Blood pressure is the force exerthttps://www.healthbenefitstimes.com/health-wiki/blood-pressure/ed by circulating blood on the walls of the arteries as the heart pumps it throughout the body. It is measured using two values: systolic pressure, which is the maximum pressure during a heartbeat, and diastolic pressure, the minimum pressure between heartbeats. Blood pressure is expressed in millimeters of mercury (mmHg) and typically recorded as systolic over diastolic, such as 120/80 mmHg. Maintaining normal blood pressure is crucial for overall health, as both high blood pressure (hypertension) and low blood pressure (hypotension) can lead to serious health issues, including heart disease, stroke, and kidney problems.
How Blood Pressure is measured
It is a critical indicator of cardiovascular health and is measured using a device called a sphygmomanometer. This process involves several steps to ensure accurate readings. Here are the steps involved in measuring blood pressure:
1. Instruments Used
Blood pressure (BP) measurement relies on various instruments, each with its own advantages and limitations. The traditional mercury sphygmomanometer, used with the auscultatory method, remains a gold standard due to its accuracy, though its use is declining due to environmental concerns. Aneroid devices, which require frequent calibration, and hybrid devices that use electronic transducers instead of mercury, are also common alternatives. Oscillometric devices, which measure BP automatically, are widely used in clinical settings due to their ease of use and ability to reduce human error. Additionally, cuffless BP estimation algorithms based on pulse arrival time (PAT) are emerging as promising tools for continuous BP monitoring. Each instrument must be validated according to standardized protocols to ensure accuracy.
2. Procedure for Accurate Measurement
Accurate BP measurement requires adherence to specific procedures to minimize errors. The patient should be seated comfortably with their back supported, legs uncrossed, and the arm supported at heart level. A properly sized cuff should be used, as an incorrect cuff size can lead to significant measurement errors. The patient should rest for at least five minutes before the measurement, and factors such as recent physical activity, caffeine intake, and stress should be controlled. Multiple readings should be taken, and the average of these readings should be used to obtain a more accurate assessment. Training of healthcare providers in the correct measurement techniques and regular calibration of devices are also crucial for ensuring accurate BP readings.
3. Interpreting Results
Interpreting BP results involves understanding the context in which the measurements were taken and recognizing potential sources of error. Office BP measurements can differ significantly from those taken in other settings, such as at home or through ambulatory monitoring, which can provide a more comprehensive picture of an individual’s BP profile. White-coat hypertension, where BP is elevated in a clinical setting but normal at home, and masked hypertension, where BP is normal in a clinical setting but elevated at home, is important considerations. High nighttime BP, detected through ambulatory monitoring, is associated with increased cardiovascular risk. Therefore, a single BP reading should be interpreted with caution, and further measurements should be taken to confirm any abnormal values. Understanding these nuances is essential for accurate diagnosis and effective management of hypertension.
Normal vs. Abnormal Blood Pressure
Understanding the difference between normal and abnormal blood pressure is crucial for maintaining cardiovascular health. Blood pressure readings are categorized to help identify potential health risks. Here are the categories of blood pressure readings:
1. Normal Blood Pressure Range
Normal blood pressure is typically defined by systolic blood pressure (SBP) and diastolic blood pressure (DBP) measurements. According to the Joint National Committee on the Detection, Evaluation, and Treatment of High Blood Pressure, a normal DBP is 84 mmHg or less, while 85-89 mmHg is considered high-normal. SBP in the range of 120-140 mmHg is associated with the lowest cardiovascular risk, particularly when DBP is maintained between 70-80 mmHg. This range is crucial for minimizing the risk of cardiovascular events and ensuring optimal health outcomes.
2. High Blood Pressure
High blood pressure, or hypertension, is defined as a DBP of 90 mmHg or above. Causes of high blood pressure include genetic factors, poor diet, and lack of physical activity, obesity, and excessive alcohol consumption. Symptoms may not always be apparent but can include headaches, shortness of breath, and nosebleeds. High blood pressure significantly increases the risk of cardiovascular events such as stroke, myocardial infarction, and heart failure. Effective management often involves lifestyle changes and medication to reduce these risks.
