental framework for the human body, ensuring structural integrity and stability. This mechanical support is crucial for maintaining posture and enabling locomotion. The skeleton’s mineralized structure withstands functional load-bearing and opposes muscular contraction, facilitating movement. Additionally, bones adapt to mechanical demands, enhancing their strength and resilience during growth and physical activity. This dynamic nature of bone tissue underscores its role in providing robust support throughout an individual’s life.
2. Movement
Bones play a pivotal role in facilitating movement by serving as attachment points for muscles. When muscles contract, they pull on bones, creating motion. This interaction between bones and muscles is essential for all voluntary movements, from walking to complex athletic activities. The skeletal system’s ability to remodel and adapt to physical demands ensures that bones remain strong and capable of supporting various types of movement throughout life. This intricate relationship between bones and muscles highlights the importance of the skeletal system in enabling mobility.
3. Protection
One of the primary functions of bones is to protect vital internal organs from injury. The skull encases the brain, the rib cage shields the heart and lungs, and the vertebrae safeguard the spinal cord. This protective role is crucial for maintaining the body’s overall health and functionality. The mineralized structure of bones provides a sturdy barrier against external forces, ensuring that delicate organs remain safe from harm. This protective function underscores the importance of a healthy skeletal system in preserving life and well-being.
4. Blood Cell Production
Bones are integral to the production of blood cells through a process known as hematopoiesis. This occurs in the bone marrow, a specialized tissue found within the cavities of certain bones. The bone marrow produces red blood cells, white blood cells, and platelets, which are essential for oxygen transport, immune response, and blood clotting, respectively. This function highlights the critical role of bones in maintaining the body’s overall health and homeostasis by ensuring a continuous supply of vital blood cells.
5. Mineral Storage
Bones serve as a reservoir for essential minerals, particularly calcium and phosphate. These minerals are crucial for various physiological processes, including nerve transmission, muscle contraction, and energy metabolism. The skeleton’s ability to store and release these minerals helps maintain their balance in the bloodstream, ensuring that the body functions optimally. This storage capability underscores the importance of bones in regulating mineral homeostasis and supporting overall metabolic health.
6. Fat Storage
In addition to mineral storage, bones also store fat within the yellow bone marrow. This fat serves as an energy reserve that the body can utilize during periods of increased energy demand or nutritional deficiency. The presence of adipocytes in the bone marrow highlights the multifaceted role of bones in energy metabolism and storage. This function is particularly important for maintaining energy balance and supporting the body’s metabolic needs during various physiological states.
7. Hormonal Regulation
Bones function as an endocrine organ by secreting hormones that regulate various physiological processes. Key hormones include osteocalcin, which influences glucose metabolism and insulin sensitivity, and fibroblast growth factor 23 (FGF23), which regulates phosphate homeostasis. These hormones enable bones to communicate with other organs, thereby playing a crucial role in maintaining systemic metabolic balance. This endocrine function of bones underscores their importance beyond structural support, highlighting their role in overall health and disease prevention.
8. pH Balance
Bones contribute to maintaining the body’s pH balance by acting as a buffer system. They can release or absorb alkaline salts, such as calcium phosphate, to neutralize excess acids or bases in the bloodstream. This buffering capacity is essential for maintaining the body’s acid-base homeostasis, which is crucial for normal cellular function and overall metabolic health. The ability of bones to regulate pH balance underscores their importance in ensuring the body’s internal environment remains stable and conducive to optimal physiological functioning.
Factors affecting bone growth
Bone growth is influenced by a variety of factors, including genetics, nutrition, physical activity, and hormonal levels. Understanding these factors is crucial for maintaining healthy bone development and preventing disorders. Below is a detailed examination of these factors:
1. Genetic Factors
Genetic factors play a crucial role in determining bone growth and development. Studies have shown that up to 60-80% of the variance in peak bone mass is attributable to genetic factors. These genetic influences affect bone cell function, cartilage quality, calcium and vitamin D homeostasis, and sex hormone metabolism. Family and twin studies have consistently demonstrated the significant heritability of bone density, suggesting that genetic predisposition is a major determinant of bone health. Understanding the genetic basis of bone growth can help in identifying individuals at risk for metabolic and developmental bone diseases and in developing targeted interventions.