3. Low Blood Pressure
Low blood pressure, or hypotension, is typically defined as a DBP below 70 mmHg. Causes can include dehydration, prolonged bed rest, nutritional deficiencies, and certain medical conditions such as heart problems or endocrine disorders. Symptoms of low blood pressure can include dizziness, fainting, blurred vision, and fatigue. While low blood pressure is often less concerning than high blood pressure, it can still pose significant health risks, particularly in older adults or those with underlying health conditions. Maintaining a balanced DBP is essential for reducing the risk of adverse cardiovascular outcomes.
Factors Affecting Blood Pressure
Blood pressure is influenced by a variety of factors that can either elevate or lower it. Understanding these factors is crucial for maintaining cardiovascular health and preventing hypertension. Below are some of the key elements that affect blood pressure:
1. Diet
Diet plays a crucial role in managing blood pressure. Studies have shown that dietary patterns such as the Dietary Approaches to Stop Hypertension (DASH) diet, Nordic diet, and Mediterranean diet significantly lower both systolic and diastolic blood pressure. These diets are rich in fruits, vegetables, whole grains, legumes, seeds, nuts, fish, and dairy, while being low in meat, sweets, and alcohol. Additionally, reducing sodium intake and increasing potassium intake are effective strategies for lowering blood pressure, particularly in black and older individuals.
2. Physical Activity
Regular physical activity is essential for maintaining healthy blood pressure levels. Engaging in moderate-intensity exercise, such as brisk walking, for at least 150 minutes per week can help reduce systolic and diastolic blood pressure. Physical activity helps improve heart health, reduce stress, and promote weight loss, all of which contribute to lower blood pressure. Studies have shown that combining physical activity with dietary changes, such as the DASH diet, can lead to even greater reductions in blood pressure.
3. Stress
Stress and anxiety are significant contributors to elevated blood pressure. Chronic stress can lead to long-term hypertension, which increases the risk of cardiovascular diseases. Work-related stress, in particular, has been identified as a major risk factor for hypertension. Managing stress through relaxation techniques, mindfulness, and regular physical activity can help mitigate its impact on blood pressure. Addressing mental health issues such as anxiety and depression is also crucial for maintaining healthy blood pressure levels.
4. Weight
Maintaining a healthy weight is vital for blood pressure control. Obesity is a major risk factor for hypertension, with studies indicating that it may be responsible for 40% to 78% of hypertension cases. Weight loss through dietary modifications and increased physical activity can lead to significant reductions in blood pressure. The POUNDS Lost trial demonstrated that participants with lower genetic risk for high blood pressure had better control of their blood pressure after diet-induced weight loss. Weight loss also improves metabolic profiles and reduces the activation of the renin-angiotensin-aldosterone system and the sympathetic nervous system.
5. Age
Age is a non-modifiable risk factor for hypertension. Blood pressure tends to increase with age due to the stiffening of arteries and the accumulation of risk factors over time. Preventing age-related increases in blood pressure can significantly reduce the risk of cardiovascular diseases. Lifestyle modifications, such as a healthy diet and regular physical activity, can help mitigate the impact of aging on blood pressure. Older individuals can make and sustain dietary changes that lower blood pressure, thereby reducing their risk of hypertension-related complications.
6. Genetics
Genetic predisposition plays a significant role in determining an individual’s risk of developing hypertension. Over 314 genetic variants have been identified to be associated with blood pressure levels. Individuals with a higher number of these genetic variants tend to have higher blood pressure and a more rapid increase in blood pressure with aging. However, healthy lifestyle choices, such as a balanced diet and regular exercise, can offset the adverse effects of genetic susceptibility to high blood pressure. Population-wide efforts to lower blood pressure through lifestyle modifications are essential for managing genetic risk.
7. Medications
Medications are often necessary for individuals with hypertension that cannot be controlled through lifestyle changes alone. Antihypertensive drugs, such as diuretics, beta-blockers, ACE inhibitors, and calcium channel blockers, are commonly prescribed to manage high blood pressure. These medications work through various mechanisms to lower blood pressure and reduce the risk of cardiovascular events. Adherence to prescribed medications, along with lifestyle modifications, is crucial for effective blood pressure control. The Chronic Care Model emphasizes a collaborative approach among patients, providers, and health systems to optimize hypertension management.
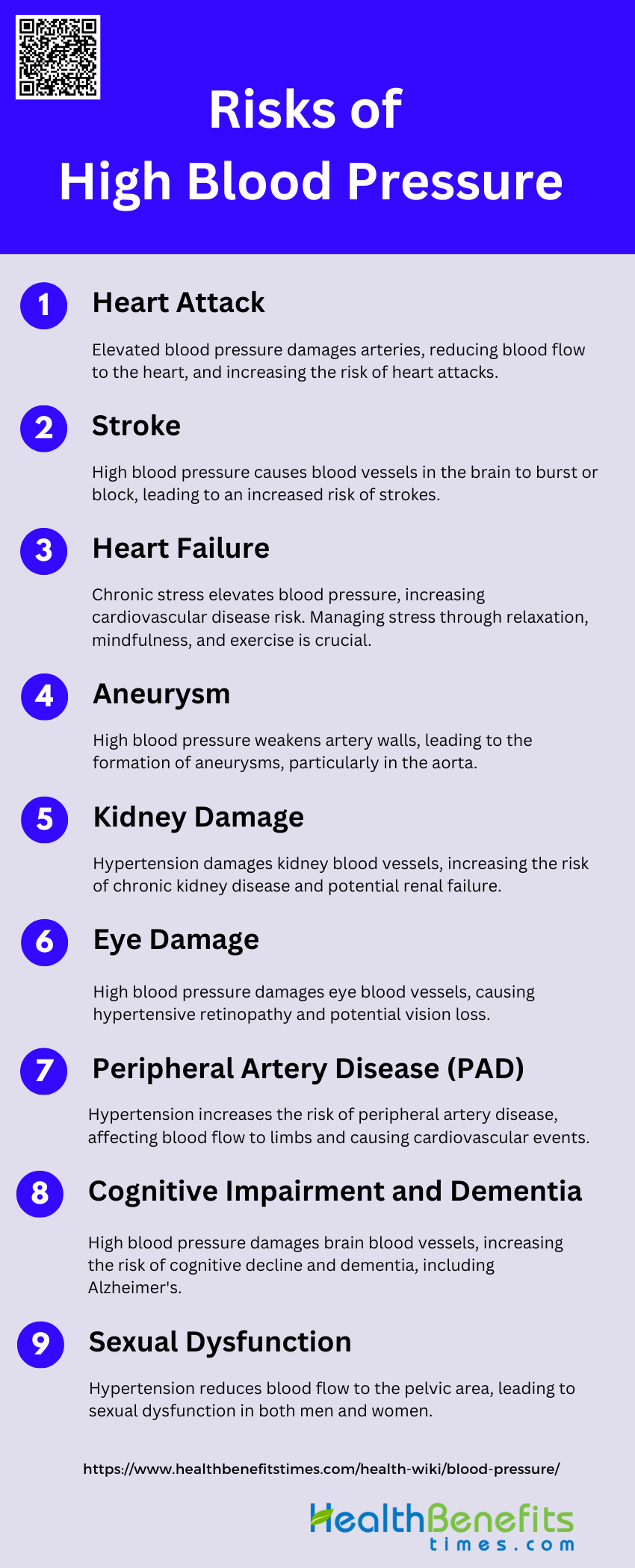
Risks of High Blood Pressure
High blood pressure, or hypertension, can lead to a variety of serious health complications if left unmanaged. It is crucial to be aware of these risks to take proactive measures for maintaining heart health. Below are some of the primary risks associated with high blood pressure:
1. Heart Attack
High blood pressure (BP) is a significant risk factor for heart attacks. Elevated BP causes damage to the arteries, making them less elastic, which decreases the flow of blood and oxygen to the heart. This can lead to a heart attack, as the heart muscle becomes starved of oxygen and nutrients. Studies have shown that reducing systolic BP by 12-13 mm Hg can lower the risk of coronary heart disease by 21%. Therefore, managing BP is crucial in preventing heart attacks.
2. Stroke
High blood pressure is the leading cause of strokes. It can cause blood vessels in the brain to burst or become blocked, leading to a stroke. Observational studies have demonstrated a continuous and graded relationship between systolic BP and the risk of stroke. Lowering BP has been shown to significantly reduce the incidence of stroke, with a 37% reduction observed in clinical trials. Thus, controlling BP is essential for stroke prevention.