2. Hormones
Hormones are vital regulators of bone growth, influencing both the replication and differentiation of bone cells. Insulin-like growth factors (IGFs), growth hormone (GH), and sex steroids are among the key hormones involved in this process. IGFs, particularly IGF-I, have been shown to stimulate both bone cell replication and differentiation, making them critical for bone formation during growth periods. GH/IGF-I axis is essential for puberty-induced bone growth, with IGF-I playing a more significant role than IGF-II or GH alone. Hormonal imbalances can lead to various bone growth disorders, emphasizing the need for hormonal regulation in maintaining bone health.
3. Nutrition
Nutrition significantly impacts bone growth and health, with adequate intake of calcium, vitamin D, and protein being essential for optimal bone development. Nutritional factors influence bone modeling and remodeling processes, either directly or through changes in hormone secretion and action. Studies have shown that modifying environmental factors like nutrition can positively influence peak bone mass, thereby reducing the risk of fragility fractures later in life. Nutritional deficiencies during critical growth periods can lead to suboptimal bone mass acquisition, highlighting the importance of a balanced diet for bone health.
4. Physical Activity and Mechanical Loading
Physical activity and mechanical loading are crucial for bone growth and strength. Mechanical stress stimulates bone formation by promoting osteoblast activity and enhancing bone density. Exercise during growth periods has been shown to positively influence peak bone mass, with weight-bearing activities being particularly beneficial. The interaction between physical activity and genetic factors can further enhance bone growth, suggesting that an active lifestyle can help in achieving optimal bone density. Mechanical loading also regulates periosteal apposition, contributing to bone growth in width.
5. Growth Factors
Growth factors such as IGFs, transforming growth factor-betas (TGF-betas), and bone morphogenetic proteins (BMPs) play a significant role in bone growth and repair. These growth factors are produced by osteoblasts and other bone cells, influencing osteoblast proliferation and differentiation. They are incorporated into the bone matrix and retain activity, thereby regulating local bone formation. IGFs, in particular, are critical for bone accretion during growth periods, with IGF-I being more influential than IGF-II. Understanding the role of these growth factors can aid in developing therapies for enhancing bone growth and repair.