3. Heart Failure
High blood pressure increases the risk of heart failure by causing the heart to work harder than normal, leading to the thickening of the heart muscle and eventually heart failure. Large cohort studies have confirmed that high BP is a critical risk factor for heart failure. Effective management of BP can significantly reduce the risk of developing heart failure, highlighting the importance of BP control in cardiovascular health.
4. Aneurysm
Hypertension is a major risk factor for the development of aneurysms, particularly aortic aneurysms. High BP can weaken the walls of the arteries, leading to the formation of an aneurysm. Observational studies have shown that hypertension is associated with an increased risk of aortic syndromes, including aneurysms. Therefore, maintaining normal BP levels is crucial in preventing aneurysms.
5. Kidney Damage
High blood pressure can cause damage to the kidneys’ blood vessels, leading to chronic kidney disease (CKD). Elevated BP increases glomerular pressure, which can result in renal failure. Studies have shown that controlling BP can help prevent the progression of CKD, emphasizing the importance of BP management in protecting kidney health.
6. Eye Damage
Hypertension can lead to damage to the blood vessels in the eyes, causing conditions such as hypertensive retinopathy. This can result in vision loss if left untreated. High BP is known to affect small blood vessels, including those in the eyes, leading to various forms of eye damage. Regular monitoring and control of BP are essential to prevent eye-related complications.
7. Peripheral Artery Disease (PAD)
High blood pressure is a significant risk factor for peripheral artery disease (PAD), which affects the arteries in the limbs. Studies have shown that patients with PAD often have a history of hypertension, and BP variability is associated with adverse cardiovascular and limb events. Effective BP management is crucial in reducing the risk and progression of PAD.
8. Cognitive Impairment and Dementia
Hypertension is linked to cognitive decline and dementia, including Alzheimer’s disease. High BP can cause damage to the brain’s blood vessels, leading to cognitive impairment. Long-term BP variability has been identified as an independent risk factor for dementia. Managing BP effectively can help reduce the risk of cognitive decline and dementia.
9. Sexual Dysfunction
High blood pressure can lead to sexual dysfunction in both men and women. It can cause reduced blood flow to the pelvic area, affecting sexual function. Hypertension is known to be associated with various forms of sexual dysfunction, and managing BP can help improve sexual health. Therefore, controlling BP is important for maintaining sexual function.
Risks of Low Blood Pressure
Low blood pressure, or hypotension, can lead to various health issues that may affect daily functioning and overall well-being. Recognizing these risks is essential for managing and mitigating potential complications. Below are some of the primary risks associated with low blood pressure:
1. Inadequate Blood Flow to Vital Organs
Low blood pressure can lead to inadequate blood flow to vital organs, resulting in insufficient oxygen and nutrient delivery. This can cause organ dysfunction and damage, particularly in the kidneys, heart, and brain. For instance, intraoperative hypotension has been associated with increased risks of acute kidney injury and myocardial injury due to inadequate perfusion during surgery. Additionally, chronic low blood pressure can impair the body’s ability to maintain adequate circulation, exacerbating the risk of organ failure.
2. Dizziness and Fainting
Dizziness and fainting are common symptoms of low blood pressure, often resulting from insufficient blood flow to the brain. This can lead to a sudden loss of consciousness, posing significant risks, especially in older adults. Studies have shown that individuals with chronic hypotension frequently experience dizziness and fainting, which can severely impact their quality of life and increase the risk of falls and related injuries.
3. Shock
Severe hypotension can lead to shock, a life-threatening condition characterized by critically low blood pressure and inadequate blood flow to the body’s tissues. Shock can result from various causes, including blood loss, severe infection, or heart failure. It requires immediate medical intervention to restore blood pressure and ensure adequate perfusion to vital organs. The association between low blood pressure and increased risk of shock highlights the importance of maintaining adequate blood pressure levels.
4. Cognitive Impairment
Low blood pressure has been linked to cognitive impairment due to reduced cerebral perfusion. Chronic hypotension can lead to insufficient blood flow to the brain, resulting in symptoms such as confusion, memory loss, and difficulty concentrating. Research indicates that individuals with chronic low blood pressure may experience adverse emotional states and depressive symptoms, further contributing to cognitive decline.
5. Cardiovascular Problems
While high blood pressure is a well-known risk factor for cardiovascular disease, low blood pressure can also pose significant risks. Studies have shown that excessively low blood pressure can increase the risk of cardiovascular events, particularly in patients with pre-existing conditions such as diabetes and coronary artery disease. For example, low diastolic blood pressure has been associated with an increased risk of cardiovascular death in diabetic patients with coronary artery disease.
6. Falls and Injuries
Low blood pressure can lead to postural hypotension, a condition where blood pressure drops significantly upon standing, causing dizziness and increasing the risk of falls. This is particularly concerning in older adults, who are more prone to falls and related injuries. Research has shown that postural hypotension is common in older individuals and is associated with an increased risk of falls and fractures.
7. Complications during Pregnancy
Hypotension during pregnancy can lead to complications for both the mother and the fetus. Pregnant women with low blood pressure may experience poor placental perfusion, which can result in fetal growth restriction and other adverse outcomes. Additionally, chronic hypotension in pregnant women can increase the risk of preterm delivery and low birth weight. Proper management of blood pressure during pregnancy is crucial to minimize these risks.
8. Increased Risk during Surgery
Intraoperative hypotension, or low blood pressure during surgery, is a common side effect of general anesthesia and can lead to adverse postoperative outcomes. Prolonged periods of low blood pressure during surgery can result in inadequate organ perfusion, increasing the risk of complications such as acute kidney injury, myocardial injury, and stroke. Maintaining stable blood pressure levels during surgery is essential to reduce these risks.
9. Interactions with Medications
Patients with low blood pressure who are treated with antihypertensive medications may experience hypotension-related adverse events, such as dizziness, weakness, and syncope. This is particularly concerning in older adults and those with multiple comorbidities. Studies have shown that low systolic blood pressure in patients treated with antihypertensives is associated with an increased risk of adverse events, highlighting the need for careful monitoring and adjustment of medication dosages.
Causes of High blood pressure
High blood pressure can result from a combination of lifestyle factors, genetic predispositions, and underlying health conditions. Identifying these causes is essential for effective management and prevention. Below are some of the primary causes of high blood pressure:
1. Age: As individuals age, the elasticity of their blood vessels decreases, leading to increased arterial stiffness and higher blood pressure levels.
2. Family History: Genetic predisposition plays a significant role in hypertension, with studies showing that individuals with a family history of high blood pressure are at a higher risk.
3. Obesity: Obesity is a major cause of hypertension due to increased activity of the renin-angiotensin-aldosterone system and sympathetic nervous system, leading to higher blood pressure.
4. Lack of Physical Activity: Physical inactivity contributes to weight gain and poor cardiovascular health, both of which are risk factors for developing high blood pressure.
5. Unhealthy Diet: Diets high in sodium, trans fats, and saturated fats are strongly linked to elevated blood pressure, while diets rich in potassium and polyunsaturated fats can help reduce it.
6. Excessive Alcohol Consumption: Increased alcohol intake is associated with acute elevations in blood pressure and long-term hypertension, particularly in individuals with existing high blood pressure.
7. Tobacco Use: Smoking and tobacco use cause immediate increases in blood pressure and long-term damage to blood vessel walls, contributing to sustained hypertension.
8. Stress: Chronic stress can lead to persistent elevations in blood pressure through increased sympathetic nervous system activity and hormonal changes.
9. Poor Sleep: Inadequate or poor-quality sleep is linked to higher blood pressure, as disrupted sleep patterns can affect cardiovascular health and increase hypertension risk.
10. Birth Control Pills: Oral contraceptives can elevate blood pressure in some women, particularly those with other risk factors for hypertension.
11. Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs can cause significant increases in blood pressure, especially in individuals with pre-existing hypertension, due to their effects on renal function and prostaglandin synthesis.
12. Hormonal Imbalances: Hormonal imbalances, such as those involving the thyroid or adrenal glands, can lead to secondary hypertension by affecting vascular resistance and fluid balance.