6. Environmental Factors
Environmental factors, including lifestyle choices and exposure to risk factors, significantly influence bone growth and health. Factors such as alcohol consumption, smoking, and certain medications can negatively impact bone density and increase the risk of fractures. Additionally, environmental influences interact with genetic factors to either enhance or inhibit bone growth, suggesting a complex interplay between genes and the environment. Modifying these environmental factors through lifestyle changes and interventions can help in achieving optimal bone health and reducing the risk of bone-related diseases.
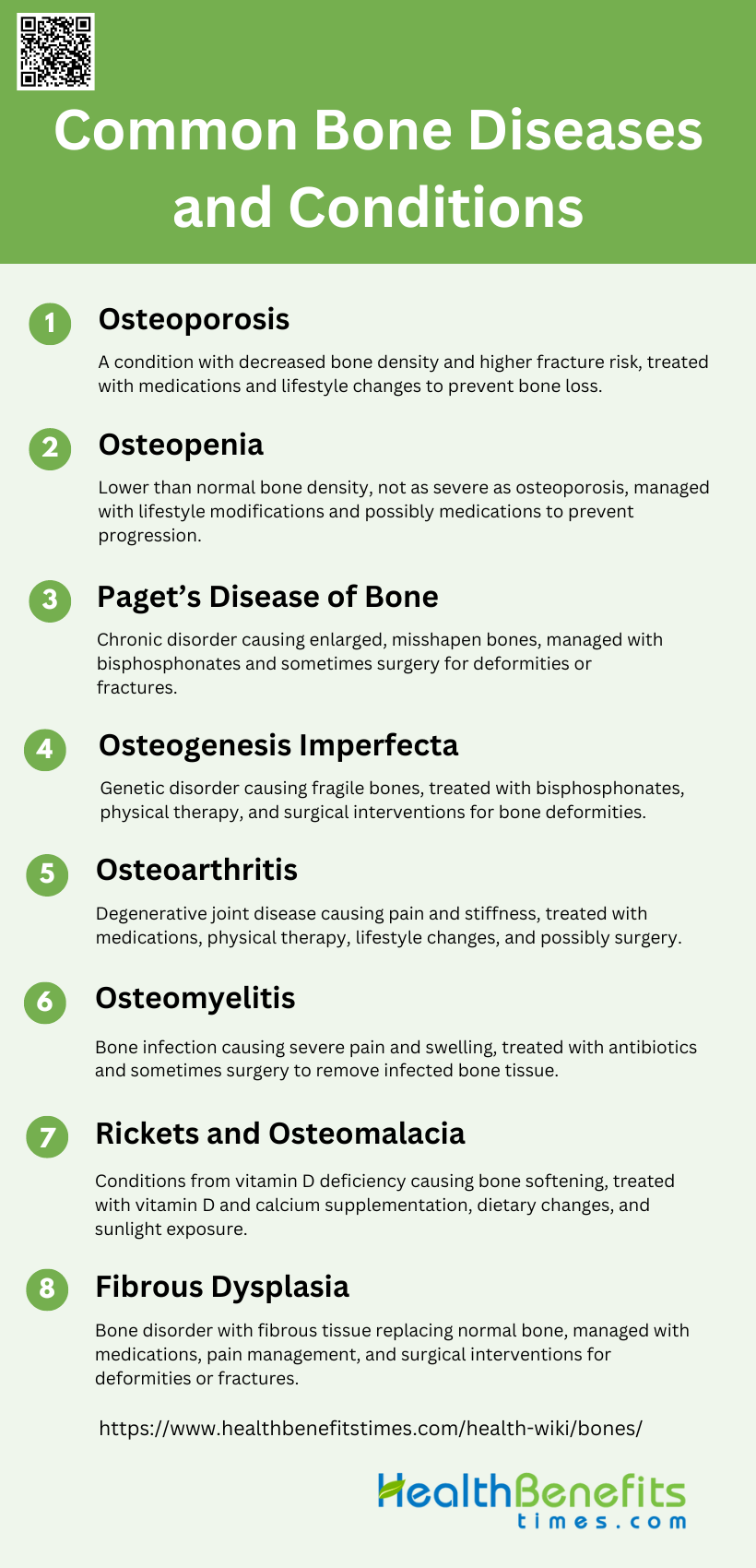
Common Bone Diseases and Conditions
Bones are essential to our body’s structure and function, but they can be affected by various diseases and conditions. Understanding these common bone diseases is crucial for early detection and treatment. Below is a list of some prevalent bone diseases and conditions:
1. Osteoporosis
Osteoporosis is a common metabolic bone disease characterized by decreased bone density and increased fracture risk. Symptoms often include back pain, loss of height over time, a stooped posture, and bones that break more easily than expected. Treatments focus on preventing bone loss and fractures, and include medications such as bisphosphonates, denosumab, and selective estrogen receptor modulators (SERMs). Lifestyle changes like increased physical activity, calcium and vitamin D supplementation, and avoiding smoking and excessive alcohol consumption are also recommended.
2. Osteopenia
Osteopenia is a condition where bone mineral density is lower than normal but not low enough to be classified as osteoporosis. It is often asymptomatic and is usually detected through bone density scans. The primary goal in managing osteopenia is to prevent progression to osteoporosis. This can be achieved through lifestyle modifications such as weight-bearing exercises, adequate intake of calcium and vitamin D, and avoiding smoking and excessive alcohol. In some cases, medications may be prescribed to strengthen bone density.
3. Paget’s Disease of Bone
Paget’s disease of bone is a chronic disorder that can result in enlarged and misshapen bones. It is characterized by excessive bone resorption followed by an increase in bone formation, leading to structurally disorganized bone. Symptoms may include bone pain, deformities, and fractures. Treatments often involve bisphosphonates to regulate bone remodeling and pain management strategies. In severe cases, surgery may be required to correct bone deformities or fractures.