Causes of low blood pressure
Low blood pressure can arise from various factors, ranging from dehydration to underlying medical conditions. Recognizing these causes is essential for proper diagnosis and treatment. Below are some of the primary causes of low blood pressure:
1. Dehydration: Insufficient fluid intake or excessive fluid loss can reduce blood volume, leading to a drop in blood pressure. This can occur due to sweating, diarrhea, vomiting, or inadequate water consumption.
2. Heart Problems: Conditions like heart attack, heart failure, bradycardia, and heart valve issues can impair the heart’s ability to pump blood effectively, resulting in low blood pressure.
3. Endocrine Disorders: Hormonal imbalances from conditions such as diabetes, thyroid problems, and Addison’s disease can affect blood pressure regulation, potentially causing hypotension.
4. Severe Infection (Septicemia): When bacteria enter the bloodstream, they can produce toxins that affect blood vessels, leading to a dangerous drop in blood pressure known as septic shock.
5. Severe Allergic Reaction (Anaphylaxis): A life-threatening allergic response to drugs, foods, or insect stings can cause a sudden, severe drop in blood pressure, requiring immediate medical attention.
6. Blood Loss: Significant blood loss from injury, internal bleeding, or excessive menstrual flow can reduce blood volume, leading to a decrease in blood pressure.
7. Nutritional Deficiencies: Lack of essential vitamins like B-12 and folic acid can cause anemia, resulting in a lower-than-normal amount of healthy red blood cells and potentially leading to hypotension.
8. Autonomic Dysfunction: Disorders affecting the autonomic nervous system can impair the body’s ability to regulate blood pressure, particularly when changing positions, causing orthostatic hypotension.
9. Prolonged Bed Rest: Extended periods of inactivity can lead to cardiovascular deconditioning and a decrease in blood volume, potentially resulting in low blood pressure.
10. Postprandial Hypotension: Some individuals, especially older adults, may experience a drop in blood pressure 1-2 hours after eating due to blood flow changes during digestion.
11. Emotional Stress: Strong emotions, particularly fear or pain, can trigger a vasovagal response, causing a temporary drop in blood pressure and potentially leading to fainting.
12. Heart Medications: Certain drugs used to treat high blood pressure, such as diuretics, beta-blockers, and ACE inhibitors, can sometimes lower blood pressure too much.
13. Heat Exposure: High temperatures can cause blood vessels to dilate and lead to dehydration, both of which can contribute to a decrease in blood pressure.
14. Alcohol Consumption: Drinking alcohol can lead to dehydration and cause blood vessels to dilate, potentially resulting in a temporary drop in blood pressure.
How to Maintain Healthy Blood Pressure
Maintaining healthy blood pressure is essential for overall cardiovascular health and can be achieved through various lifestyle adjustments. By adopting certain habits and making mindful choices, you can effectively manage and prevent hypertension. Below are some key strategies to maintain healthy blood pressure:
1. Follow a Healthy Diet
Adopting a healthy diet is crucial for maintaining healthy blood pressure. The Dietary Approaches to Stop Hypertension (DASH) diet, which is rich in fruits, vegetables, and low-fat dairy products, has been shown to significantly lower blood pressure. This diet reduces systolic and diastolic blood pressure by 5.5 and 3.0 mm Hg, respectively, compared to a control diet. The Mediterranean diet, which includes whole grains, vegetables, fruits, nuts, and extra virgin olive oil, also has a favorable effect on blood pressure. These dietary patterns are effective because they are low in saturated fats and high in essential nutrients like potassium, magnesium, and fiber.
2. Exercise Regularly
Regular physical activity is another key factor in maintaining healthy blood pressure. Exercise helps to strengthen the heart, enabling it to pump blood more efficiently, which reduces the pressure on the arteries. Studies have shown that engaging in moderate-intensity exercise, such as brisk walking, for at least 150 minutes per week can significantly lower blood pressure. Exercise also helps in weight management, which is another important aspect of controlling blood pressure.
3. Maintain a Healthy Weight
Maintaining a healthy weight is essential for blood pressure control. Excess body weight increases the strain on the heart and can lead to higher blood pressure. Weight loss has been shown to reduce blood pressure significantly. For instance, a reduction in body weight by just 5-10% can lead to a noticeable decrease in blood pressure levels. Combining a healthy diet with regular exercise is the most effective way to achieve and maintain a healthy weight.
4. Manage Stress
Chronic stress can contribute to high blood pressure. Stress management techniques such as mindfulness, meditation, deep breathing exercises, and yoga can help lower stress levels and, consequently, blood pressure. Studies have shown that these practices can lead to reductions in both systolic and diastolic blood pressure. Additionally, engaging in hobbies and activities that you enjoy can also help manage stress effectively.
5. Limit Harmful Substances
Limiting the intake of harmful substances such as alcohol and tobacco is crucial for maintaining healthy blood pressure. Excessive alcohol consumption can raise blood pressure, while smoking damages blood vessels and accelerates the hardening of the arteries. Reducing alcohol intake to moderate levels and quitting smoking can lead to significant improvements in blood pressure and overall cardiovascular health.
6. Monitor Blood Pressure Regularly
Regular monitoring of blood pressure is important for early detection and management of hypertension. Home blood pressure monitors can help individuals keep track of their blood pressure levels and make necessary lifestyle adjustments. Regular monitoring also helps in assessing the effectiveness of any ongoing treatment and in making timely decisions regarding medication adjustments.
7. Take Medications as Prescribed
For individuals diagnosed with hypertension, taking medications as prescribed by a healthcare provider is essential. Antihypertensive medications help to control blood pressure and prevent complications such as heart disease and stroke. It is important to follow the prescribed dosage and schedule, and to consult with a healthcare provider before making any changes to the medication regimen.
8. Reduce Salt Intake
Reducing salt intake is one of the most effective dietary changes for lowering blood pressure. High sodium intake is associated with increased blood pressure. Studies have shown that reducing sodium intake can lead to significant reductions in both systolic and diastolic blood pressure. The DASH diet, which emphasizes low sodium intake, has been particularly effective in lowering blood pressure.
9. Get Regular Medical Check-Ups
Regular medical check-ups are important for monitoring blood pressure and overall health. These check-ups allow healthcare providers to detect any early signs of hypertension and to provide timely interventions. Regular check-ups also help in monitoring the effectiveness of lifestyle changes and medications, and in making necessary adjustments to the treatment plan.
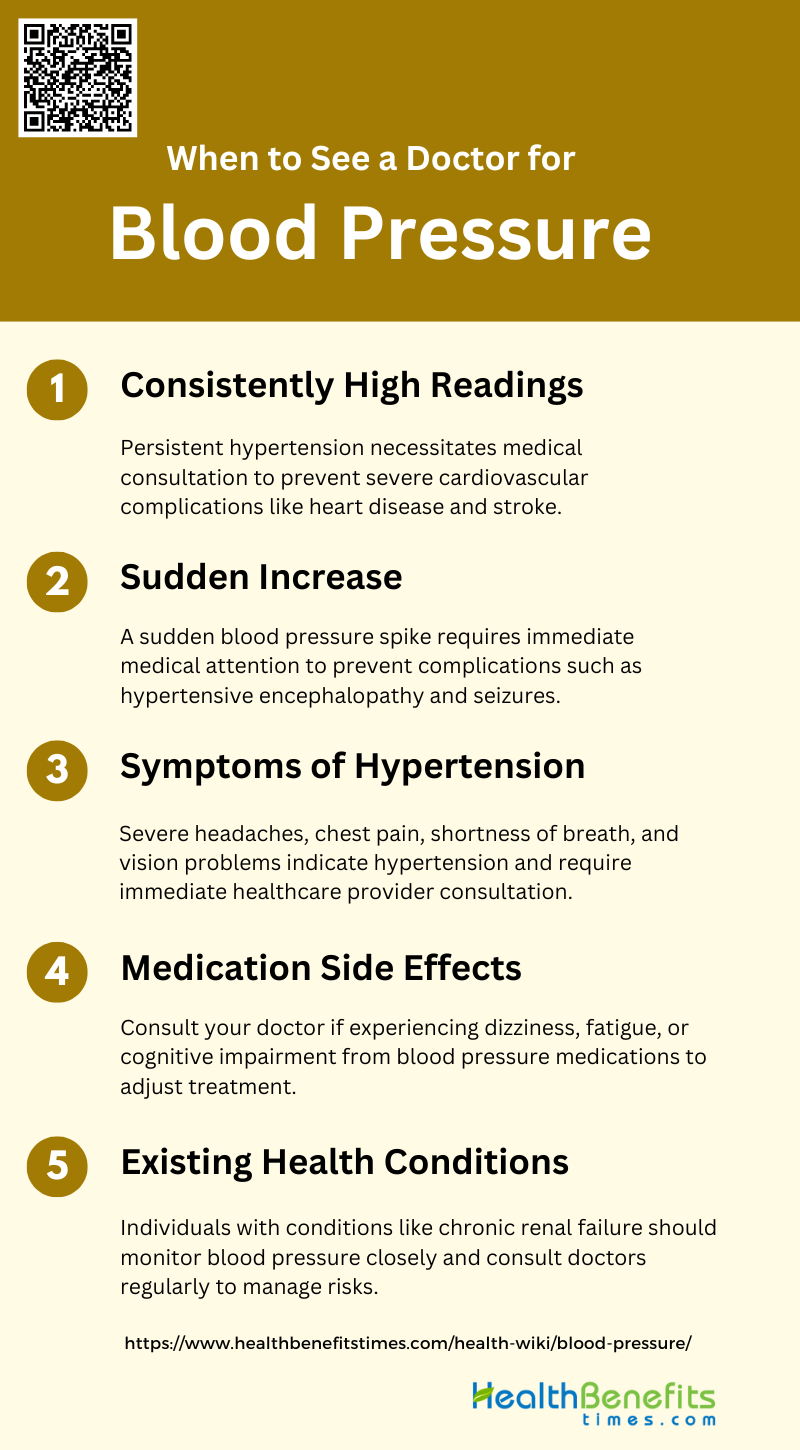
When to See a Doctor for Blood pressure
It’s important to know when to seek medical advice for blood pressure issues to prevent potential complications. Here are some situations when you should see a doctor:
1. Consistently High Readings
Consistently high blood pressure readings are a significant indicator that you should see a doctor. Persistent hypertension can lead to severe cardiovascular complications, including heart disease and stroke. Studies have shown that intensive blood pressure treatment can substantially improve outcomes in patients with moderate to severe hypertension, reducing the risk of mortality, stroke, and cardiac events. Regular monitoring and medical consultation are crucial to manage and mitigate these risks effectively.
2. Sudden Increase
A sudden increase in blood pressure can be alarming and warrants immediate medical attention. Acute elevations in blood pressure, especially during treatments like recombinant human erythropoietin (rHuEPO) therapy, can lead to severe complications such as hypertensive encephalopathy and seizures. These sudden spikes are often unrelated to the dosage or rate of increase in hematocrit but are associated with rapid increases in blood pressure, necessitating prompt medical intervention to prevent serious health issues.
3. Symptoms of Hypertension
Symptoms of hypertension, such as severe headaches, chest pain, shortness of breath, and vision problems, should prompt an immediate visit to a healthcare provider. Hypertension is often called the “silent killer” because it can cause significant damage to the cardiovascular system without noticeable symptoms until it reaches a critical level. Intensive blood pressure management in older adults has been shown to reduce the risk of severe outcomes, including stroke and cardiac events, highlighting the importance of early detection and treatment.
4. Medication Side Effects
If you experience side effects from blood pressure medications, it is essential to consult your doctor. Common adverse effects include dizziness, fatigue, and cognitive impairment, which can significantly impact your quality of life. Adjusting the medication type or dosage under medical supervision can help manage these side effects while maintaining effective blood pressure control. Regular follow-ups are crucial to ensure that the benefits of the medication outweigh the potential harms.
5. Existing Health Conditions
Individuals with existing health conditions, such as chronic renal failure, should be particularly vigilant about their blood pressure. Treatments like rHuEPO can exacerbate hypertension, necessitating the initiation or adjustment of antihypertensive therapy. Managing blood pressure in the context of other health conditions requires a tailored approach to avoid complications and ensure overall health stability. Regular medical consultations are essential to monitor and adjust treatment plans as needed.