4. Osteogenesis Imperfecta
Osteogenesis Imperfecta (OI) is a genetic disorder characterized by fragile bones that break easily, often with little or no apparent cause. It is caused by mutations in the genes responsible for collagen production. Symptoms can include frequent fractures, bone deformities, and short stature. Treatment focuses on managing symptoms and may include bisphosphonates to increase bone density, physical therapy, and surgical interventions to correct bone deformities. Newer treatments are being explored, such as sclerostin inhibitory antibodies and TGF beta inhibition.
5. Osteoarthritis
Osteoarthritis is a degenerative joint disease characterized by the breakdown of cartilage, leading to pain, stiffness, and reduced joint mobility. Commonly affected areas include the knees, hips, and hands. Treatment options aim to relieve symptoms and improve joint function and include pain relievers, anti-inflammatory medications, physical therapy, and in severe cases, joint replacement surgery. Lifestyle changes such as weight management and regular exercise are also beneficial.
6. Osteomyelitis
Osteomyelitis is an infection of the bone, typically caused by bacteria. Symptoms include severe bone pain, fever, and swelling over the affected area. Treatment usually involves antibiotics to eradicate the infection, and in some cases, surgical intervention may be necessary to remove infected bone tissue. Early diagnosis and treatment are crucial to prevent complications such as chronic infection or bone necrosis.
7. Rickets and Osteomalacia
Rickets and osteomalacia are conditions caused by vitamin D deficiency, leading to softening of the bones. Rickets affects children and results in bone deformities, while osteomalacia affects adults and causes bone pain and muscle weakness. Treatment involves correcting the deficiency through vitamin D and calcium supplementation, dietary changes, and exposure to sunlight. In severe cases, additional treatments may be required to address bone deformities.
8. Fibrous Dysplasia
Fibrous dysplasia is a bone disorder where normal bone is replaced with fibrous tissue, leading to weak, deformed bones. It can affect one bone (monostotic) or multiple bones (polyostotic). Symptoms include bone pain, deformities, and fractures. Treatment focuses on managing symptoms and may include medications like bisphosphonates to strengthen bones, pain management, and surgical interventions to correct deformities or stabilize fractures. In cases associated with McCune-Albright syndrome, additional endocrine treatments may be necessary.
Preventative measures of Bones
Ensuring strong and healthy bones requires proactive steps and lifestyle choices. By adopting preventative measures, you can significantly reduce the risk of bone-related issues. Here are some essential strategies to maintain optimal bone health:
1. Adequate Calcium Intake
Adequate calcium intake is essential for maintaining bone health and preventing osteoporosis. Calcium is a critical component of bone tissue, and its deficiency can lead to weakened bones and increased fracture risk. Studies have shown that a daily intake of calcium, particularly from dairy products, is associated with higher bone mineral density and reduced risk of fractures. The National Osteoporosis Foundation recommends calcium intake as a key factor in achieving peak bone mass during youth and maintaining bone health throughout life. Additionally, calcium supplements may be necessary for individuals with low dietary calcium intake, although their use should be carefully considered due to potential side effects.
2. Sufficient Vitamin D
Vitamin D plays a crucial role in bone health by facilitating calcium absorption in the gut and maintaining adequate serum calcium and phosphate levels for bone formation. Insufficient vitamin D can lead to bone disorders such as rickets in children and osteomalacia in adults. Research indicates that adequate vitamin D levels are necessary to prevent osteoporosis and related fractures, especially in older adults. The European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis recommends a daily intake of 800 IU of vitamin D to maintain optimal bone health in postmenopausal women. Sun exposure and dietary sources such as fatty fish and fortified foods are important for maintaining sufficient vitamin D levels.
3. Eat a Balanced Diet
A balanced diet rich in essential nutrients is vital for bone health. Nutrients such as magnesium, potassium, vitamin C, vitamin K, and protein have been shown to support bone structure and function. Consuming a variety of fruits, vegetables, dairy products, and lean proteins can provide these necessary nutrients. Observational studies have linked higher dietary protein intake with improved bone mineral density and reduced fracture risk, provided that calcium intake is sufficient. Adherence to dietary patterns like the Mediterranean diet, which emphasizes fruits, vegetables, whole grains, and healthy fats, is associated with lower fracture risk and better overall bone health.
4. Exercise Regularly
Regular physical activity, particularly weight-bearing and resistance exercises, is essential for maintaining bone density and strength. Exercise stimulates bone formation and slows bone loss, making it a critical component of osteoporosis prevention and treatment. Activities such as walking, running, and strength training have been shown to improve bone mineral density and reduce the risk of fractures. The National Osteoporosis Foundation highlights the importance of physical activity in achieving peak bone mass during youth and maintaining bone health throughout life. For older adults, regular exercise can help maintain muscle mass and balance, reducing the risk of falls and fractures.
5. Maintain a Healthy Lifestyle
Maintaining a healthy lifestyle, including avoiding smoking and limiting alcohol consumption, is crucial for bone health. Smoking and excessive alcohol intakes have been shown to have adverse effects on bone density and increase the risk of fractures. A healthy body weight, achieved through a balanced diet and regular exercise, also supports bone health. The National Osteoporosis Foundation emphasizes the importance of lifestyle choices in achieving and maintaining peak bone mass. Additionally, avoiding cola beverages and ensuring adequate nutrient intake can further support bone health.
6. Ensure Proper Nutrition throughout Life
Proper nutrition throughout life is essential for maintaining bone health and preventing osteoporosis. Nutritional needs for bone health change with age, and it is important to ensure adequate intake of calcium, vitamin D, and other bone-supporting nutrients at all life stages. For children and adolescents, adequate nutrition is crucial for achieving peak bone mass, which can reduce the risk of osteoporosis later in life. For older adults, maintaining a balanced diet with sufficient protein, calcium, and vitamin D is important for preserving bone density and preventing fractures. Tailored prevention strategies focusing on nutrition can help individuals at high risk of osteoporosis maintain good bone health.
Interesting Facts about Bones
Bones are fascinating structures that play a crucial role in our bodies. They not only provide support and protection but also have unique characteristics and functions. Here are some interesting facts about bones:
1. Number of Bones
The human skeleton is composed of 206 bones in adulthood, although this number is higher in infants due to the presence of additional bones that fuse together as one ages. These bones provide structural support, facilitate movement, and protect vital organs. The skeleton also serves as a reservoir for minerals such as calcium and phosphorus, which are essential for various bodily functions.
2. Bone Composition
Bones are dynamic tissues composed of a matrix of collagen fibers and mineral deposits, primarily hydroxyapatite, which provide both flexibility and strength. The extracellular matrix of bone includes collagenous and non-collagenous proteins that play crucial roles in bone formation and mineralization. Additionally, bones contain small amounts of lipids, which are important for bone physiology and health.
3. Bone Marrow
Bone marrow is a vital component of bones, housed within the medullary cavities. It is responsible for the production of blood cells, including red blood cells, white blood cells, and platelets. The bone marrow also contains adipocytes and hematopoietic stem cells, which are essential for the continuous renewal of blood cells and the maintenance of bone health.
4. Bone Remodeling
Bone remodeling is a continuous process involving the resorption of old bone by osteoclasts and the formation of new bone by osteoblasts. This process is crucial for maintaining bone strength and integrity, adapting to mechanical stress, and repairing micro-damages. The remodeling cycle is regulated by various systemic and local factors, including hormones, cytokines, and mechanical stimuli.
5. Smallest and Largest Bones
The smallest bone in the human body is the stapes, located in the middle ear, which measures about 3 mm in length. The largest bone is the femur, or thigh bone, which is crucial for supporting the body’s weight and enabling locomotion. These bones exemplify the diverse functions and sizes of bones within the human skeleton.
6. Bone Density and Strength
Bone density and strength are determined by the composition and structure of the bone matrix, as well as the balance between bone resorption and formation. Mechanical loading and physical activity are key factors that enhance bone strength by stimulating bone formation and inhibiting bone loss. Age-related changes and hormonal imbalances can negatively impact bone density, leading to conditions such as osteoporosis.
7. Bone Health and Lifestyle
Maintaining bone health requires a combination of proper nutrition, regular physical activity, and lifestyle choices. Adequate intake of calcium and vitamin D, along with weight-bearing exercises, can help preserve bone density and prevent bone-related diseases. Avoiding smoking and excessive alcohol consumption also contributes to better bone health and reduces the risk of fractures.